
خير الناس من نفع الناس
)
)
مجمىعت منتخبت من الساليذاث الطبيت تم
جمعها وصياغتها هي هذيتي المتىاضعت
الى ابنائي وبناتي طلبت المرحلت السادست
األعزاء متمنين لهم التىفيق واالستفادة منها
والذعاء لنا
د
.
اسماعيل
2016
PICTURES
IN
GENERAL
MEDICINE
More than 150 medical pictures are collected and edited
specially for teaching purpose of sixth year undergraduate
students. No one is authorized to add, delete, distribute
and use these slides for purposes other than teaching
without prior permission.
For each picture there is/are a question/questions followed
by an answer in the next slide
دكتىر اسماعيل داود
فرع الطب
–
كليت طب المىصل
2016

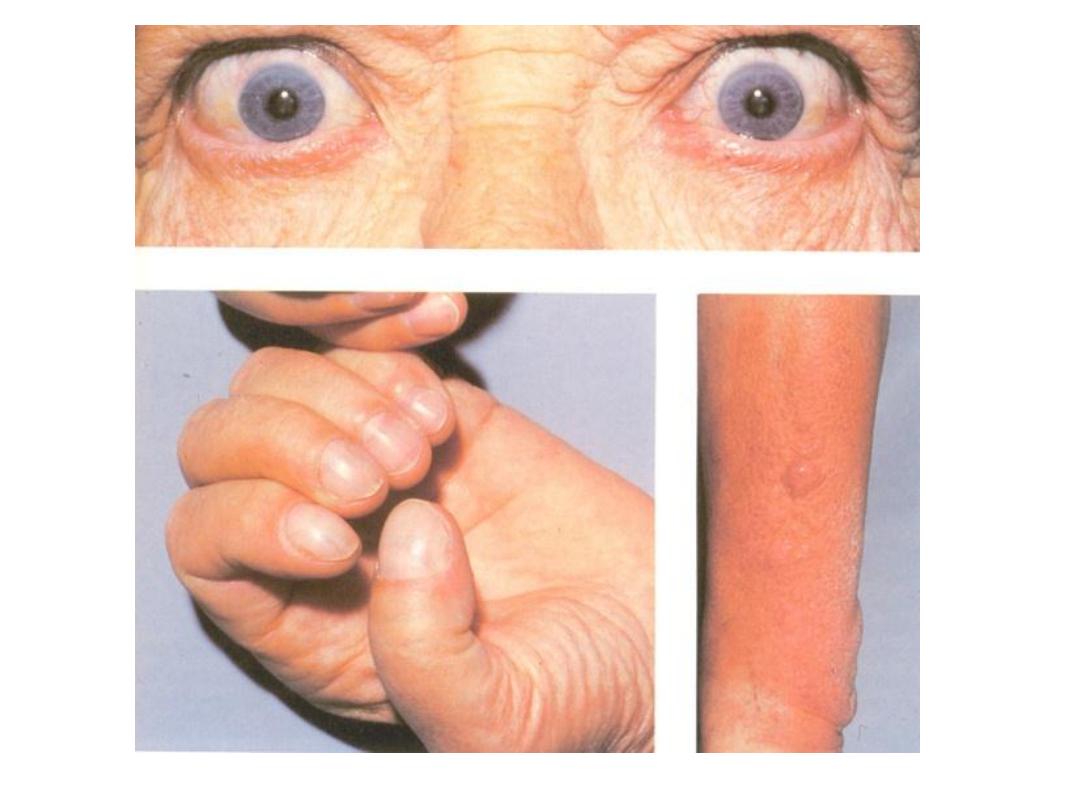
What is the diagnosis? What are
the systemic complications

The patient received a diagnosis of neurofibromatosis
type 1, a syndrome caused by neurogenic tumors
arising from neural sheath cells located along
peripheral and cranial nerves. Inheritance is
autosomal dominant, although half of cases are
caused by a spontaneous mutation. Clinical findings
can include Lisch nodules of the iris, schwannomas,
café au lait macules, axillary freckling, optic-nerve
gliomas, astrocytomas, multiple neurofibromas, and
plexiform neurofibromas.
2. Hypertension and mass effects.

What is the diagnosis?
Reactivation of varicella-zoster virus (VZV) that has remained
dormant within dorsal root ganglia, often for decades after the
patient’s initial exposure to the virus in the form of varicella
(chickenpox), results in herpes zoster (shingles).
[1]
Although it is
usually a self-limited dermatomal rash with pain, herpes zoster can
be far more serious; in addition, acute cases often lead to
postherpetic neuralgia (PHN).

What is the diagnosis?
This patient had a 4-month history of
painful
and
progressive
ischemic
gangrene of the right lower leg. The
ankle
brachial index was 0.2 in the right
leg and 0.8 in the left leg. He elected to
be managed conservatively.

What is the diagnosis? Enumerate 3 causes.
Pyoderma gangrenosum is an uncommon cause of skin
ulceration. It may affect any part of the skin, but the lower
legs are the most common site.
Pyoderma gangrenosum often affects a person with an
underlying internal disease such as:
Systemic Causes:
■Inflammatory bowel diseases (ulcerative colitis and Crohn
disease)
■Rheumatoid arthritis
■Myeloid blood dyscrasias
■Chronic active hepatitis.
■Wegener granulomatosis

What is the diagnosis? What is
the underlying cause?

Necrobiosis Lipoidica Diabeticorum (NLD)
– It is a rash that
occurs gradually and affects the shins. It looks like a patch
of plaque and its color can range from yellow to purple. The
affected area of skin tends to get thinner and starts
developing ulcers.
Occurs in Diabetes Mellitus.
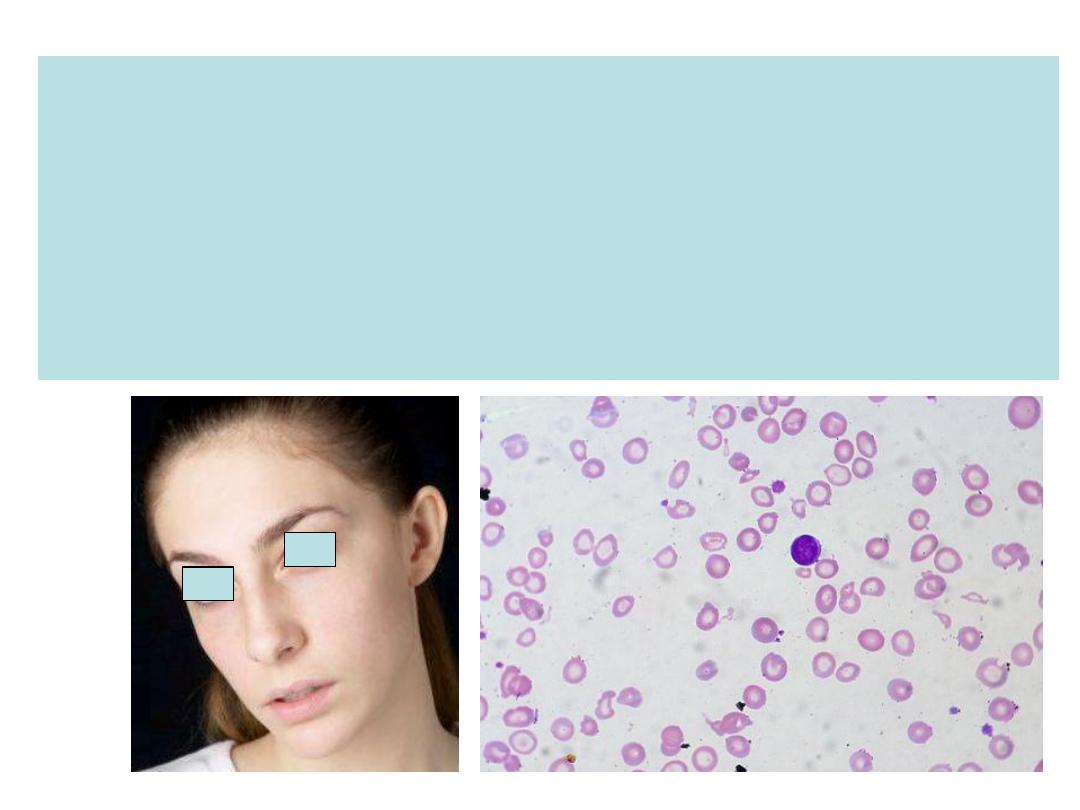
This young female patient is suffering from recent onset dysphagia
A. Is her symptom has any relation with her blood film.
B. How do you treat her dysphagia if other serious causes are
excluded?
C. Name other important physical signs associated with this
condition.
D. If a 70-year-old present with same symptom, do you change
your diagnosis and why? The answers are in the next slide.
A. Yes, iron deficiency anemia causing
post-cricoid's web. This is called
Paterson-Kelly or Plummer-Vinson
syndrome.
B. By treating her iron deficiency and some
time the web may be disrupted during
endoscopy.
C. Pallor (anaemia) and Koilonychia.
Anaemia and dysphagia in this age are due
to ca. esophagus or proximal stomach
unless proved otherwise
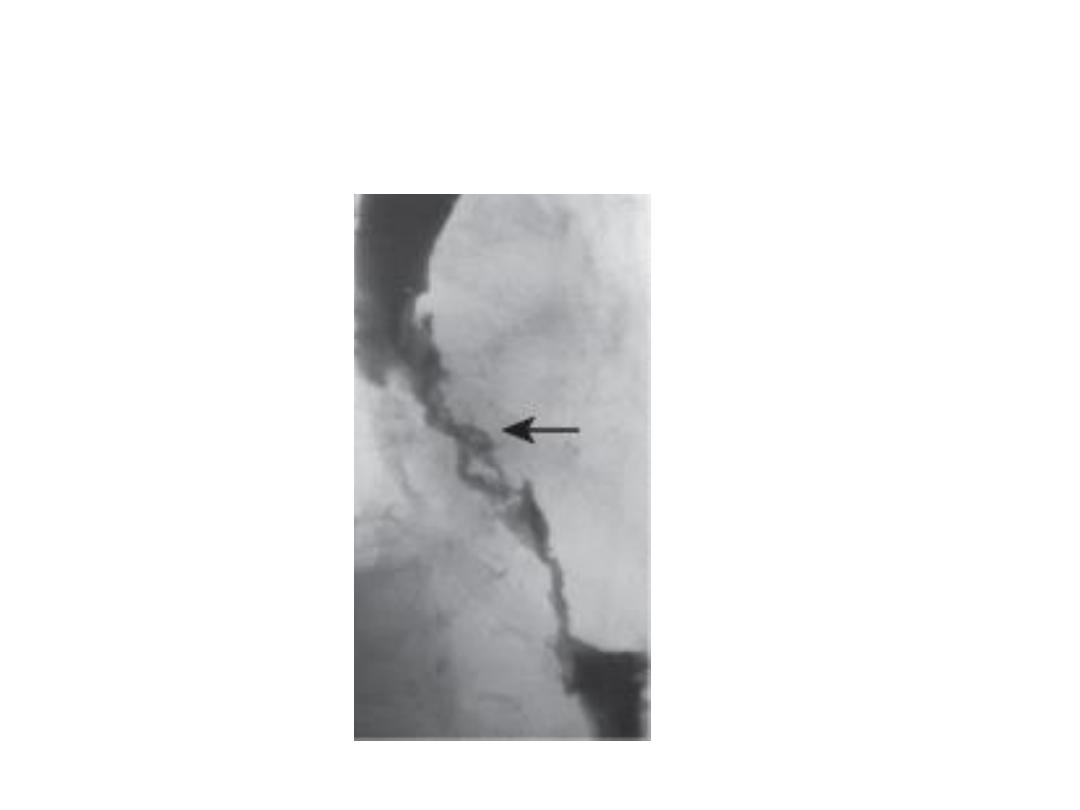
A long irregular stricture (arrowed) caused
by oesophageal cancer.
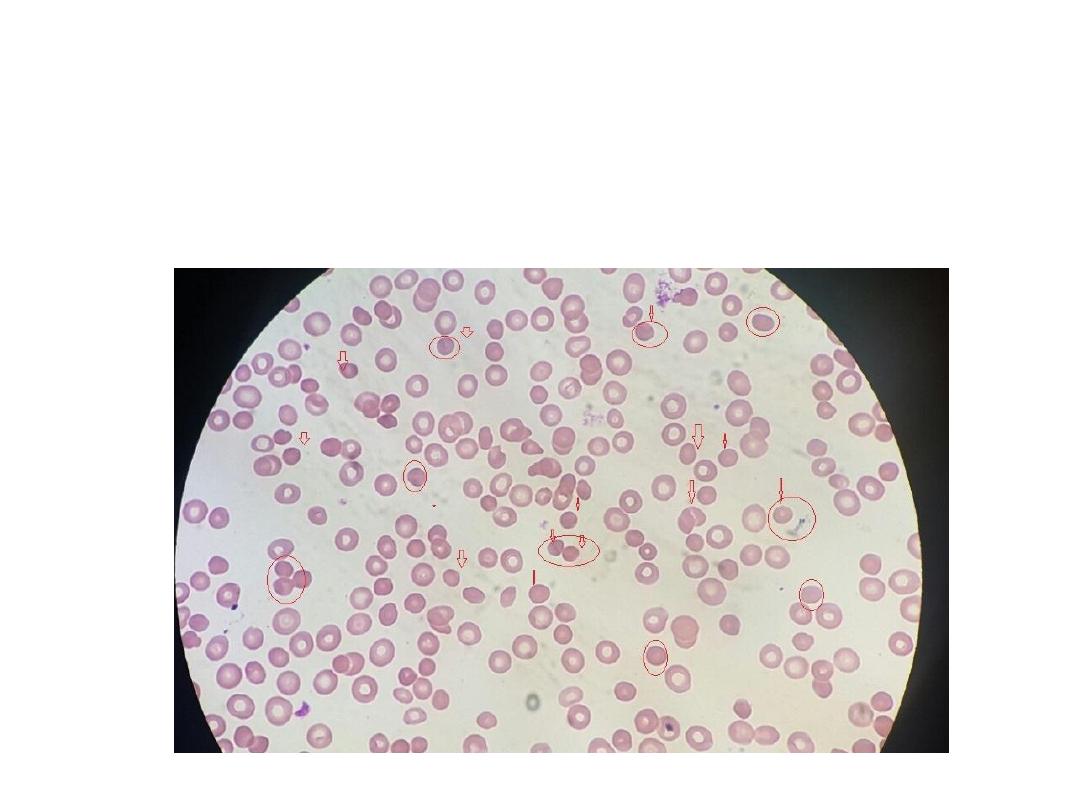
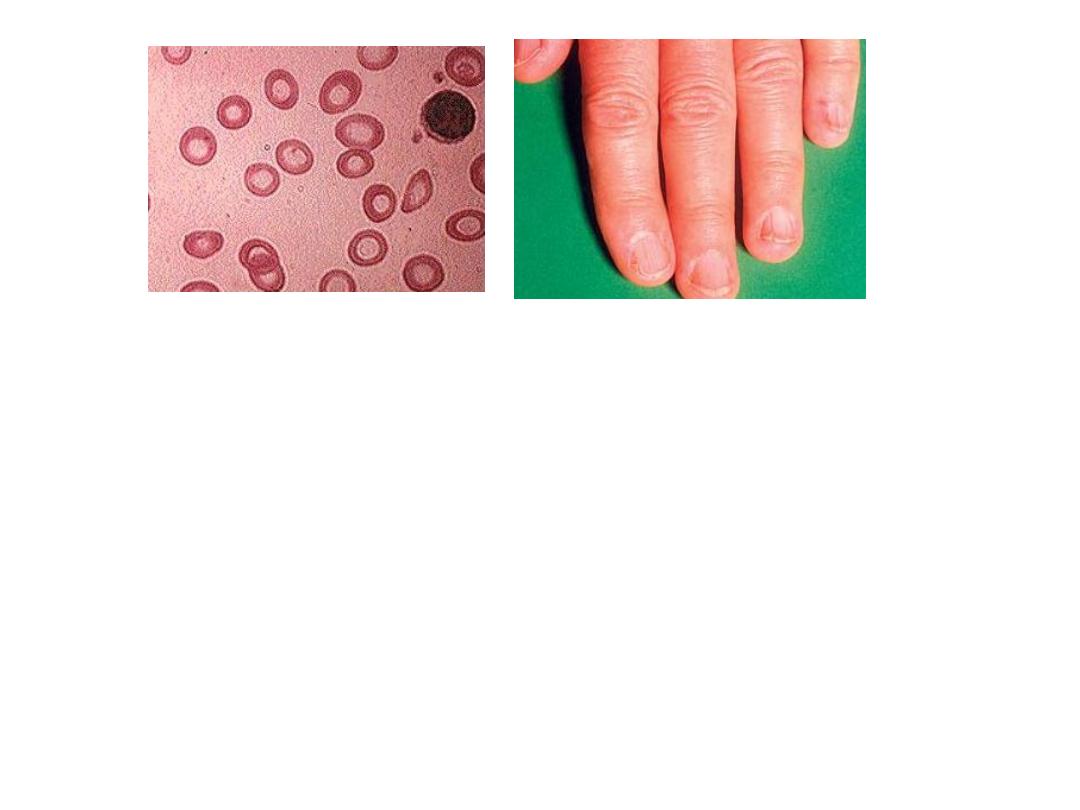
This is a blood film of 15-year-old male patient presented
with pallor, excessive fatigue and splenomegaly. Comb's
test was negative. What is the main finding and what is
diagnosis?

Spherocytes.
Diagnosis
: Hereditary spherocytosis.

This child had history of a
disease during last few
months. He suffers
from recent onset
alopecia and he is pale.
His blood film showed
very high count of cells
shown on the right.
A. What is the most likely
cause for his alopecia?
B. What is the most likely
diagnosis?
Answer
A. Cytotoxic therapy.
B. ALL (Acute lymphoblastic leukaemia0.
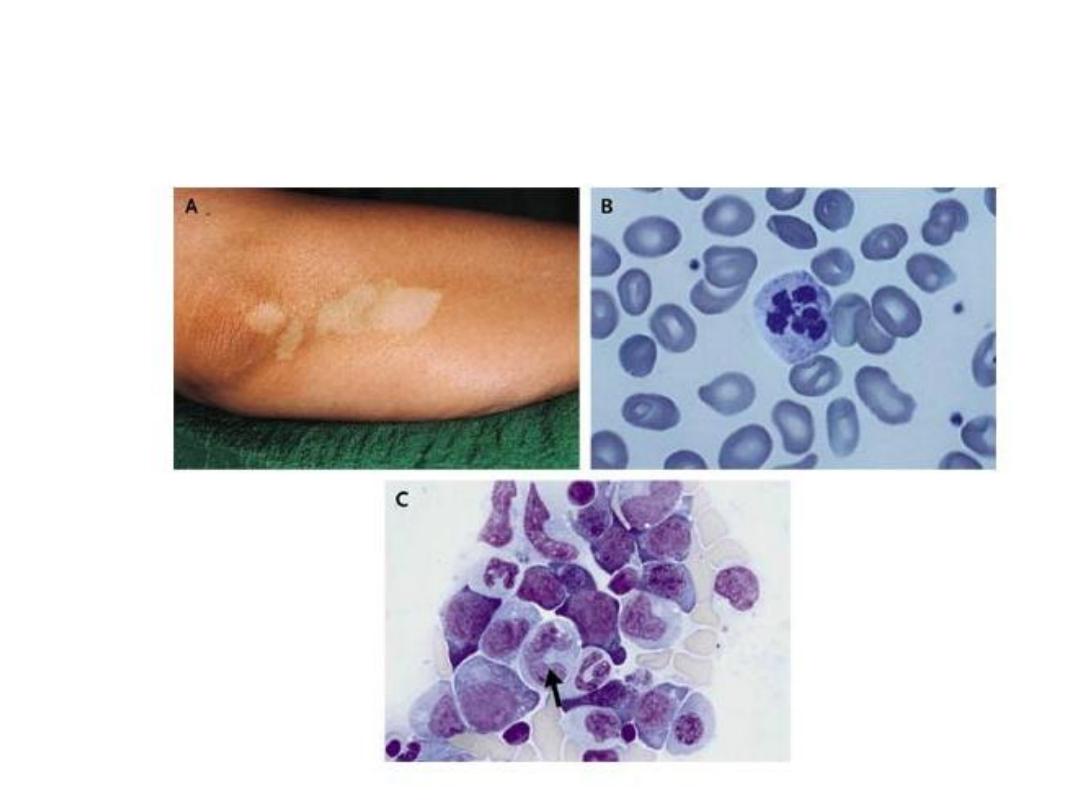
What is the association between skin
lesion and blood film?

A. Vetiligo: skin depigmentation
B. Macro and ovalocytosis: B12 deficiency (lack of
intrinsic factor due to atrophic gastritis).
C. Megaloblasts
These are autoimmune associated diseases.
Also look for atrophic gastritis.
The next slide is also related but resulted from
gastrectomy rather than autoimmunity.
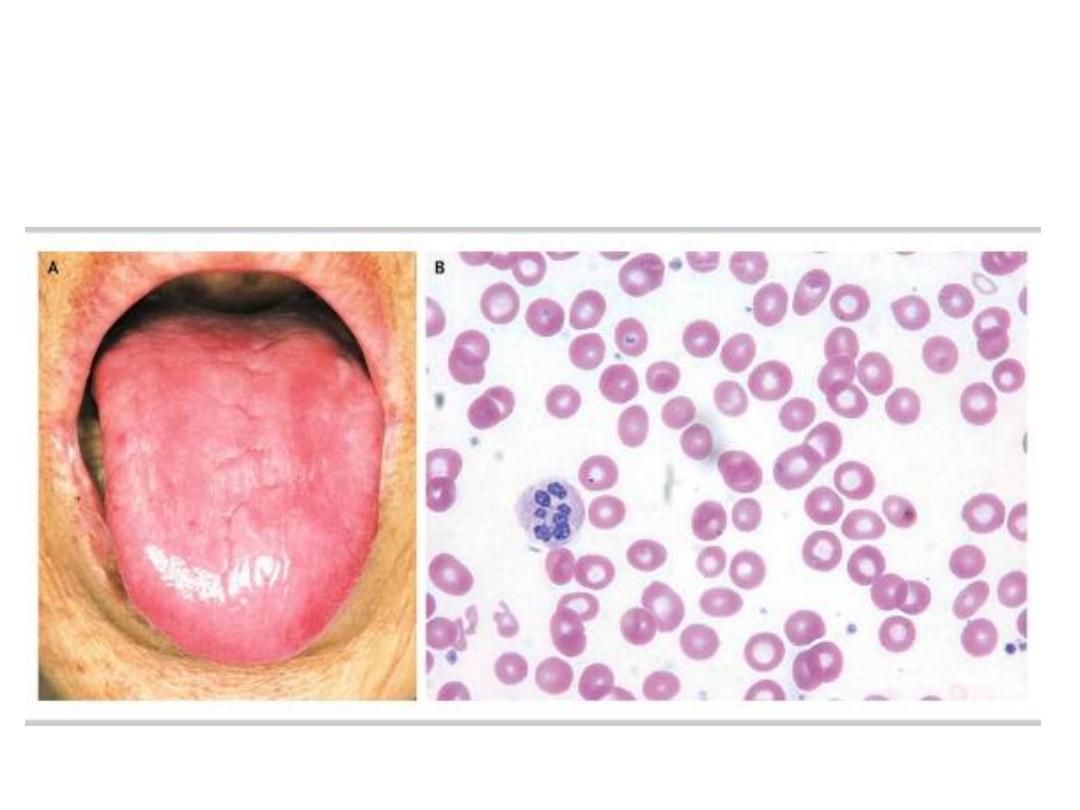
the tongue and blood with
history of gastroectomy
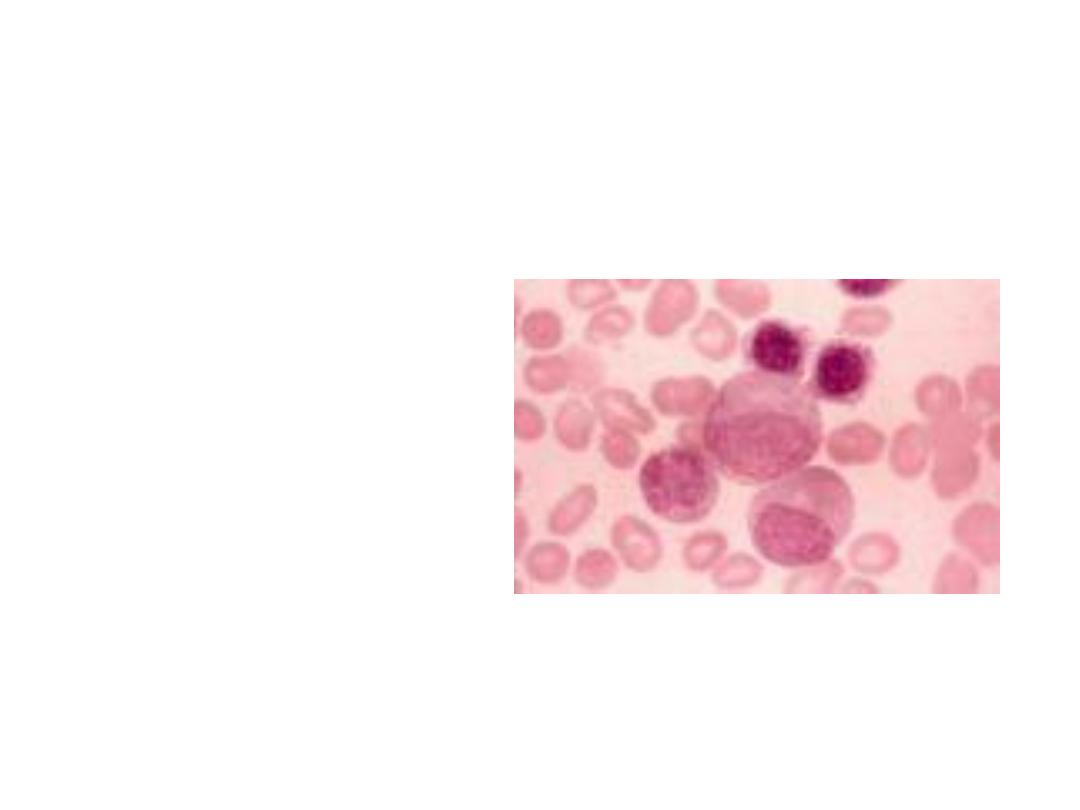
Myeloblasts
What are the
histochemical stains
which can
differentiate between
acute lymphoblastic
and myeloblastic
leukemia?
See textbook
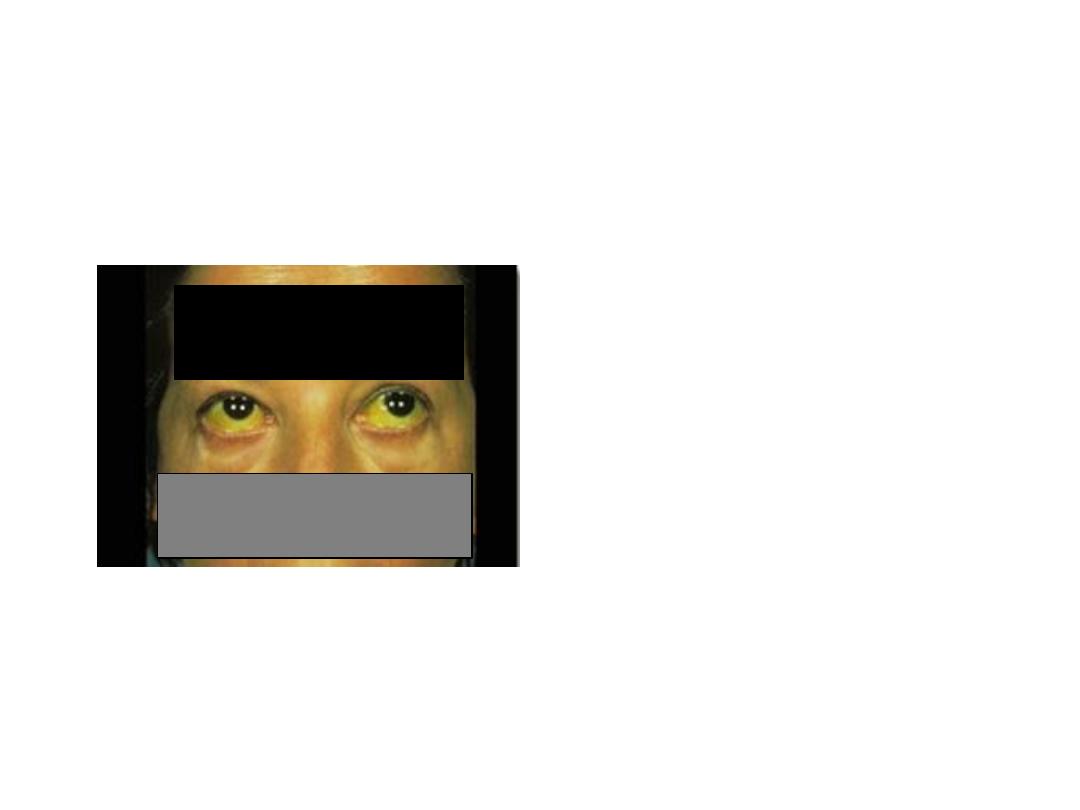
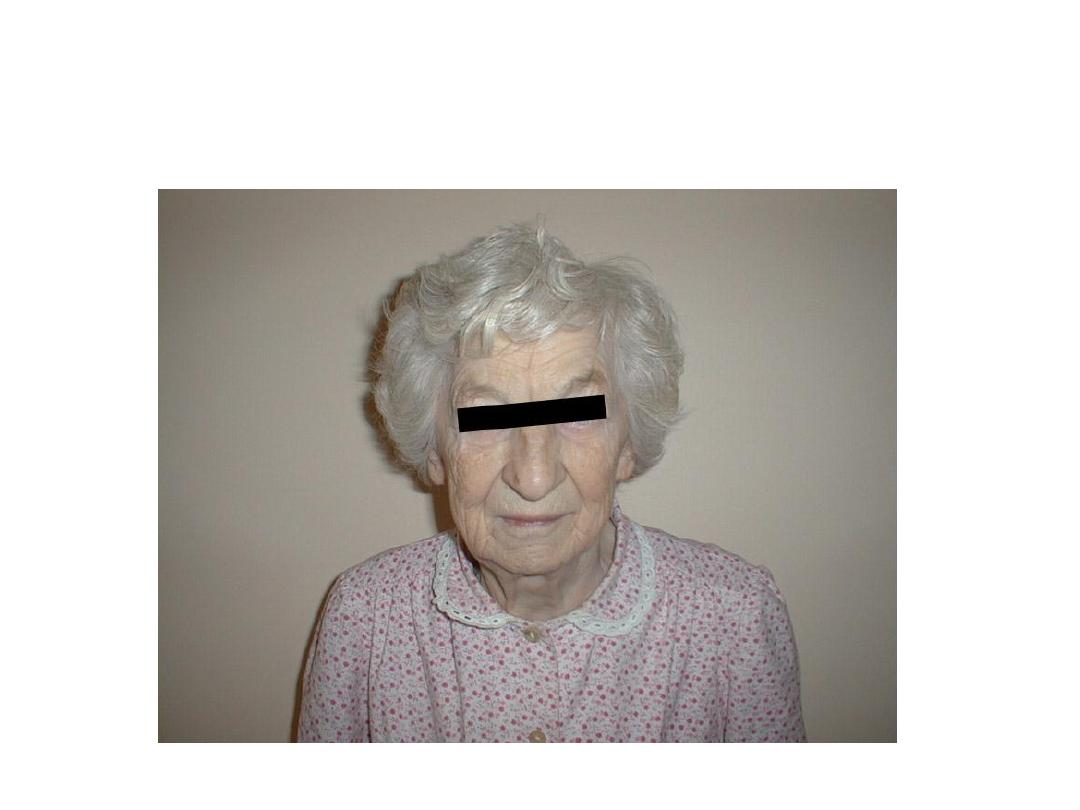
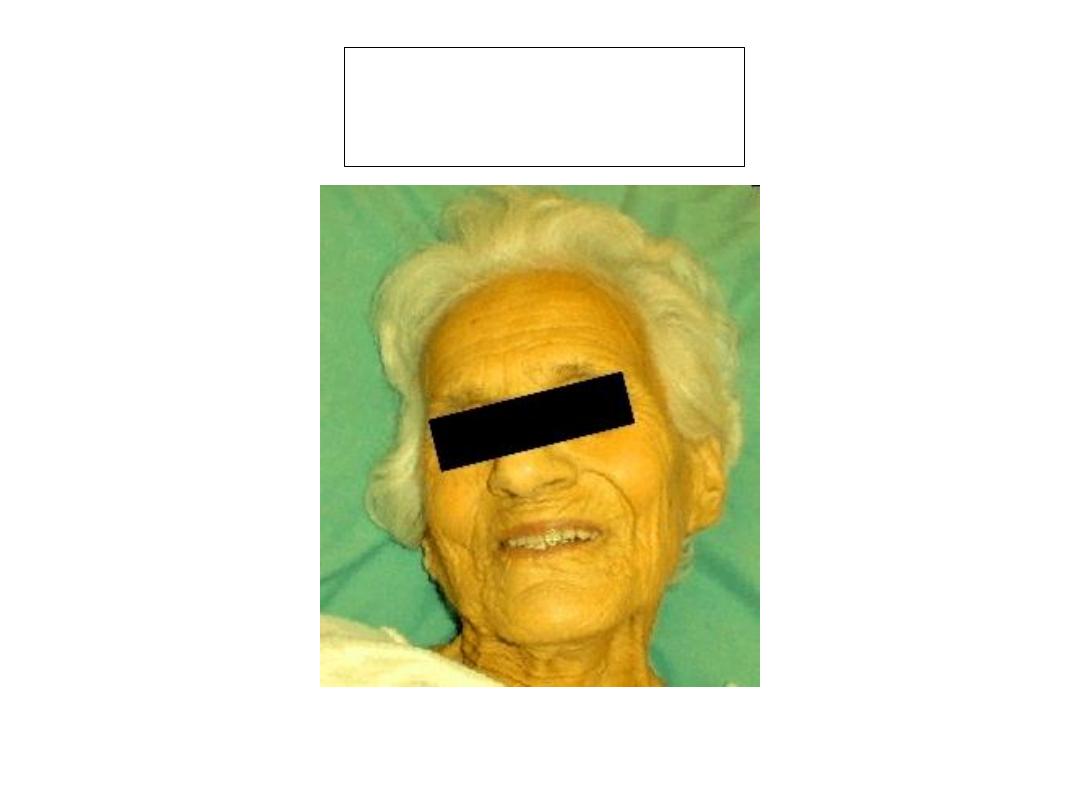
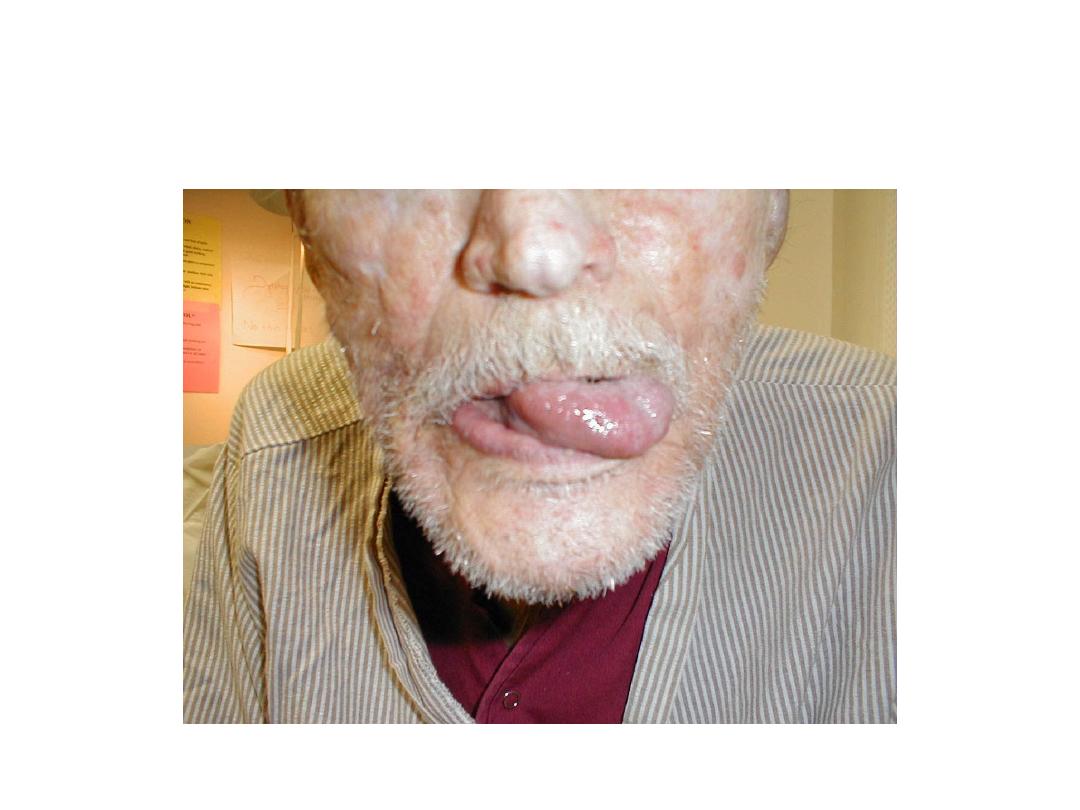
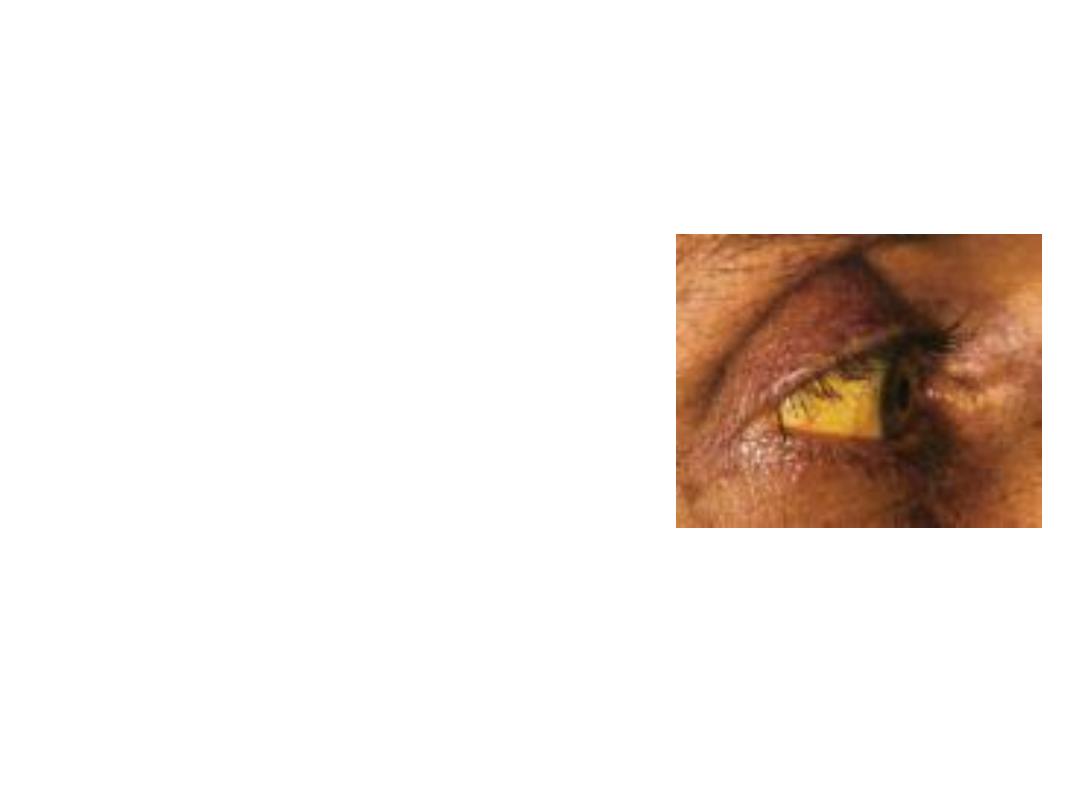
Look to the face of this patient.
Describe the finding and comment on
causes. The answer in next slide
Answer: Jaundice
Classified as :
1. Hemolytic: Usually mild with changes in blood film and CBC.
2. Congenital non-haemolytic: Usually mild and benign in most cases. The
commonest is Gilbert syndrome or disease.
3. Hepatocellular: drugs, infection(viral, bacterial, protozoa) , ischemic, metabolic,
hereditary, alcohol, NASH, etc. Do liver function test
4. Obstructive: intra and extra hepatic causes. Extra-hepatic: CBD stones, CBD
strictures, primary sclerosing cholangitis, parasitic obstruction of CBD like
Hydatid cyst, ascariasis, etc. ca. of head of pancreas. Usually severe and
progressive.
Progressive jaundice
Carcinoma of head of pancreas

What is the most likely diagnosis. How would you confirm the
diagnosis? Enumerate hormonal, Metabolic changes and complications
in this patient. The answer in next slide.


Cushing’s syndrome
is caused by excessive activation of glucocorticoid receptors.
It is most commonly iatrogenic, due to prolonged administration of synthetic
glucocorticoids such as prednisolone. Endogenous Cushing’s syndrome is
uncommon but is due to chronic over-production of cortisol by the adrenal glands,
either as the result of an adrenal tumour or because of excessive
production of ACTH by a pituitary tumour or ectopic ACTH production by other
tumours.
Complications:
Osteoporosis, compression fracture, Tendency to infections with
poor wound healing and little inflammatory response, Hyperglycaemia, Menstrual
disturbance, Peptic ulcer, Hypertension, psychosis, etc.

Tests
to Diagnose Cushing’s Syndrome:
1. 24-hour urinary free cortisol level. up to three 24-h urine collections
should be performed. If cortisol excretion results are normal in three
collections, then CS is highly unlikely, Levels higher than 50 to 100
micrograms a day for
an adult suggest Cushing’s syndrome.
2. Midnight plasma cortisol and late-night salivary cortisol measurements:
The midnight plasma cortisol test also measures cortisol concentrations
in the blood. Cortisol production is normally suppressed at night, but in
Cushing’s syndrome, this suppression doesn’t occur.
3. Low-dose dexamethasone suppression tests (LDDST): Consists of the
oral intake of 1 mg dexamethasone between 2300 and 2400 h, followed
by measurement of fasting plasma cortisol between 0800 and 0900 h the
following morning. A serum cortisol level below 1.8
μg/dl (50 nmol/liter)
excludes active CS at that time.
4. Late-night salivary cortisol.

This patient complains
of tiredness.
A. What principle
abnormality is seen
in
1. Hands?
2. The abdominal X-
ray.
B. What is the
diagnosis, and what
is the likely
underlying cause in
this case?
A.
1. Hyperpigmentation
2. Adrenal calcification
B. Addison’s disease due to tuberculosis.

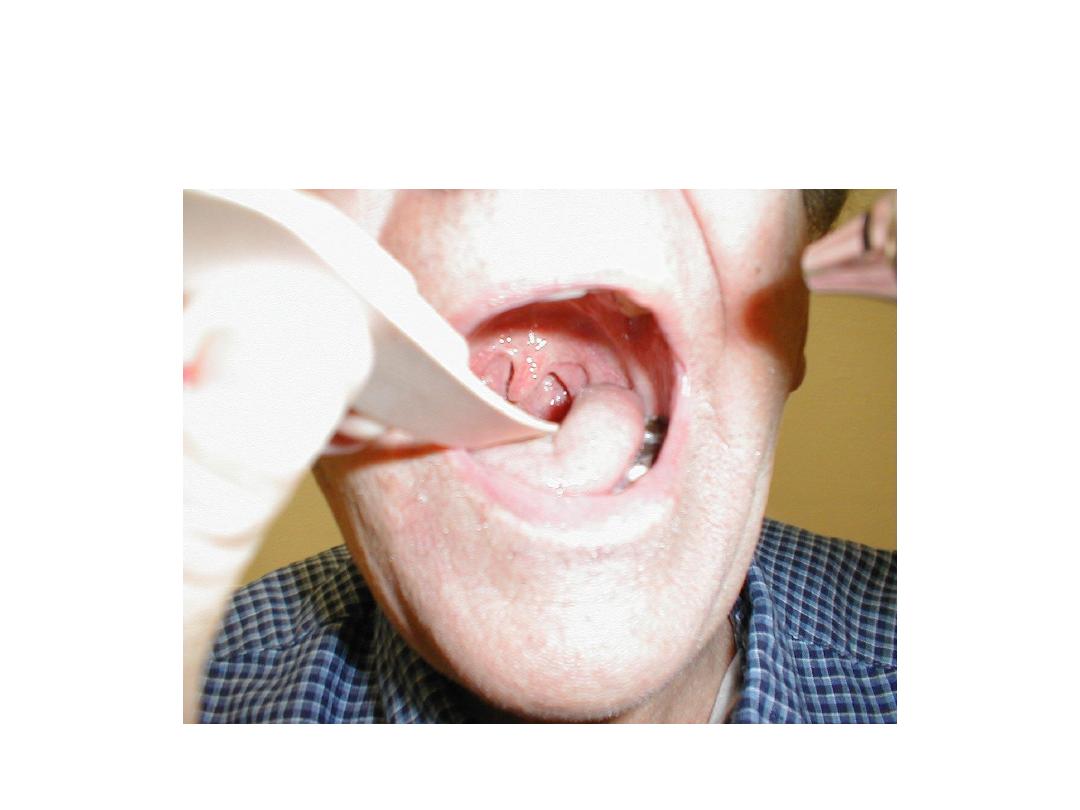
This patient is dyspnic. What are other areas to
look for? Mention the mechanism and
enumerate some causes
1. Central cyanosis as the patient is dyspnic. It is
due presence of reduced haemoglobin (at
least 5 gm/dl).
2. Look to the tongue.
3. Some causes:
•
Respiratory diseases: like COPD, Severe
pneumonia, tension pneumothorax,…etc.
•
Cardiovascular: like cyanotic congenital heart
diseases, bacterial endocarditis, and severe
heart failure.
•
Others: like septicaemia
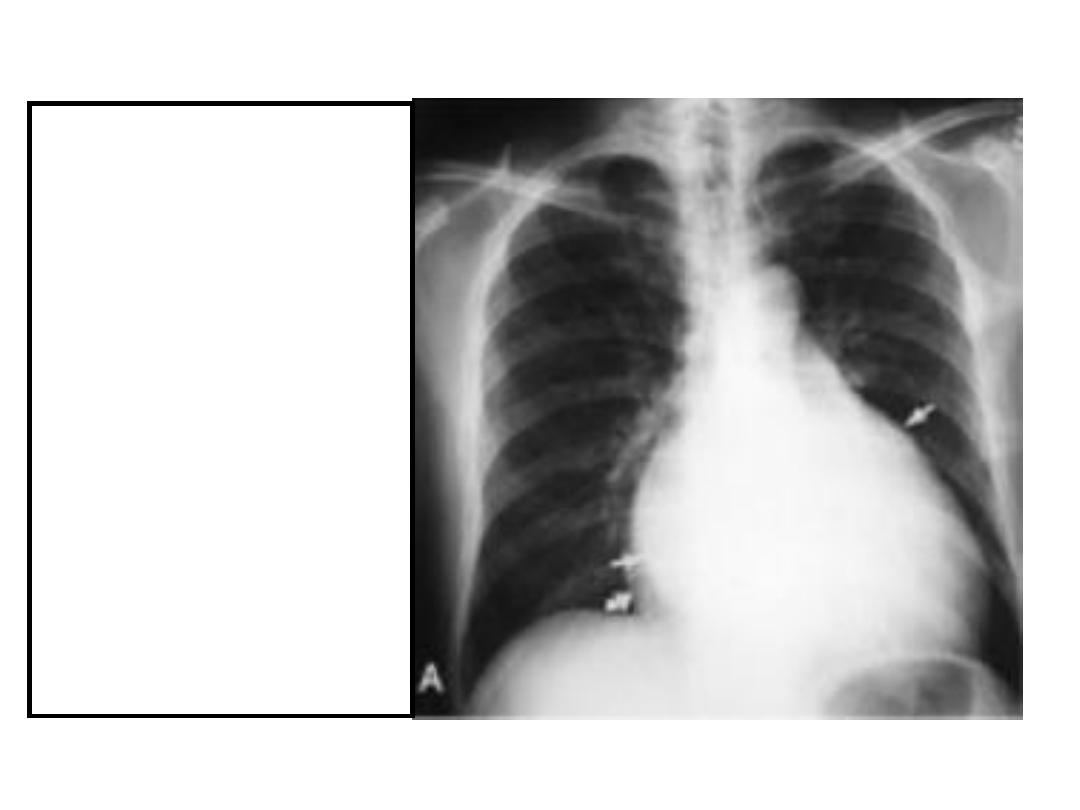
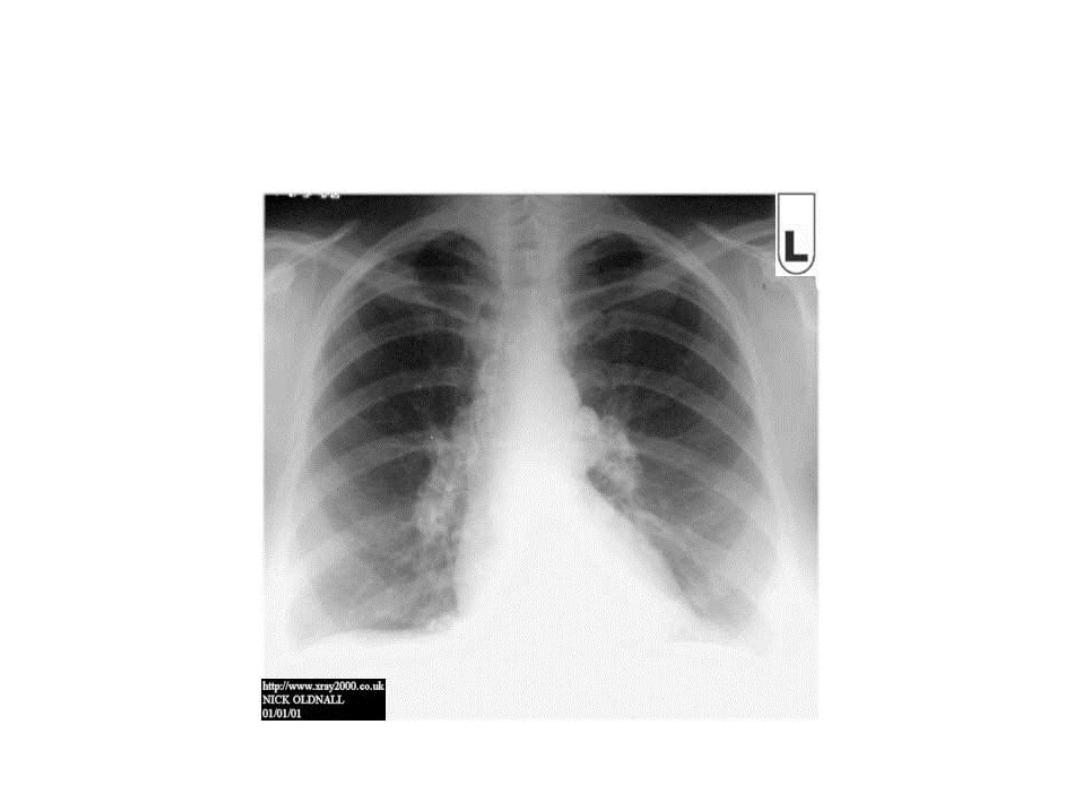
A. What are the
important findings
In this chest X-ray?
B. What is the
most likely
Diagnosis?
C. Enumerate 3
physical signs
that may be helpful
for diagnosis?
A. 1. Straightening of the left cardiac
border due to enlarged pulmonary trunk.
2. Double shadow of the R heart border
due to L atrial enlargement.
3. Distended pulmonary veins.
B. Mitral stenosis.
C. Tapping cardiac apex beat, loud S
1
and
mid-diastolic rumbling murmur.
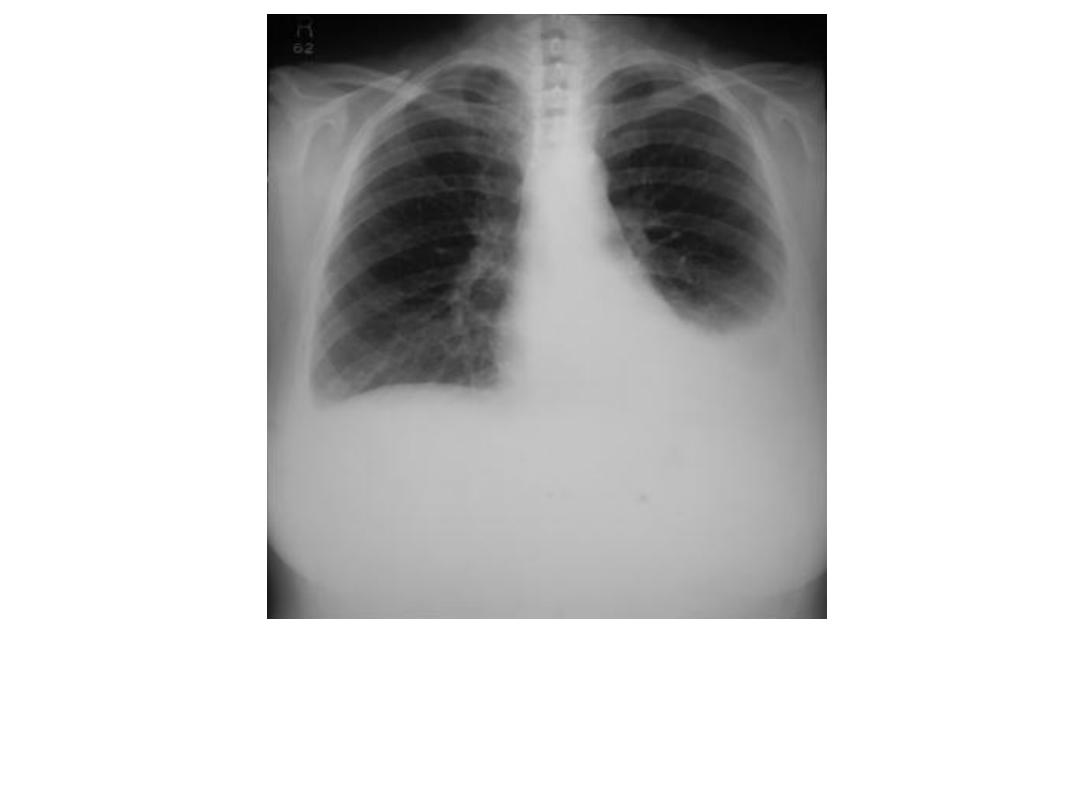
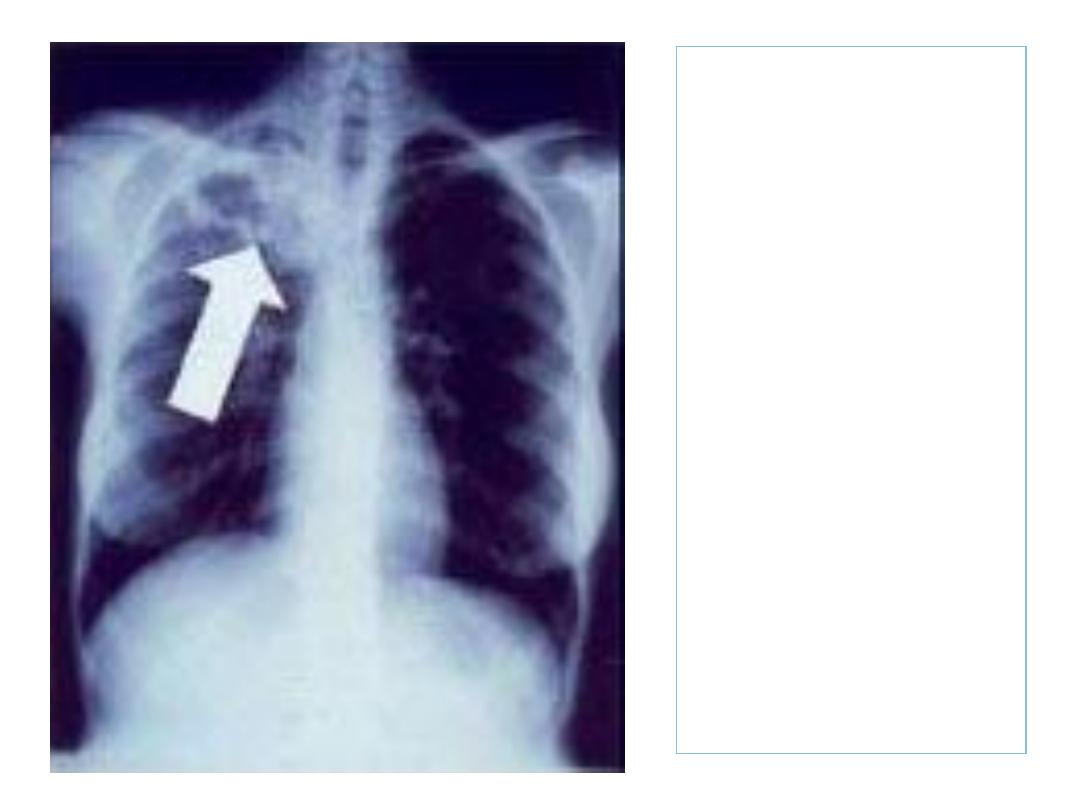
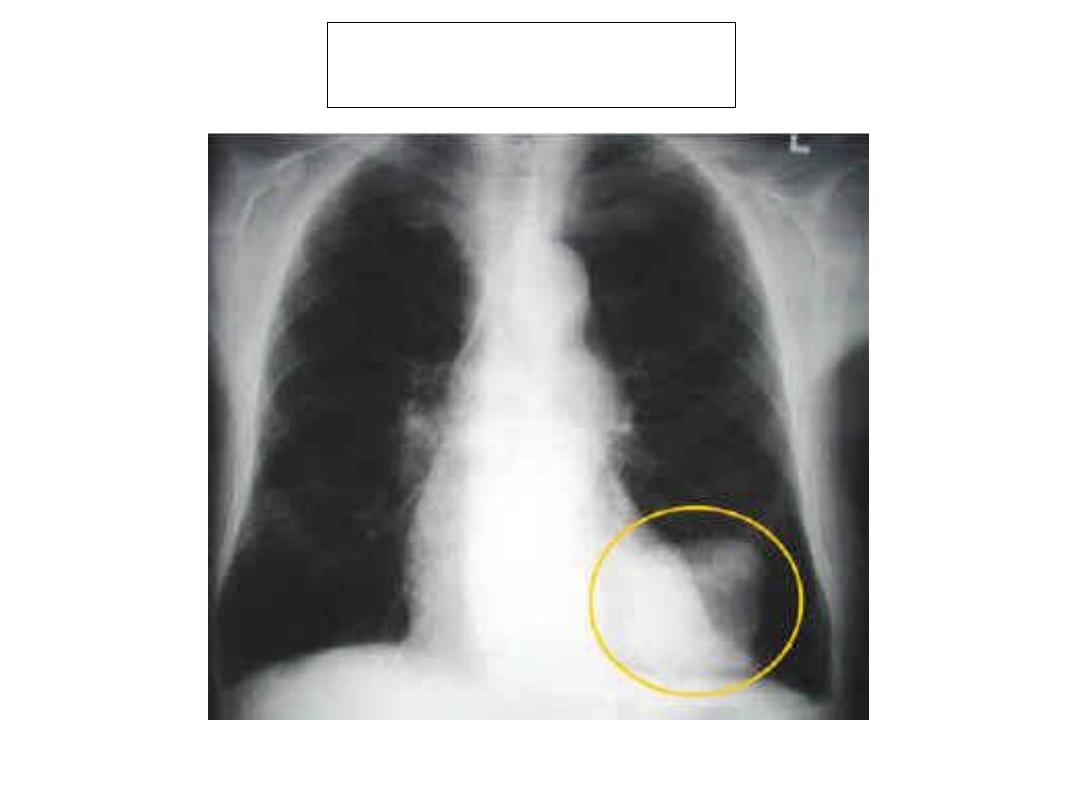
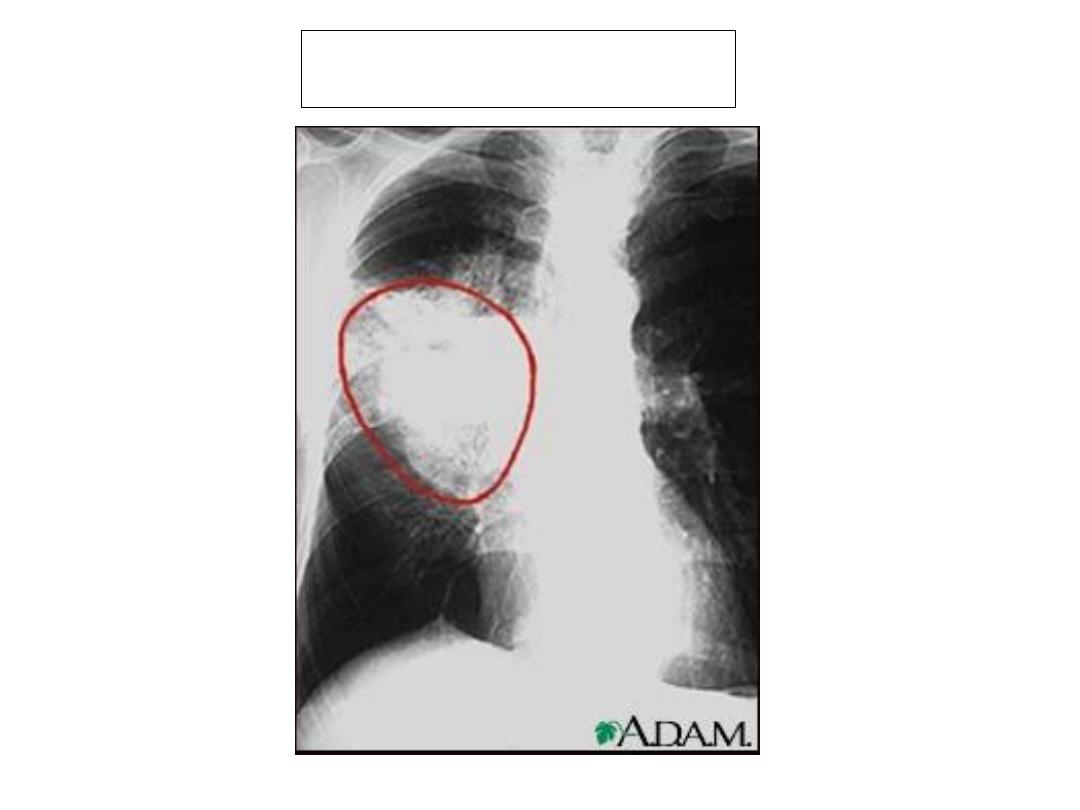
1.Describe your findings ? 2. Mention some
causes of this abnormality? 3. What other
investigations might one consider?
1.
Description:
• Opacification of the left hemi-thorax
• A meniscus is seen at the lateral chest wall
• Radiological findings suggestive of a pleural effusion
• Normal contra-lateral hemi-thorax/remainder of film
normal
• What could cause this abnormality?
2.
Causes of pleural effusion:
• Post-pneumonic
• TB
• Primary or secondary lung tumour
• Mesothelioma
• Pulmonary embolus/infarction
• Pancreatitis
• Rheumatoid disease
The following are usually associated with
bilateral pleural effusions.
• Congestive cardiac failure
• Renal Failure
• Liver Failure
• Hypoalbuminaemia
3.
Specific investigations
Pleural aspiration (always preceded by chest X-
ray) and pleural biopsy (if aspirate is exuadate)

What is the X-ray diagnosis?

This chest radiograph demonstrates free air
under the diaphragm, indicating bowel
perforation (stomach, duodenum, small
bowel, appendix and large bowel).
Usually the patient presents with acute
abdomen.

This patient presented with severe
abdominal pain and distension

• Multiple fluid levels occupying central part
of abdomen indicating small bowel
obstruction.
• Some causes:
1. postoperative adhesions.
2. malignancy.
3.
Crohn’s disease.
4.Complication of Hernias.
5. Intussusception.

This is a plain abdominal X-ray of a 70-year-old
man presented with lower abdominal pain,
abdominal distension and absolute
constipation

• The shadow is peripheral indicating Large
bowel obstruction.
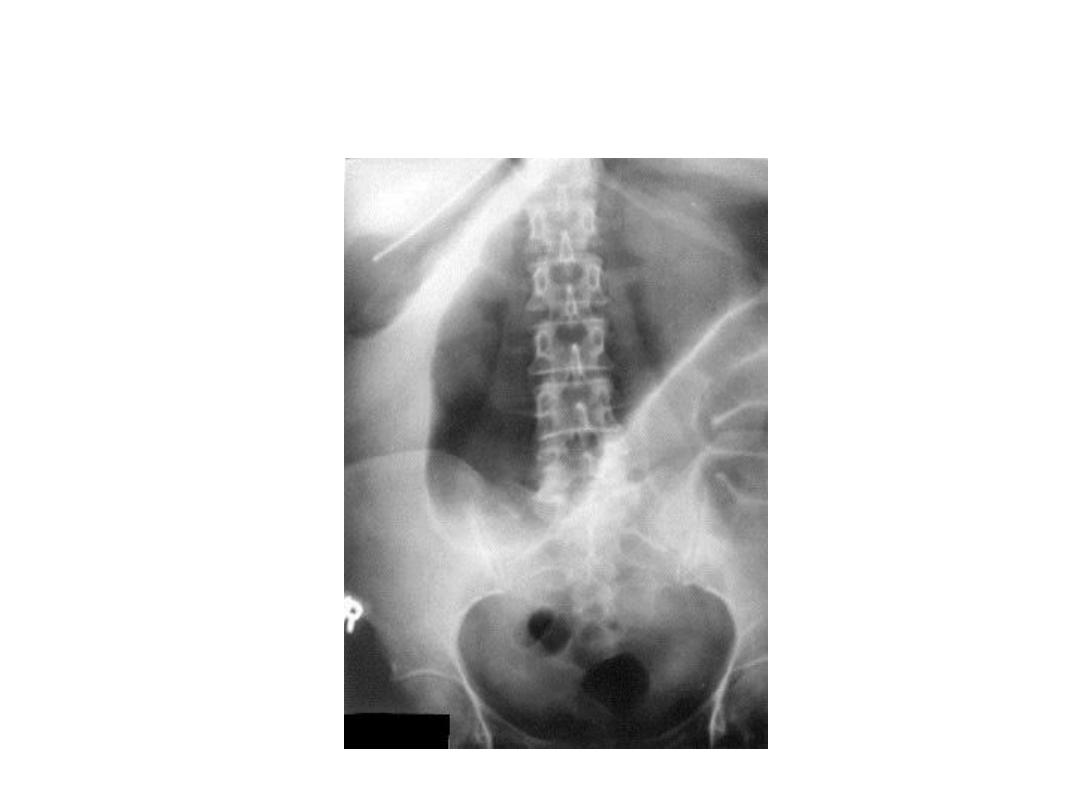
The diagnosis in next slide

Volvulus
Sigmoid or cecal volvulus may have a kidney-
bean appearance on the abdominal films.

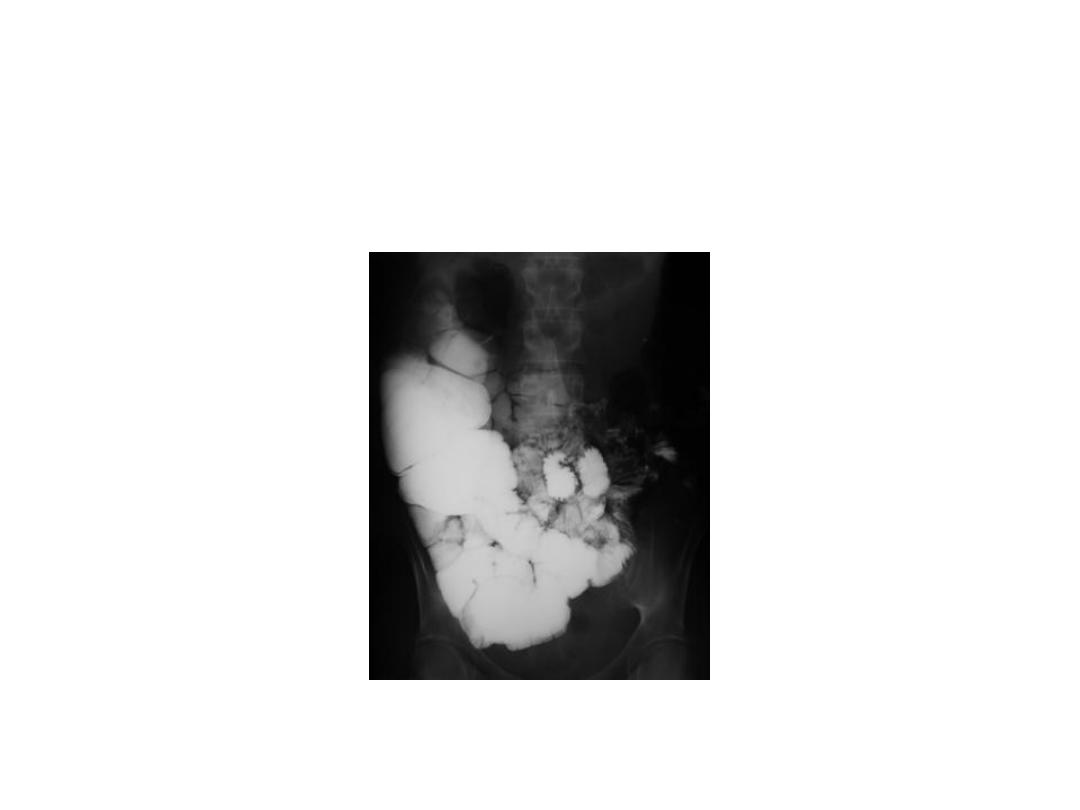
This is barium follow through of a patient with
chronic diarrhea. What is/are finding. What is
diagnosis?
small-bowel series reveals barium flocculation, contrast-
agent dilution, and distal small-bowel dilatation.
Diagnosis: malabsorption syndrome like Celiac disease.

A 55-year-old chronic smoker, male patient presented with
history of frequent epigastric pain and acidity in last 3 months.
The pain occur specifically during fasting and at late night.
What is the diagnosis and best first line investigation?
The most likely diagnosis is duodenal
ulcer and upper GIT endoscopy is the
best first line investigation of choice
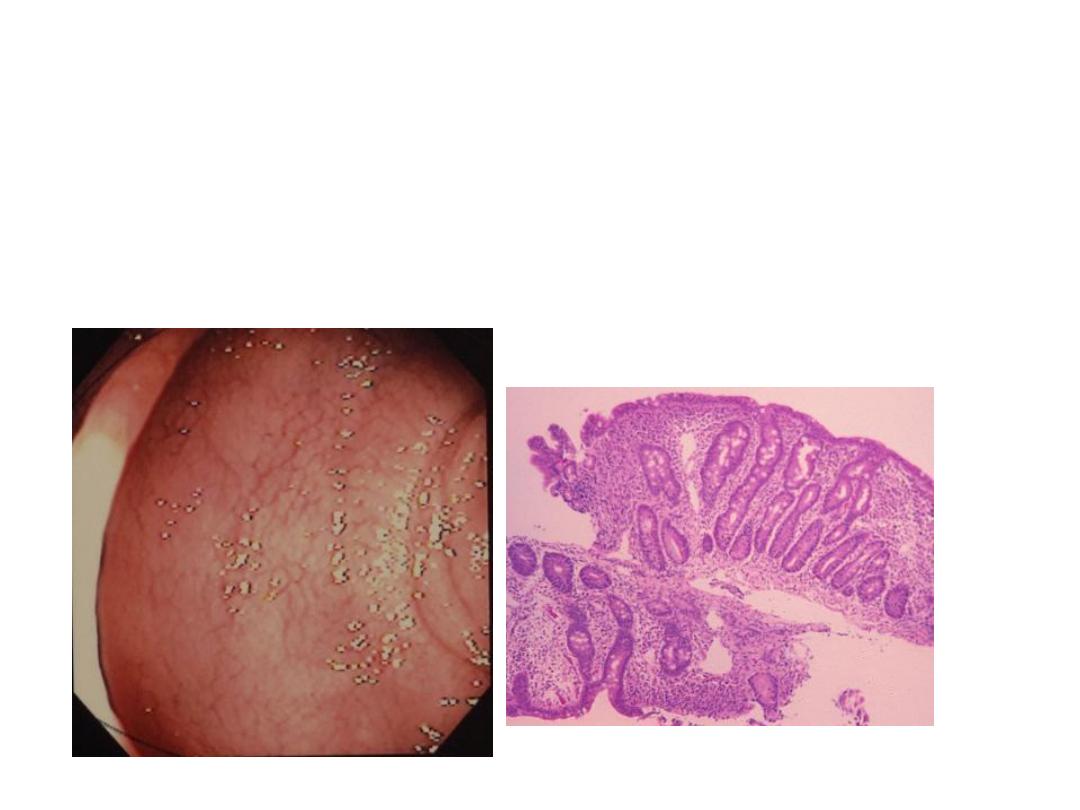
This is a colonoscopy of a patient
with chronic bloody diarrhea.
What is the likely diagnosis?

Diagnosis: Ulcerative colitis.
Complications of IBD (UC and CD):
1. Toxic megacolon.
2. Perforation.
3. Bleeding.
4. Colonic cancer.
5. Stricture, fistula, perianal abscess,
nutritional complications mainly in
Crohn’s
disease.
6. Extraintestinal complications (joint, eye,
hepatobiliary, skin, etc.)
MRI Machine
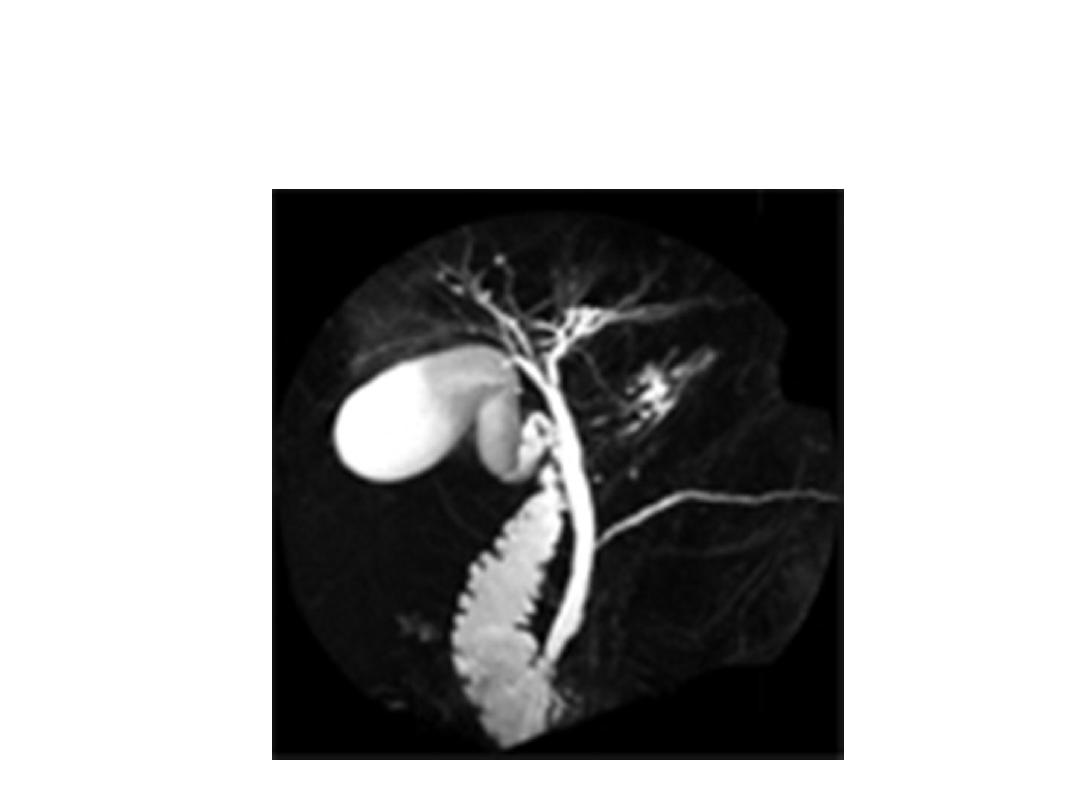
MRCP view
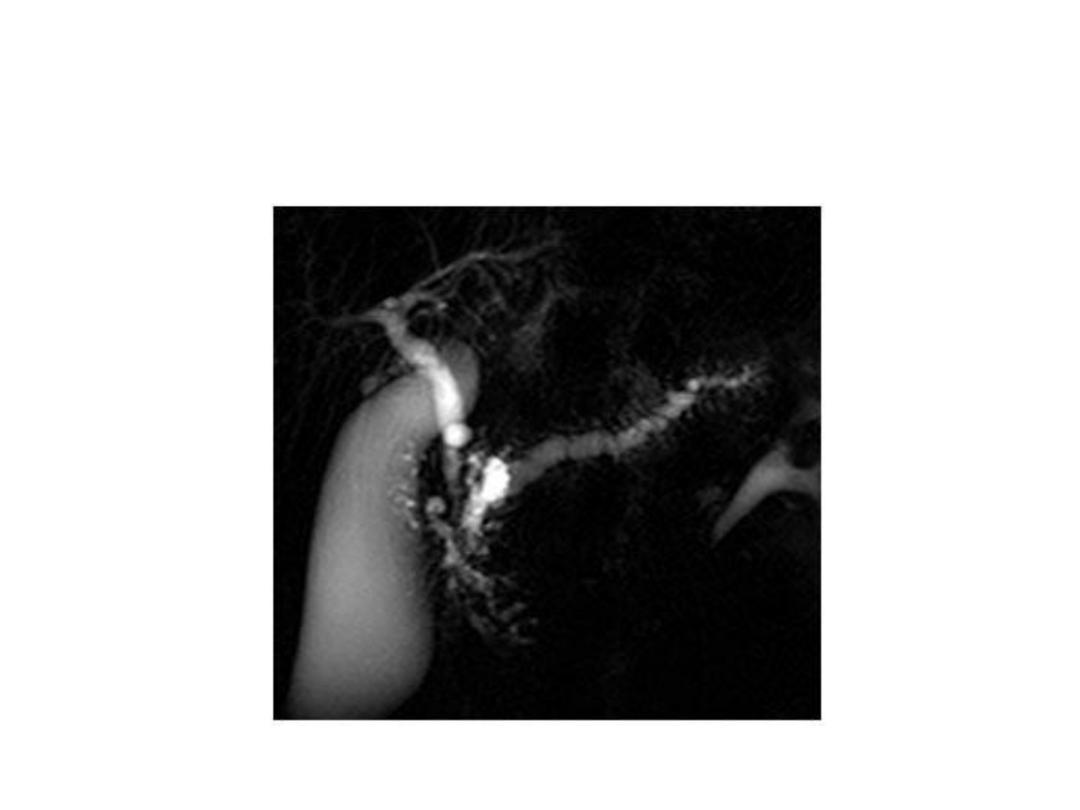
MRCP
– Main pancreatic duct
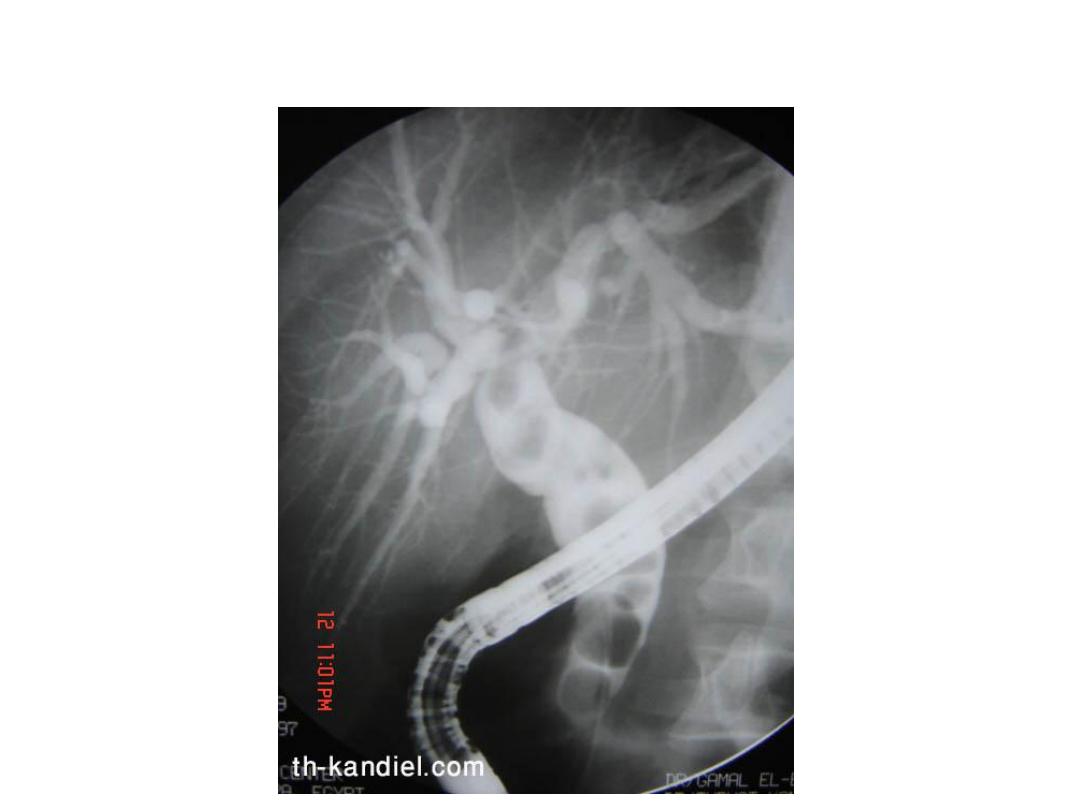
ERCP - 3 stones in CBD

The main two 2 differences between
MRCP and ERCP are:
1. MRCP is non invasive while ERCP is
invasive and may be associated with
complications (acute pancreatitis,
bleeding, perforation, etc.).
2. ERCP is used for diagnostic and
therapeutic purposes while MRCP is
used for diagnosis.
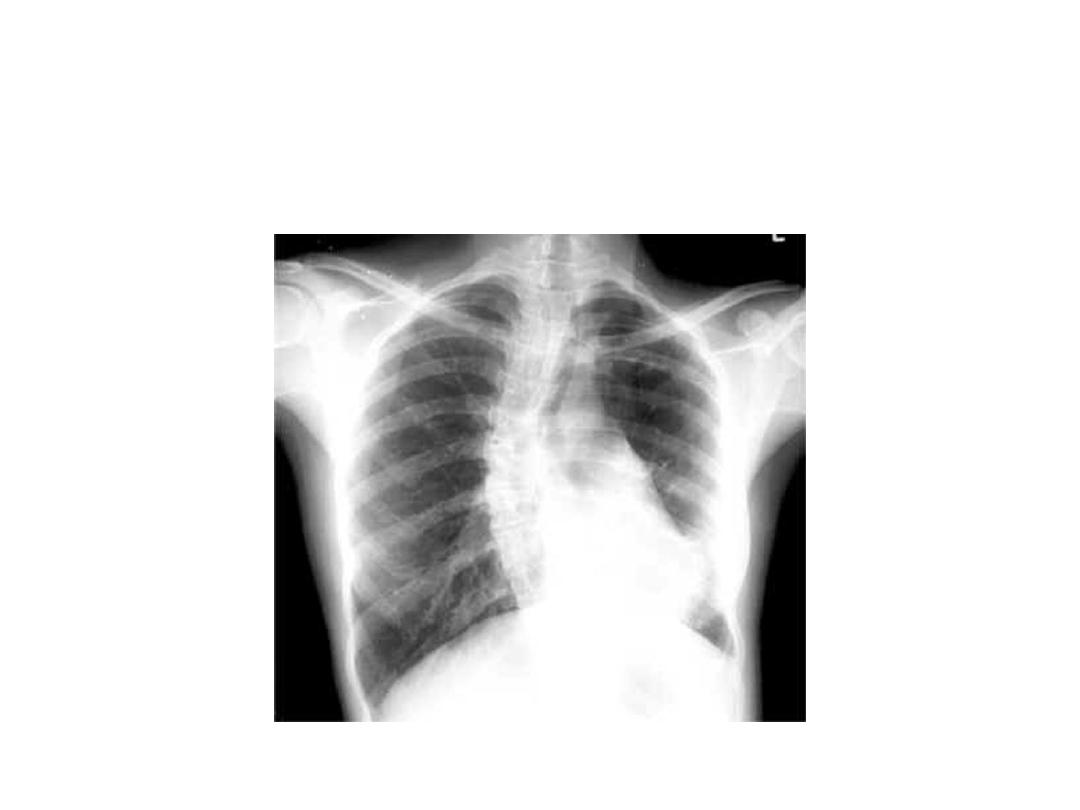
Describe the pathology
Give possible diagnosis

Bilateral Hillar lymphadenopathy
1. Sarcoidosis.
2.
Hodgkin’s Lymphoma.
Because primary TB causes unilateral
lymphadenopathy so it is not included in
D.D

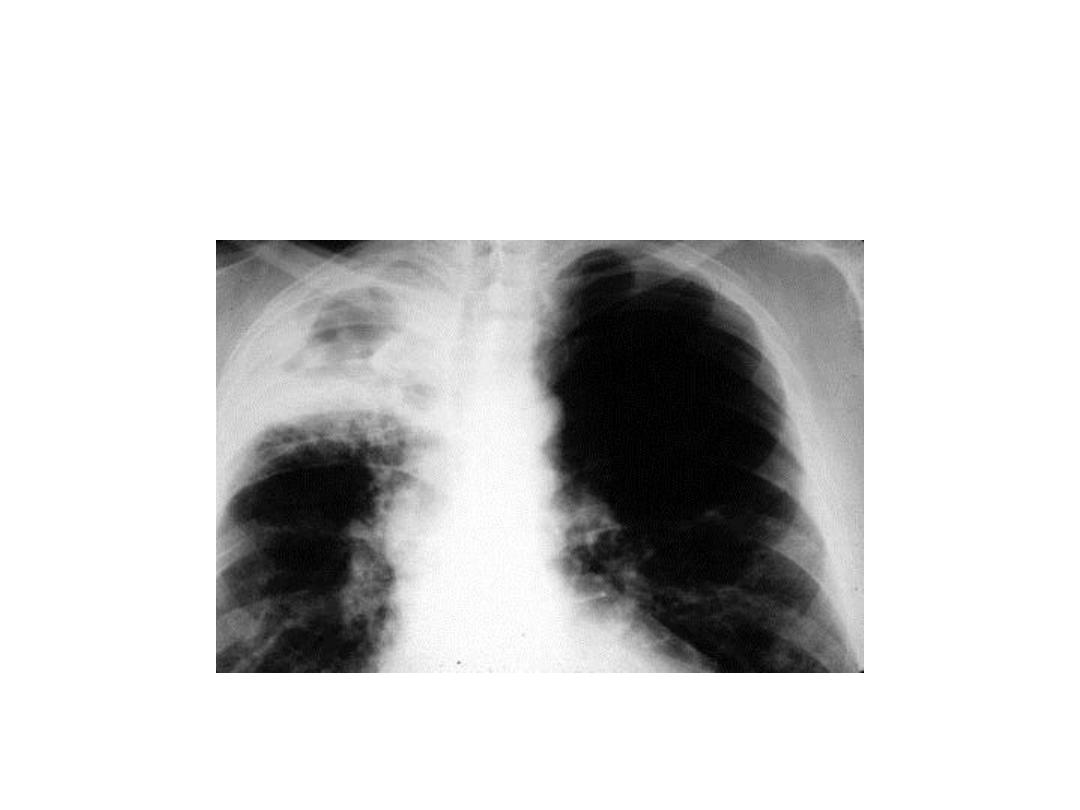
Describe
and give
diagnosis
.

• Advanced bilateral pulmonary TB with
cavities and fibrosis
A 30-year-old
male patient
presented
with fuel
smelling
productive
cough of
yellow-
greenish in
color
What is the
lesion

• Apical TB cavity or abscess

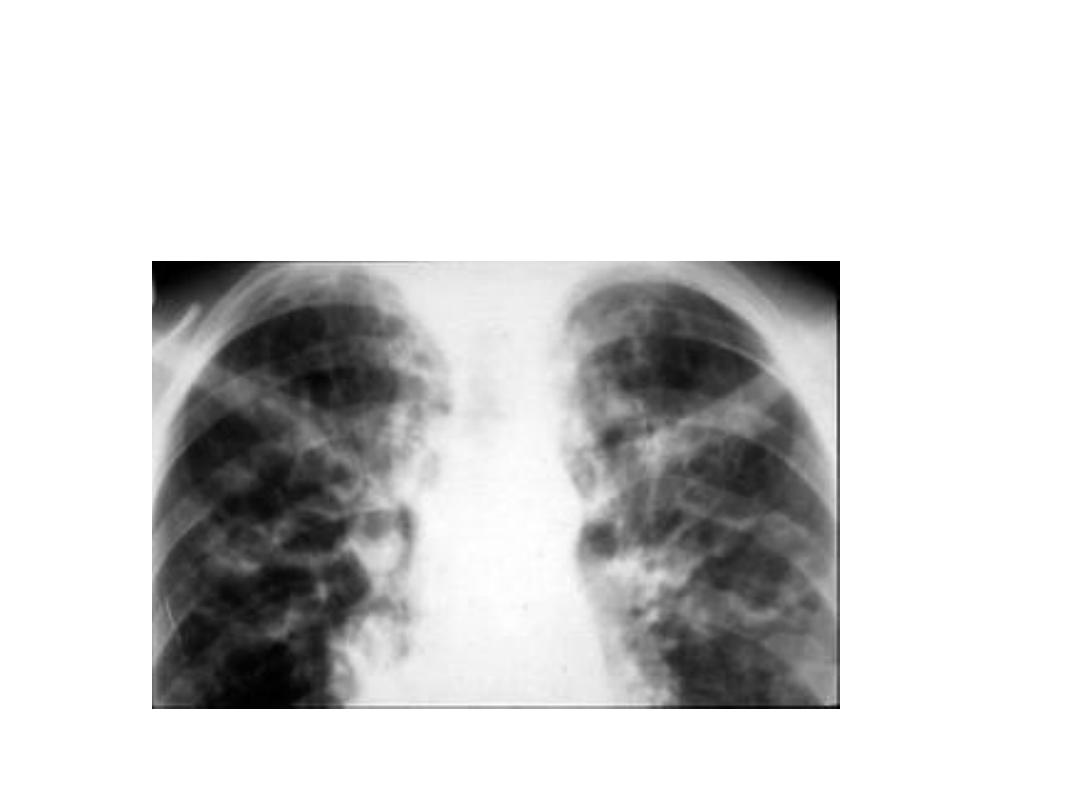
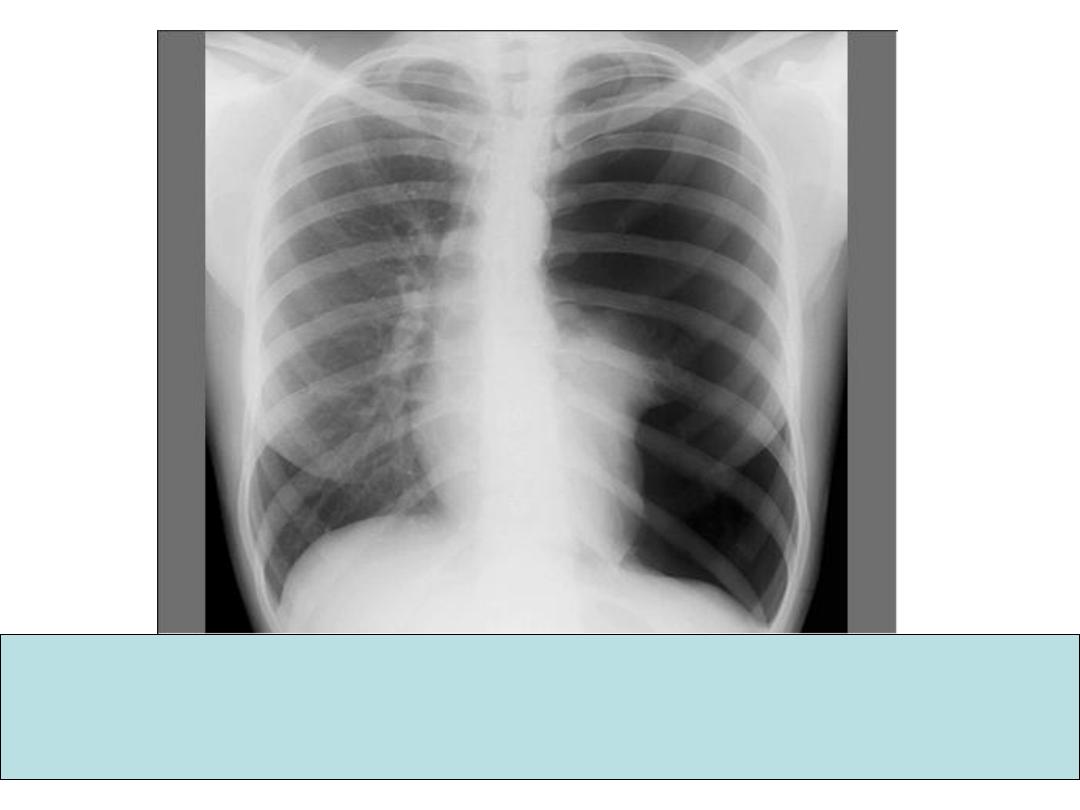
What is the chest condition?
bilateral micronodular interstitial pattern
indicating miliary TB
Usually the patient is immune compromised
like patients with AIDS and those on
immunosuppressant medications. Monteux
test may be negative.

What is diagnosis? Answer in next
slide

Cardiomegaly
Some
causes of huge cardiomegaly
1. Cardiomyopathy.
2. Multiple valve lesions.
3. Pericardial effusion

TB fibrosis with shifting trachea
to the R
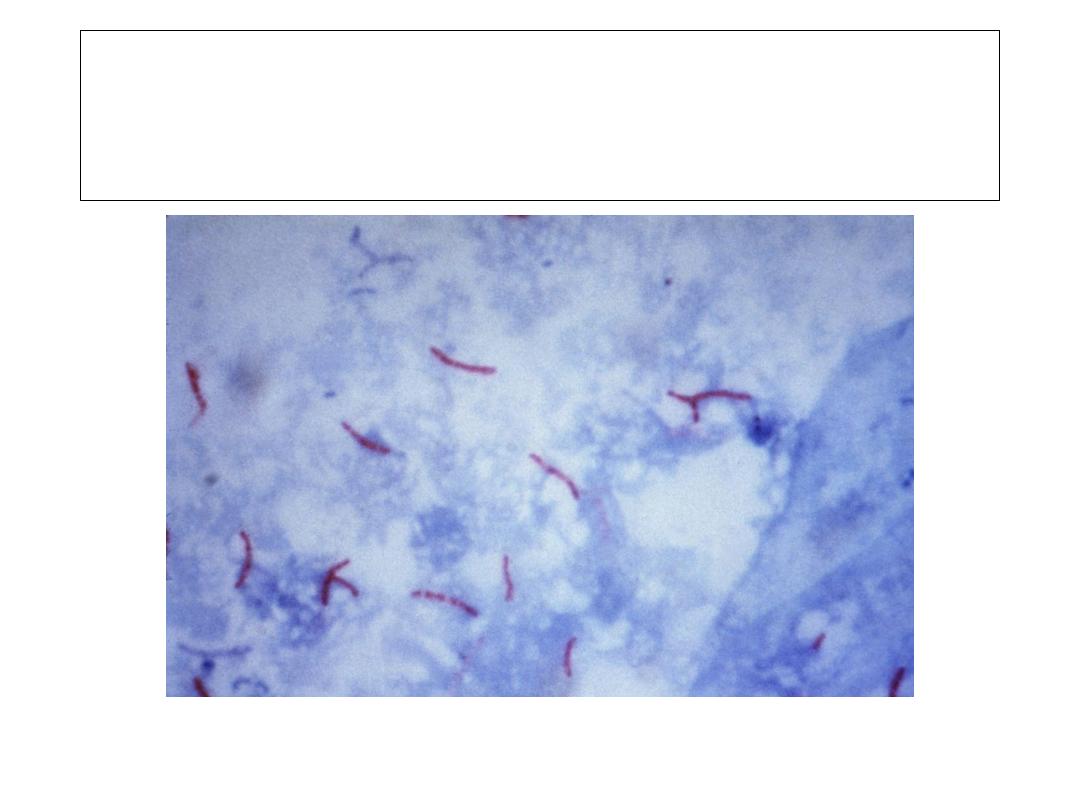
What this slide shows? The answer in
next slide

Sputum smear showing TB bacilli (AFB)
This is an X-ray of 35 year old patient who presented with
long standing cough productive of huge amount of
yellowish - greenish, foul smelling sputum and recent onset
of fever. What is the most likely diagnosis? Mention the
complications.
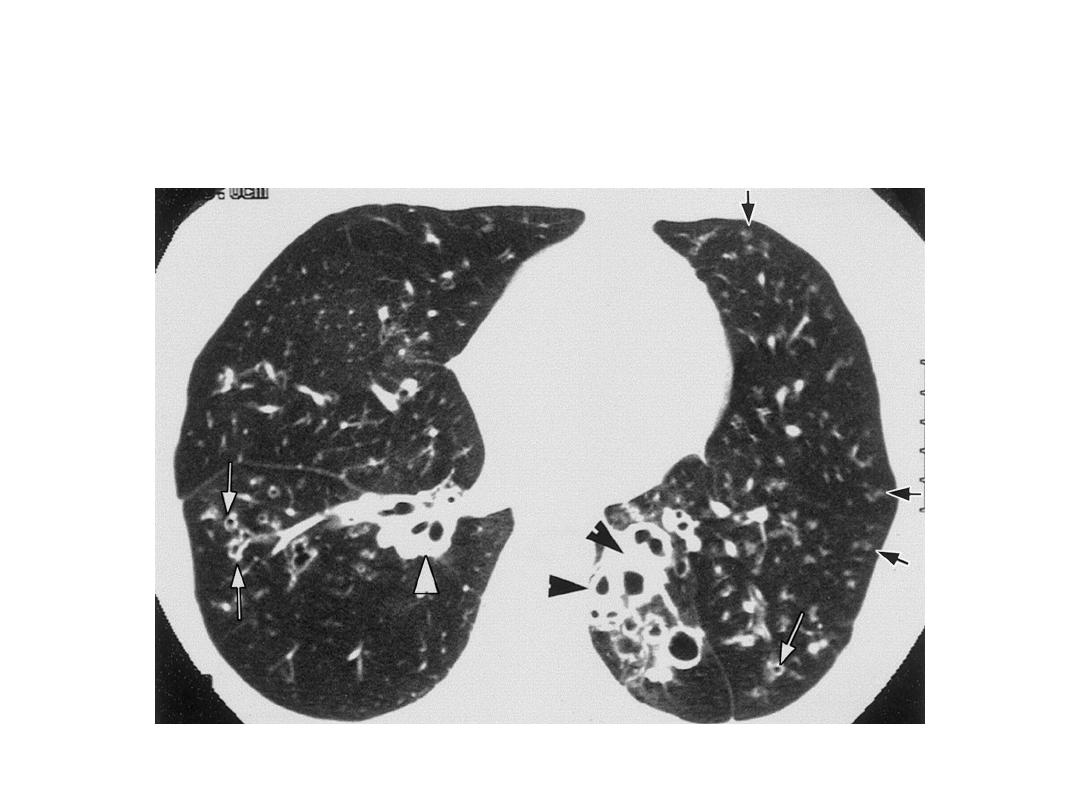
CT chest: Bronchiectasis

• bronchiectasis
• Complication:
1. Massive hemoptysis
2. Recurrent pneumonia(viral, streptococci,
penumococci, klebsiella and anaerobes).
3. Emphysema.
4. Septicemia.
5. Brain abscess.
6. Cor pulmonale.
7. Anemia develops in long standing cases due to
chronic sepsis and recurrent hemoptysis.
8. In untreated cases, secondary amyloidosis may
develop.
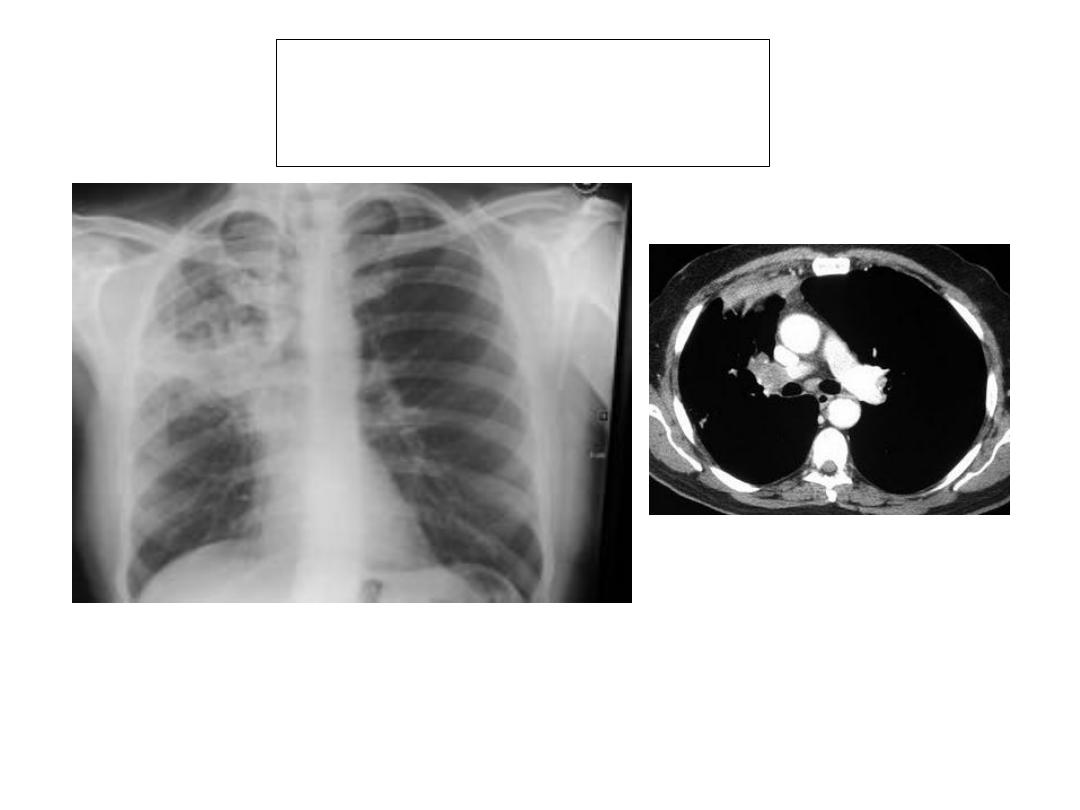
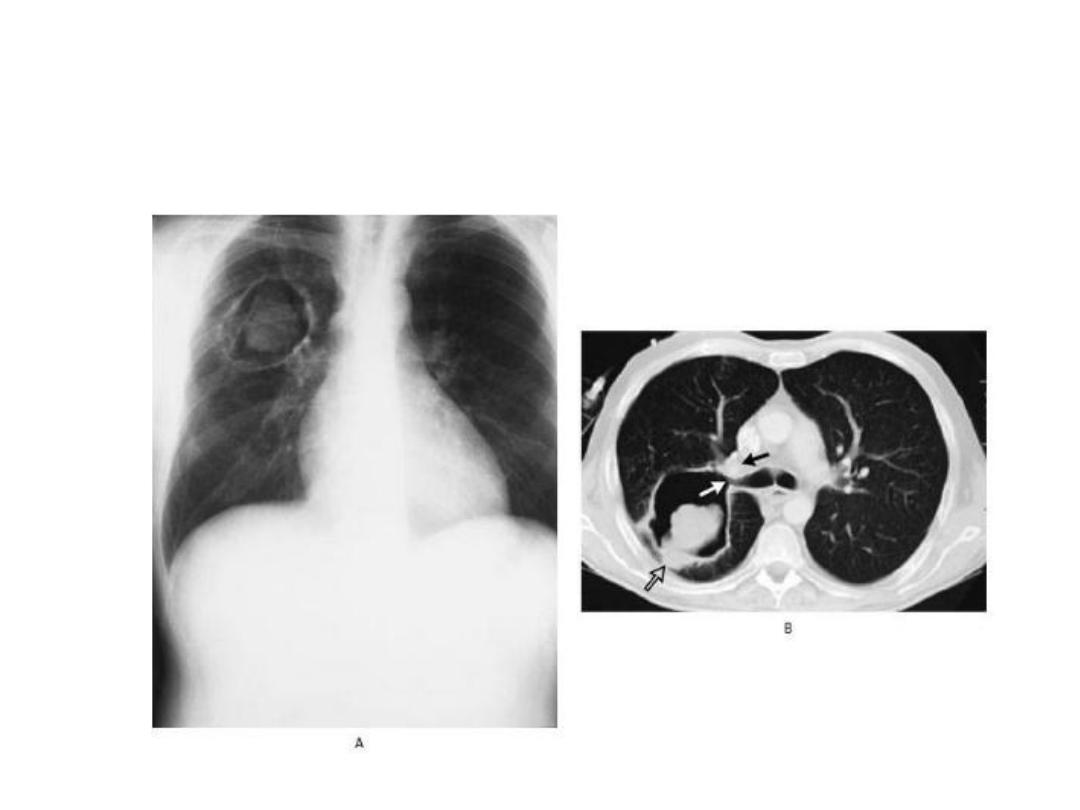
What these CXR and CT are showing?
The answer is in next slide

Bronchogenic carcinoma
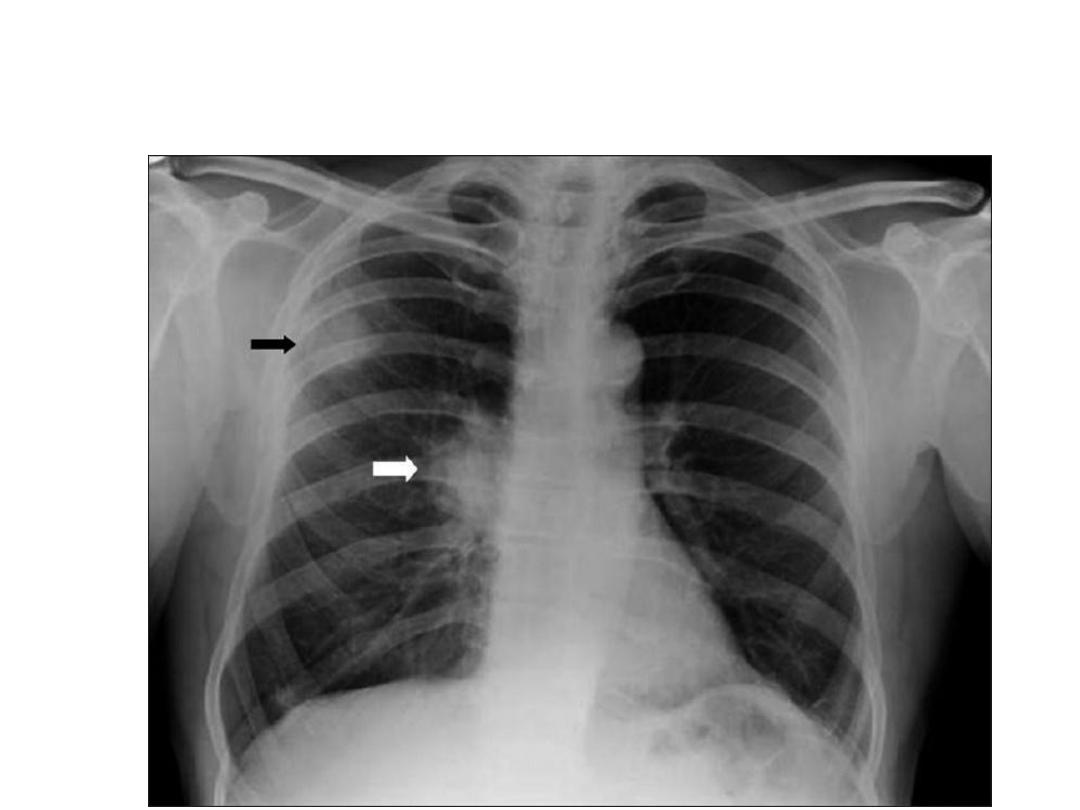
A 70-year-old patient, chronic smoker. Presented with history with dry
cough for last 3 months and several attacks of haemoptysis during last
3 weeks. Diagnosis

Lung cancer. The commonest type is
squamous cell carcinoma (60%). See a
peripheral mass (black arrow) with right
lymphadenopathy (white arrow).
Another lung cancer
Again it is a lung cancer
(bronchogenic carcinoma)
A male patient presented with severe chest pain and dyspnea.
What are the chest X-ray Findings? What is the diagnosis?
How you manage him?

1. Radio lucent left hemi-thorax with lack of
vascular marking and total collapse of
the left lung.
2. Tension pneumothorax.
3. This specific patient needs chest tube
with under water-seal

Malignant abscess with thick wall. Most likely pathology is sq cell carcinoma,
also see if the patient has clubbing. Ask about history of smoking and
hemoptysis, cough and other respiratory symptoms including hoarseness of
voice. After proper chest examination look for evidence of lymphadenopathy
and examine the abdomen for hepatomegaly and ascites. Bronchoscopy with
cytology and biopsy is needed for confirmation of diagnosis of lung cancer. CT
for evidence of distal metastasis is also necessary.
A CAVITY CONTAINING A BALL (MASS)
TYPICAL OF…? See textbook
What is the radiological
diagnosis?
SCOLIOSIS
• What abnormalities
are seen in this
CXR?
Answer
Bilater hilar lymphadenopathy.
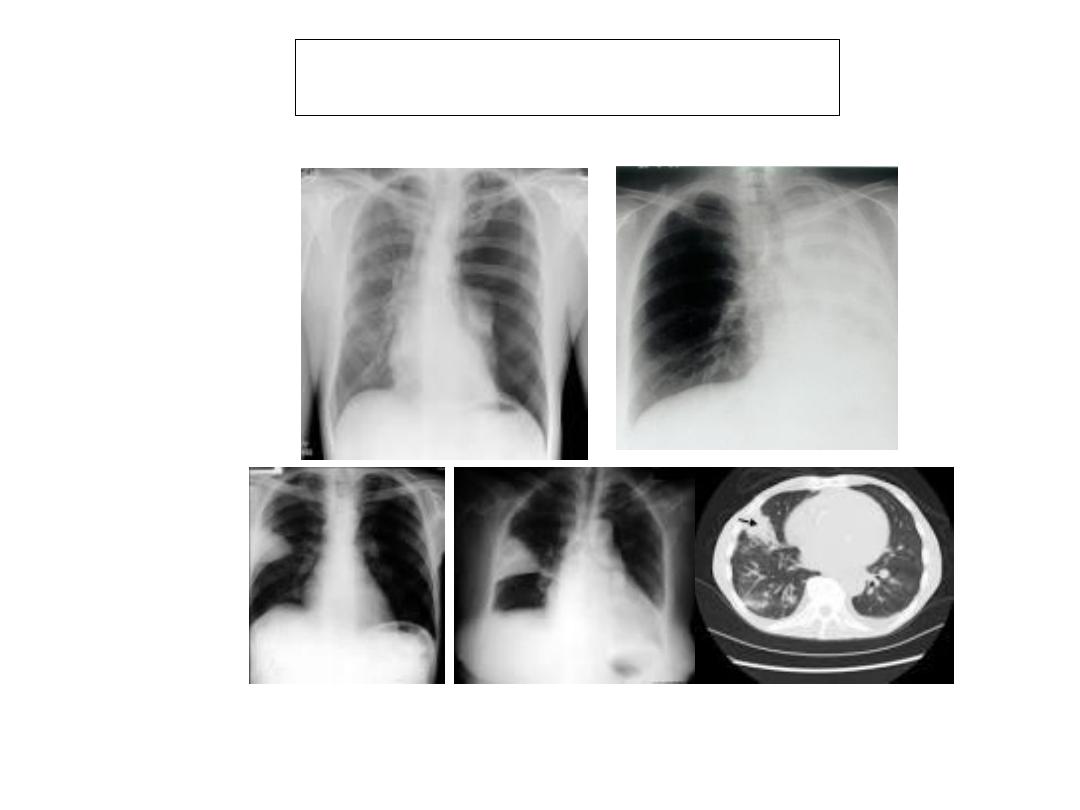
Describe the finding for each CXR. What is
diagnosis for each? Answer in next slide

• Tension pneumothorax
• Complete left lung collapse
• Wedge shaped pulmonary infarction
• CT pulmonary infarction.
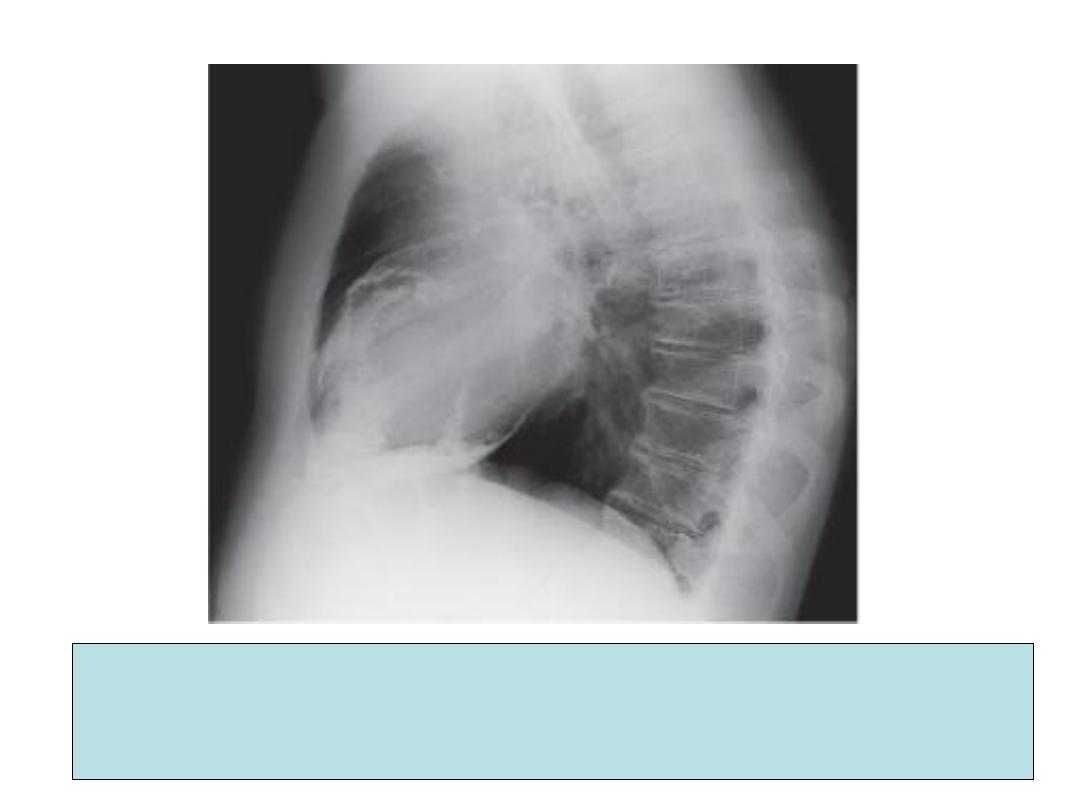
1. What is/are finding in this lateral CXR?
2. Enumerate other Physical signs of this condition?
3. Name one important cause of this condition in our country?
1. Pericardial calcification.
2.
• Rapid, low-volume pulse.
• Kussmaul's sign (a paradoxical rise in the
JVP during inspiration.
• Hepatomegaly
• Ascites
• Peripheral oedema
• Pulsus paradoxus (an excessive fall in
blood pressure during inspiration), present
in some cases.
3. Tuberculosis.
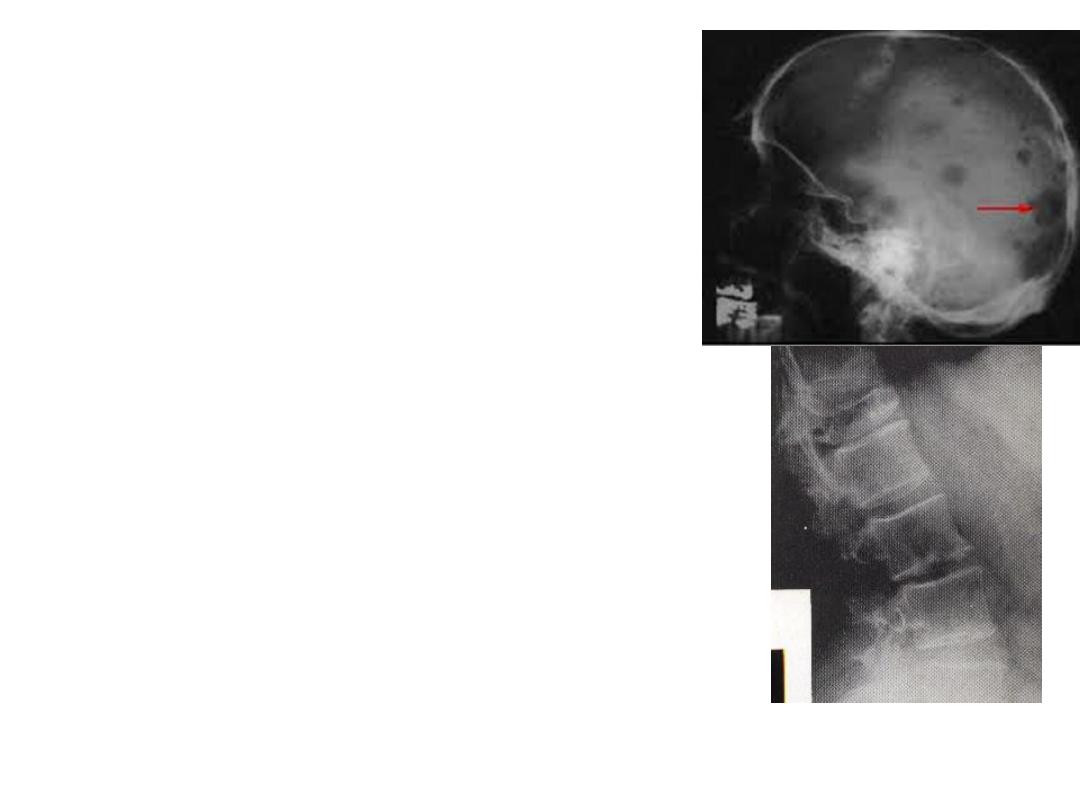
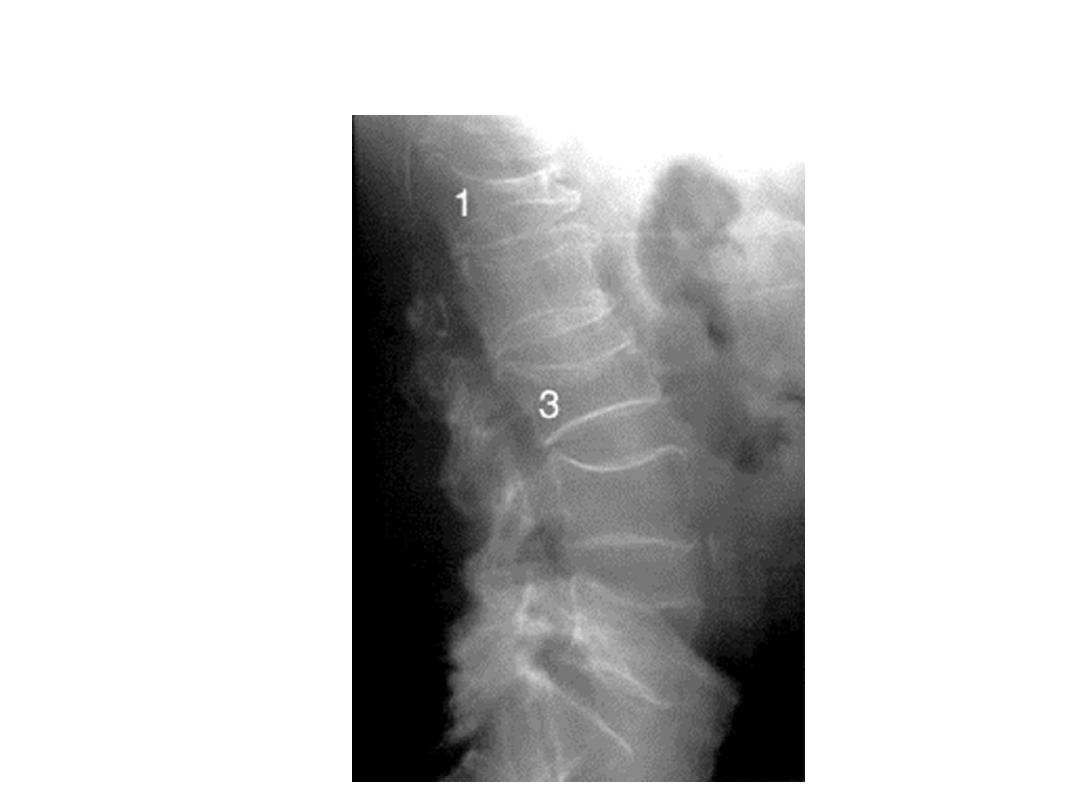
This man presented with
malaise, backache, and
deteriorating visual acuity.
Hemoglobin was 8.8g/l and
the ESR was 118mm in
the first hour.
A. What radiological
abnormalities are shown?
B. What is pathophysiology of
visual disturbace?
C. what simple laboratory
investigations are of great
prognostic value?

A. Slides 85 and 86 are showing multiple
discrete lytic lesions in the skull. Lytic
lesions of the lumber vertebral bodies.
Compression fracture of the body of the
twelfth thoracic vertebral body.
B. Hyperviscosity syndrome due to
polymerisation of the excessive
immunoglobulin and / or
thrombocytopenia and anaemia due to
marrow failure.
C. S. creatinine, S. or blood urea,
hemoglobin and S. albumin.
This is x-ray of 60 year old female presented with
fatigue and episodes of severe back ache.
Diagnosis is compressed fractures
in lumber vertebrae due to
osteoporosis
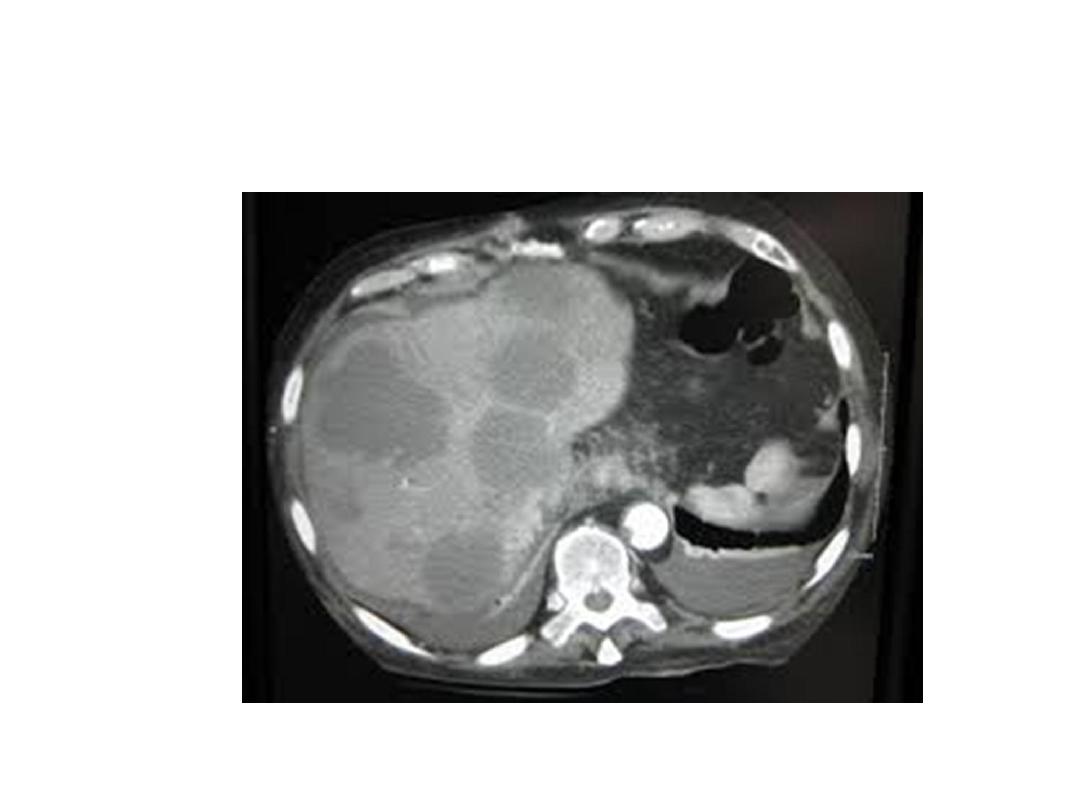
What is the diagnosis? The answer is in
the next slide

Multiple Metastatic deposits in the
liver on CT scan

What is diagnosis?

Describe this hand? What is the
diagnosis? Answer is in next slide.
1. Ulnar deviation of the fingers with wasting of the
small muscles of the hands , swelling and
flexion at the metacarpophalangeal joints. 2.
Typical of Rheumatoid arthritis hand.
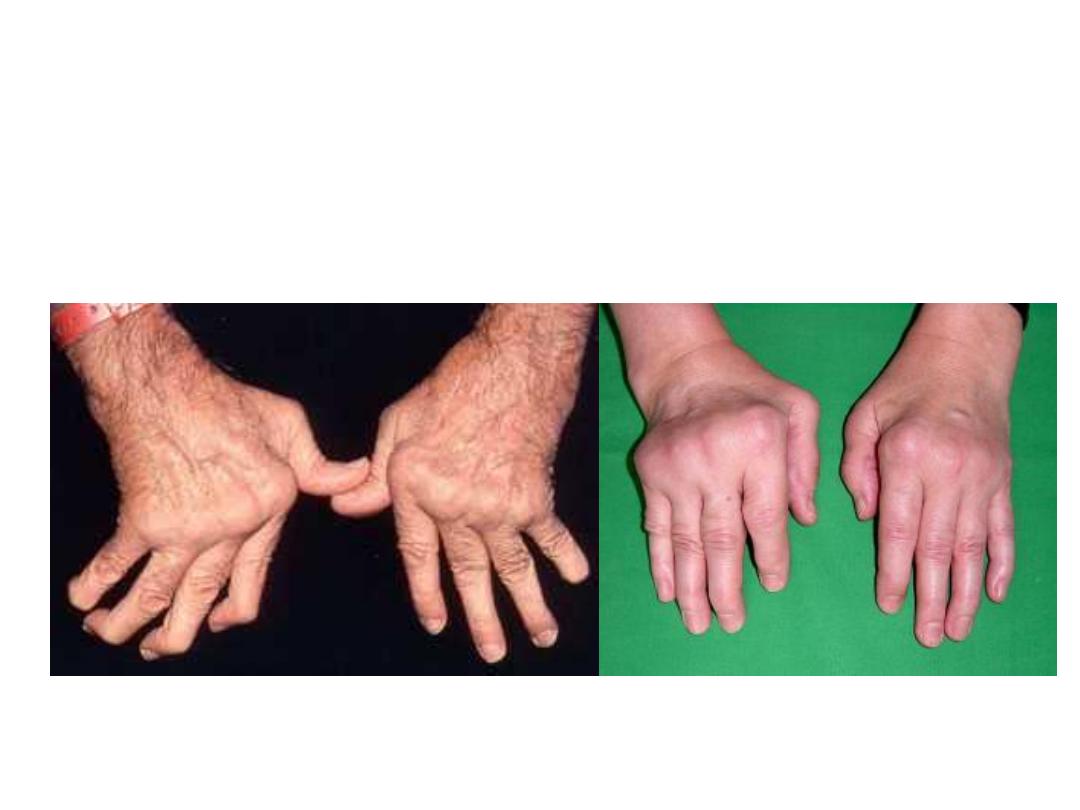
Also these are hands of advanced Rheumatoid
arthritis. Always symmetrical. Look for new criteria
for diagnosis of Rheumatoid arthritis in the
textbook.

Again Rheumatoid hands
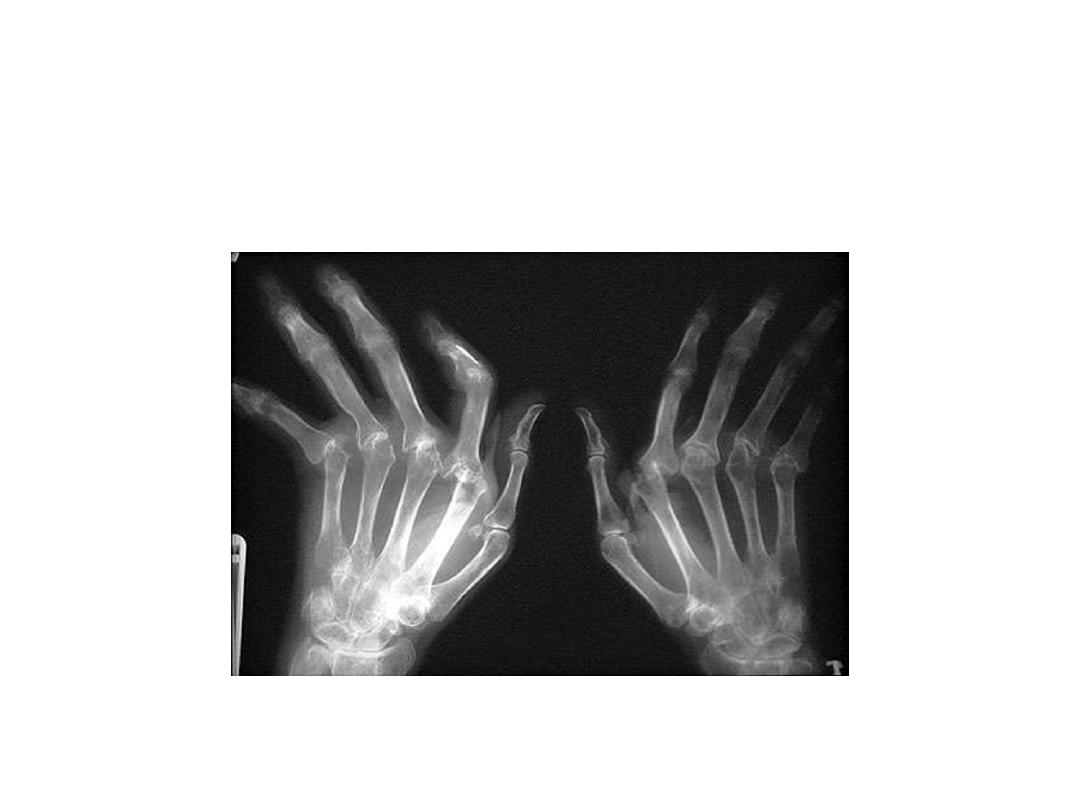
Rheumatoid hands X-ray
(advanced)
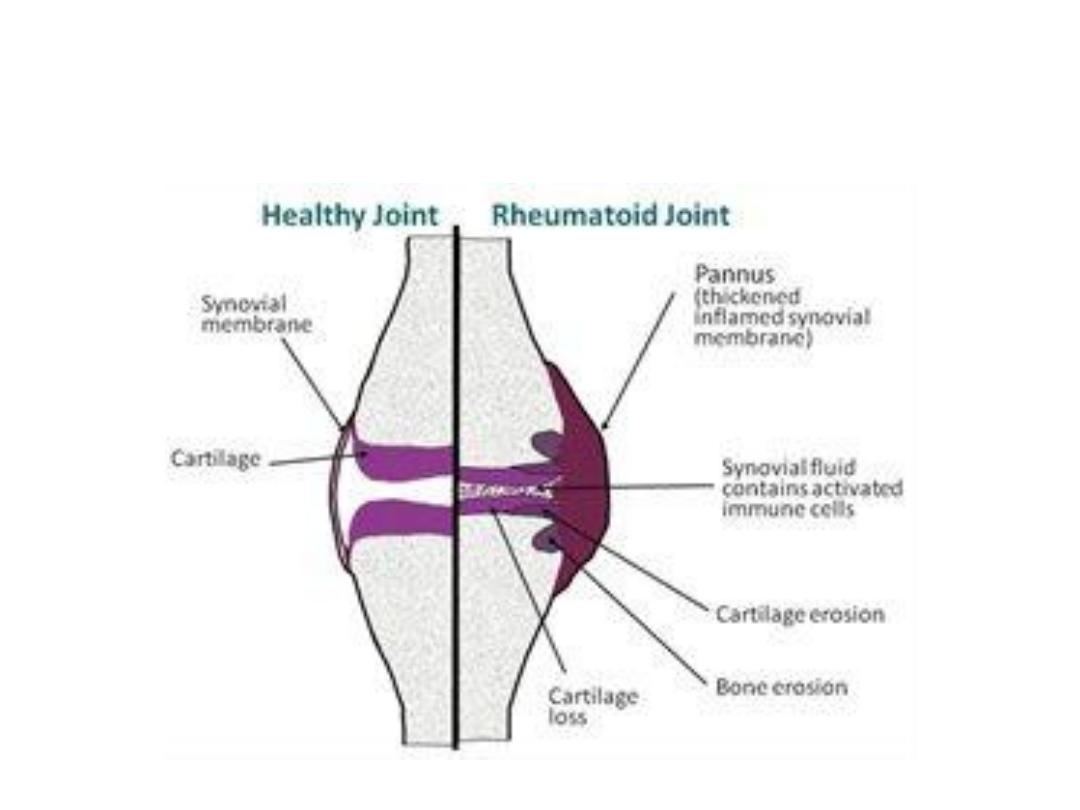
Demonstrating the pathological and radiological
changes in Rheumatoid hands
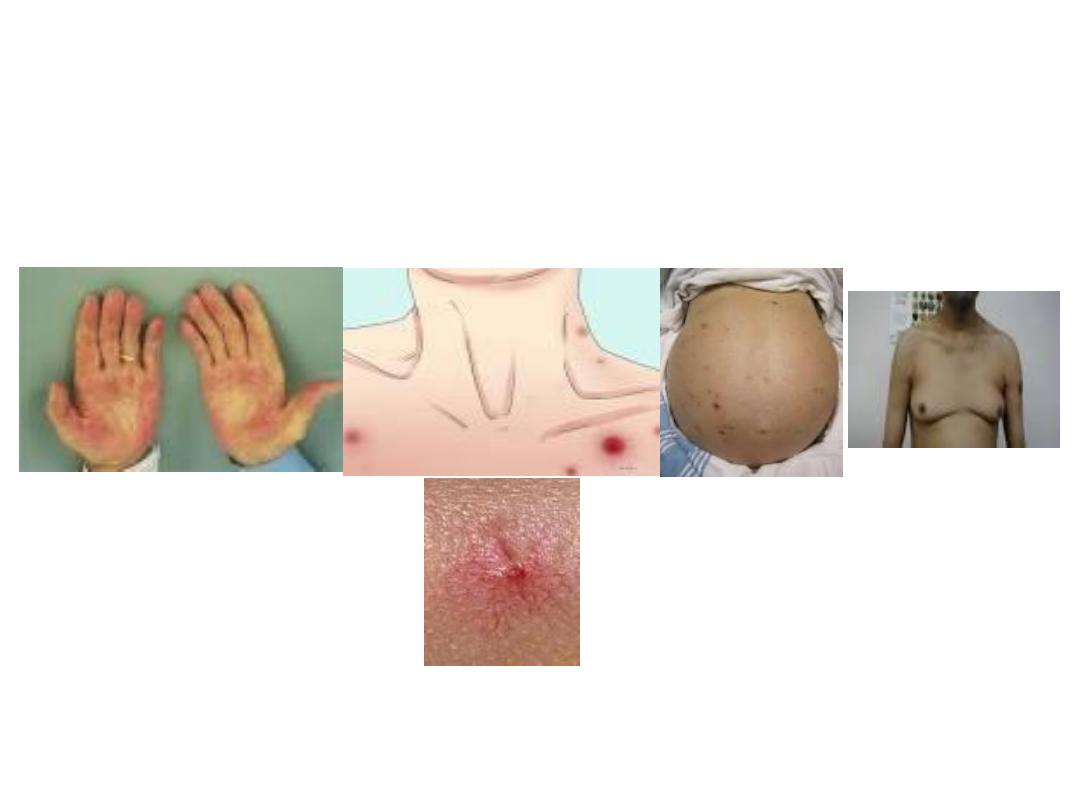
These are finding in a 50-year-old, chronic alcoholic man.
What abnormalities are demonstrating in these pictures?
1. palmar erythema.
2. Spider telangiectasia.
3. Ascites.
4. Gynaecomastia.
Others (not demonstrated here):
parotid gland enlargement,, Duptyrian
contracture, finger clubbing and cyanosis.
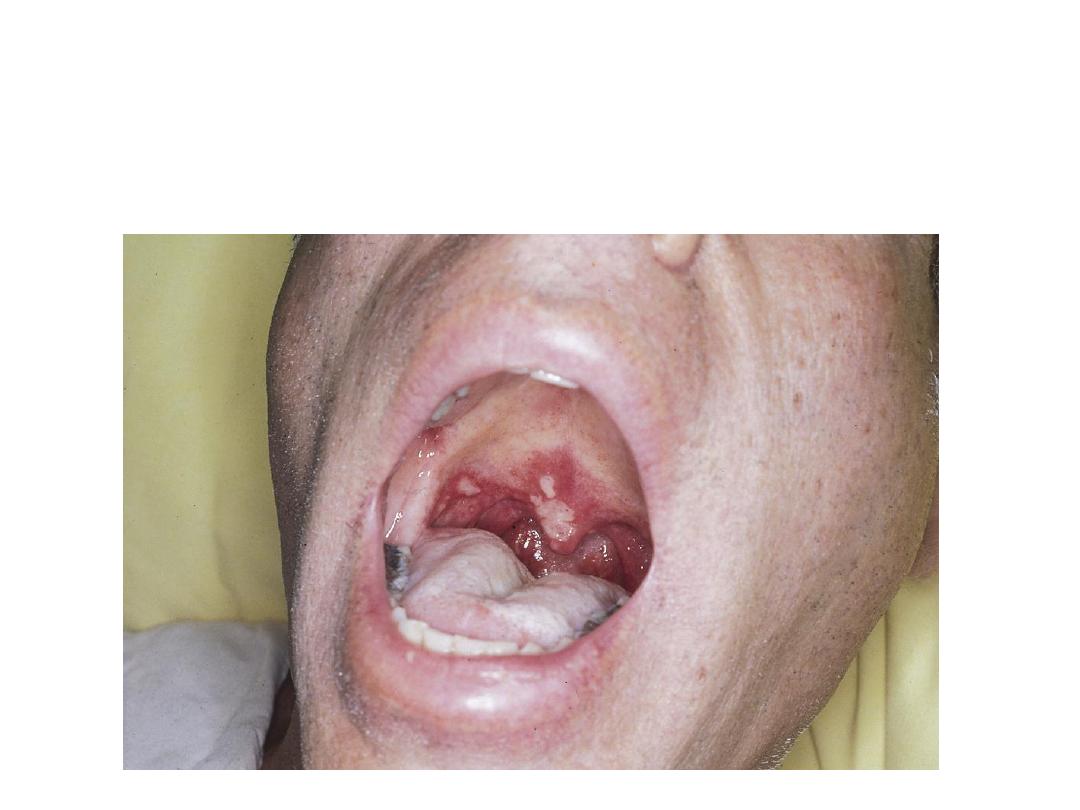
This patient is complaining of multiple
painful mouth ulcers. What name is given to
such ulcers? Mention some systemic causes
for this condition.
1. Aphthous ulcers
2. Some systemic causes:
Bahcet’s syndrome.
SLE
Crohn’s disease and UC
Coeliac disease
Leukaemia and carcinoma
What features are seen in looking to the
face of this patient? What is the diagnosis?
What are other features to look for?

1.
Enlargement of lower jaw (prognathism), lips , nose and prominent
supraorbital ridges.
2.
Acromegaly.
3.
Large hands and feet, enlargement of thyroid, liver and heart.
4.
Confirmatory test: During glucose tolerance test measurement of IGF
1 and GH is done and if the level is above the referred range the
diagnosis of excessive GH is confirmed. Also measurement of
Prolactin Hormone is indicated. Imaging of pituitary gland using MRI
is indicated also. Trans-sphenoidal surgery may perform in addition
to medical treatment like octreotide.

Different diabetes patients presented with these foot
lesions What each lesion is called? How you manage?
1. Diabetic foot: One of the bad chronic
sequel of DM. may occur spontaneously or
triggered by an injury that may be trivial.
Neuropathy, vascular causes as well as
bacterial infection have their roles in this
condition. It may lead to more serious
conditions like gangrene and septicaemia.
Foot deformity with bone destruction also
may occur.
2. Management; See text.
What feature was demonstrated in this
patient? What is the lesion?
1. Deviation of the tongue to the left side.
2. Left sided hypoglossal (12
th
cranial nerve)
palsy.
What is the neurological diagnosis?
1. Deviation of the uvula toward right side.
2. Lt sided paralysis of vagus nerve (10
th
cranial nerve).
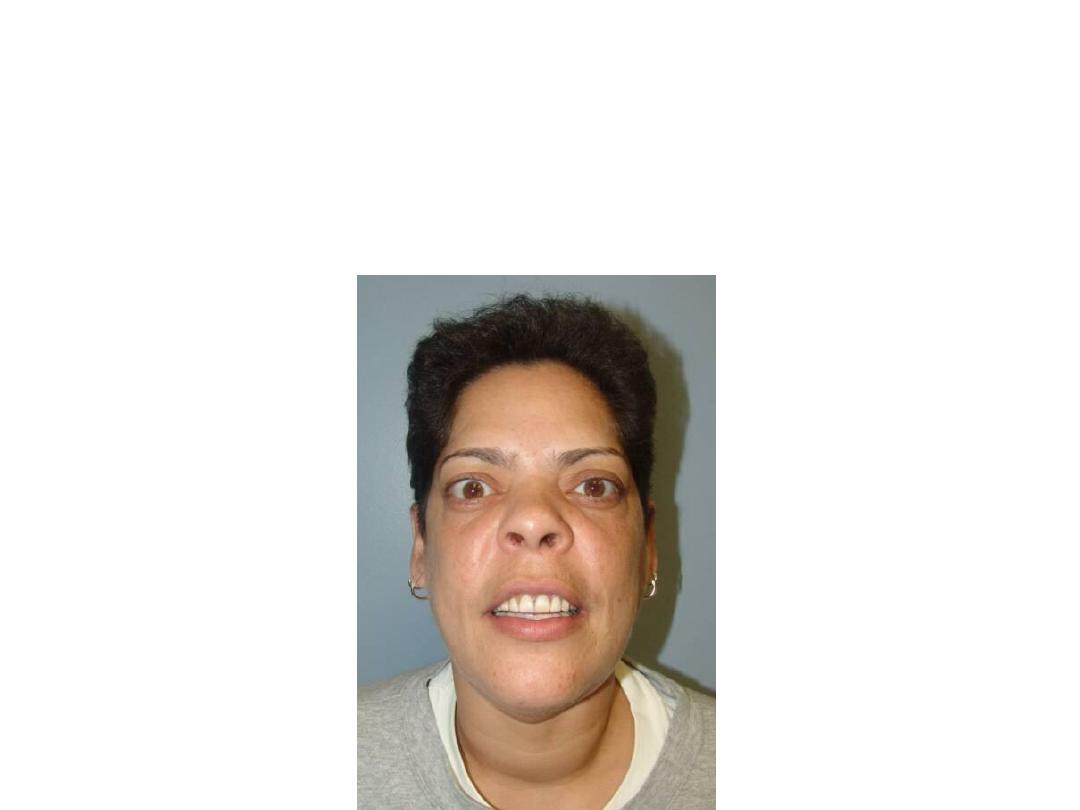
SPOT DIAGNOSIS
Left side facial palsy )Bell’s palsy) this of
lower motor neuron type involving the
whole left side of the face with inability to
close left eye or to contract frontal muscles
and deviation of the mouth angle to
opposite side.
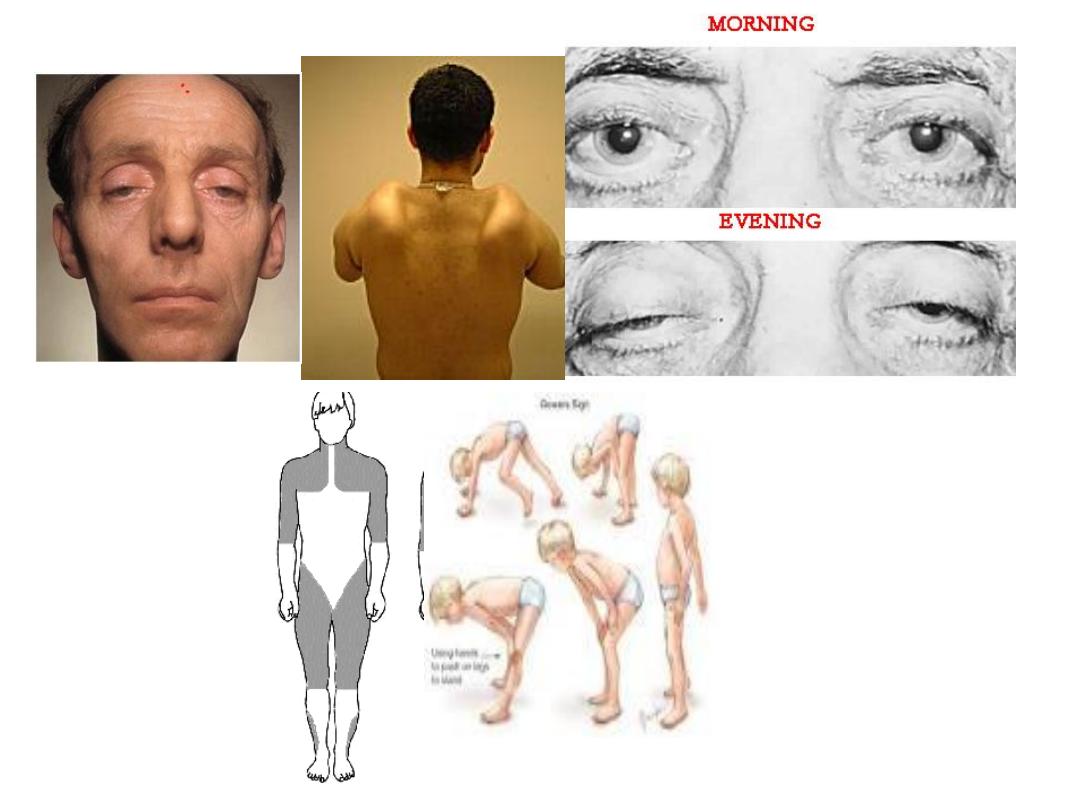

• Myotonic dystrophy: Myotonic dystrophy is characterized by progressive
muscle wasting and weakness. People with this disorder often have
prolonged muscle contractions (myotonia) and are not able to relax
certain muscles after use. For example, a person may have difficulty
releasing their grip on a doorknob or handle. Also, affected people may
have slurred speech or temporary locking of their jaw. It is an autosomal
dominant, other features are: frontal baldness, bilateral ptosis,
ophthalmoplegia, pupil anomaly and infertility.
• Winging of scapula (trapezius muscle weakness), a common first sign of
facioscapulohumeral dystrophy(FSHD), usually in adult, asymmetrical
and asymptomatic but the patient has difficulty reaching above the
shoulder level
• The ptosis of myasthenia can be temporarily improved with an
acetylcholine esterase inhibitor medication such as an injection of
edrophonium (Tensilon) and this can used a diagnostic test.
• Duchenne muscular dystrophy: x-linked, early in life, pseudohypertrophy,
myopathy.
• Diagnosis of MD: creatine kinase (CK), muscle biopsy.

This young lady was treated for chronic
renal failure
after a chronic illness consist mainly of malaise and
joint pain. In looking to her face, what diagnosis comes
in your mind? How do you diagnose this condition?
What are other complications that might be associated
with this condition?
1. SLE (systemic lupus erythematosis)
2. The diagnosis depends on the recognition
of specific symptoms and identification of
auto-antibodies, to fulfill current
classification criteria. 4 of 11 factors
must
be present or have occurred in the past
(see textbook).
3. In addition to renal involvement, other
systems ( respirotory: pleursy,
cardiovascular: pericarditis, CNS:
epilepsy…etc.) may be involved.
This patient is complaining of multiple joint pain and stiffness with red-bluish discoloration
of finger tips on cold exposure . What is the most likely diagnosis? What caused finger tips
discoloration? Mention GIT problems that may be associated with this condition.
1. Systemic sclerosis (Scleroderma).
2
. Rayanaud’s phenomenon.
3. A. Diarrhea and blind loop syndrome
and malabsorption.
B. GERD and Dysphagia
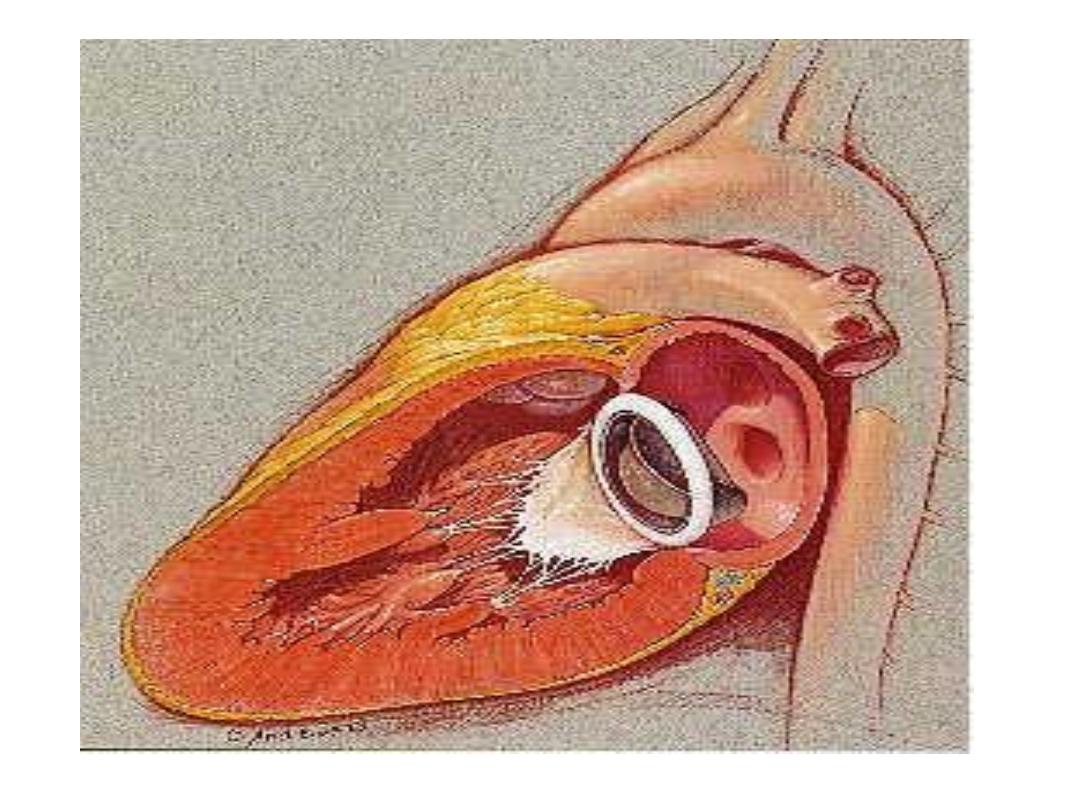
What is the diagnosis?
What are the possible complications?
A. Prosthetic valve
B. Possible complications:
1. Thrombo-embolic phenomenone:
prophylactic anticoagulant may be
needed.
2. Bacterial endocarditis: Give antibiotic
prophylaxis before procedures.
3. Others.
Roth’s spot
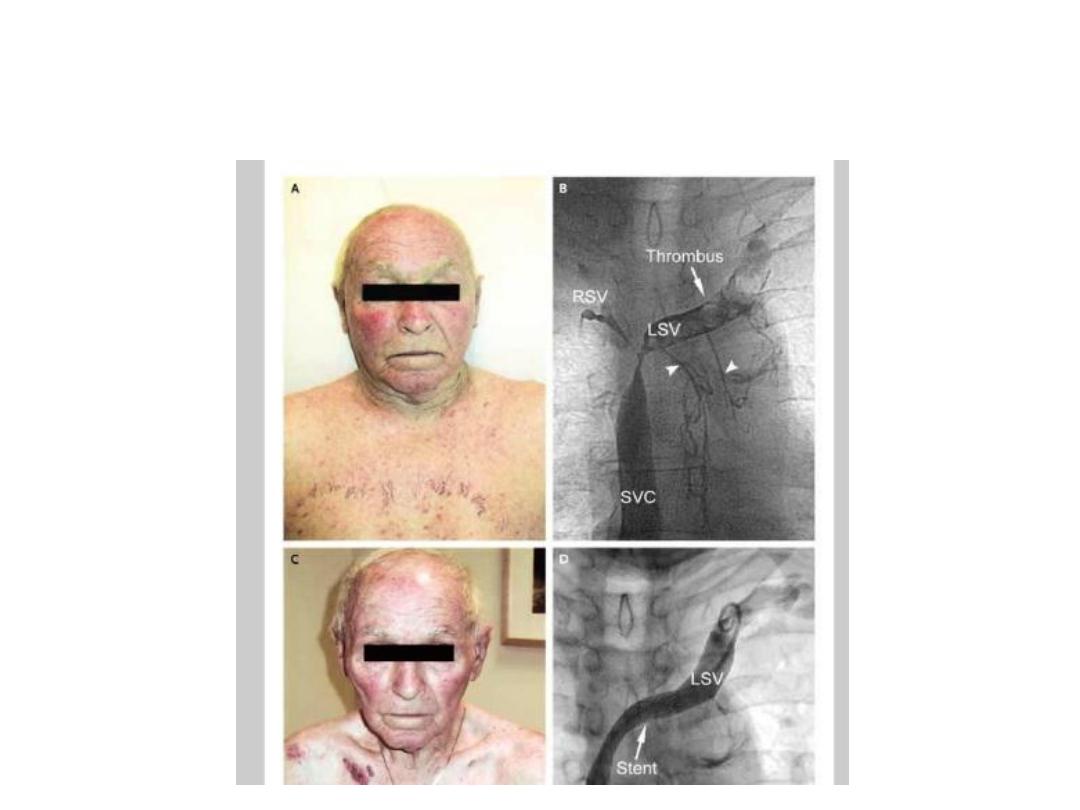
A 75-year-old man with smoking history and stage IV non
–small-cell carcinoma of the
lung presented with progressive symptoms of cough, hoarseness, and swelling of the
face and arms. On examination, he appeared plethoric, with pitting edema of the face
and upper torso. The jugular veins were non pulsatile and distended
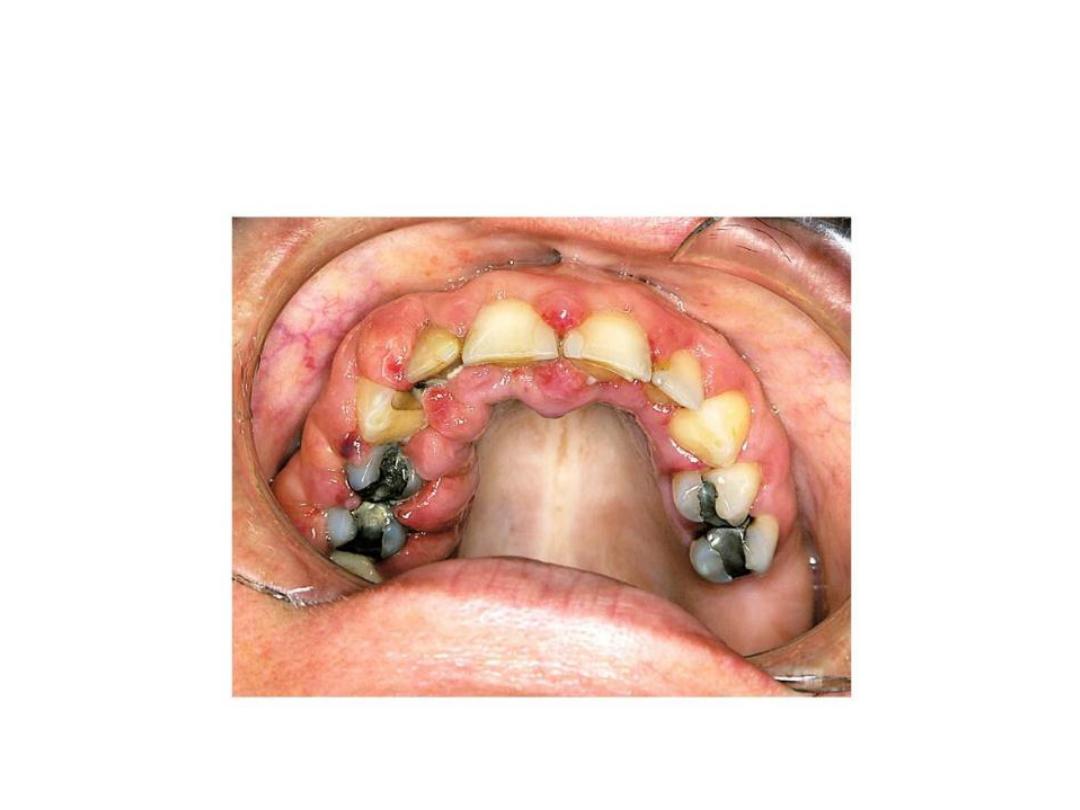
Gingival hypertrophy (causes)

• AML M
4
•
R Epilepsy
This patient is complaining of cough productive of large amount of yellowish
–
geenish Sputum especially at morning for several months. What is the most likely
diagnosis? What is the best way for confirming diagnosis? Mention other condition
that might produce this physical sign.
1. Bronchiectasis.
2. Diagnosis: CXR, CT-scan (the best).
3. Lung abscess, bronchogenic
carcinomas, mesothelioma, fibrosing
alveolitis, cyanotic congenital syndrome,
subacute bacterial endocarditis, liver
cirrhosis and malabsorption.
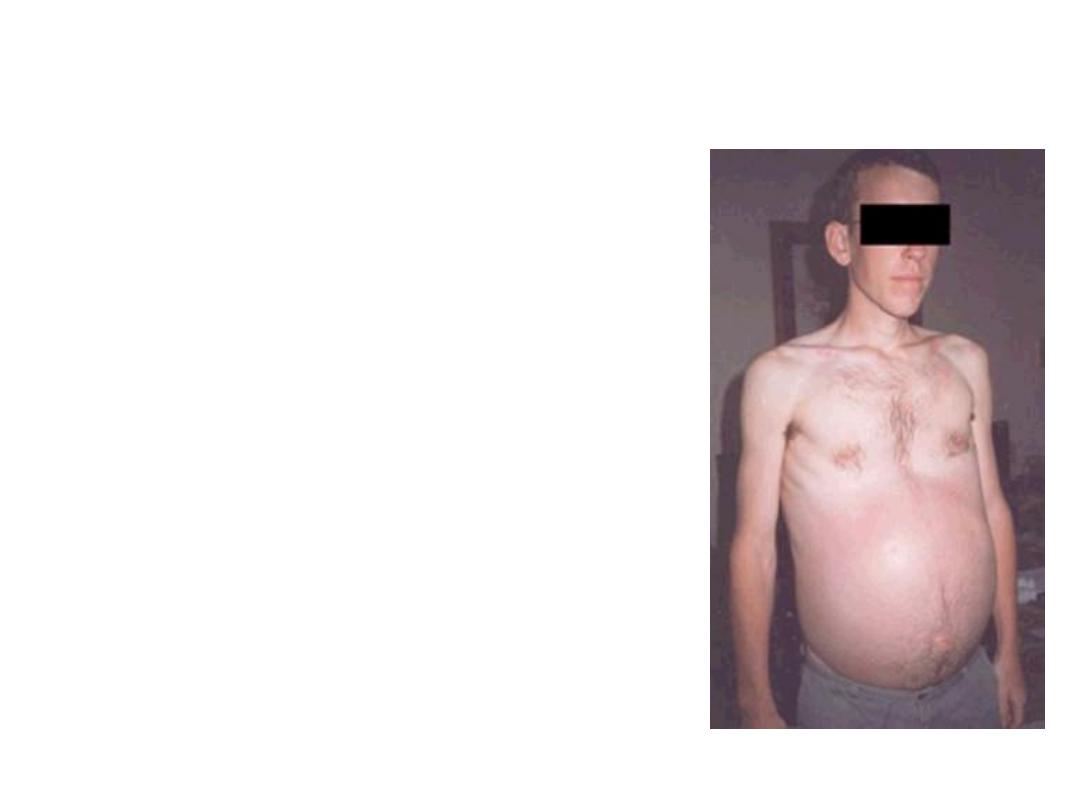
• This patient with chronic
compensated liver failure
complained of increasingly
abdominal distension and was
admitted to hospital. A few days
after admission he became
mildly encephalopathic.
• A. What principle abnormality is
seen here?
• B. What is lokely to have
precipitated his
encephalopathy?
• C. List 5 other factors which
may precipitate encephalopathy
in these patients.
Answer
a. Ascites.
b. Paracentesis
c.
1. Alcohol
2. Drugs e. g. diuretics, narcotics
3. GIT bleeding
4. Infection
5. Surgery (especialy portacaval shunting)
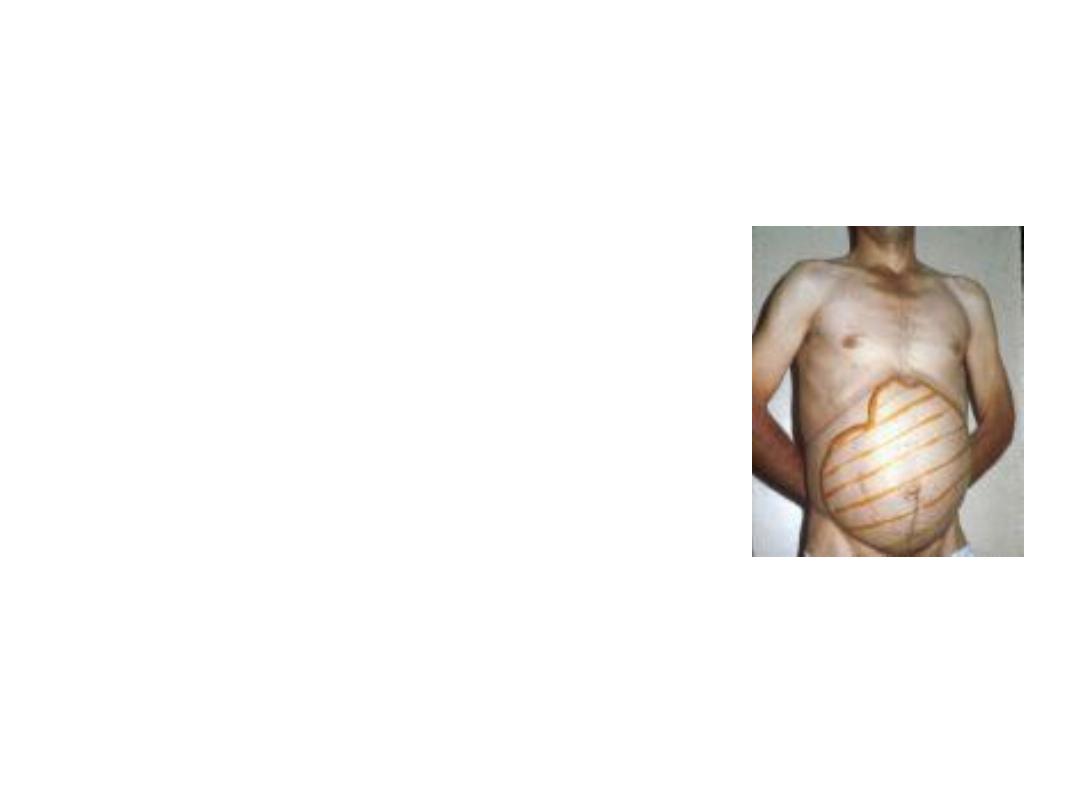
What is this picture is
demonstrating?

The preceding slide is showing huge splenomegaly
(outlined) which is a common medical problem.
Huge splenomegaly is defined by palpable spleen of > 8
cm below costal margin in left mid-clavicular line.
Some causes:
Myelofibrosis.
Malaria faciparum
Liver cirrhosis (due to portal hypertension).
Thalasemia major
Chronic infestation with schistosoma mansoni (unexpected
in S. hematobium).

What is finding? Mention some
important causes
A. Palmar erythema
B. 1. Liver Cirrhosis especialy alcoholic.
2. Normal pregnancy
3. Rheumatoid arthritis.
4. Thyrotoxicosis.
5. Dermatological causes like eczema,
psoriasis,
6. polycythemia
7. Mitral vave disease.

Patchy tender red nodules on
shins and sore throat

Diagnosis is erythema nodosum.
Some causes:
1. TB
2. Sarcoidosis.
3. Streptococcal infection
4. Inflammatory bowel disease.




Diagnosis?

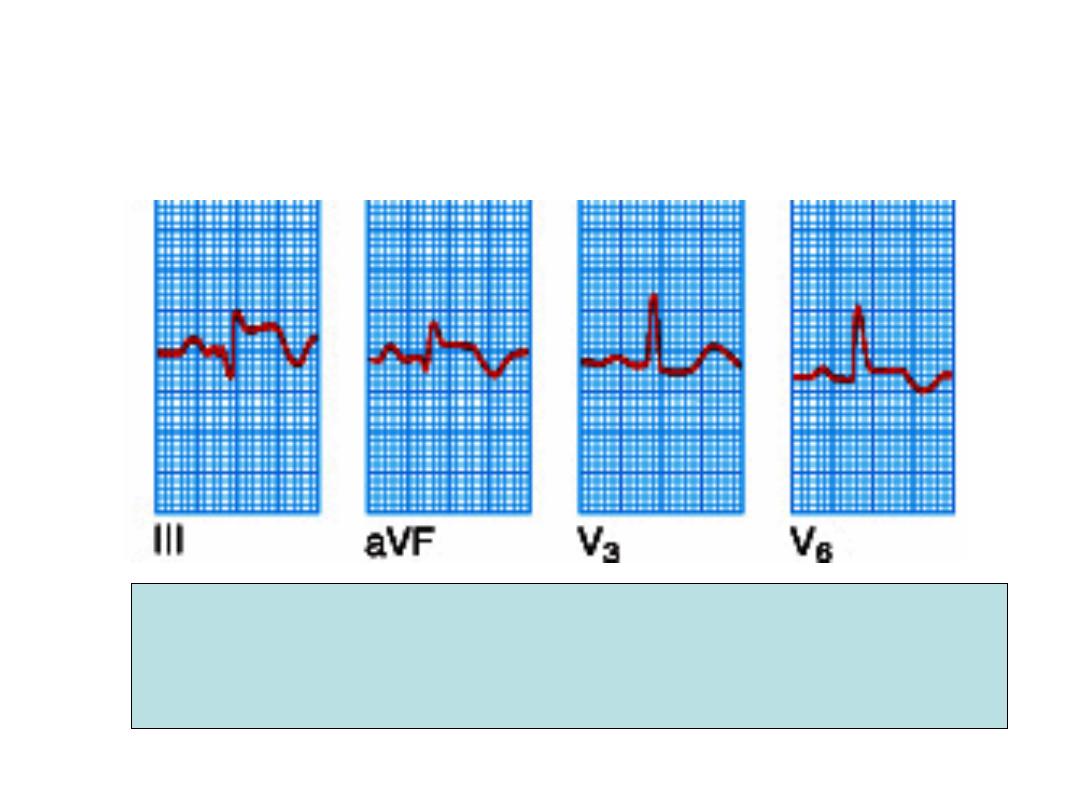
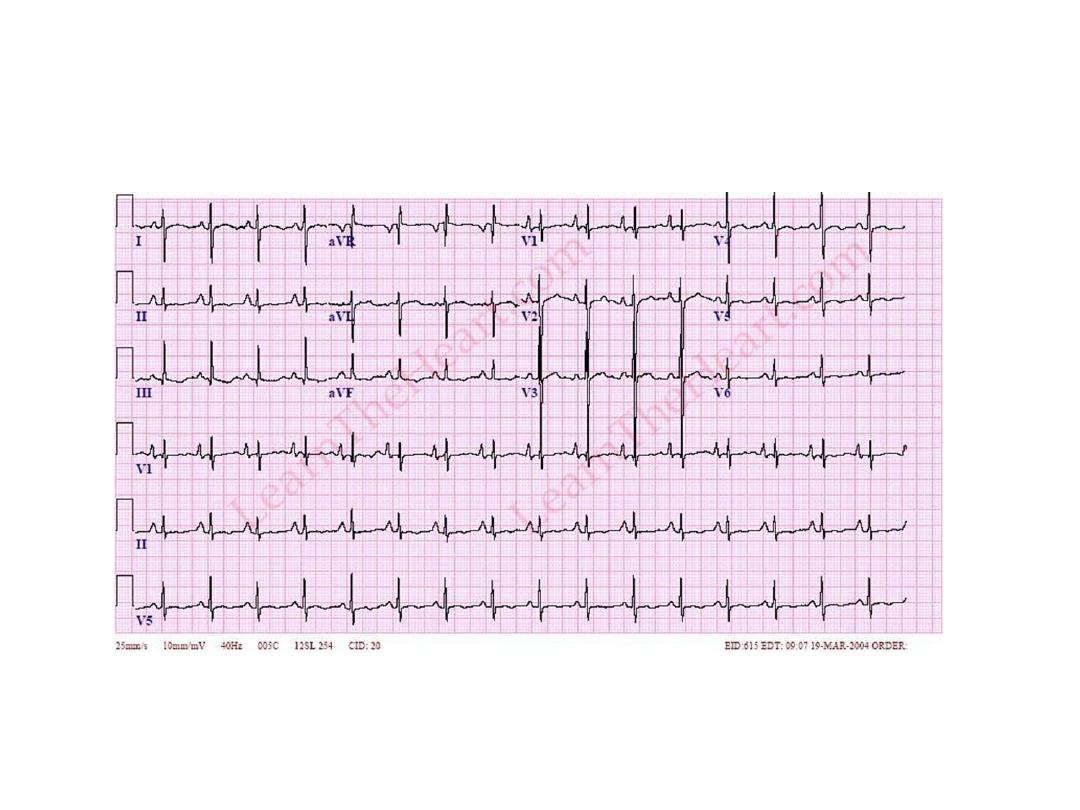
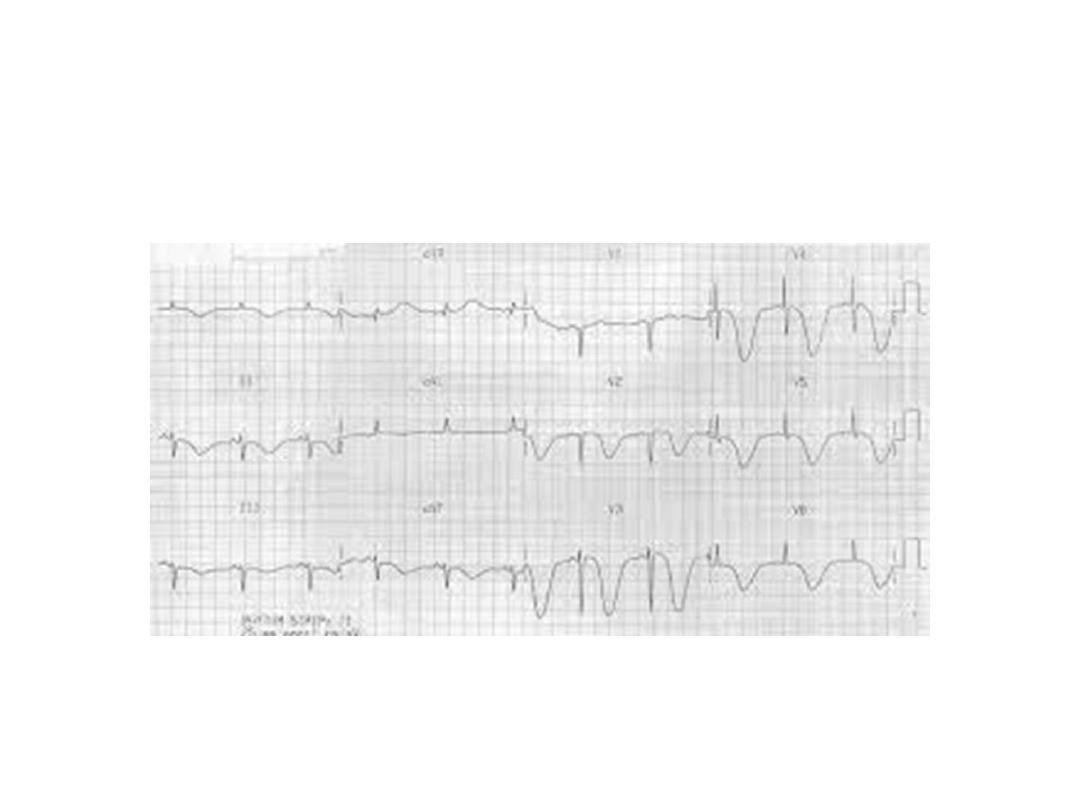
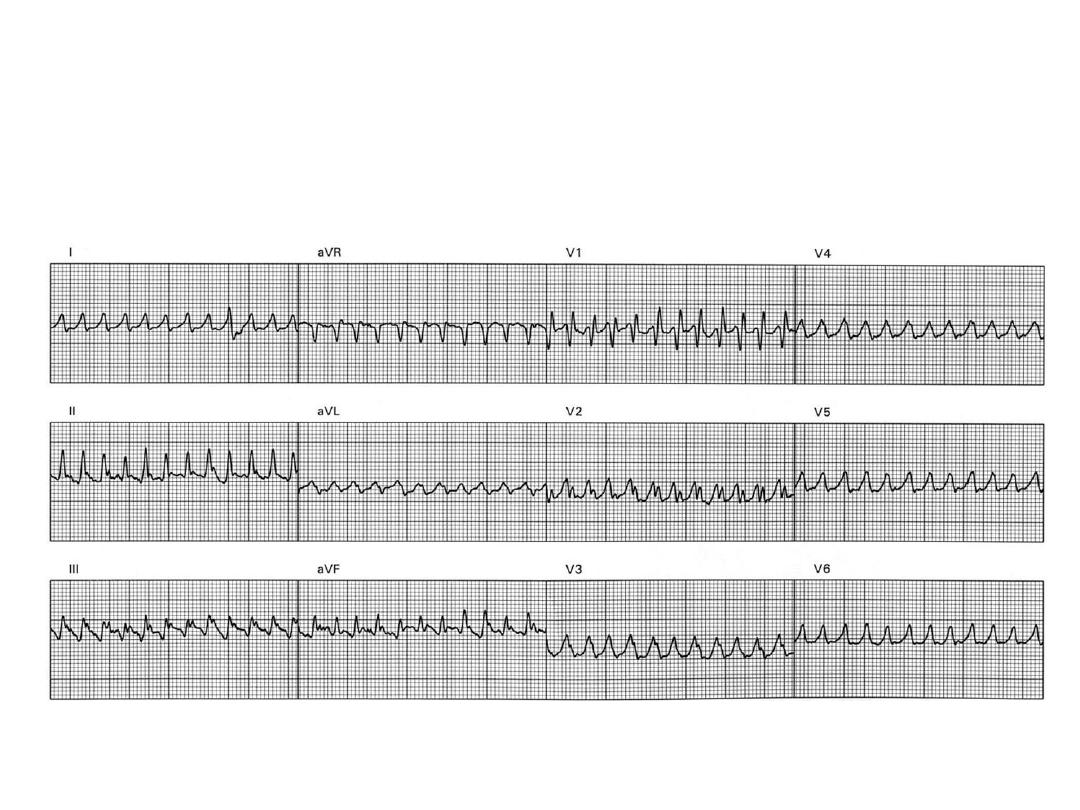
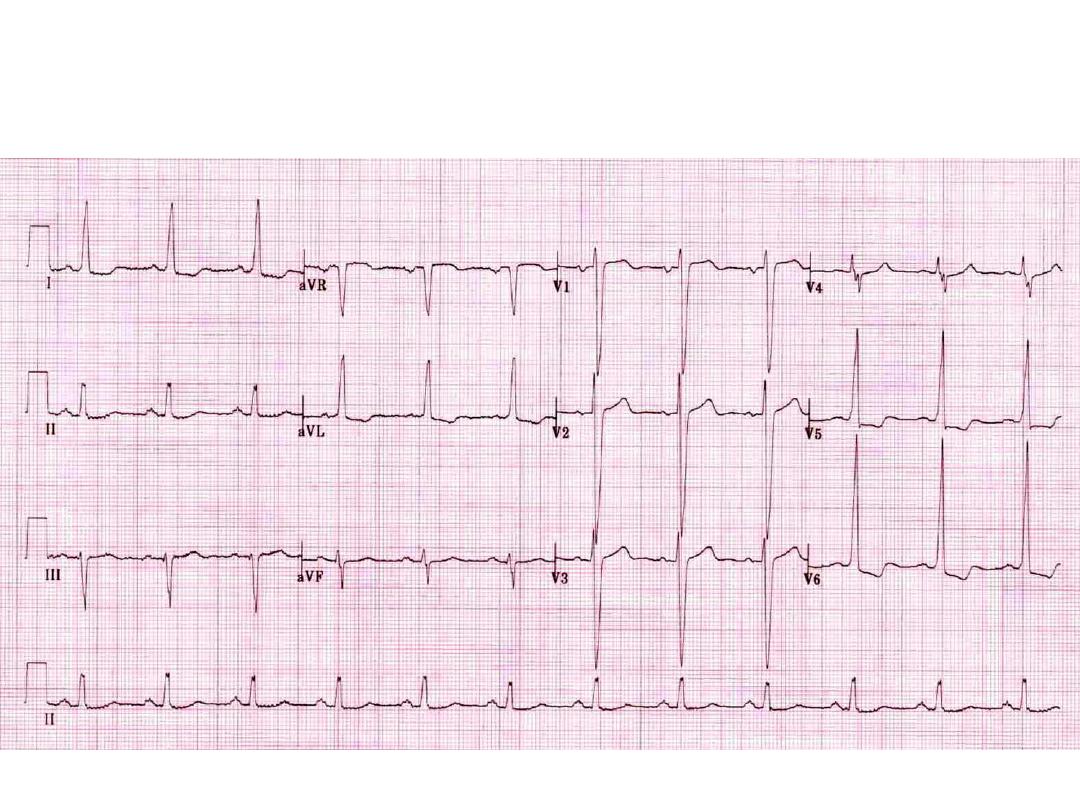
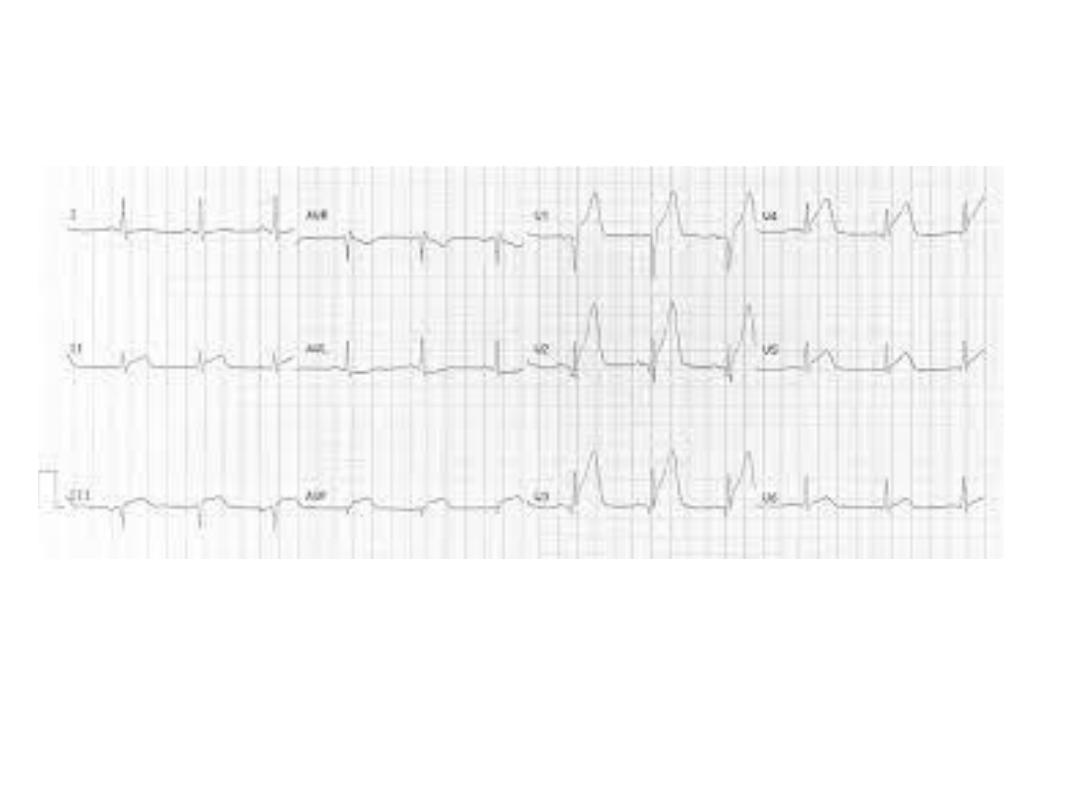
Describe ECG changes. What is the diagnosis?
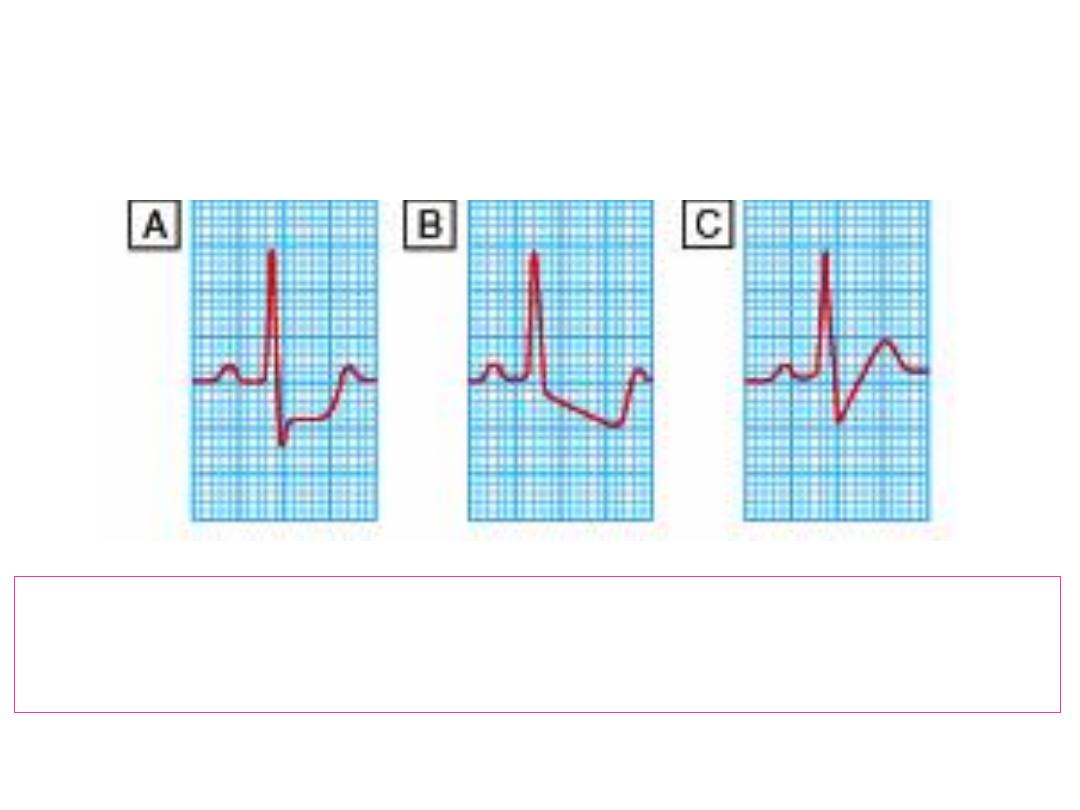
What of ECG changes in angina pectoriss is characteristic?
A
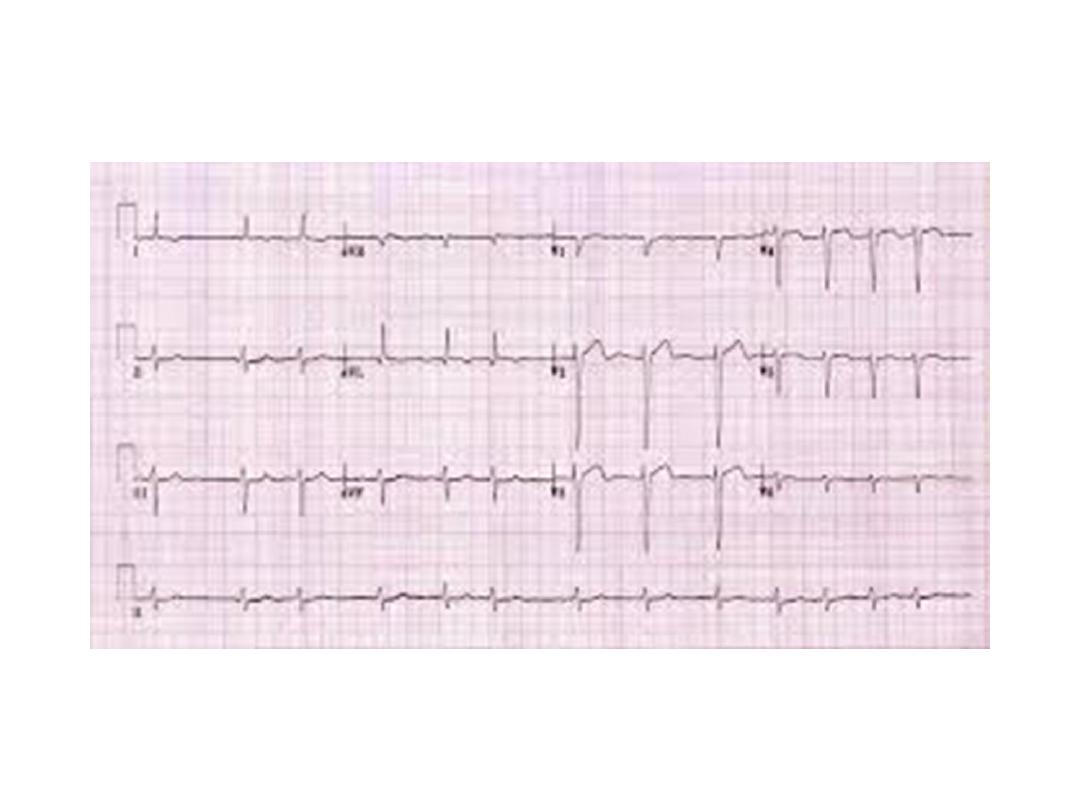
What is the ECG diagnosis?
Enumerate 3 causes

Atrial fibrillation
Three causes:
1. Ischaemic heart disease.
2. Mitral stenosis.
3. Thyrotoxicosis.
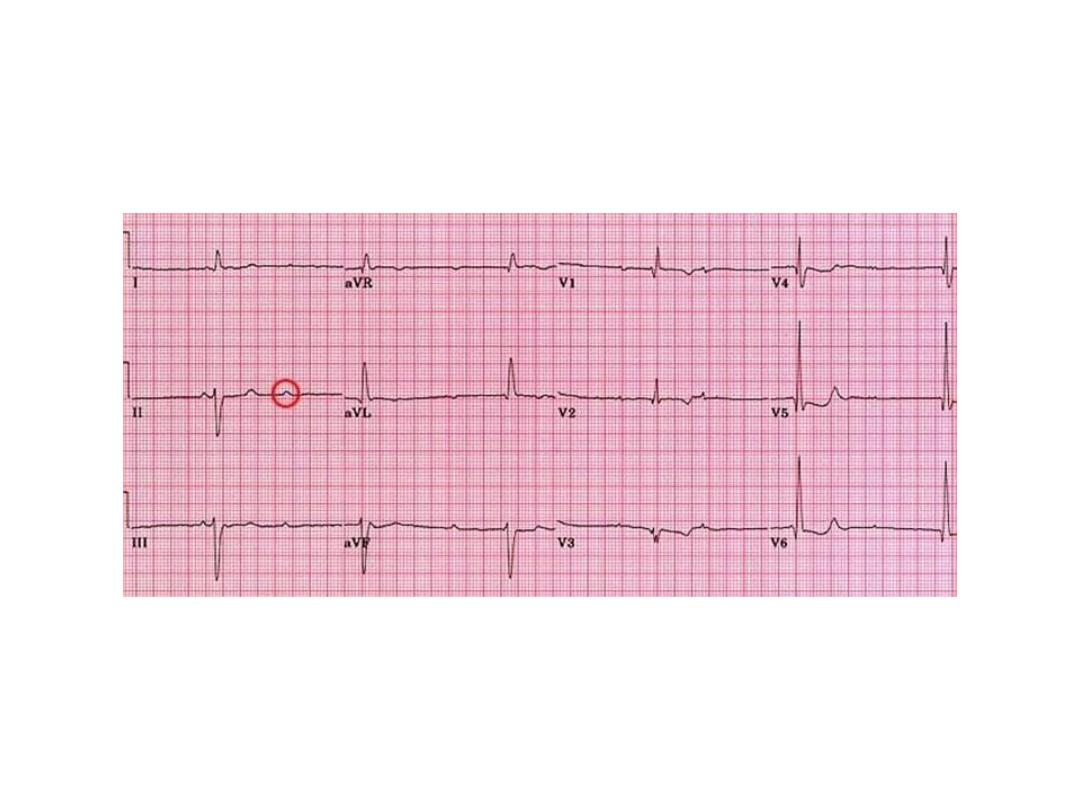
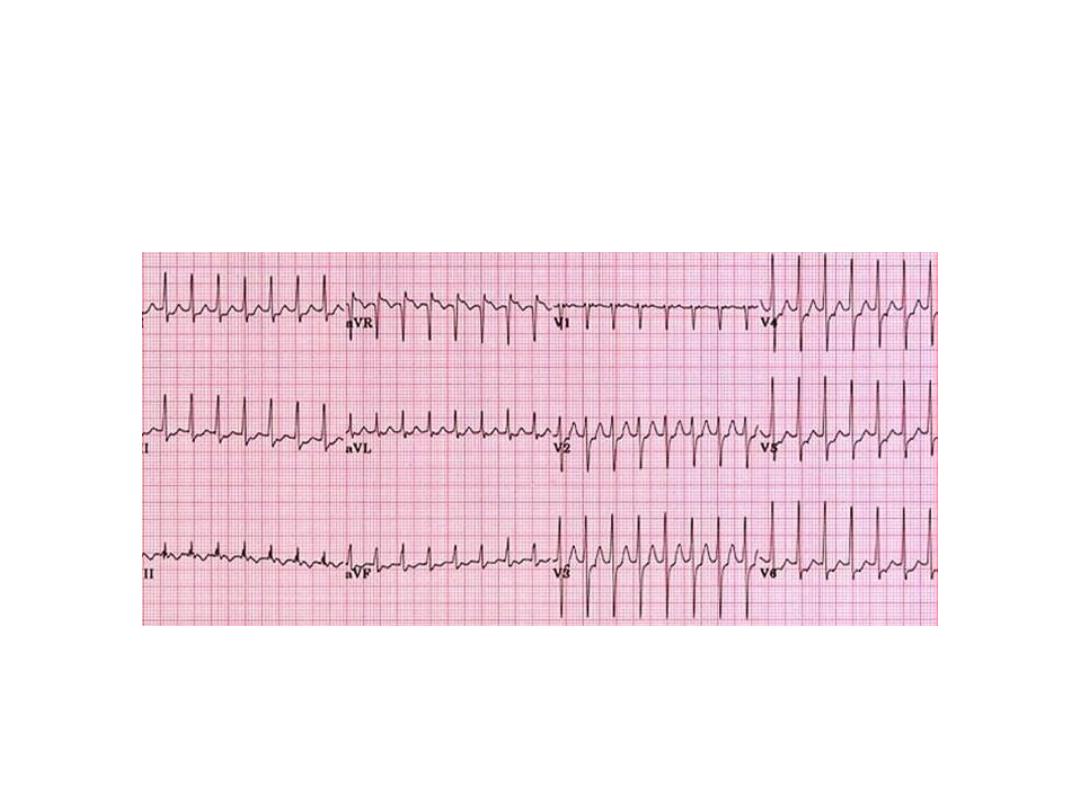
This is an ECG of a patient who
presented with syncopal attacks.

Complete heart block
What is the ECG changes?
Give 2 causes.

RBBB
1. Some times it could normal and
not associated with underlying
organic causes.
2. It may be organic e. g. IHD.
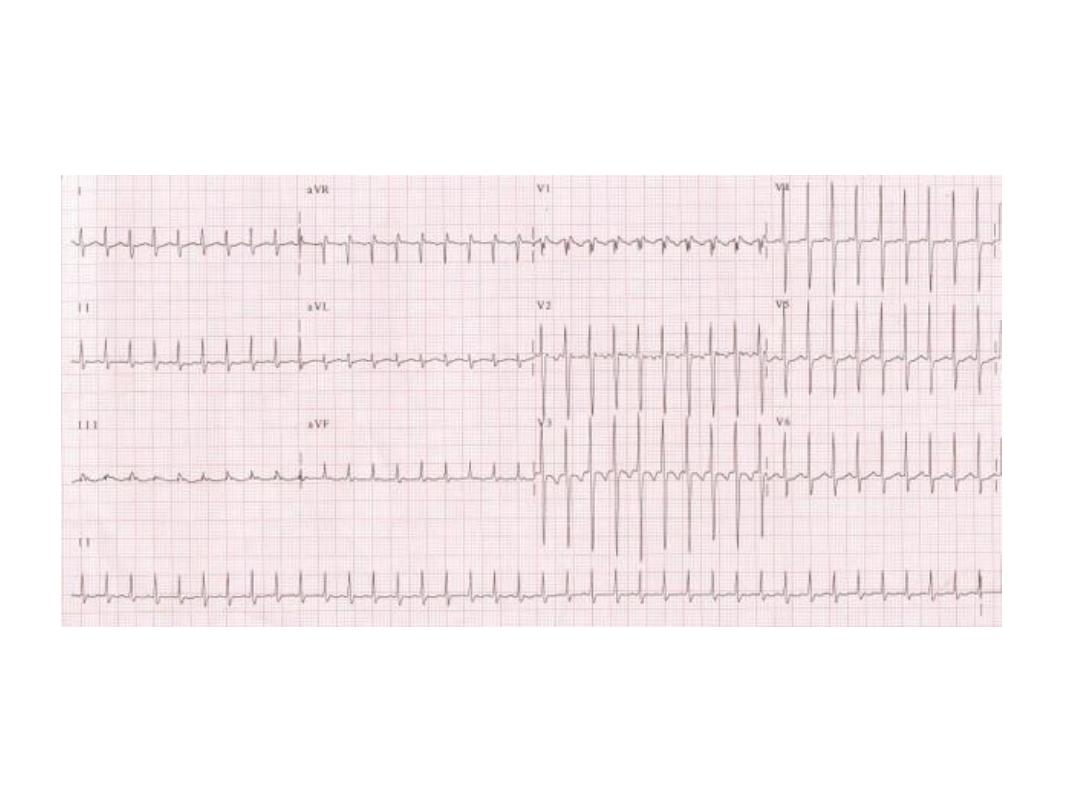
What are the ECG changes? Pick the answer in next
slide.

Prominent P wave (p pulmonale)
especially in lead 2 and V1, RAD,
Prominent R in V1.
This patient had history of CRF? What is
the prominent change(s)? What is the
underlying cause?
Prominent T waves.
Hyperkalaemia.
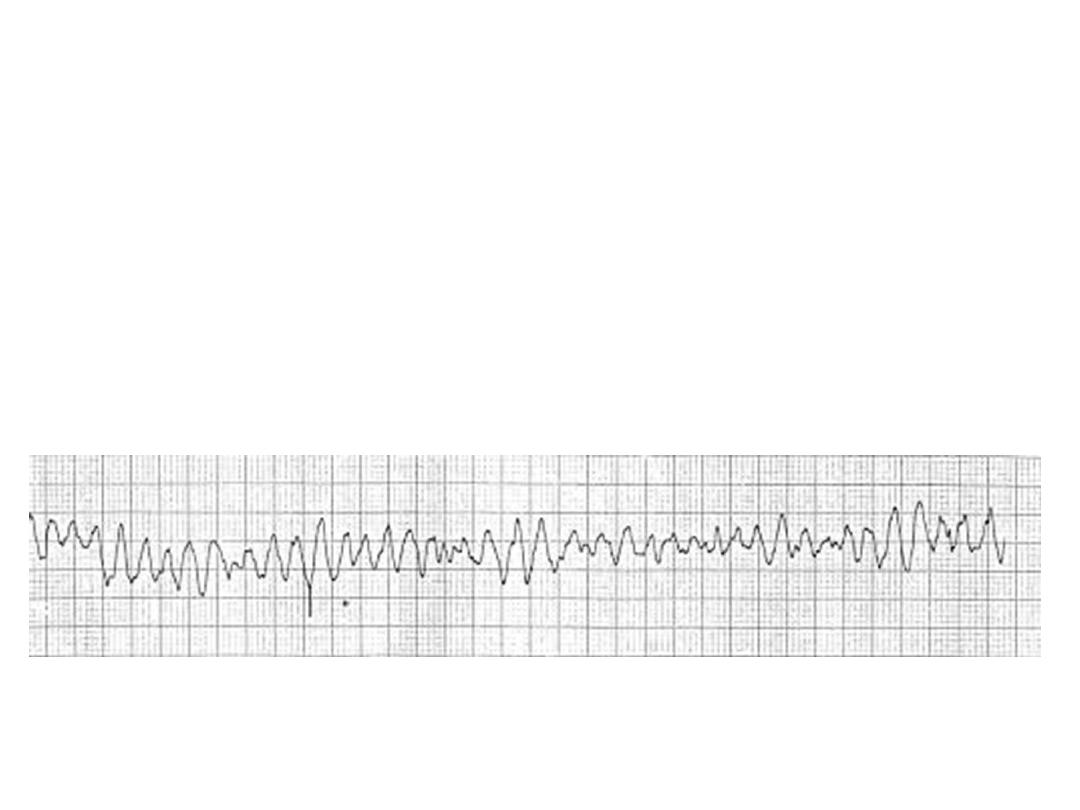
This 65 year-old- patient in CCU because of chest pain
become unconscious with pulseless. What is diagnosis?
What is the immediate action?

• Ventricular fibrillation.
• High Jules DC and cardiopulmonary
resuscitation.

This is the ECG of a patient after treatment for
palpitation? What are the changes? What is the
diagnosis?

Short PR intervals with slurred
QRS complexes.
WPW syndrome
Difficult ECG
What are the findings?
What are the causes?
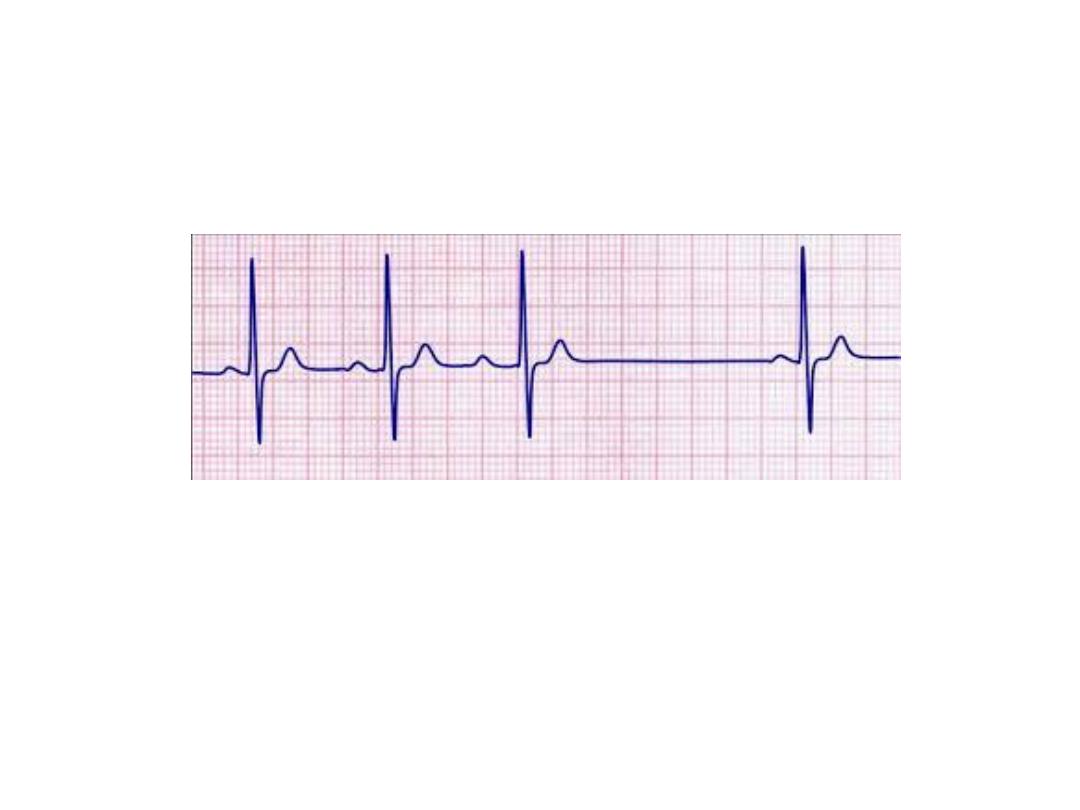
Prominent upright U waves
Causes:
1. Sinus bradycardia accentuates the U wave
2. Hypokalemia (remember the triad of ST segment depression, low amplitude
T waves, and prominent U waves)
3. Quinidine and other type 1A antiarrhythmic.
4. CNS disease with long QT intervals (often the T and U fuse to form a giant
"T-U fusion wave")
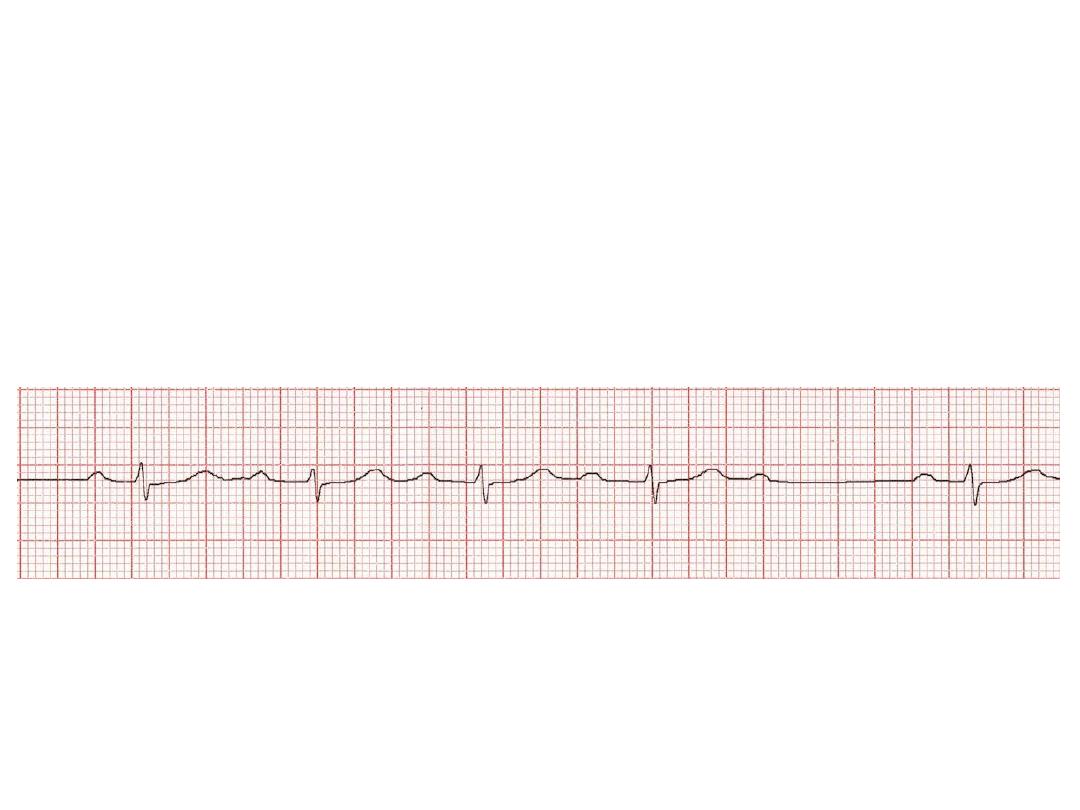
AV Block: 2nd degree, Mobitz I
(Wenckebach Phenomenon)
•Progressive prolongation of the PR interval culminating in a non-conducted P
wave.
•The PR interval is longest immediately before the dropped beat
•The PR interval is shortest immediately after the dropped beat
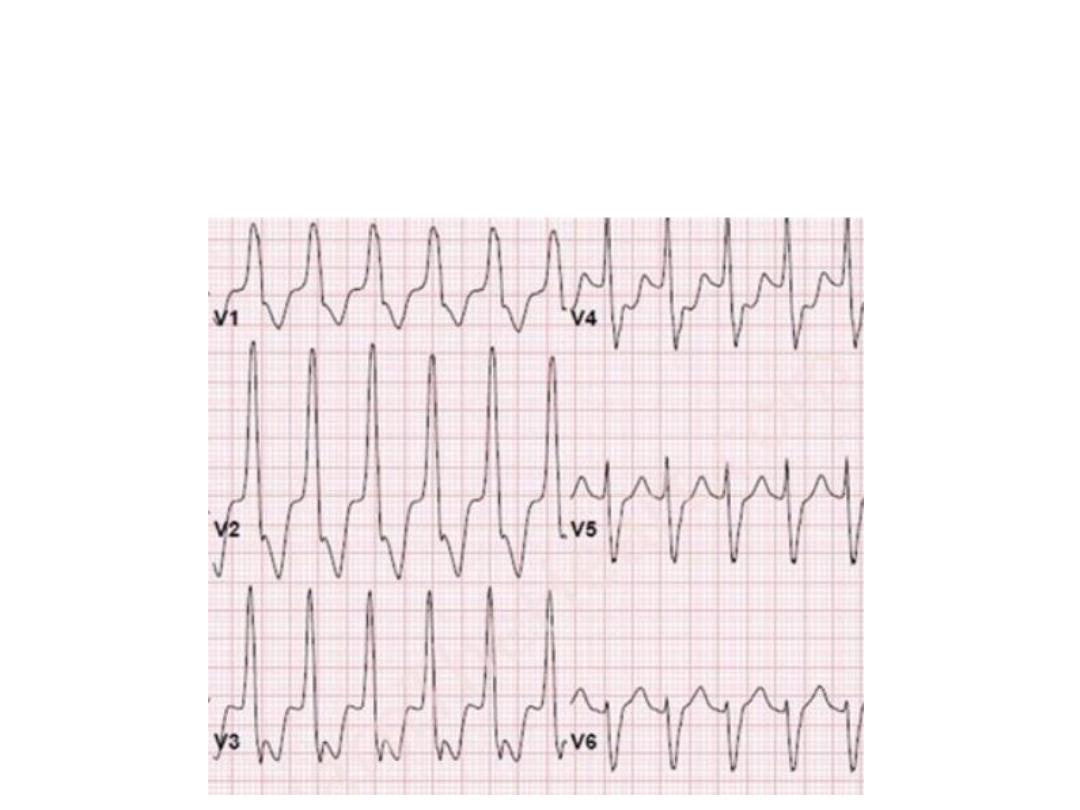
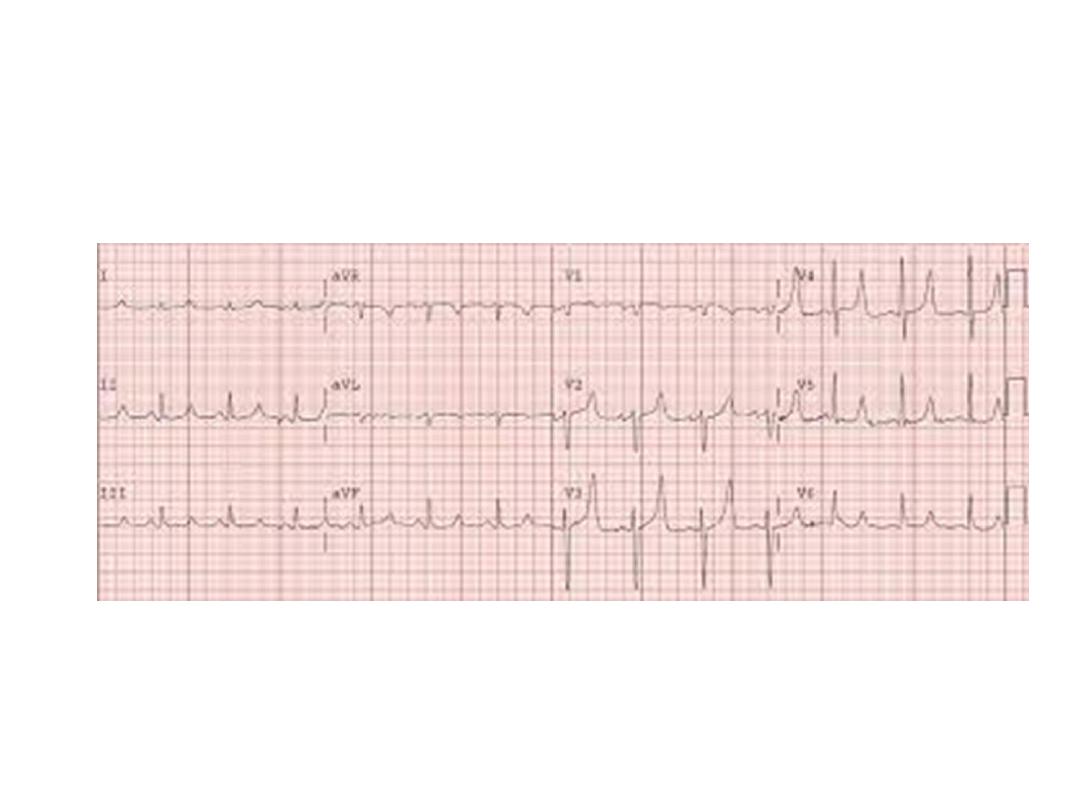
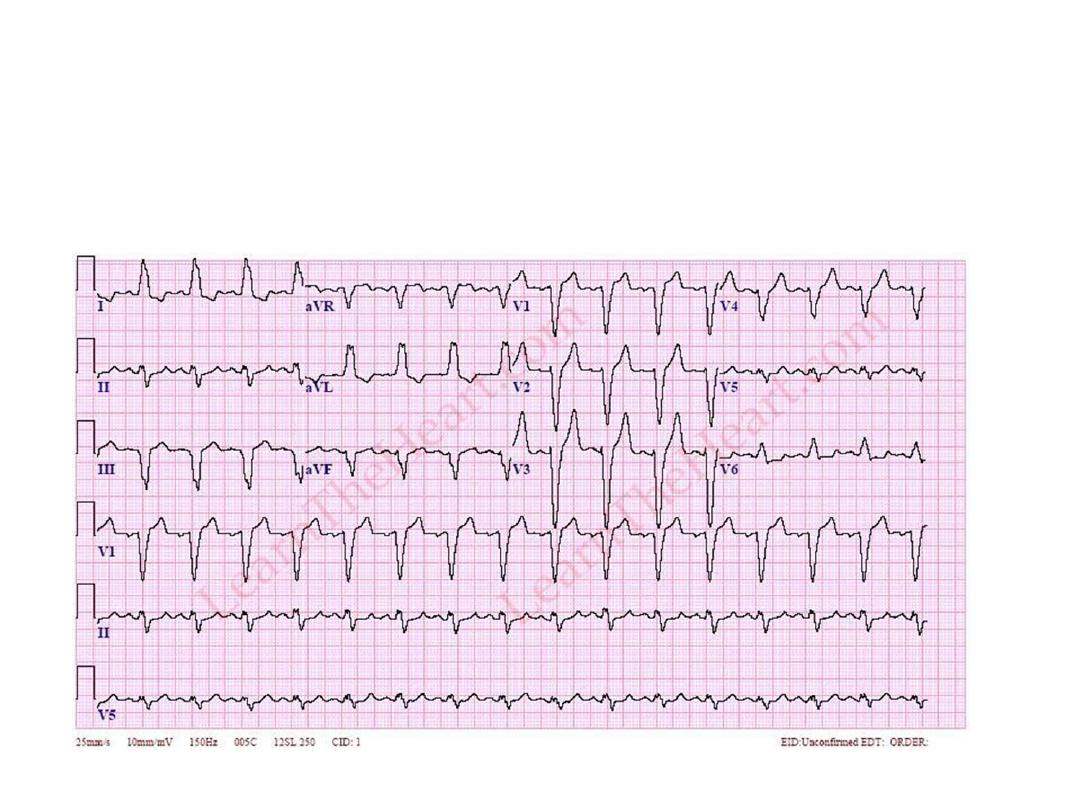
Describe the changes. What is the
diagnosis?

ECG shows rapid monomorphic ventricular tachycardia (VT).
Symptoms of VT include the following:
Palpitation, light-headedness , syncope, chest pain, anxiety
Physical examination:
Hypotension, tachypnea, signs of diminished perfusion,
including a diminished level of consciousness, pallor, and diaphoresis, high jugular
venous pressure, cannon a waves (if the atria are in sinus rhythm).
Mostly due to ischaemia but may be due to other causes.
Management
Unstable patients with monomorphic VT should be immediately treated with
synchronized direct current (DC) cardioversion, usually at a starting energy dose of
100 J (monophasic). Unstable polymorphic VT is treated with immediate
defibrillation. Medications: In stable patients with monomorphic VT and normal left
ventricular function, restoration of sinus rhythm is typically achieved with
intravenous (IV) procainamide or sotalol. IV lidocaine is effective at suppressing
peri-infarction VT but may increase the overall mortality risk. In torsades de
pointes, magnesium sulfate may be effective if a long QT interval is present at
baseline. For long-term treatment of most patients with left ventricular dysfunction,
current clinical practice favors class III antiarrhythmics (eg, amiodarone and
sotalol). In patients with heart failure, the best proven antiarrhythmic drug
strategies include the use of beta receptor
–blocking drugs (eg, carvedilol,
metoprolol, and bisoprolol); angiotensin-converting enzyme (ACE) inhibitors; and
aldosterone antagonists
This is ECG of a patient with history of episodic palpitations.
What is ECG diagnosis? Mention the short term drug treatment.

SVT (AV reentry ) is not usually associated with structural heart
disease and commonly presents as a variety of symptoms
including palpitations, nervousness, anxiety, syncope or heart
failure.
Treatment: short-term management of supraventricular
tachycardia (SVT) involves intravenous adenosine or calcium
channel blockers
What is the ECG diagnosis?
Enumerate some causes.

LBBB:
Always pathological
Among the causes of LBBB are:
Aortic stenosis
Dilated cardiomyopathy
Acute myocardial infarction
Extensive coronary artery disease
Primary disease of the cardiac electrical conduction system
Long standing hypertension leading to aortic root dilatation
and subsequent aortic regurgitation
Lyme disease
Side effect of some cardiac surgeries (e.g., aortic root
reconstruction)
What are the ECG changes? Mention the causes.

Tall R in V6 and deep S in V1(sum >
35mm) with strain pattern in V5 and V6.
Tall R in I and AVL leads (> 20mm).
Diagnosis: LVH
Causes:
Hypertension.
Aortic stenosis.
Hypertrophic cardiomyopathy.
Athletic training.
What are the ECG finding and diagnosis?
Comment on emergency treatment goals

•ST elevation in leads II, III and aVF
•Progressive development of Q waves in II, III and aVF
•Reciprocal ST depression in aVL )± lead I)
Diagnosis
is acute inferior STEMI.
Emergency treatment:
Once the diagnosis of an acute STEMI
is made, the early management of the patient involves the
simultaneous achievement of several goals:
●Relief of ischemic pain
●Assessment of the hemodynamic state and correction of
abnormalities that are present
●Initiation of reperfusion therapy with primary percutaneous
coronary intervention (PCI) or fibrinolysis
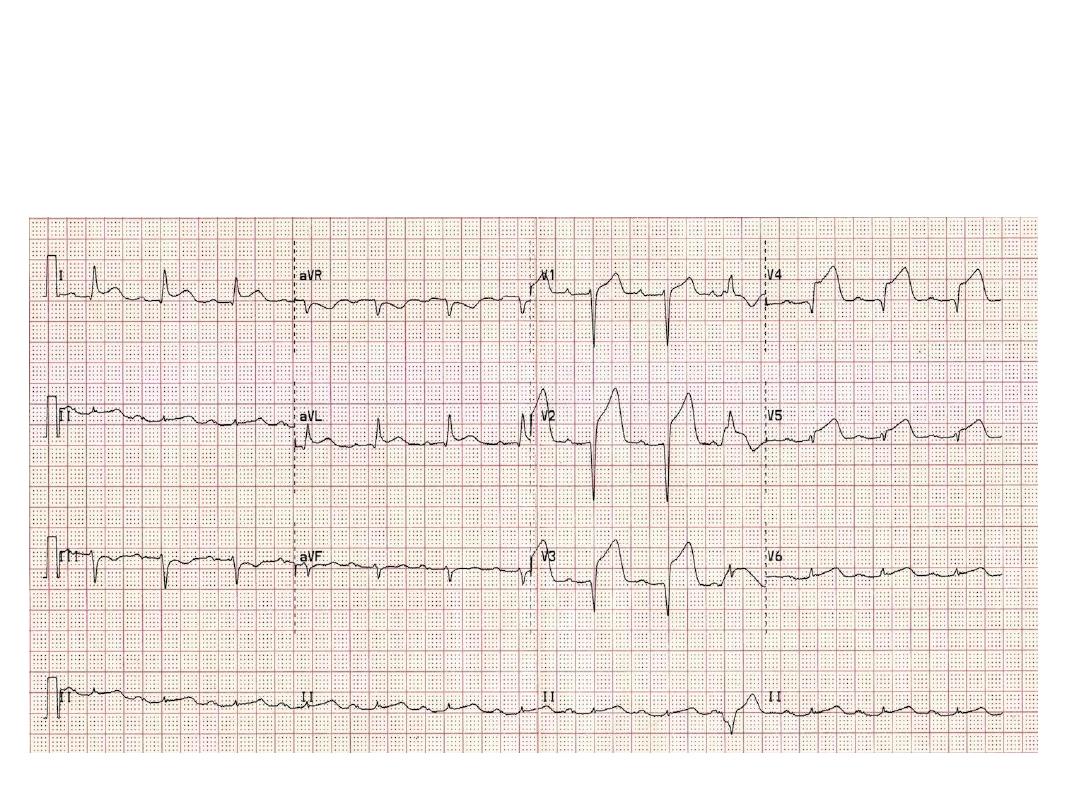
What is this ECG is demonstrating? What is the
likely complaint of the patient?

Acute anterior STEMI.
The likely presentation is chest
pain.
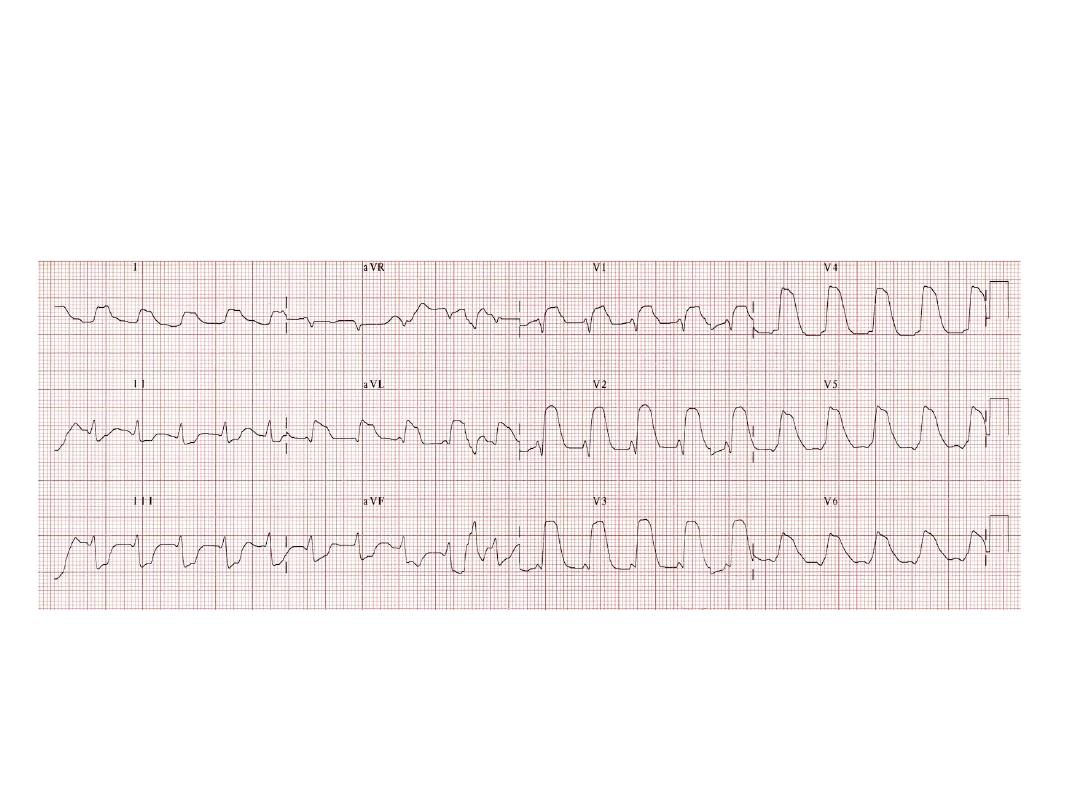
Another extensive acute
STEMI
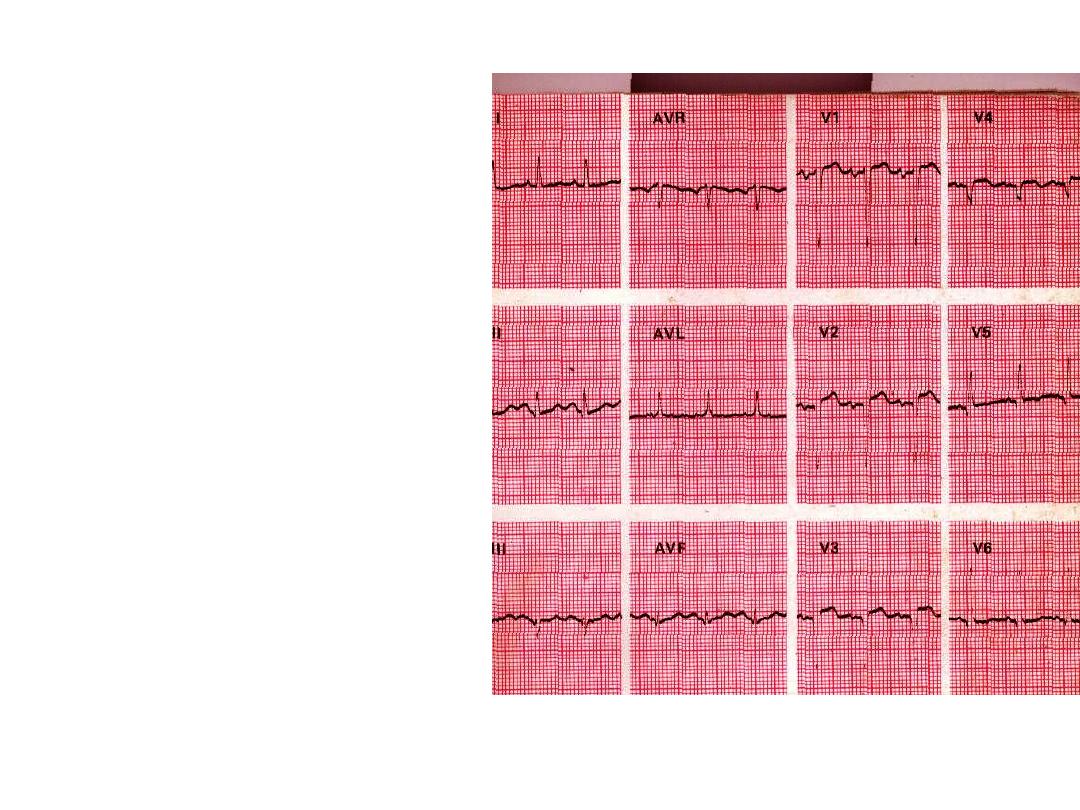
This sixty year old man
had a
myocardial infarction 8
months
Ago. He has now
developed
Refractory heart failure.
a. What abnormalities are
present?
b. How may this explain
his HF?
c. What clinical signs may
be
Present in addition to
those of
HF?
Answer:
a. Sinus tachycardia, P mitrale, anteroseptal MI:
ST elevation in lead V1-V4.
b. He has developed a ventricular aneurysm. The
p mitrale may indicate mitral regurgitation and
dilatation of left atrium.
c.
A diffuse, often laterally displaced apex beat
with a double or paradoxical impulse is
characteristic of ventricular aneurysm, the
murmur of MR may be present.
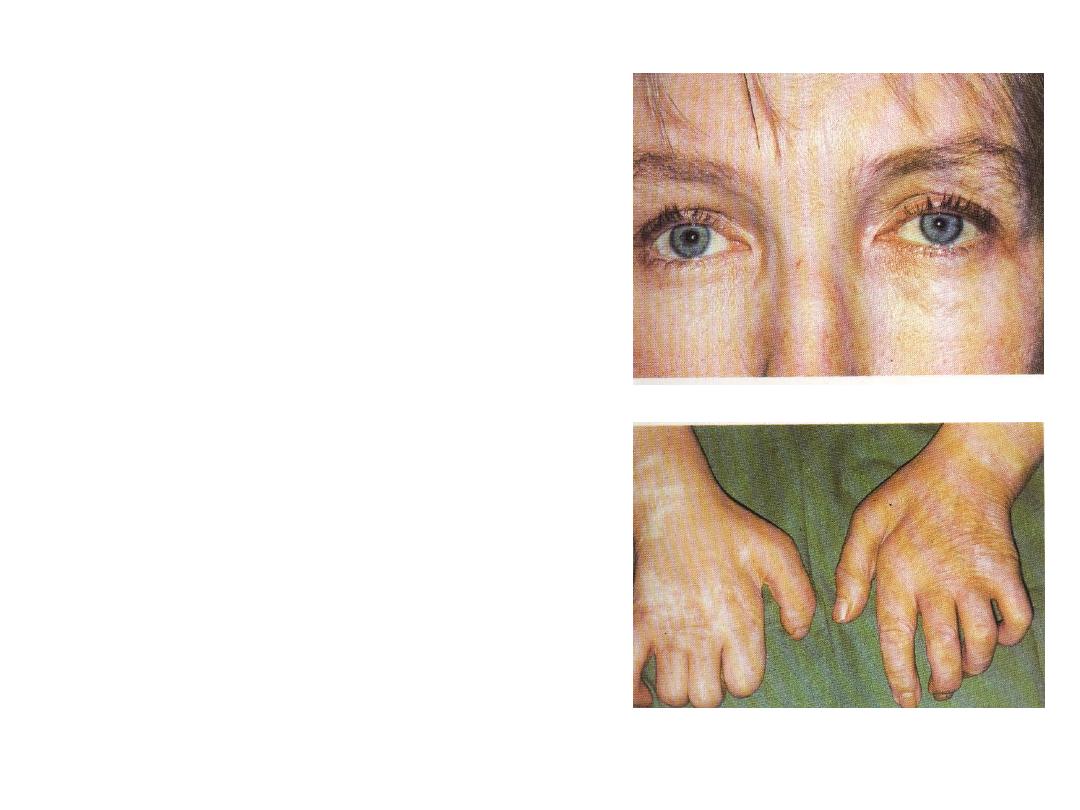
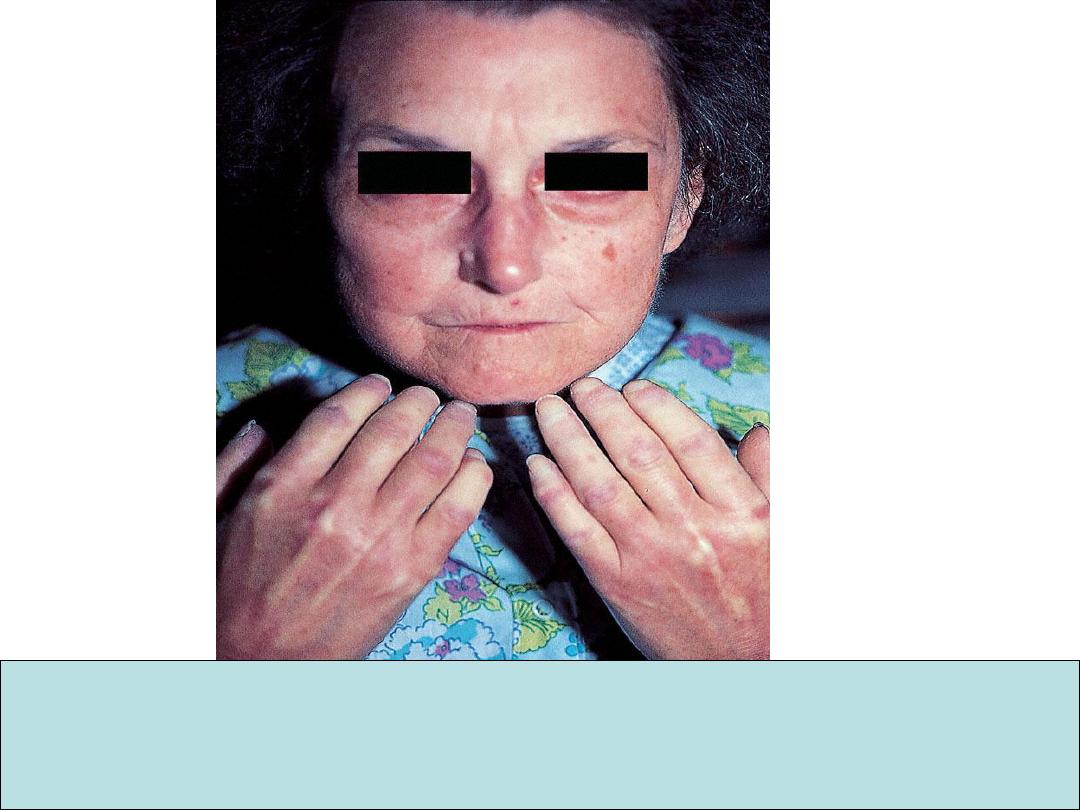
This patient’s principal
complaint is of pain across
the shoulder girdle.
A. What abnormalities are
seen in:
1. Her face (look to eyes)
2. Her hands
B. Suggest two possible
diagnosis.
a.
1
. L horner’s syndrome.
2. Wasting of first dorsal interosseus muscle on
both sides, multiple healed scars, claw hand on
the R.
b.
1. Syringomyelia.
2. Intrinsic tumour of the spinal cord (e. g.
ependymoma, glioma).
3. Bilateral lower brachial plexus lesions (e. g.
in association with pancoast tumours) unlikely.
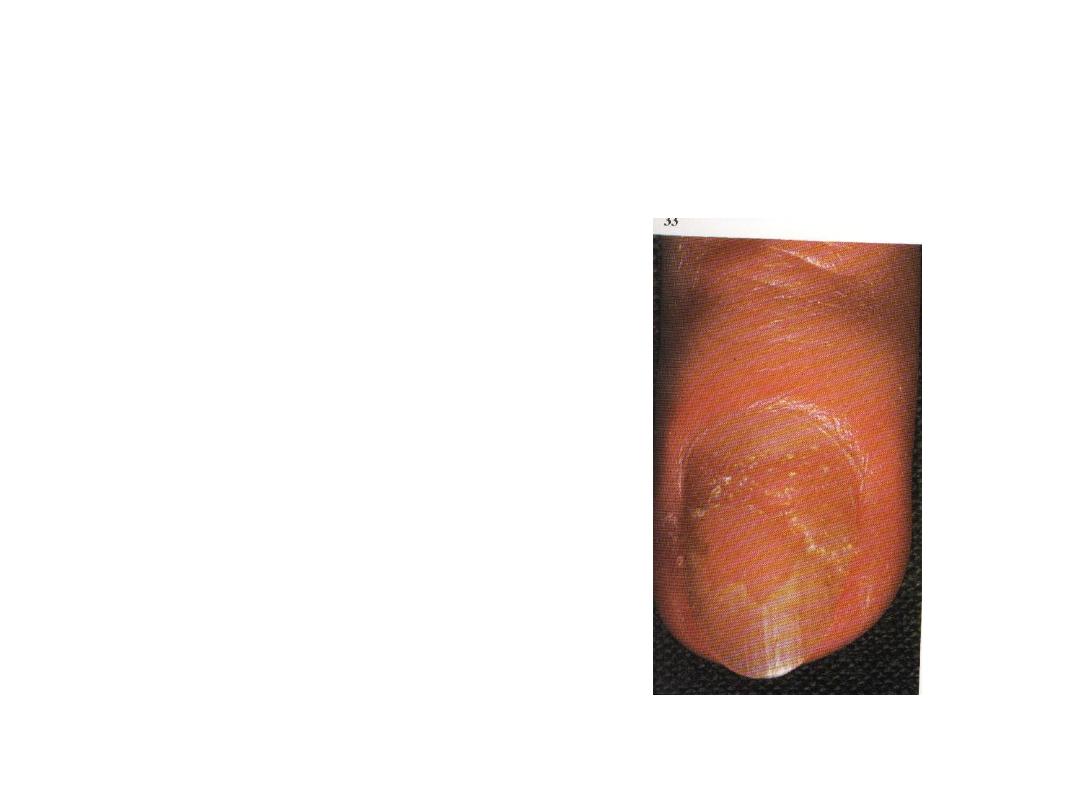
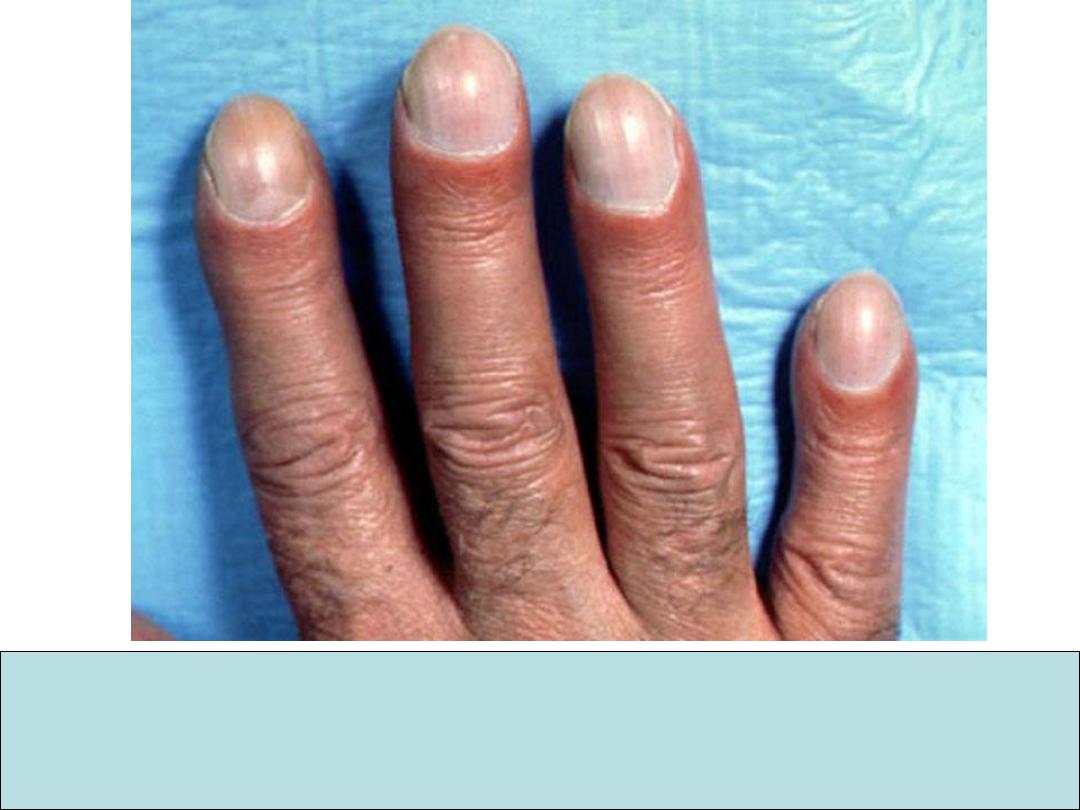
A. What is the most likely
diagnosis associated with
the nail abnormalities
shown?
B. What are the
characteristic nail
changes in this condition?
Answer
a. Psoriasis
b. Nail changes include:
1. Pitting
2. Onycholysis
3. Discoloration
4. Thickening
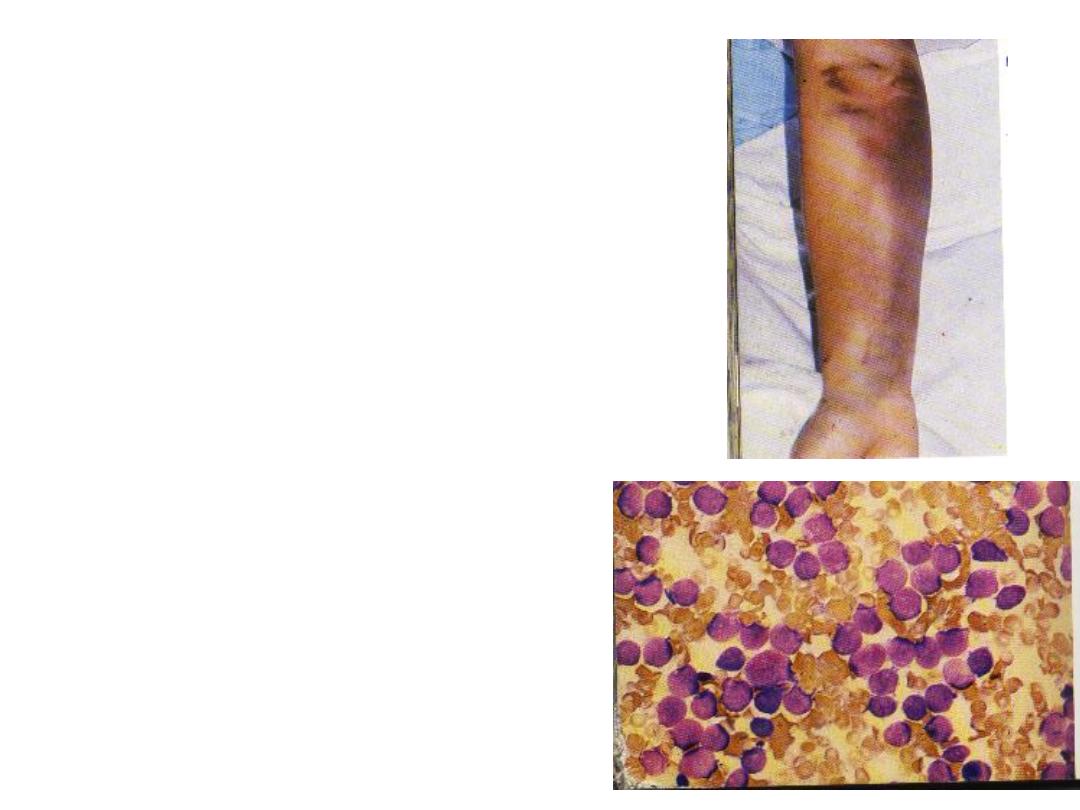
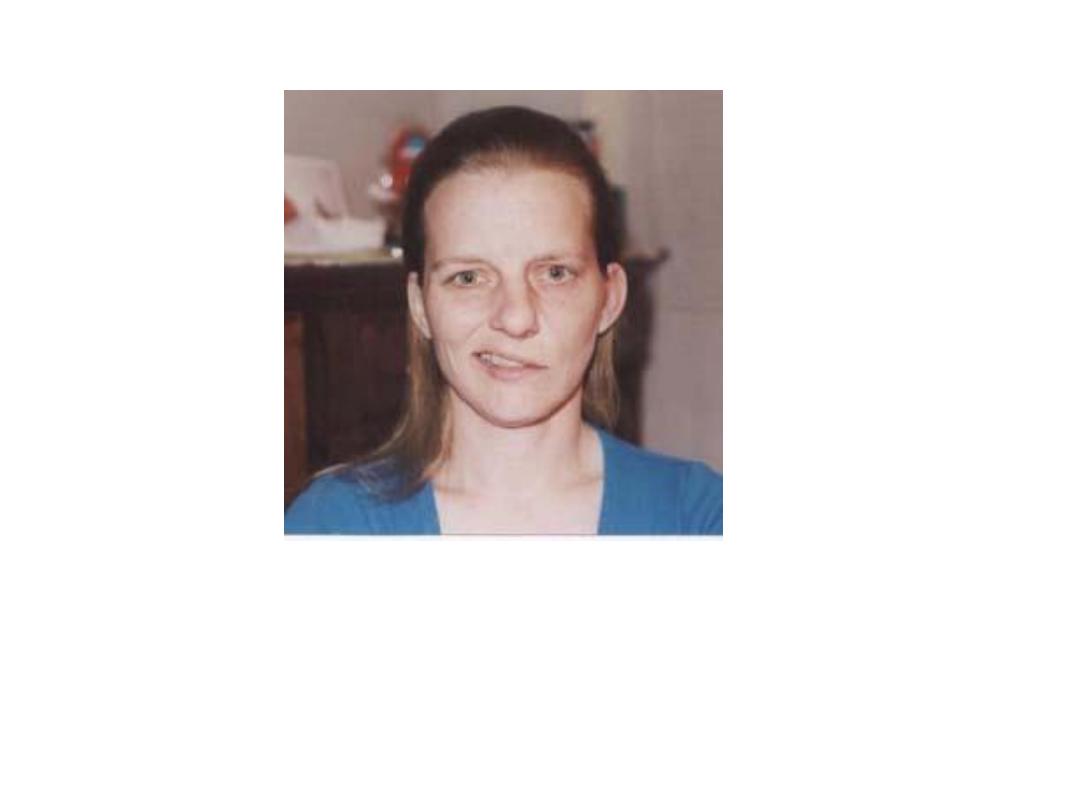
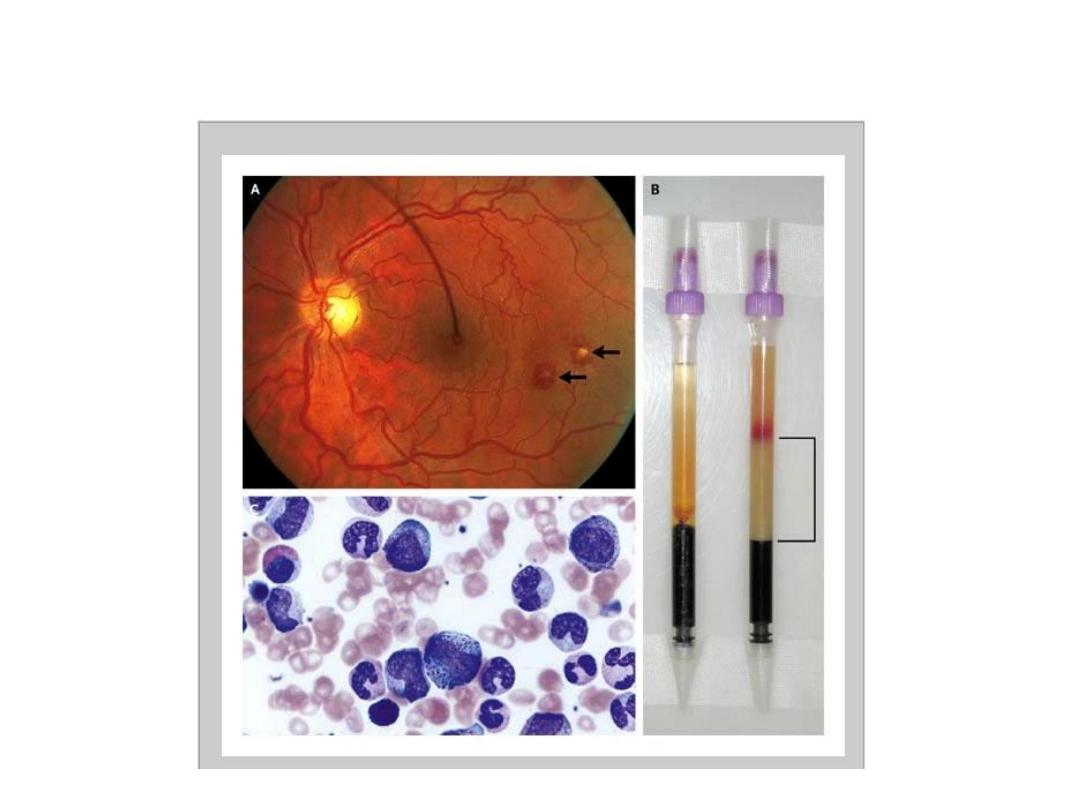
This patient complained of
lethargy, pallor and
increasing bruising. She
was noted to bleed
excessively from
venepuncture sites. Her
hemoglobin was 8g/dl,
WBC 178
×10
9
/l and platelet
count 21
×10
9
/l. PT and
PTT prolonged. FDP
present in excess.
A. What is diagnosis?
B. What complication
occurred?
Answer
A. Acut myeloblastic leukaemia,
promyelocytic variant.
B. DIC
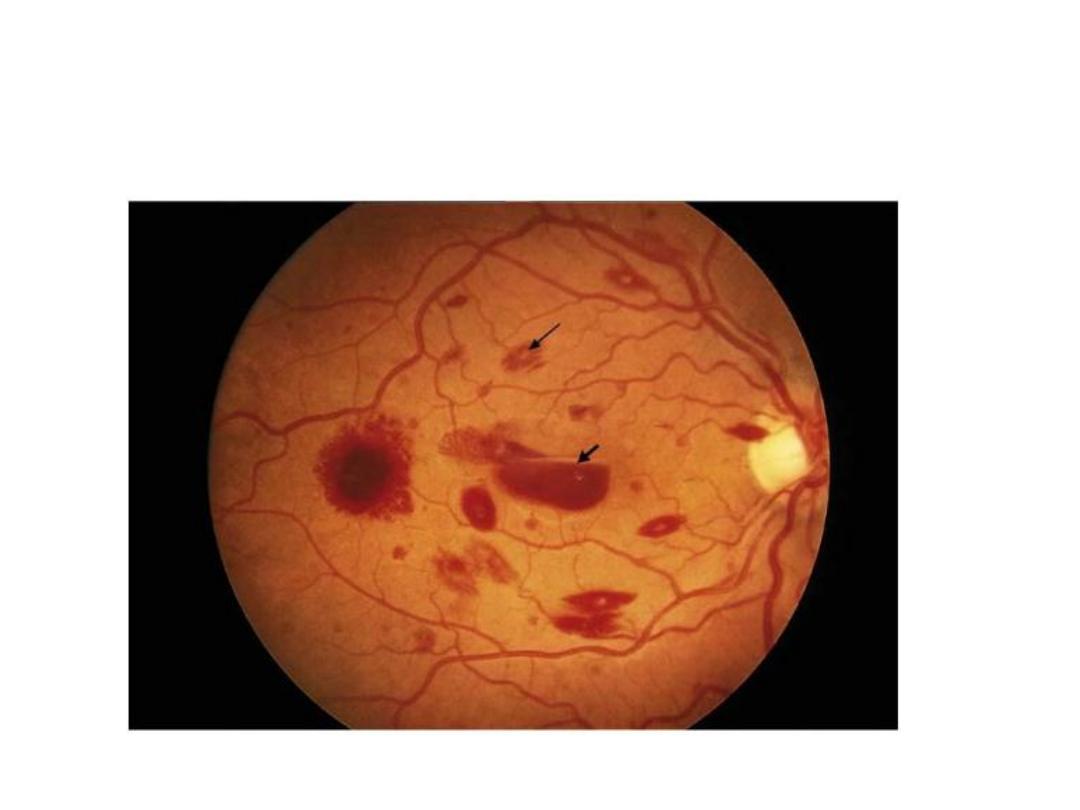
Retinal haemorrhage in AML

Extensive purpuric lesions in extremeties
(Henoch-Sconlein Purpura)

Pathological fracture - MM

Acanthosis nigricans (causes)
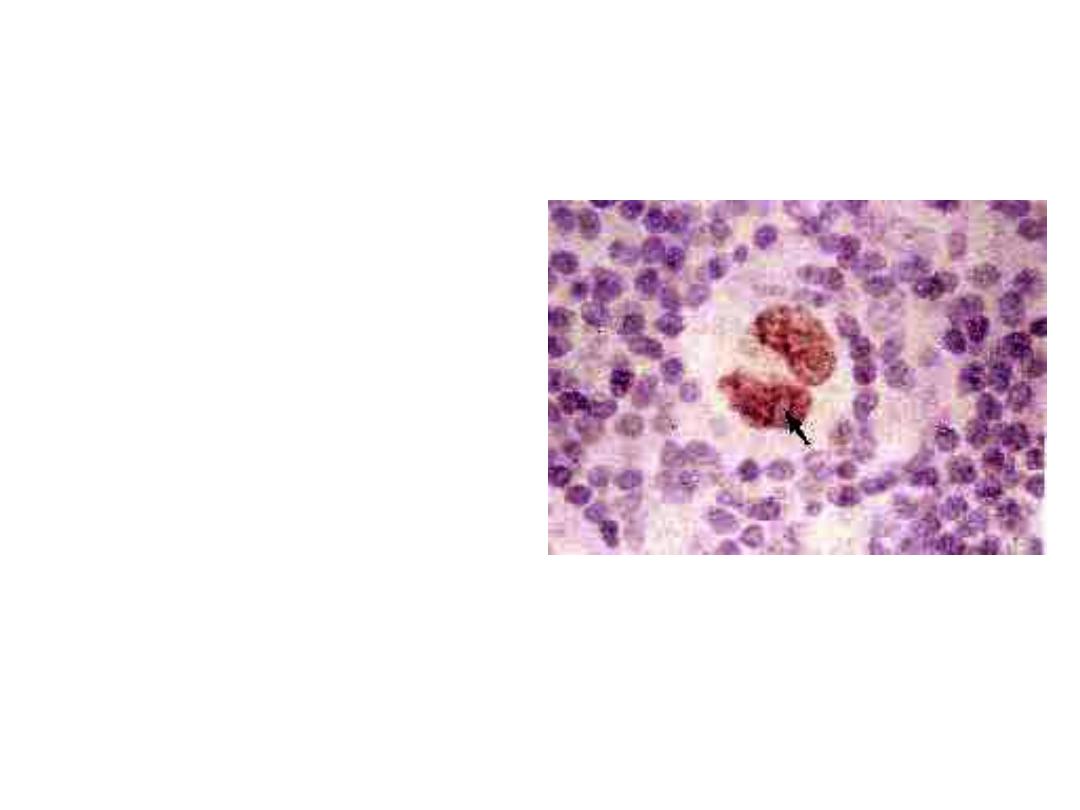
This is a histopathogy of
an enlarged cervical
lymph node:
A. What are findings in
this slide?
B. What is clinical
diagnosis?
C. What are the
histological types?
D. Enumerate some
investigations that
are useful for
diagnosis and
staging.
A.
1. A large numbers of lymphocytes (T-cells)
2. The presence of histological hallmark of HD
“Reed – Sternberg’ cells.
3. Other cells like plasma cells and eosinophils.
B. HD
C. 4 types: 1. L-predominant. 2. Nodular sclerosis.
3. Mixed cellularity. 4. L depleted.
D. Lymph node biopsy, CXR, CT-Abdomen, LF
and RF tests, LDH,ESR and CBP.
•
This 32 year old female
patient complains of
generalized pruritis.
Examination reveals no
dermatological
abnormality.
A. What abnormality is seen
on CXR?
B. What is the likely
diagnosis?
C. What is the most likely
histological varietyin this
case?
A. Massive hilar, paratracheal and upper
mediastinal lymphadenopathy.
B.
Hodgkin’s disease.
C. Nodular sclerosing (the most frequent
variety), more in young and female
patient.

•
This patient was admitted
to hospital complaining of
headache, neck stiffness,
and drowsiness. The
following day this facial
appearance had
developed.
A. What is the likely
diagnosis?
B. What would lumber
puncture show?
C. How is the diagnosis
confirmed?
A. Mumps meningitis.
B. Lymphocytosis, high protein but normal
sugar 9Aseptic meningitis
C. Confirm by serogy for mumps (if
available).
This is a 45 year old female
patient, her condition
preceded by prolonged
pruritis.
A. What is the most likely
diagnosis?
B. Give the name of a single
laboratory test helps to
confirm diagnosis.
C. What are other
investigations to be done
for this patient?
D. What are other D. D?
A. Primary biliary cirrhosis.
B. AMA assay (anti-mitochondrial-
antibodies).
C. S. bilirubin, liver enzymes, ANF,
immunoglobulins, US of liver and biliary
passage, CT scan or MRI with MRCP
and ERCP. Liver biopsy may be needed
but should be avoided in the presence of
dilated biliary passages.
A. Describe the
principle abnormality
shown?
B. Suggest 3
investigations which
would help in
making a diagnosis.
C. List 4 possible
diagnosis.
A. Goiter.
B. 1. Isotopic thyroid scan
2. US scan of thyroid
3. FNA
– aspiration biopsy.
4. S. T4 and T3 and TSH
C. Colloid cyst of thyroid, thyroid adenoma,
thyroid carcinoma and thyro-glossal cyst.

This patient has Graves’
disease.
a. Which ocular feature is
demonstrated here?
b. How is the abnormality
measured objectively?
a. Proptosis (this patient also may also have
exophthalmos-sclera visible between the
iris and lower lid- this is best seen from the
front.
b. Exophthalmometer: Measuring the
distance between the later angle of the
orbit and an imaginary line perpendicular
to the cornea’s anterior surface.
This patient presented with heat intolerance.
What is the likely diagnosis? Mention an
investigation to confirm diagnosis.

Grave’s disease )thyrotoxicosis)
Hormonal assay: T4, T3 and TSH
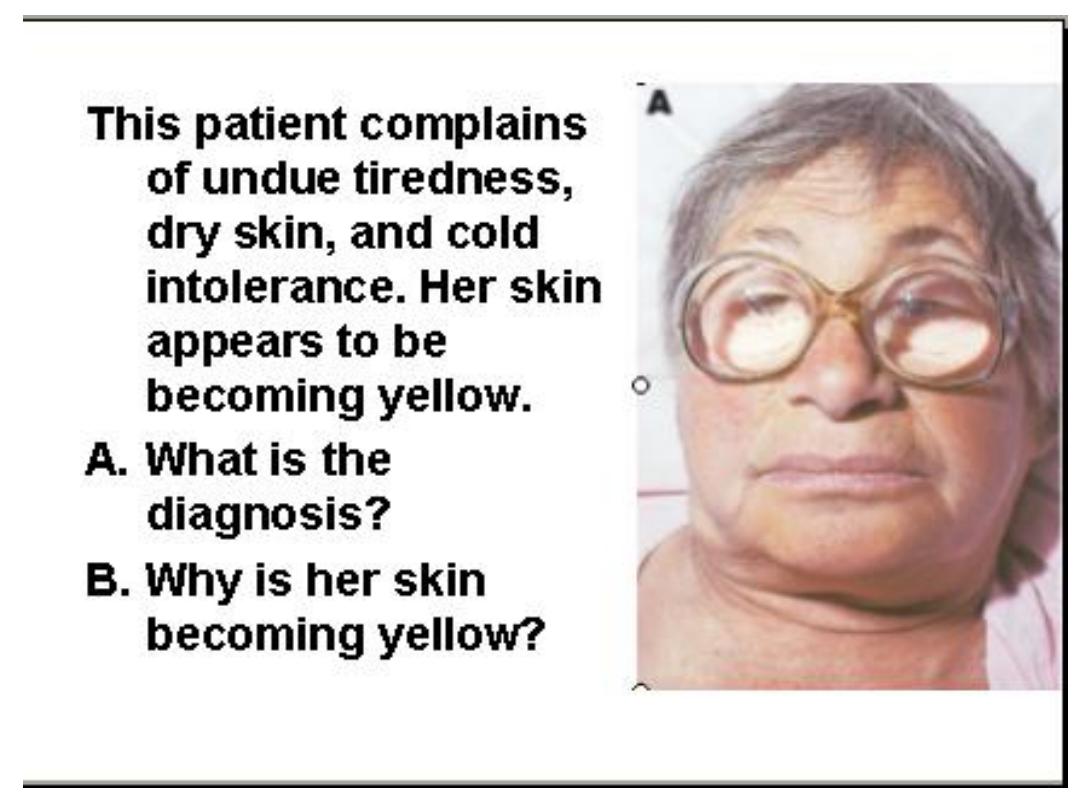

A. Hypothyroidism.
B. She is hypercarotenaemia.
B12 deficiency anaemia may be
associated.
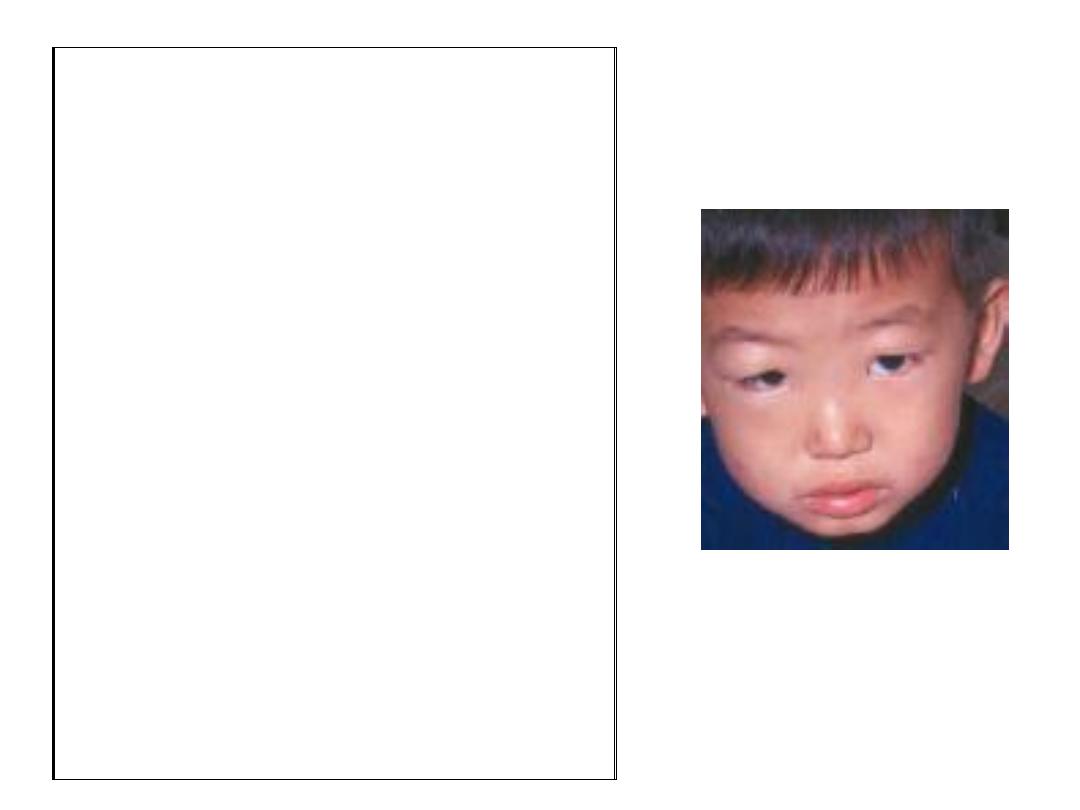
This young boy serum
calcium is low. He
does not have clinical
features of latent
tetany.
A. What is the clinical
diagnosis?
B. What is the most likely
histological finding on
biopsy of the
appropriate organ?
This young boy serum
calcium is low. He
does not have clinical
features of latent
tetany.
A. What is the clinical
diagnosis?
B. What is the most likely
histological finding on
biopsy of the
appropriate organ?
A. Nephrotic syndrome. His S. calcium
corrected for hypoalbuminaemia is
normal.
B. Minimal change glomerulonephritis on
renal biopsy.

Ascariasis
About 18-20 cm in
length. Cause
eosinophilia, cough and
other respiratory
problems in acute phase
then settle in intestine
and cause GIT
disturbances.
May causes some
complications (intestinal
obstruction,
appendicitis, biliary and
pancreatic tracts
obstruction.
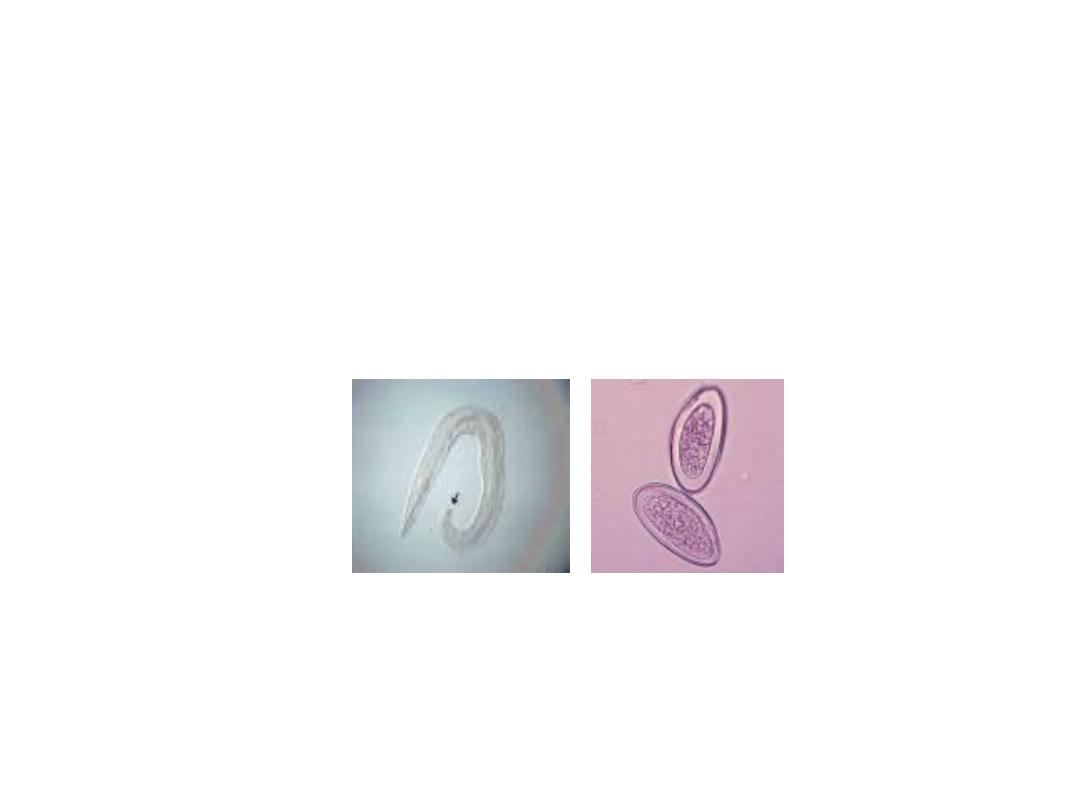
enterobiasis vermicularis
The helminth is few centimeters in length and
ova is D shaped and transparent. Causes
severe nocturnal pruritus ani especially occur
in children and may involve genital
tract.

hookworm (ancylostoma)
Mainly cause iron deficiency
anaemia
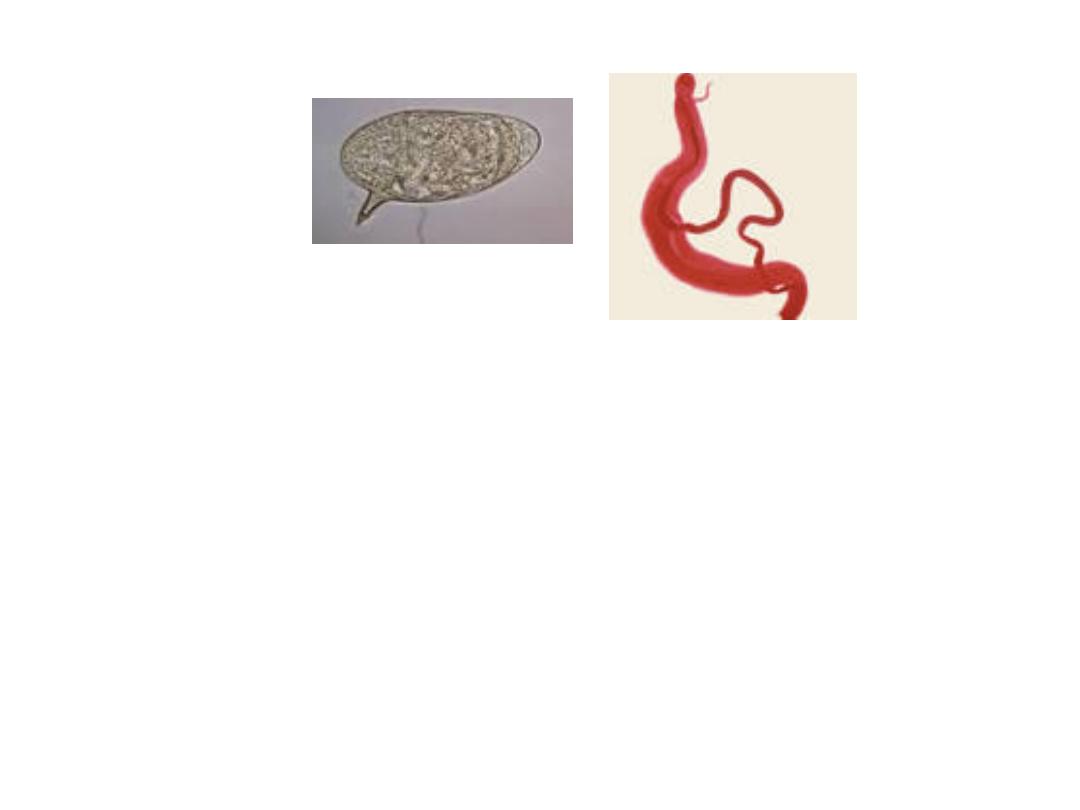
S. Mansoni: Transmission through the skin
or mucous membrane mainly cause portal
hypertension and liver fibrosis but usually
without jaundice and hepatic failure.
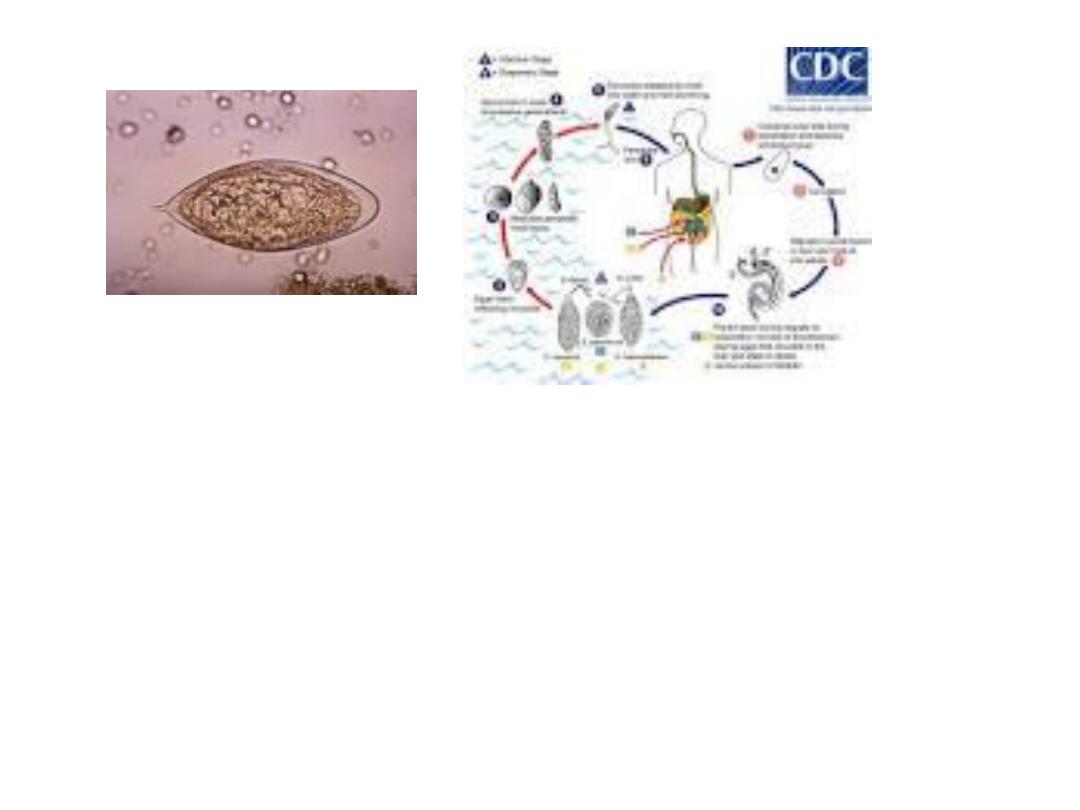
S. haematobium
Involve mainly the bladder and other part of
urinary tract, and cause terminal hematuria,
bladder fibrosis, hydronephrosis, etc. Praziquantel
in single dose is treatment of choice.
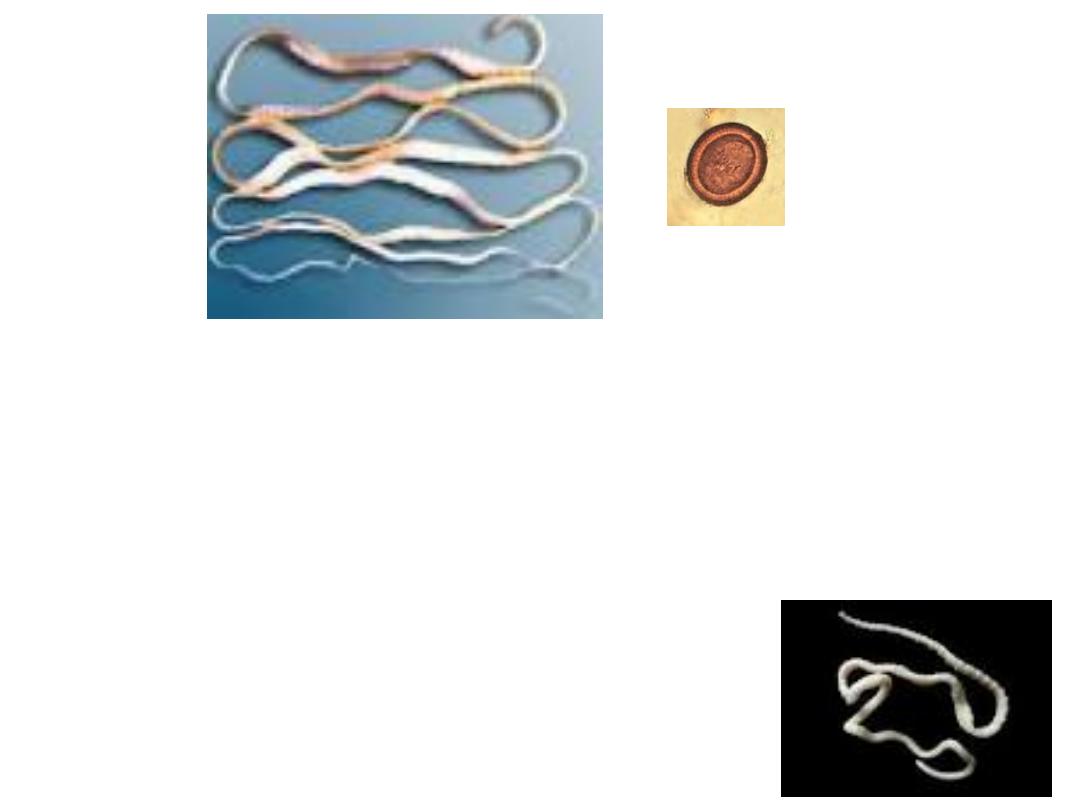
T. Saginata (Beef tapeworm): up to 20 meters in
length. No much problem. Treatment niclosamide,
albendazole and praziquantel .
Taenia solium (Pig tapeworm): Problem of larval stage
in brain and striated muscles (cysticercosis).
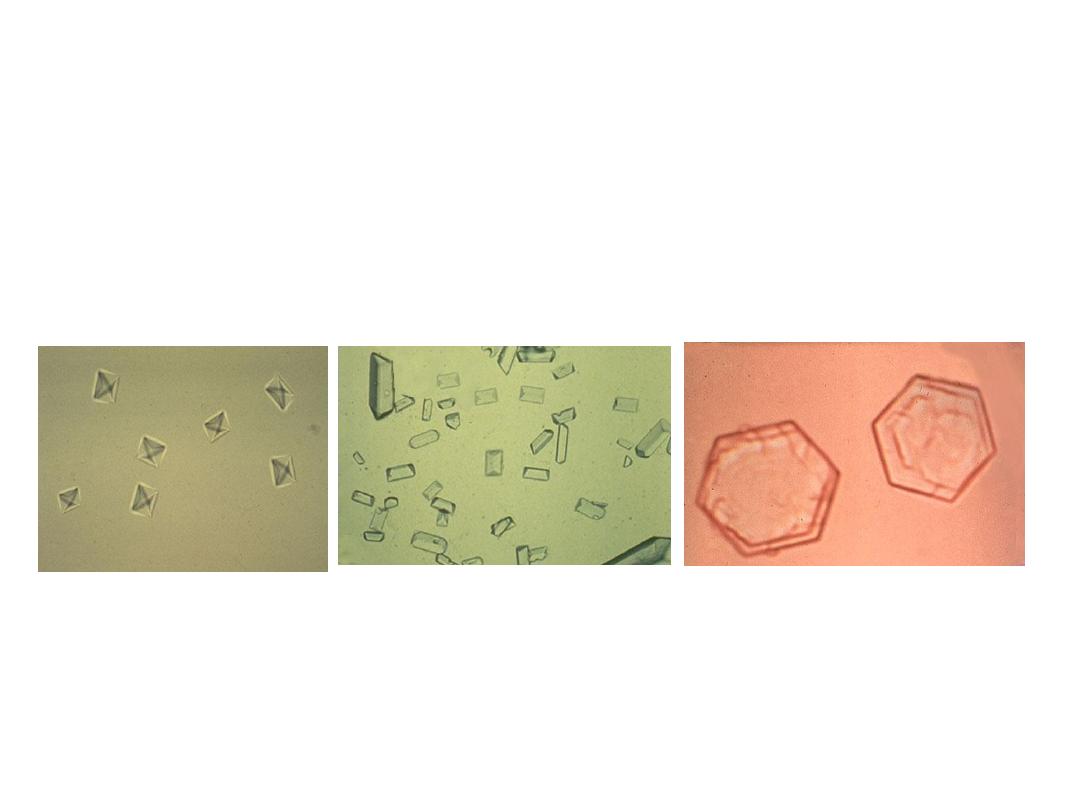
Crystals in urine
Left oxalate crystals
Middle phosphate crystals
Right: cystine crystals
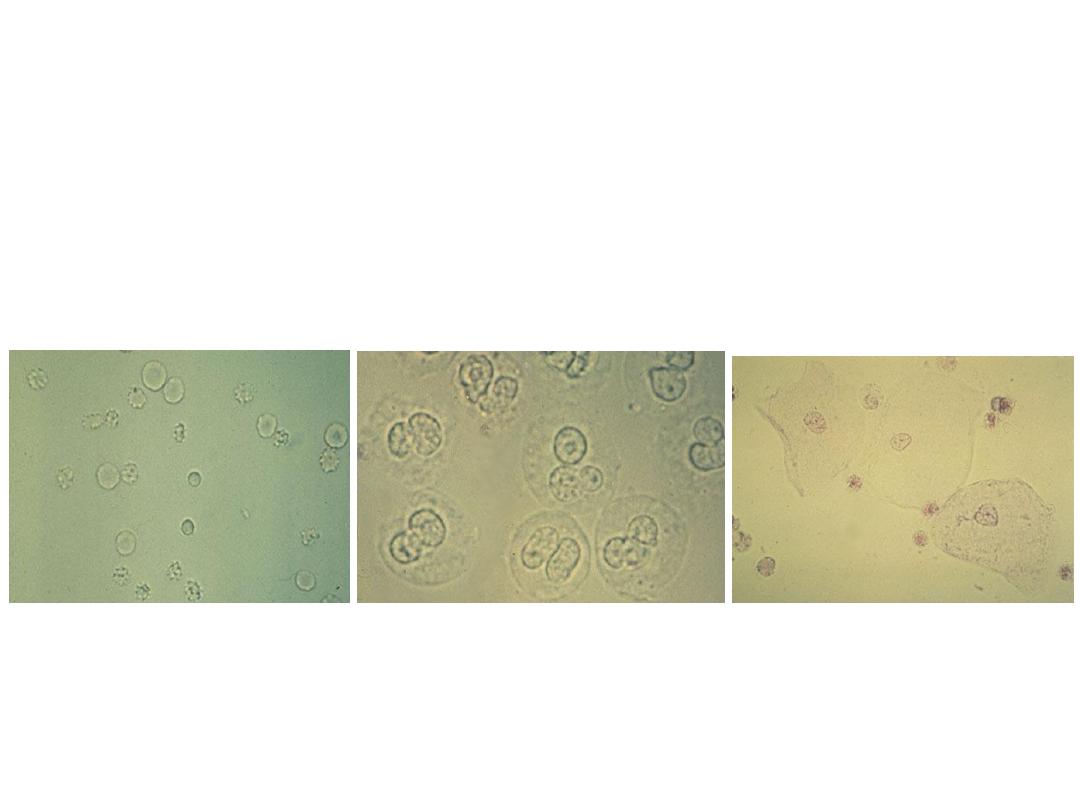
Left RBCs in urine
Middle: WBCs (pus cells) in urine
Right: Epithelial cells in urine
