
1
Fifth stage
Pediatric
Lec-1
.د
أوس
11/11/2015
Acute Gastroenteritis in Children
infections of the gastrointestinal tract caused by bacterial, viral, or parasitic pathogens
Many of these infections are foodborne illnesses
The most common manifestations are diarrhea and vomiting, which can also be
associated with systemic features such as abdominal pain and fever.
Diarrheal disorders in childhood account for a large proportion (9%) of childhood deaths,
with an estimated 0.71 million deaths per year globally,
ETIOLOGY OF DIARRHEA
Gastroenteritis is the result of infection acquired through the fecal–oral route or by
ingestion of contaminated food or water
Gastroenteritis is associated with poverty, poor environmental hygiene, and
development indices.
rotavirus and the noroviruses (small round viruses such as Norwalk-like virus and
caliciviruses) are the most common viral agents, followed by sapoviruses, enteric
adenoviruses and astroviruses
Shigella, Salmonella, E. coli, Campylobacter are examples of bacterial causes
Giardia and Entamoeba histolytica are examples of paracytic causes
PATHOGENESIS OF INFECTIOUS DIARRHEA
1- non-inflammatory diarrhea through enterotoxin production by some bacteria,
destruction of villus (surface) cells by viruses, adherence by parasites, and adherence
and/or translocation by bacteria
2- Inflammatory diarrhea is usually caused by bacteria that directly invade the intestine or
produce cytotoxins
Risk factors for diarrhea
Lack of exclusive breastfeeding (0-5 mo)
No breastfeeding (6-23 mo)
Underweight,stunted,wasted(malnourished)

2
Vitamin A deficiency
Zinc deficiency
Crowding (>8 persons/kitchen)
Indoor air pollution
Unwashed hands
Poor water quality
Inappropriate excreta disposal
Definition
Acute diarrhea is defined as the abrupt onset of 3 or more loose stools per day and lasts no
longer than 14 days
Increase frequency and/or liquidity of stool
Stool output >10 g/kg/24 hr, or more than the adult limit of 200 g/24 hr.
Rotavirus infection
typically begins after an incubation period of <48 hr with mild to moderate fever as well as
vomiting, followed by the onset of frequent, watery stools. All 3 symptoms are present in
about 50-60% of cases. Vomiting and fever typically abate during the 2nd day of illness, but
diarrhea often continues for 5-7 days. The stool is without gross blood or white blood cells.
Dehydration may develop and progress rapidly, particularly in infants. The most severe
disease typically occurs among children 4-36 mo of age. Malnourished children and children
with underlying intestinal disease, are particularly likely to acquire severe rotavirus diarrhea
Shigella
Four species of Shigella are responsible for bacillary dysentery:
S. dysenteriae
S. flexneri
S. boydii
S. sonnei
It is most common in the 2nd and 3rd year of life, infection in the 1st 6 mo of life is rare
(may be due to Breast feeding)
The colon is the target organ for shigellae

3
Symptoms:
generalized toxicity
urgency, and painful defecation characteristically occur.
watery → bloody mucoid stools
Convulsions, headache, lethargy, confusion, nuchal rigidity, or hallucinations may be
present before or after the onset of diarrhea.
Escherichia Coli
gram-negative bacilli
5 major groups of diarrheagenic E. coli:
(1) enterotoxigenic E. coli (ETEC)
(2) enteroinvasive E. coli (EIEC)
(3) enteropathogenic E. coli (EPEC)
(4) Shiga toxin–producing E. coli (STEC) also known as enterohemorrhagic E. coli (EHEC)
(5) enteroaggregative E. coli (EAEC).
Giardia Lamblia
It infects the duodenum and small intestine
Clinically: asymptomatic, acute infectious diarrhea (insidious onset of progressive anorexia,
nausea, gaseousness, abdominal distention, watery diarrhea) or chronic diarrhea with
persistent GIT signs and symptoms, including FTT and abdominal pain or cramping.
There is usually no extraintestinal spread.
Entamoeba histolytica
Clinical presentations range from asymptomatic cyst passage to amebic colitis, amebic
dysentery, ameboma, and extraintestinal disease as amebic liver disease.
Amebic colitis, gradual onset of colicky abdominal pains and frequent bowel movements
(6–8/day). Diarrhea is frequently associated with tenesmus. Stools are blood stained and
contain a fair amount of mucus with few leukocytes. Generalized constitutional symptoms
and signs are characteristically absent, with fever documented in only ⅓ of patients.
4
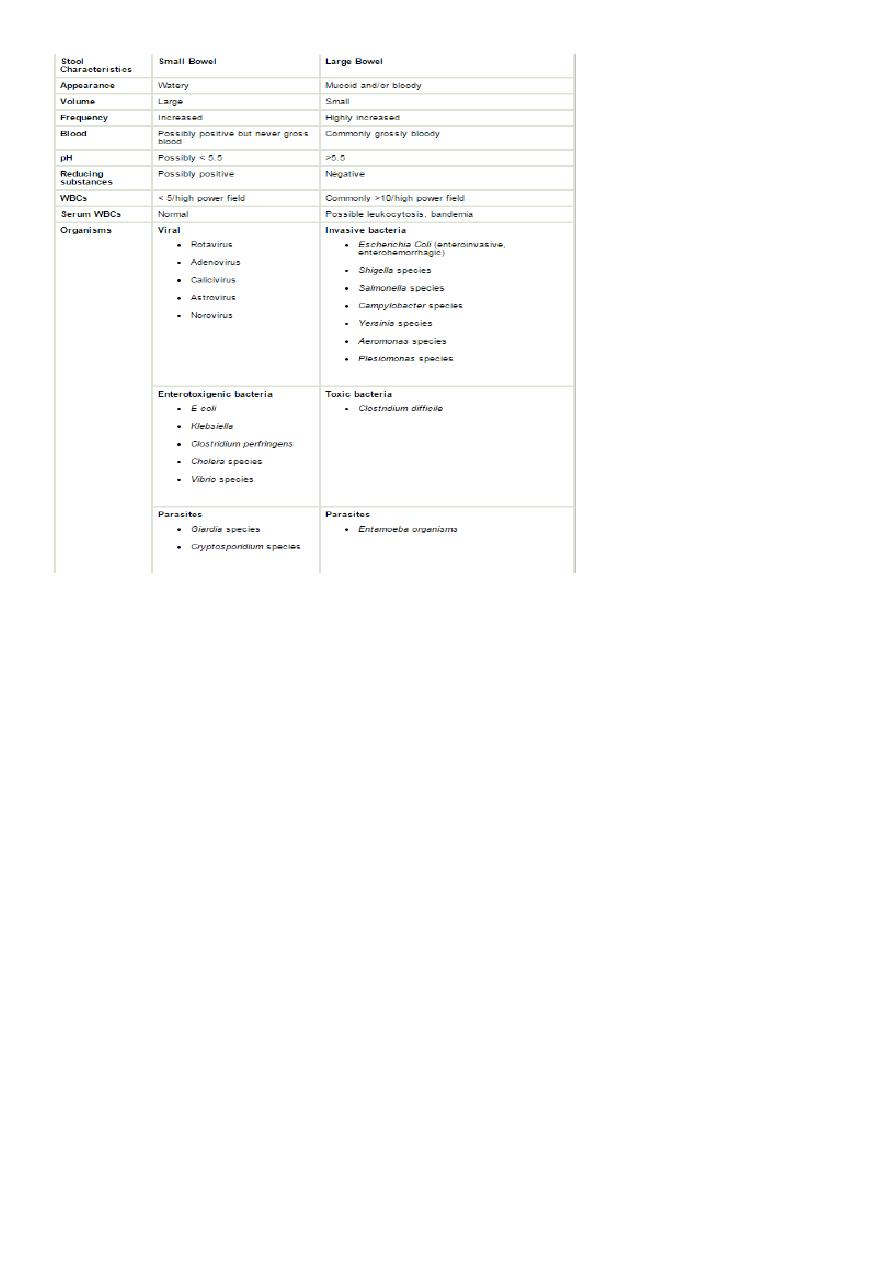
Clinical Evaluation of Diarrhea
1- Assessing the degree of dehydration and acidosis and provide rapid resuscitation and
rehydration with oral or intravenous fluids as required
2- Clinically determining the etiology of diarrhea for institution of prompt antibiotic
therapy, if indicated
Stool characteristics (eg, consistency, color, volume, frequency)
Presence of associated enteric symptoms (eg, nausea/vomiting, fever, abdominal pain)
Use of child daycare (common pathogens: rotavirus, astrovirus,
calicivirus;Campylobacter, Shigella, Giardia, and Cryptosporidium species [spp])
Food ingestion history (eg, raw/contaminated foods, food poisoning)
Water exposure (eg, swimming pools, marine environment)
Camping history (possible exposure to contaminated water sources)
Travel history (common pathogens affect specific regions; also consider rotavirus
and Shigella, Salmonella, and Campylobacter spp regardless of specific travel history, as
these organisms are prevalent worldwide)
Animal exposure (eg, young dogs/cats: Campylobacter spp; turtles:Salmonella spp)
Predisposing conditions (eg, hospitalization, antibiotic use, immunocompromised state)
Although nausea and vomiting are nonspecific symptoms, they indicate infection in the
upper intestine.
Fever suggests an inflammatory process(inflammatory diarrhea) but also occurs as a
result of dehydration or coinfection (e.g., urinary tract infection, otitis media)called
also parenteral diarrhea(etiology outside the G.I system)
Severe abdominal pain, tenesmus and bloody diarrhoea indicate involvement of the
large intestine and rectum.
Features such as nausea and vomiting and absent or low-grade fever with mild to
moderate periumbilical pain and watery diarrhea indicate small intestine involvement and
also reduce the likelihood of a serious bacterial infection.
5
InvestigationS
1-Stool Examination
A-Microscopic examination of the stool: Fecal leukocytes and RBC indicate bacterial
invasion of colonic mucosa, stool microscopy must include examination for parasites
causing diarrhea, such as G. lamblia and E. histolytica
B- Stool culture is required if the child appears septic, if there is blood or mucus in the
stools or the child is immunocompromised.It may be indicated following recent foreign
travel, if the diarrhoea has not improved by day 7 or the diagnosis is uncertain
3- Plasma electrolytes, urea, creatinine and glucose should be checked if intravenous fluids
are required or there are features suggestive of hypernatraemia.
4- If antibiotics are started, a blood culture should be taken.
5- urinalysis to exclude UTI (parenteral diarrhea)
6- Enzyme immunoassay for rotavirus or adenovirus antigens

6
BLOODY DIARRHEA
Causes of bloody diarrhoea (real or apparent) in infants and children Infants aged <1 year
1- Intestinal infection(shigella,salmonella,E-coli,campylobacter,Yersinia)
And Entamoeba histolytica
2- Infant colitis(Cow’s milk colitis)—non specific allergic colitis
3- rare causes like Intussusception, Malrotation and volvulus
Infants aged >1 year
1- Intestinal infection
2- Inflammatory bowel disease
3- Juvenile polyp
4- rare causes Intussusception , Malrotation and volvulus and Henoch-Schönlein purpura
Recent antibiotic use raises suspicion for antibiotic-associated colitis and Clostridium
difficile colitis.
