1
Fifth stage
Medicine
Lec-9
د.بشار
15/12/2015
Intracerebral hemorrhage
Intracerebral hemorrhage is focal bleeding from a blood vessel in the brain parenchyma.
The cause is usually hypertension. Typical symptoms include focal neurologic deficits, often
with abrupt onset of headache, nausea, and impairment of consciousness. Most
intracerebral hemorrhages occur in the basal ganglia, cerebral lobes, cerebellum, or pons.
Intracerebral hemorrhage may also occur in other parts of the brain stem or in the
midbrain.
Etiology
Intracerebral hemorrhage usually results from rupture of an arteriosclerotic small artery
that has been weakened, primarily by chronic arterial hypertension. Such hemorrhages are
usually large, single, and catastrophic. Other modifiable risk factors that contribute to
arteriosclerotic hypertensive intracerebral hemorrhages include cigarette smoking, obesity,
and a high-risk diet (eg, high in saturated fats, trans fats, and calories). Use of cocaine or,
occasionally, other sympathomimetic drugs can cause transient severe hypertension
leading to hemorrhage.
Less often, intracerebral hemorrhage results from congenital aneurysm, arteriovenous or
other vascular malformation ,trauma , mycotic aneurysm, brain infarct (hemorrhagic
infarction), primary or metastatic brain tumor, excessive anticoagulation, blood dyscrasia,
intracranial arterial dissection, moyamoya disease, or a bleeding or vasculitic disorder.
لالطالع فقط
Vascular Lesions in the Brain
Common brain vascular lesions include
arteriovenous malformations and
aneurysms.
Arteriovenous malformations
(AVMs):AVMs are tangled, dilated blood
vessels in which arteries flow directly into
veins. AVMs occur most often at the
junction of cerebral arteries, usually within
the parenchyma of the frontal-parietal
region, frontal lobe, lateral cerebellum, or
overlying occipital lobe. AVMs also can
occur within the dura. AVMs can bleed or
directly compress brain tissue; seizures or
ischemia may result.
Many aneurysms are
asymptomatic, but a few cause
symptoms by compressing adjacent
structures. Ocular palsies, diplopia,
squint, or orbital pain may indicate
pressure on the 3rd, 4th, 5th, or 6th
cranial nerves. Visual loss and a
bitemporal field defect may
indicate pressure on the optic
chiasm. Aneurysms may bleed into
the subarachnoid space, causing
subarachnoid hemorrhage. Before
rupture, aneurysms occasionally
cause sentinel (warning) headaches
due to painful expansion of the
aneurysm or to blood leaking into
2
Neuroimaging may detect them incidentally;
contrast or noncontrast CT can usually
detect AVMs > 1 cm, but the diagnosis is
confirmed with MRI. Occasionally, a cranial
bruit suggests an AVM. Conventional
angiography is required for definitive
diagnosis and determination of whether the
lesion is operable.
Superficial AVMs > 3 cm in diameter are
usually obliterated by a combination of
microsurgery, radiosurgery, and
endovascular surgery. AVMs that are deep
or < 3 cm in diameter are treated with
stereotactic radiosurgery, endovascular
therapy (eg, preresection embolization or
thrombosis via an intra-arterial catheter), or
coagulation with focused proton beam.
Aneurysms: Aneurysms are focal dilations in
arteries. They occur in about 5% of people.
Common contributing factors may include
arteriosclerosis, hypertension, and
hereditary connective tissue disorders (eg,
Ehlers-Danlos syndrome, pseudoxanthoma
elasticum, autosomal dominant polycystic
kidney syndrome). Occasionally, septic
emboli cause mycotic aneurysms. Brain
aneurysms are most often < 2.5 cm in
diameter and saccular (noncircumferential);
sometimes they have one or more small,
thin-walled, outpouchings (berry aneurysm).
Most aneurysms occur along the middle or
anterior cerebral arteries or the
communicating branches of the circle of
Willis, particularly at arterial bifurcations.
Mycotic aneurysms usually develop distal to
the first bifurcation of the arterial branches
of the circle of Willis.
the subarachnoid space. Actual
rupture causes a sudden severe
headache called a thunderclap
headache.
Neuroimaging may detect
aneurysms incidentally.
Diagnosis requires angiography, CT
angiography, or magnetic
resonance angiography.
If < 7 mm, asymptomatic aneurysms
in the anterior circulation rarely
rupture and do not warrant the
risks of immediate treatment. They
can be monitored with serial
imaging. If aneurysms are larger,
are in the posterior circulation, or
cause symptoms due to bleeding or
due to compression of neural
structures, endovascular therapy, if
feasible, can be tried
Lobar intracerebral hemorrhages (hematomas in the cerebral lobes, outside the basal
ganglia) usually result from angiopathy due to amyloid deposition in cerebral arteries
(cerebral amyloid angiopathy), which affects primarily the elderly. Lobar hemorrhages may
be multiple and recurrent.

3
Pathophysiology
Blood from an intracerebral hemorrhage accumulates as a mass that can dissect through
and compress adjacent brain tissues, causing neuronal dysfunction. Large hematomas
increase intracranial pressure. Pressure from supratentorial hematomas and the
accompanying edema may cause transtentorial brain herniation, compressing the brain
stem and often causing secondary hemorrhages in the midbrain and pons. If the
hemorrhage ruptures into the ventricular system (intraventricular hemorrhage), blood may
cause acute hydrocephalus. Cerebellar hematomas can expand to block the 4th ventricle,
also causing acute hydrocephalus, or they can dissect into the brain stem. Cerebellar
hematomas that are > 3 cm in diameter may cause midline shift or herniation. Herniation,
midbrain or pontine hemorrhage, intraventricular hemorrhage, acute hydrocephalus, or
dissection into the brain stem can impair consciousness and cause coma and death.
نهاية لالطالع فقط
Symptoms and Signs
Symptoms typically begin with sudden headache, often during activity. However, headache
may be mild or absent in the elderly. Loss of consciousness is common, often within
seconds or a few minutes. Nausea, vomiting, delirium, and focal or generalized seizures are
also common. Neurologic deficits are usually sudden and progressive. Large hemorrhages,
when located in the hemispheres, cause hemiparesis; when located in the posterior fossa,
they cause cerebellar or brain stem deficits (eg, conjugate eye deviation or
ophthalmoplegia, stertorous breathing, pinpoint pupils, coma). Large hemorrhages are fatal
within a few days in about half of patients. In survivors, consciousness returns and
neurologic deficits gradually diminish to various degrees as the extravasated blood is
resorbed. Some patients have surprisingly few neurologic deficits because hemorrhage is
less destructive to brain tissue than infarction.
Small hemorrhages may cause focal deficits without impairment of consciousness and with
minimal or no headache and nausea. Small hemorrhages may mimic ischemic stroke.
Diagnosis
Neuroimaging
Diagnosis is suggested by sudden onset of headache, focal neurologic deficits, and impaired
consciousness, particularly in patients with risk factors. Intracerebral hemorrhage must be
distinguished from ischemic stroke, subarachnoid hemorrhage, and other causes of acute
neurologic deficits (eg, seizure, hypoglycemia); blood glucose level should be measured at
the bedside immediately.
Immediate CT or MRI is necessary. Neuroimaging is usually diagnostic. If neuroimaging
shows no hemorrhage but subarachnoid hemorrhage is suspected clinically, lumbar
puncture is necessary .CT angiography, done within hours of bleeding onset, may show
areas where contrast extravasates into the clot (spot sign); this finding indicates that
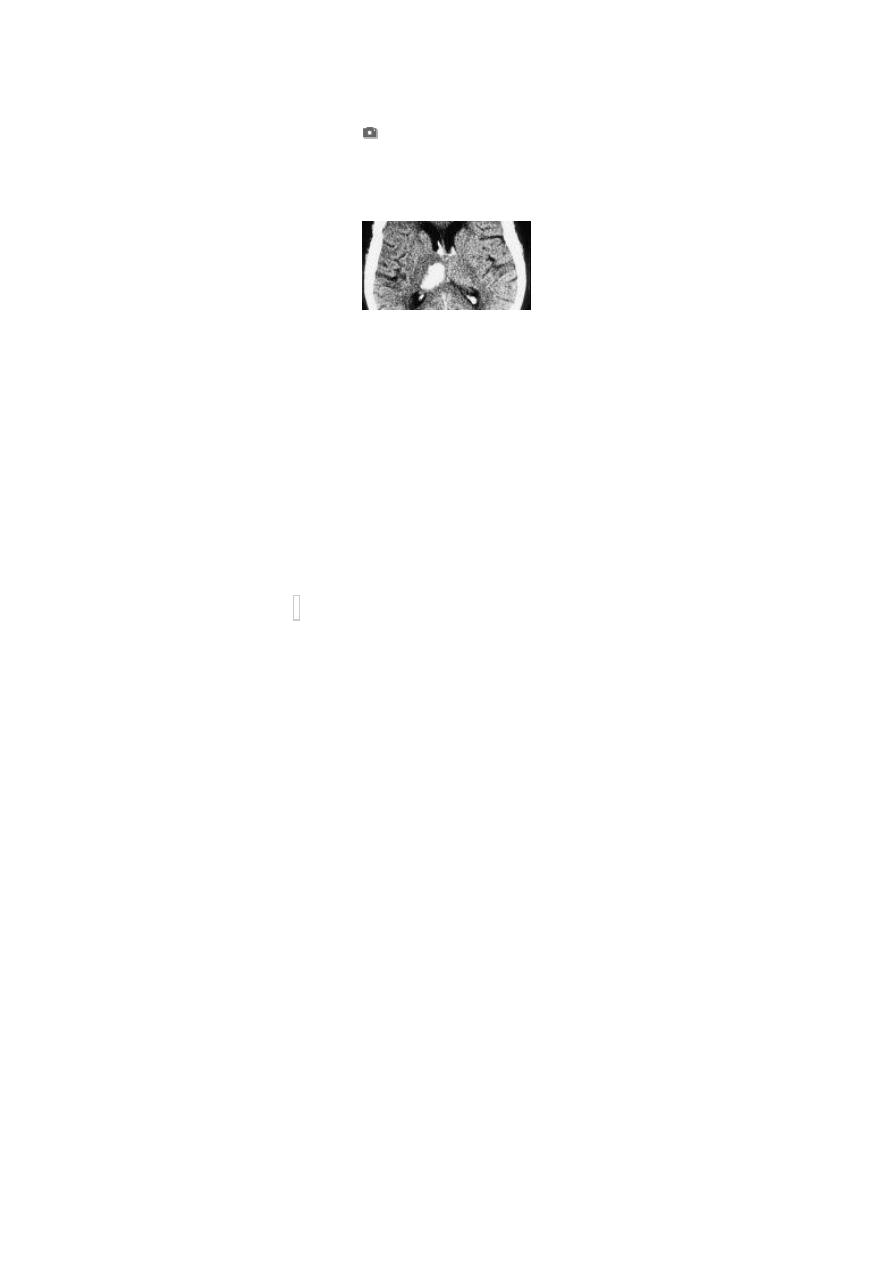
4
bleeding is continuing and suggests that the hematoma will expand and the outcome will
be poor .
Treatment
Supportive measures
Sometimes surgical evacuation (eg, for many cerebellar hematomas >3 cm)
Treatment includes supportive measures and control of modifiable risk factors.
Anticoagulants and antiplatelet drugs are contraindicated. If patients have used
anticoagulants, the effects are reversed when possible by giving fresh frozen plasma,
prothrombin complex concentrate, vitamin K, or platelet transfusions as indicated.
Hemodialysis can remove about 60% of dabigatran.
Hypertension should be treated only if mean arterial pressure is > 130 mm Hg or systolic BP
is > 185 mm Hg. Nicardipine
2.5 mg/h IV is given initially; dose is increased by 2.5 mg/h q 5
min to a maximum of 15 mg/h as needed to decrease systolic BP by 10 to 15%.
Cerebellar hemisphere hematomas that are > 3 cm in diameter may cause midline shift or
herniation, so surgical evacuation is often lifesaving. Early evacuation of large lobar cerebral
hematomas may also be lifesaving, but rebleeding occurs frequently, sometimes increasing
neurologic deficits. Early evacuation of deep cerebral hematomas is seldom indicated
because surgical mortality is high and neurologic deficits are usually severe. Anticonvulsants
are not typically used prophylactically; they are used only if patients have had a seizure.
