1
Fifth stage
Medicine
Lec-2
.د
فاخر
27/10/2015
Investigations in Rheumatology
Image study
Plain radiography
X-rays can show anatomical changes that reflect important pathological processes Although
most changes have low specificity, combinations of features and targeting of certain bones
or joints result in characteristic patterns that have high diagnostic specificity.
Joints to be X-rayed are usually selected on the basis
of involvement identified at clinical assessment. ]

2
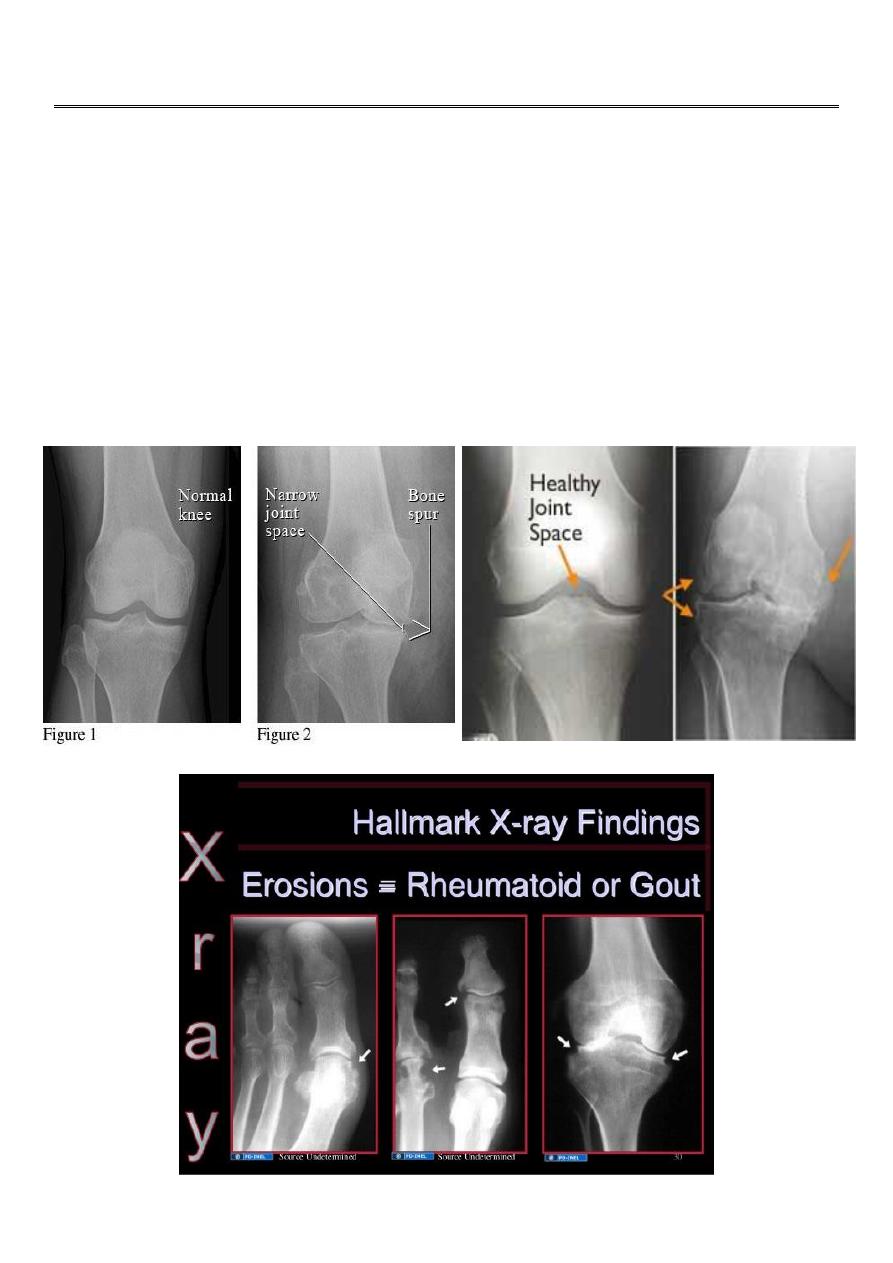
Erosions
Cartilage and bone erosion is a hallmark of major inflammatory arthropathies. Intracapsular
bone erosion first occurs at the joint margin (‘marginal erosion’) where bone is exposed
directly to inflammatory synovium without the protection of overlying cartilage. Loss of the
sharp cortical line is the first radiographic sign and precedes more definite scalloping of the
bony contour Cartilage erosion also starts at the margin and slowly works centrally,
resulting in loss of ‘joint space’.
Both RA and seronegative spondyloarthritis (especially psoriatic arthritis) can cause
marginal erosions. In RA there is no bone or periosteal reaction, resulting in atrophic ‘non-
proliferative’ erosions often with juxta-articular osteopenia and soft tissue swelling. By
contrast, in seronegative spondyloarthritis new bone formation and periosteal reaction
with retained bone density are more common, resulting in ‘proliferative’ erosions
.Accompanying ossifying enthesopathy
In the first 1–2 weeks of acute septic arthritis the Xray is often normal, apart from
osteopenia and soft tissue swelling. However, erosion proceeds rapidly and results in
generalised loss of joint space with loss of cortical integrity centrally (central erosion) as
well as marginally.
In chronic gout, bony defects develop slowly as massive crystal deposits (‘tophi’) cause
pressure necrosis to surrounding bone. Such ‘pressure erosions’ .occur at extracapsular as
well as intracapsular sites .
Calcification
Calcification of fibrocartilage and hyaline cartilage (chondrocalcinosis) is most commonly
due to calcium pyrophosphate crystals. Calcification at extracapsular sites is mainly apatite.
Spotty, multiple calcifications of soft tissues (calcinosis) mainly target peripheral and
intermediate sites such as finger pulps, wrists and forearms, and are a feature of connective
tissue disease.
Radionuclide bone scan
This is a useful investigation in patients who have bone pain. It involves gamma-camera
imaging following an intravenous injection of 99mTc-bisphosphonate. Early post-injection
images reflect vascularity and can show increased perfusion of inflamed synovium, Pagetic
bone, or primary or secondary bone tumours Delayed images taken a few hours later

3
reflect bone remodelling as the bisphosphonate localises to sites of active bone turnover.
Scintigraphy has a high sensitivity for detecting important bone and joint pathology that is
Computerised tomography (CT) and magnetic resonance imaging (MRI)
These techniques give detailed information on anatomy, allowing three-dimensional
visualisation of anatomically complex structures such as the spinal canal and facet joints
which may be inadequately assessed by plain X-rays.
Drawbacks of CT are limited soft tissue resolution and a high radiation dose, and MRI is
frequently preferred.
It provides detailed information on both structure and physiology of cartilage, bone and
other locomotor tissues,
Ultrasonography
Ultrasonography is inferior to CT or MRI for definition of deep structures and abnormalities
within bone, but is a useful outpatient investigation for confirmation of small joint
synovitis/erosion, for anatomical confirmation of periarticular lesions, and for assistance in
guiding
DEXA
Bone mineral density
Measurement of bone mineral density (BMD) plays a pivotal role in the investigation and
management of osteoporosis. The investigation .of choice is dual energy
X-ray absorptiometry (DEXA) of the spine and hip.
Blood tests
C-reactive protein (CRP)and erythrocyte sedimentation rate (ESR)
Infections, inflammation and malignancy can trigger an acute phase response (APR) with
alterations in C-reactive
protein and erythrocyte sedimentation rate CRP is the single most useful marker of the
APR..

4
Full blood count
Changes in the FBC can occur in inflammatory rheumatic diseases but are non-specific (e.g.
neutrophilia in vasculitis,acute gout and sepsis;
neutropenia in lupus). Many disease-modifying antirheumatic drugs (DMARDs)
have marrow toxicity and require regular monitoring of the FBC.
Autoantibodies
Autoantibody tests are a useful adjunct to clinical evaluation in the diagnosis of rheumatic
diseases but false positive results are common. Those most commonly used in
rheumatology are described below; antiphospholipid antibodies, which occur in systemic
lupus erythematosus
Rheumatoid factor
Rheumatoid factor (RF) is an antibody directed against the Fc fragment of human IgG and
was so named because it was first identified in patients with RA. RFs may be of any
immunoglobulin class but IgM is most commonly tested. RF also occurs in a wide variety of
other conditions and in some normal adults it therefore has low diagnostic specificity for RA
and also lacks sensitivity, since about 30% of patients with typical signs of RA are negative
for RF (so-called seronegative RA). The principal use of RF testing is for prognosis, since a
high RF titre at presentation associates with more severe disease.
Antibodies to cyclic citrullinated peptides (anti-CCP antibodies)
Anti-CCP antibodies bind to peptides in which the amino acid arginine has been converted
to citrulline by peptidylarginine deiminase, an enzyme abundant in inflamed synovium.
They have similar sensitivity to RF for RA (70%) but much higher specificity (> 95%).
Antinuclear antibodies (ANA)
These are directed against one or more components of the nucleus. gives the many causes
of a positive ANA. Low titre ANA is common in normal individuals.
The higher the ANA titre, the greater its diagnostic significance, but high titres do not imply
more severe disease.
The most common indication for ANA testing is in the diagnosis of SLE. ANA has high
sensitivity for SLE (virtually 100%) but low specificity (10–40%); a negative

5
ANA virtually excludes SLE but a positive result does not confirm it.
(p-ANCA). c-ANCA are associated with antibodies to proteinase-3 (PR3), and occur in > 90%
of patients with Wegener’s granulomatosis with renal involvement. antibodies, is
associated with microscopic polyarteritis and Churg–Strauss vasculitis
Biochemistry
Routine biochemistry is useful in the assessment of metabolic bone disease, muscle
diseases and gout. Serum levels of uric acid are usually raised in gout but a normal level
does not exclude the diagnosis .
Serum creatinine kinase (CK) levels are useful in the diagnosis of myopathy or myositis,
Several bone diseases, including Paget’s disease, renal bone disease and osteomalacia give
a characteristic pattern on biochemical testing which can be useful diagnostically The best
markers of bone resorption are N-telopeptide (NTX) and C-telopeptide (CTX)
Joint aspiration
Joint aspiration with examination of synovial fluid (SF) is pivotal in patients suspected of
having septic arthritis,
crystal arthritis or intra-articular bleeding. It should be done in all patients with acute
monoarthritis, and samples sent for microbiology and clinical chemistry
Tissue sampling
Bone biopsy is helpful in the differential diagnosis of bone diseases when less invasive tests
have proved inconclusive. If a systemic disease is suspected, the biopsy should be taken
from the iliac crest using a large diameter (8 mm) trephine needle under local anaesthetic.
Synovial biopsy may be required in patients with chronic inflammatory monoarthritis or
tenosynovitis to identify specific causes such as chronic mycobacterial infection or
pigmented villonodular synovitis
It may be obtained arthroscopically or using ultrasound guidance under local anaesthetic.
Muscle biopsy is useful in the investigation of myopathy, myositis and systemic vasculitis
