1
Fifth stage
Medicine
Lec-2
د.خالد نافع
17/11/2015
IRON deficiency anemia
Iron in the body is used primarily for the synthesis of Hemoglobin and normal
erythropoiesis requires 20-25 mg of iron per day.
Requirements for exogenous iron
All iron required for red cell production is acquired through the recycling of iron extracts
from the senescent red cells.
Only 5% of the iron needed for erythropoiesis, or 1 mg /d, is absorbed from GIT to balance
losses in the urine, stool, sweat , and de-sequamated skin
IRON STORAGE
Two different configurations
:
Ferritin : water soluble, hydroxyl iron, & protein (Apoprotein
Hemosiderin : insoluble Aggregate of ferritin molecules that have been stripped of
apoprotein.
2
Metabolic pathway of IRON
Phagocytic macrophages in the liver, spleen, BM take RBC that have complete their 120-day
life span. Hemoglobin is broken down into its constituents and iron is stored as ferritin or
hemosiderin.
Erythroid precursors in the marrow develop around the macrophages and take up the
ferritin .
Macrophages in the marrow and spleen remove excess ferritin and hemosiderin.
Transferrin mediate iron transport from macrophages and gastro-intestinal mucosa to the
immature RBC and for storage in the liver
Iron transport
Transferrin is the principle means for moving iron and is a transport protein with two iron
binding site. transferrin picks up iron from the mucosal cells of the intestine then deliver
iron to receptors on surface of nucleated RBCs and reticulocytes .the macrophages then
transport the iron-free transferrin back to the place
.
The amount of transferrin in the serum is measured directly as the total iron binding
capacity(TIBC).
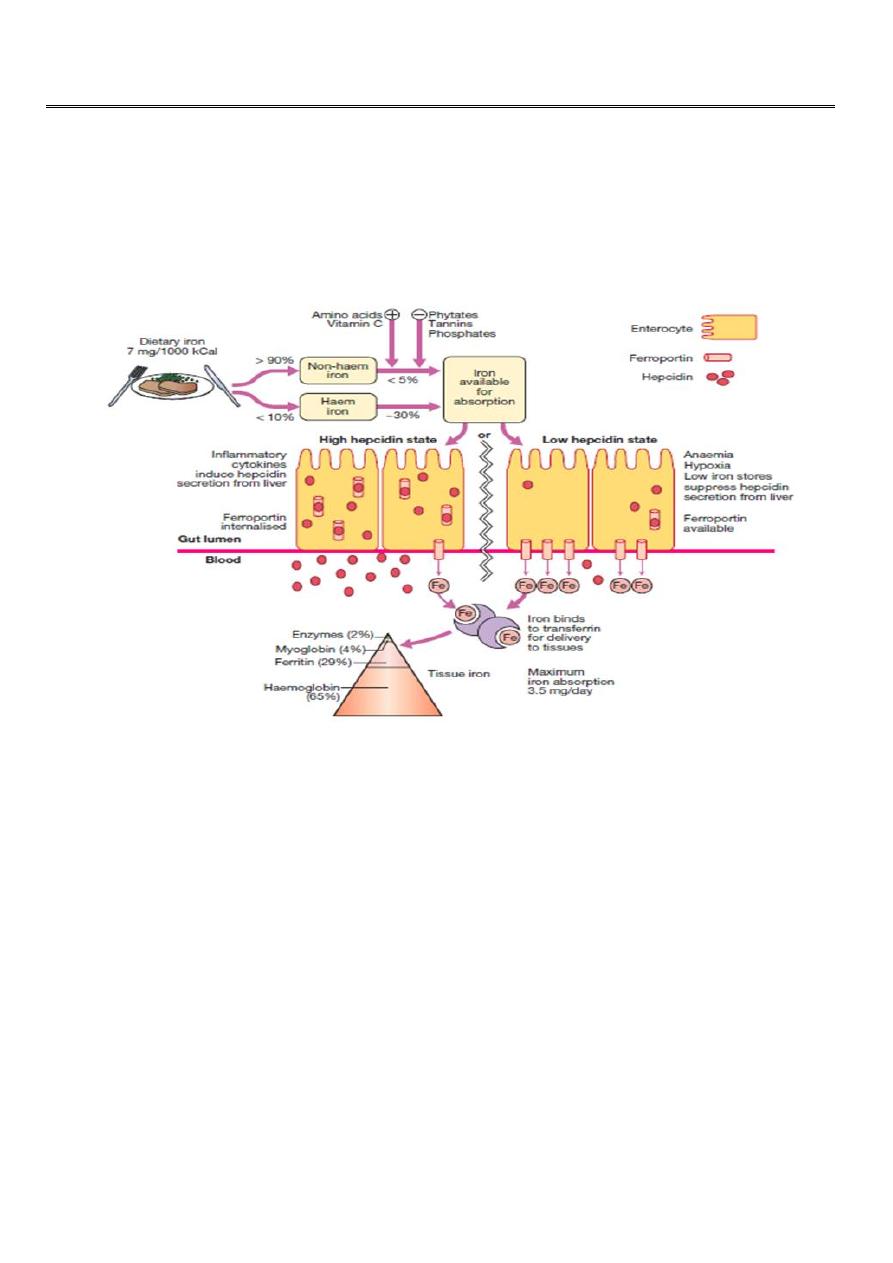
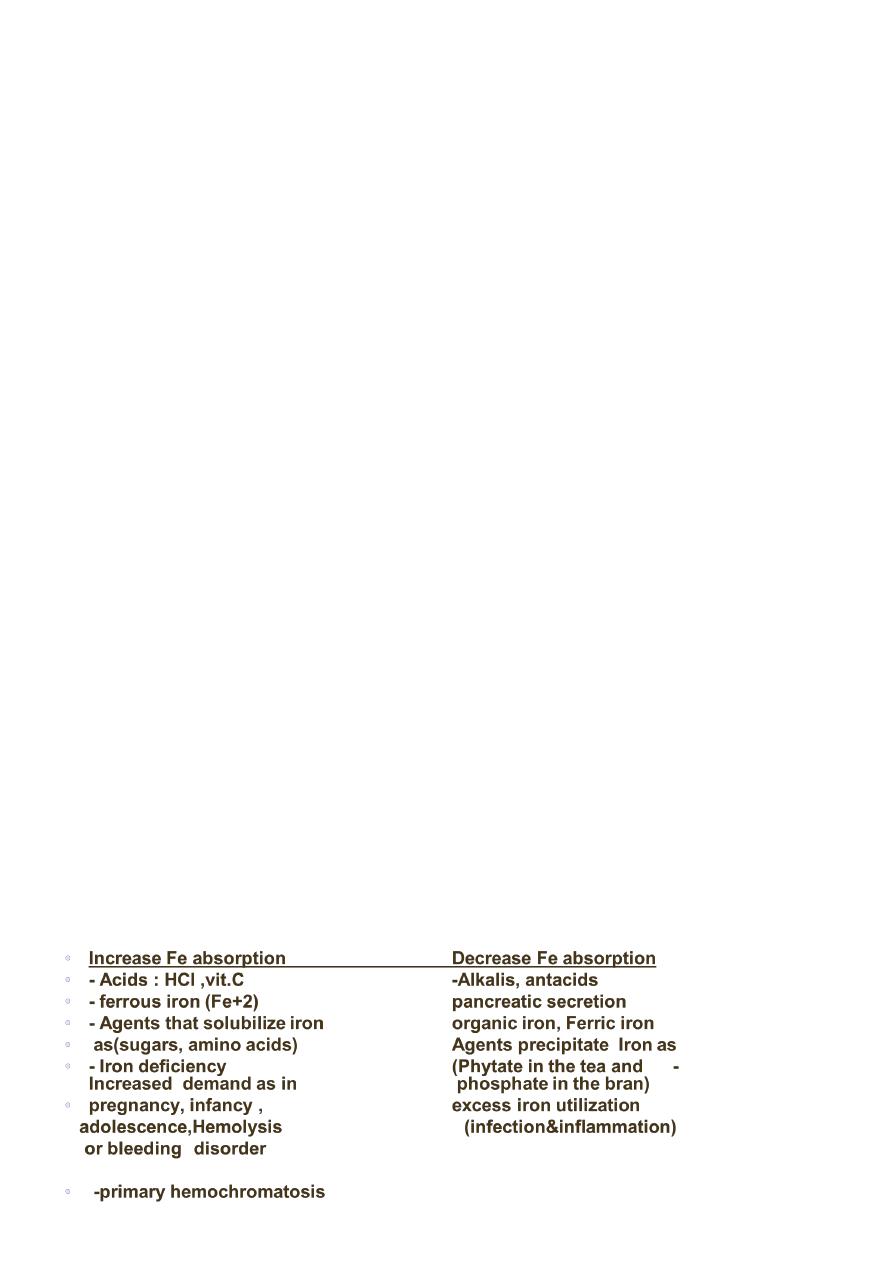
Iron Absorption
Absorption sites : maximal absorption occur in the duodenum and upper jejunum .
The acidic gastric juice reduces insoluble ferric iron to its soluble ferrous state.
Factors influence iron absorption
3
IRON DEFICIENCY ANAEMIA (Ida)
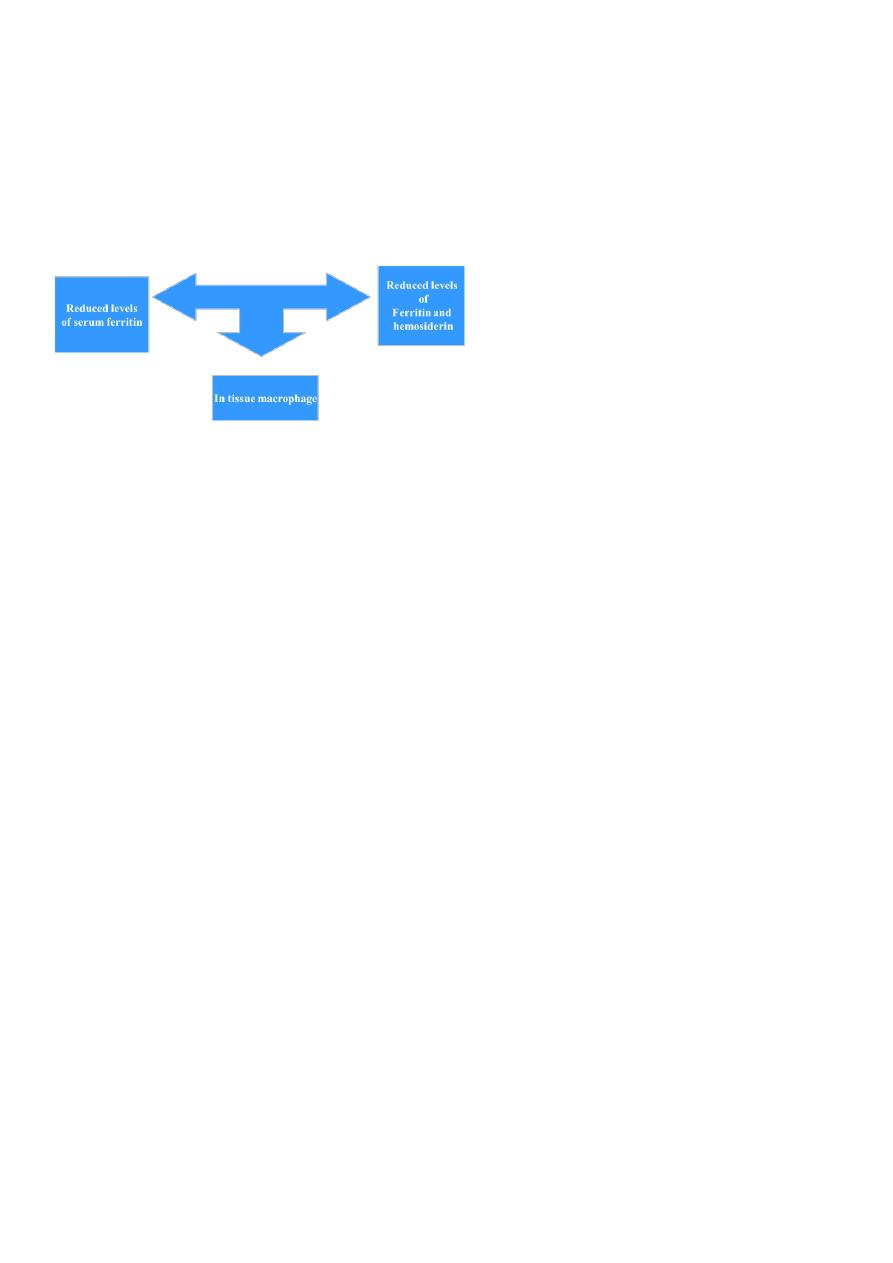
Stages of iron deficiency
a. Depletion of tissue iron.
in negative iron balance, and to preserve the level of iron in the serum and RBC, results in
Depleting the tissue iron stores and this results in:
b. Changes in serum iron are indicative of depletion of the iron stores:
Serum iron are usually low.
TIBC increase .
c. Progressive anaemia
:
initially normochronic, normocytic
eventually hypochromic, microcytic
tissue changes occur.
CAUSES OF IRON DEFICIENCY
Chronic blood loss:
uterine blood loss.
GIT blood loss .
Benign conditions:
o peptic ulcer.
o esophageal varicies.
o hiatus hernia.
o colonic diverticula or polyp.
o hemorrhoids.
o chronic aspirin use.
o Parasites (hook worm(
Malignancy:
4
o colonic ;colorectal Ca.
o Gastric Ca.
o Esophageal Ca.
o small intestinal Ca
pulmonary accumulation lead to hemosiderosis.
urinary tract:
o Hypernephroma
o Bladder Ca.
o paroxysmal nocturnal hemoglobinuria (PNH(
Increase iron requirement
Iron malabsorption
Poor diet
SYMPTOMS OF IRON DEFICIENCY
Symptoms and signs pertaining to anemia:
Non-specific symptoms: fatigue, weakness , dyspnoea, symptoms of CHF
Signs: Pallor, tachycardia, splenomegaly (minority of cases
Symptoms and signs specific to iron deficiency:
Atrophic changes in the epithelium results from levels of heme-containing enzymes
(cytochrome, succinate dehydrogenase, catalase, peroxidase, xanthine oxidase(
Oral lesions:
Angular cheilosis
Atrophy of the tongue papilla with intermittent glossitis, and stomatitis.
Dysphagia: post-cricoid esophageal webbing (Plummer Vinson syndrome.)
Nail lesions: (Koilonychias) Flattening, thinning lead to brittle, spoon- shaped nail .
Pica:
Compulsive ingestion of non nutritive substances.
Children craving for & ingestion of clay, dirt, paint
Adult: to eat ice (pagophagia) clay.

5
DIAGNOSIS
Laboratory studies: a. peripheral blood
:
RBC indices:
MCV (55-74 fl(
MCH (25-30 g/dL(
RDW > 16
Peripheral blood smears:
microcytic hypochromic
poikilocyte = abnormally shaped RBCs .
Anisocyte = vary in size of RBCs.
Blood count:
normal or low reticulocytes
occasionally high platelet count
6
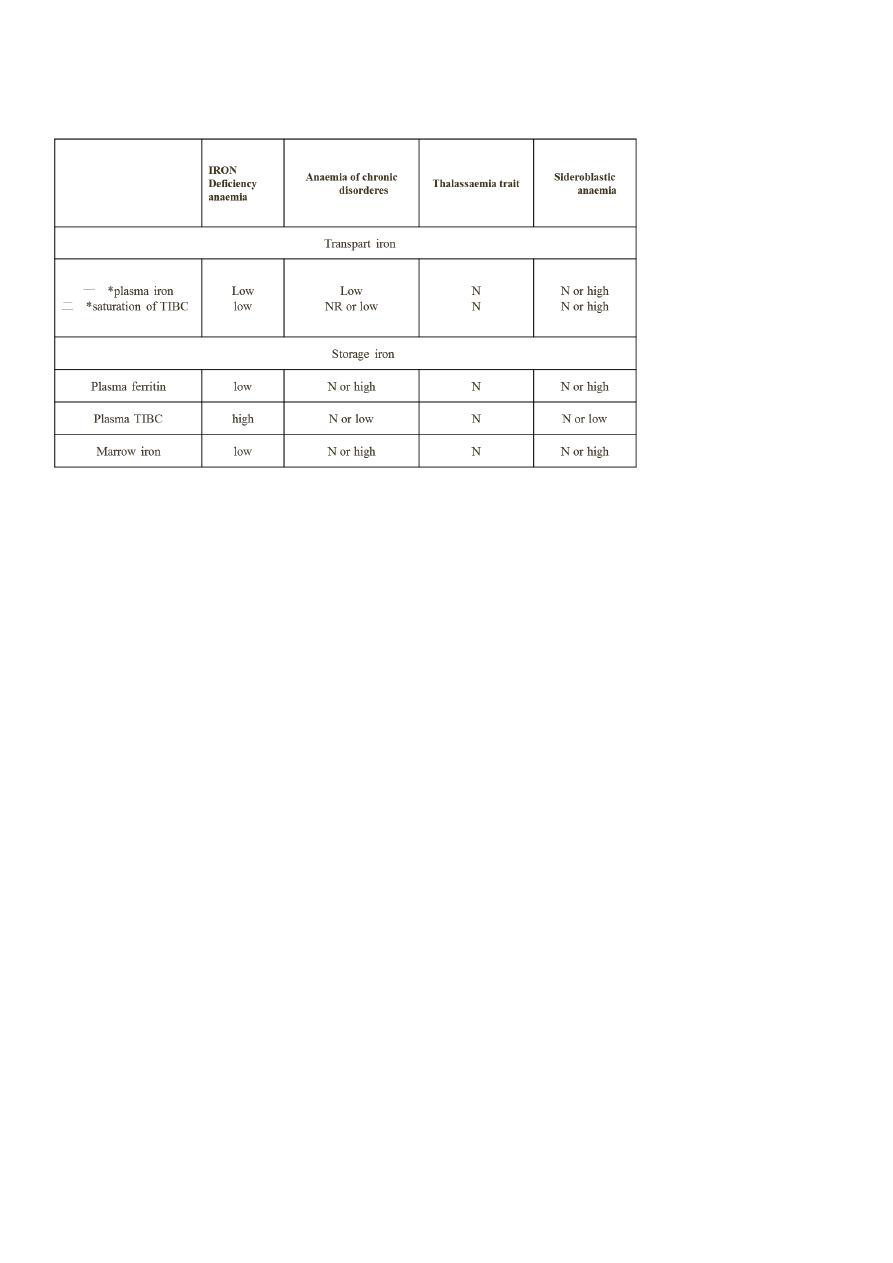
Differential diagnosis of microcytic anemia
A: disease:
B. serum iron studies:
The level of serum iron is low or normal depending on what patient eat before the
measurement .
TIBC > 400 µg/dL
Transferrin saturation <15
%
Serum Ferritin < 12 ng/ml.
Soluble transferrin receptor: increased
C. Bone marrow studies:
Absence of iron in macrophage when the sample is subjected to Perl's stain (Prussian blue
stain
TREATMENT
1- Determine the cause of iron deficiency:
Stool for occult blood loss from GIT bleeding.
Radiological analysis of upper & lower GIT for occult malignancy.
Urine analysis for hematuria.
CXR for pulmonary Hemosiderosis.
Pelvic exam. In woman.

7
Serum antiendomysial antibody or anti- transglutaminase antibodies and possibly a
duodenal biopsy are indicated to detect coeliac disease
2- Treat the underlying cause.
3- Initiate iron replacement therapy:
oral iron therapy
:
Ferrous sulfate.
Ferrous fumarate and gluconate.
Dosage The adult dose of ferrous sulfate is 300 mg/day gradually increased to 900
mg /day if tolerated.
Adverse effect GIT irritation : nausea, cramping, diarrhea
INDICATION OF parentral iron therapy
Cannot tolerate the side effect of oral iron.
Suffers from inflammatory bowel disease and peptic ulcers.
Does not comply with prescribed dosage .
Iron mal-absoption.
Suffers from condition such as hereditary hemorrhagic telengectasis (HHT) in which the
rapid loss from continuous bleeding can not be compensated by oral iron .
Transfusion of whole blood or packed red cells is generally not indicated unless a rapid
increase in haematocit is critical to the patient
PREPARATIONS
1.Iron dextran (imferon) Intramuscular injection. it may lead to hypersensitivity reaction
and anaphylaxis to the dextran and permanent stain with discoloration at the injection site.
The later can be avoided by using the Z technique of IM injection.
2.Iron sorbitol (Jectofer) IV .A small test dose 0.25 ml of the drug should be administered
before IM or IV to determine hypersensitivity to the agent
Dose in ml = 0.0476 x weight (kg) x (Hb. deficit) + 1 ml/5kg to a maximum of 14 ml to
replete iron stores.The total dose can be diluted in normal saline at 1:20 dilution and
infused slowly over several hours.
3.Iron sucrose IV in patient who are allergic to dextran.
4.new preparations of iron isomaltose and iron
carboxymaltose have fewer allergic effects and
are preferred

8
Maintain iron replacement therapy:
The treatment should be extended to beyond the point where the anemia is corrected for a
pertiod of usually 3-6 months in order to replenish depleted iron stores .
-
A failure to respond to iron therapy should suggest the following
:
incorrect diagnosis
continued loss of iron.
Presence of chronic infection or inflammation will suppress BM activity.
Lack of pt. Compliance.
Inffective release of iron.
Malabsorption of iron.
Ida criteria
LOW HB
LOW HCT
LOW MCV
LOW MCH
MCHC LOW / N
LOW FERRITIN
LOW FE
HIGH TIBC
HIGH RDW
Anaemia of chronic disease
Anaemia of chronic disease (ACD) is a common type of anaemia, particularly in hospital
populations.
It occurs in the setting of chronic infection, chronic inflammation or neoplasia .
The anaemia is not related to bleeding, haemolysis or marrow infiltration is mild, with
haemoglobin in the range of 85–115 g/L, and is usually associated with a normal MCV
(normocytic, normochromic), though this may be reduced in long-standing inflammation.
The serum iron is low but iron stores are normal or increased, as indicated by the ferritin or
stainable marrow iron

9
Pathogenesis
ACD is The regulatory protein that accounts for the findings characteristic of which is
produced by the liver Hepcidin production of hepcidin is induced by proinflammatory
cytokines, especially IL-6.
Hepcidin binds to ferroportin on the membrane of iron-exporting cells, such as small
intestinal enterocytes and macrophages, internalising the ferroportin and thereby
inhibiting the export of iron from these cells into the blood .
The iron remains trapped inside the cells in the form of ferritin, levels of which are
therefore normal or high in the face of significant anaemia. Inhibition or blockade of
hepcidin is a potential target for treatment of this form of
Diagnosis and management
It is often difficult to distinguish ACD associated with a low MCV from iron deficiency.
Examination of the marrow may ultimately be required to assess iron stores directly.
A trial of oral iron can be given in difficult situations a positive response occurs in true iron
deficiency BUT not in ACD
Measures which reduce the severity of the underlying disorder generally help to improve
ACD
