
1
Fifth stage
Plastic surgery
Lec-10
د.عبدالرحمن
1/5/2016
Basic plastic surgery
Suture technique:
1-interrupted:
Simple.(A)
Mattress: vertical (B), horizontal(C).
2-Continous:
subcutical(D).
Over and over(F).
Wound closure : by suture, skin tapes, staples, clips , glue.
Method of homeostasis
Electro-cautery.
Ligature.
Pressure and time.
Clamping and twisting.
Vasoconstrictor.
Fibrin foam.
Z-plasty
“Transposition of 2 triangular flaps”
Effects:
o Central limb lengthen.
o Change direction of scar
Uses:
o In contracture,
o Cong. Skin webs.
o U-shape scar.
2
o Circumferential scars.
o Breaking scar.
o Correction of stenotic orifice.
Vascular malformations (portwine stain)
affect boys and girls equally.
associated with other congenital syndromes.
They present at birth but missed if deep to skin.
It grows in proportion to a child’s growth
Low-flow malformations cause skeletal hypoplasia whereas high-flow can cause
hypertrophy.
Treatment with intense pulsed light and pulse–dye laser are successful.
At birth, they appear as flat, smooth, intensely purple stained areas, most frequently on the
head and neck, with age their surfaces become more keratotic and nodular.
Treatment with intense pulsed light(IPL) and pulse–dye laser are successful.
It is associated with several syndromes:
Sturge–Weber syndrome :
- affecting trigeminal dermatomes.
- associated with epilepsy and glaucoma (2ry to ipsilateral leptomeningeal angiomatosis).
-contralateral epileptic fit.
Common vascular birthmarks
Salmon patch:
as a pink macule, usually at the back of the neck, in 50% of infants.
It is caused by an area of persistent fetal dermal circulation and usually disappears
within a year.
3
Pyogenic granuloma
Small (0.5–1.5 cm), raised, pedunculated, soft, red nodular lesions with ulceration and
bleeding after trivial trauma. They should be excised.
Age: 50% below 20 years.
Pathology:
1.Acute:The increase permeability so a net flow of water, solutes and proteins from the
intravascular to the extravascular space. This flow occurs over the first 36 hours
after the injury
I.
II. Hemoconcentration.
III. Metabolic changes.
2.Subacute: diuretic phase with increase urine.
Mortality: depend on extent (%) and age.
Fluid replacement formulae in burns
1. Evans (1952):
1) 1
st
24h: 1ml crystalloid /% /kg + 1ml colloid /%/kg +D.R.(2 litre 5%GW )
2) 2nd 24 h : ½ crystalloid +1/2 colloid + D.R. crystalloid (n. saline, Ringer lacate).
Colloid (plasma, albumin, dextran,).
2. Park land :
1st 24h: 4 ml Ringer /%/kg
2nd 24h: 0.3 ml/%/kg colloid + 5% GW
In children, maintenance fluid(daily requirement) must also be given. This is normally
dextrose 5% given as follows:
• 100 ml/ kg for the first 10 kg;
• 50 ml /kg for the next 10 kg;
• 20 ml/ kg for 24 hours for each kg over 20 kg body weight.

4
Inhalational injury
Clinically: progressive increase in respiratory rate, raising pulse, anxiety and confusion and
low PO2.
symptoms may not be apparent immediately and can take 1- 5 days to develop.
Physiotherapy, nebulisers and warm humidified O2 are useful.
positive pressure(PEEP) may be used
Monitored using respiratory rate, blood gas.
Carboxyhaemoglobin levels raised above 10% must be treated with high inspired oxygen for
24 hours
Electrical burns
Low-voltage: cause small, localized, deep burns.
o May cause cardiac arrest through pacing interruption without significant direct
myocardial damage.
High-voltage:
o Myocardium may be directly damaged.
o Limbs may need fasciotomies or amputation.
o Look for and treat acidosis and myoglobinuria with mannitol & high IV fluid.
Chemical burns
o Damage is from corrosion and poisoning
o Copious lavage with water helps in most cases.
o Then identify the chemical and assess the risks of absorption

5
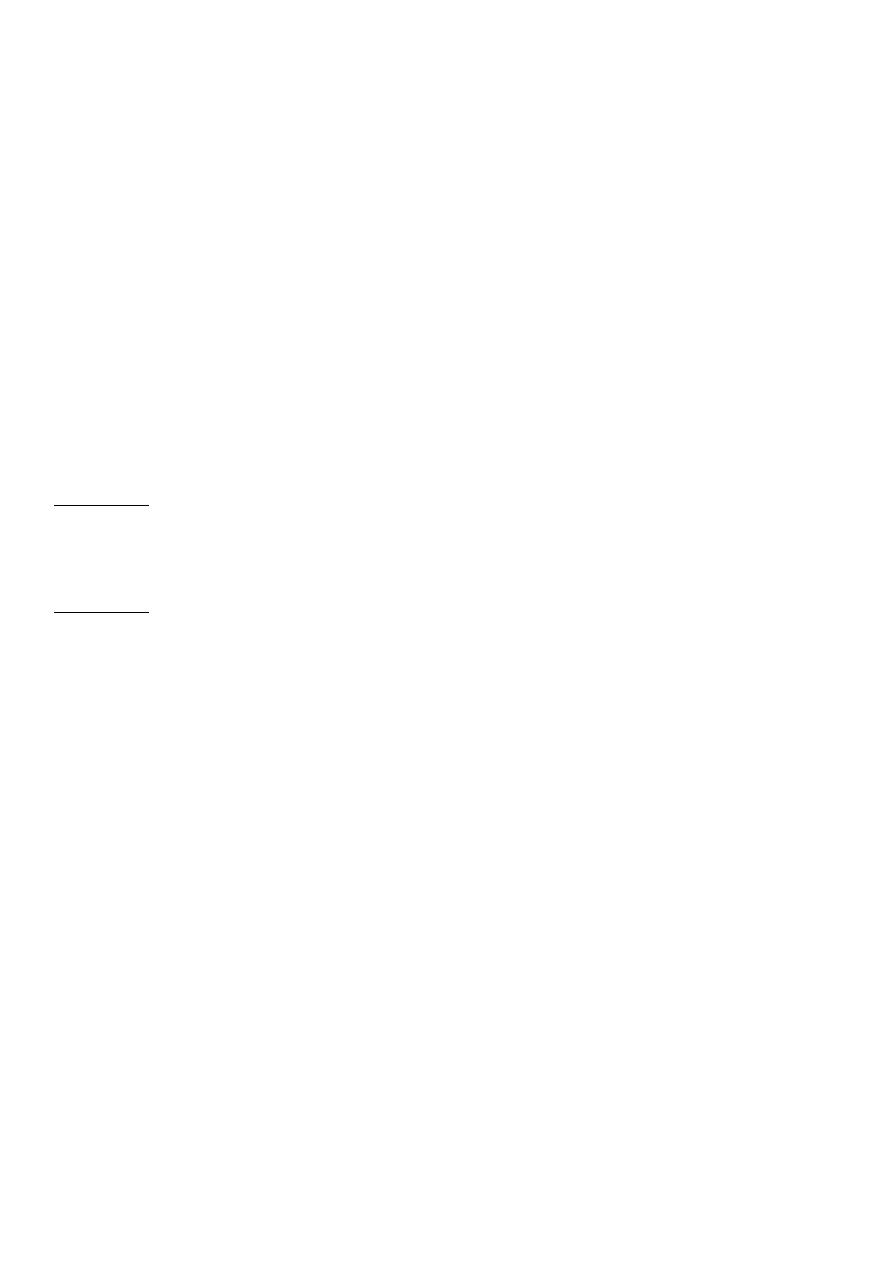
“Malignant skin tumors”
Basal cell carcinoma (BCC)
o Most common, 75% of skin tumors.
o Arise from basal layer of epidermis.
o Affects white skin, Male: Female=3:2 .
o Occurs on exposed parts: face, neck, scalp.
o No metastasis.
o Commonly Caucasian male older than 60 years
Clinical types:
1-nodulo-ulcerative : commonest type, usually single lesion, as pearly or translucent
nodule with raised borders and telangiectasias, grow slowly, tend to ulcerate, giving rise
“rodent ulcer”.
2. Pigmented BCC: second most common type, combines features of nodulo-ulcerative
&deep brown to lack brown to black nodule.
3-Superficial BCC: lightly pigmented erythematous patch, may be scaly, with areas of
scarring, mistaken for eczema ,often multiple, on trunk.
6
4-Sclerosing BCC: yellowish-white, ill-defined border, resemble scar ,it showes peripheral
growth with central scarring.
Diagnosis:
by biopsy (FNA, incisional biopsy , excisional biopsy)
Treatment:
Surgery: excision with 2-5 mm. healthy margin, & repair defect by skin graft or flap.
Radiotherapy: in large lesion, oldman, refusing operation.
Cryotherapy: for primary lesion < 2 cm., but hypopigmentation, scarring are
disadvantages.
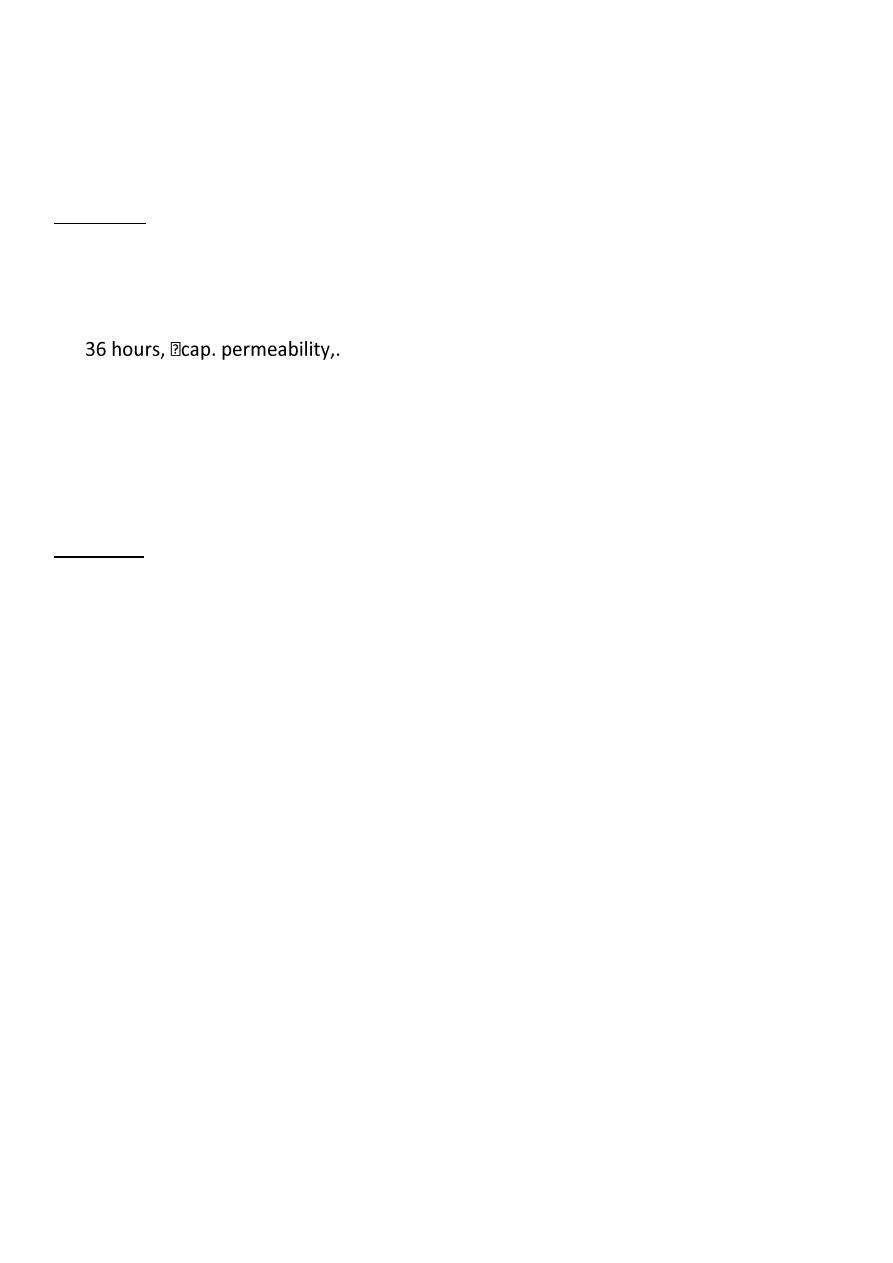
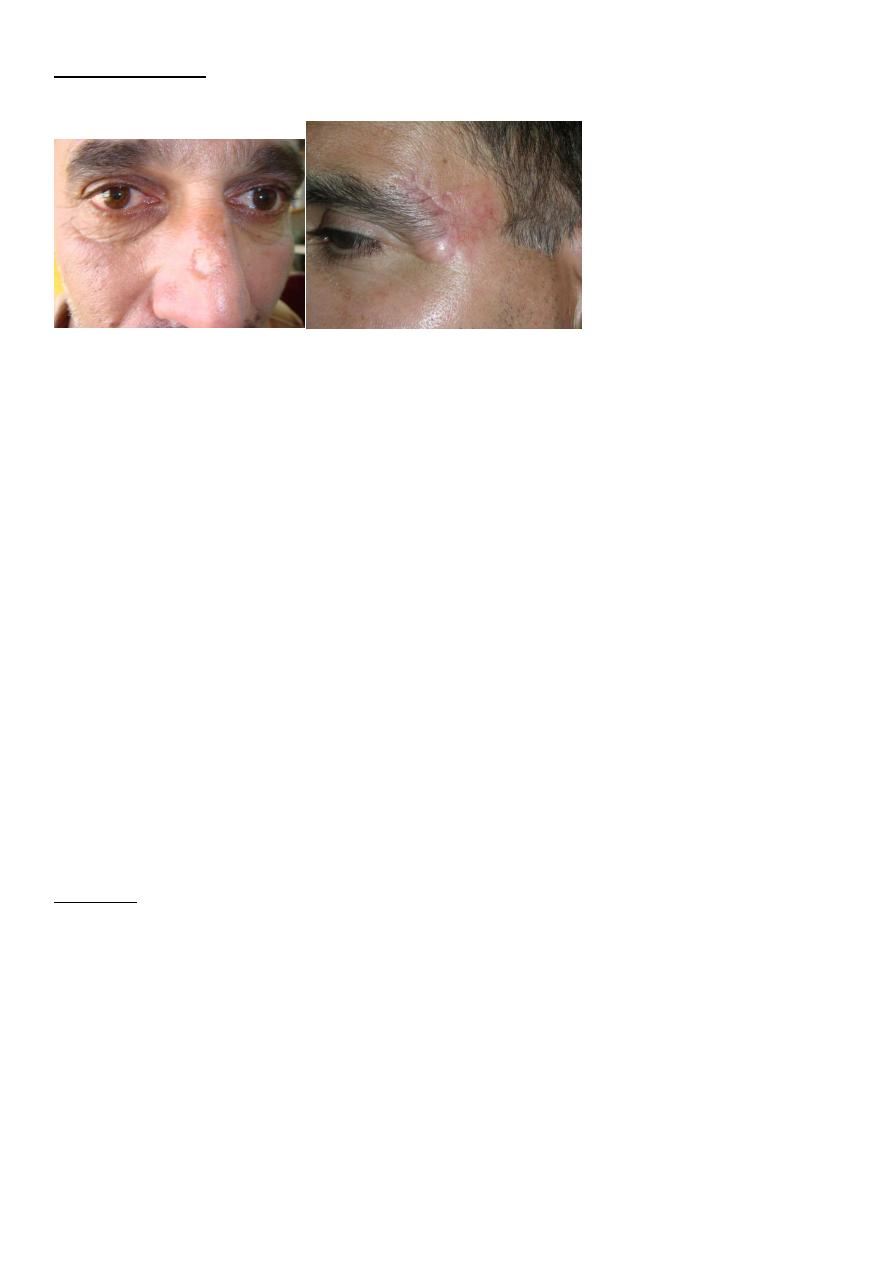
Squamous Cell Carcinoma
(SCC) is second most common skin cancer.
arises from the malignant transformation of keratinocytes in the epidermis.
arise either in normal skin or in preexisting lesion as (actinic keratosis, leukoplakia,
radiation keratosis, scars( where called Marjolin ulcer).
Clinically: present as irregular ulcer, everted edge, indurated base,attached deeply, blood-
stained discharge,frequent lymph n. positive.
Types:
1-slow growing : is verrucous,may be deeply locally invasive,likely to metastasise, more
differentiated.
7
2-Rapid growing: more nodular & indurated,early ulceration with local invasion,greater
metastasis, less differentiated.
Treatment: biopsy done.
1- Excision
Surgical excision with 10-mm margin
If lymph n. positive: excise lesion with lymph n. dissection.
2-Radiation therapy is best used in older patients,
Malignant Melanoma:
result of the malignant transformation of melanocytes, the pigment forming cells.
Occurs mainly in skin, also in eye, mouth,anus, vagina .
Malignant melanoma (MM) types:
1- Superficial spreading : 70% of MM, arise in a preexisting dysplastic nevus which changes
slowly over several months , usually flat, later become
irregular and elevated.

8
2-Nodular melanoma : 15-30%, growth deeply into dermis .
3-Lentigo maligna: 4-10%, often larger than 3 cm, flat, tan, and begin as small, frecklelike
lesions. They occur in sun-exposed areas (e.g., face and neck) of older individuals.
Breslow staging: based on vertical thickness of the lesion from thickest point:
Stage 1 : Thickness of 0.75 mm or less
Stage 2: Thickness of 0.76-1.5 mm
Stage 3 :Thickness of 1.51-4 mm
Stage 4: Thickness greater than 4 mm
Surgical treatment:
After diagnosis by biopsy, wide excision of primary lesion & removal of lymph node
involved or at high risk.
Excision with 2-3 cm healthy margin.
Elective lymph n. dissection done in lesions 1-4 mm depth, but not <1mm or >4mm.
