
1
Fifth stage
Neuro-Surgery
Lec-4
د. عبدالرحمن
2/5/2016
HEAD INJURIES
Incidence:
Major cause of morbidity and mortality.
Most common reasons for attending accident and emergency department,
accounting 3.4% of presentations.
Traumatic injury (head injury>50%) leading cause of death in the population below
45 years of age and, overall, the third leading cause of death, succeeded only by
cardiocerebral vascular disease and cancer.
Head injury is the most common cause of death in young adults (age 15-24 years)
and is more common in males than females.
Head Injuries according to Mechanisms of Injury:
a. BLUNT (CLOSED) Head Injuries:
Road traffic accidents.
Falls.
Assaults.
Workplace injuries.
Sport injuries.
Home injuries.
b. Penetrating Head injuries:
Low Velocity Injuries like Stab injuries.
High Velocity Injuries such as gunshots injuries.
Pathophysiology of head injuries:
Head Motion (Inertial) Injuries
Contact Injuries
Contact Injuries
1. Linear skull fractures.
2
2. Depressed skull fractures.
3. Basilar skull fractures.
4. Vascular damage (Extradural haematoma).
5. Coup contusions
6. Countercoup contusions
Head Motion (Inertial) Injuries
1. Translational acceleration.
2. Rotational acceleration.
3. Angular acceleration.
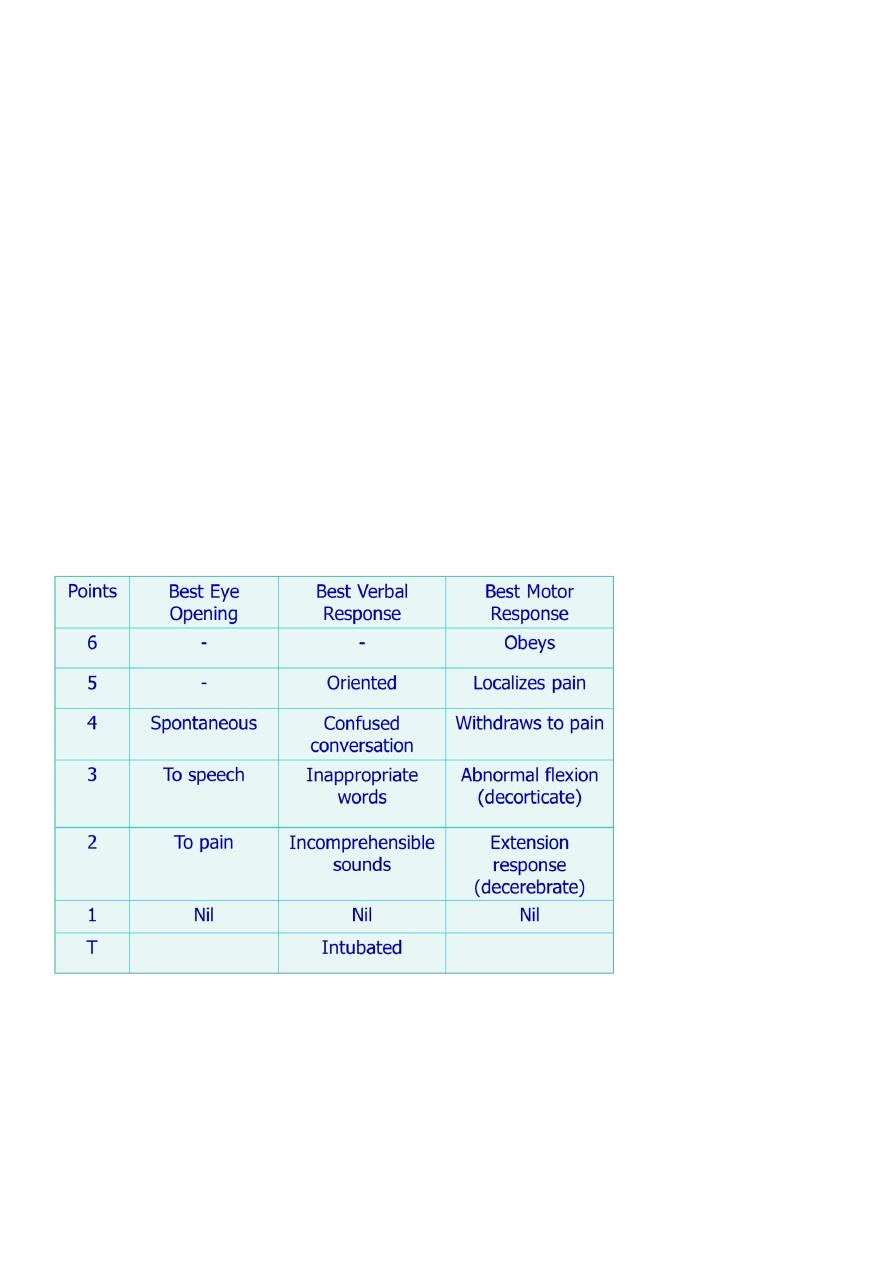
Classification of Head Injuries according to the Severity of Head Injury:
by using The Glasgow Coma Score (GCS)
The total points are added. The higher the score, the better is the prognosis. According to
this scale, cases of head injury are classified into:
Minor Head injury: GCS 15 with no loss of consciousness.
Mild Head Injury: GCS 14 or 15 with loss of consciousness.
Moderate Head Injury: GCS 9-13.
Severe Head Injury: GCS 3-8

3
Primary vs. Secondary Brain Injuries:
Primary Brain Injury: occurs at the time of impact.
Secondary Brain injuries: occurs at some time after the moment of impact and is often
preventable.
Classification of Head Injuries according to the SITE of injury:
A. Scalp Injuries
B. Skull Injuries
C. Intra-cranial Injuries (Brain Injuries)
Scalp Injuries
1. Scalp laceration (wounds of the scalp)
2. Scalp Haematoma (Subgaleal Haematoma)
1. Scalp laceration (wounds of the scalp)
o They are caused by sharp or blunt instruments or fall on the head.
o Common and may give rise to sever haemorrhage if not controlled.
o In infants this can cause sever shock.
o Depressed skull fractures may underlie a scalp injury.
o Healing is rapid.
o If infection occurs in the area of loose areolar tissue, extensive cellulitis is likely to
occur.
Management of Scalp laceration (wounds of the scalp):
o Plain X-ray is performed.
o Shaving widely around the wound.
o Closure in 2 layers
2. Scalp Haematoma (Subgaleal Haematoma)
o May be subgaleal or subpericranial.
o The soft fluctuant centers of scalp haematoma may be disguising as depressed skull
fracture on palpation.
o They are always associated with skull fracture in infants.
4
Management of Scalp Haematoma (Subgaleal Haematoma)
o Leave the lesion alone.
o It should not be tapped.
o Correction of anaemia in children less than 1 year of age.
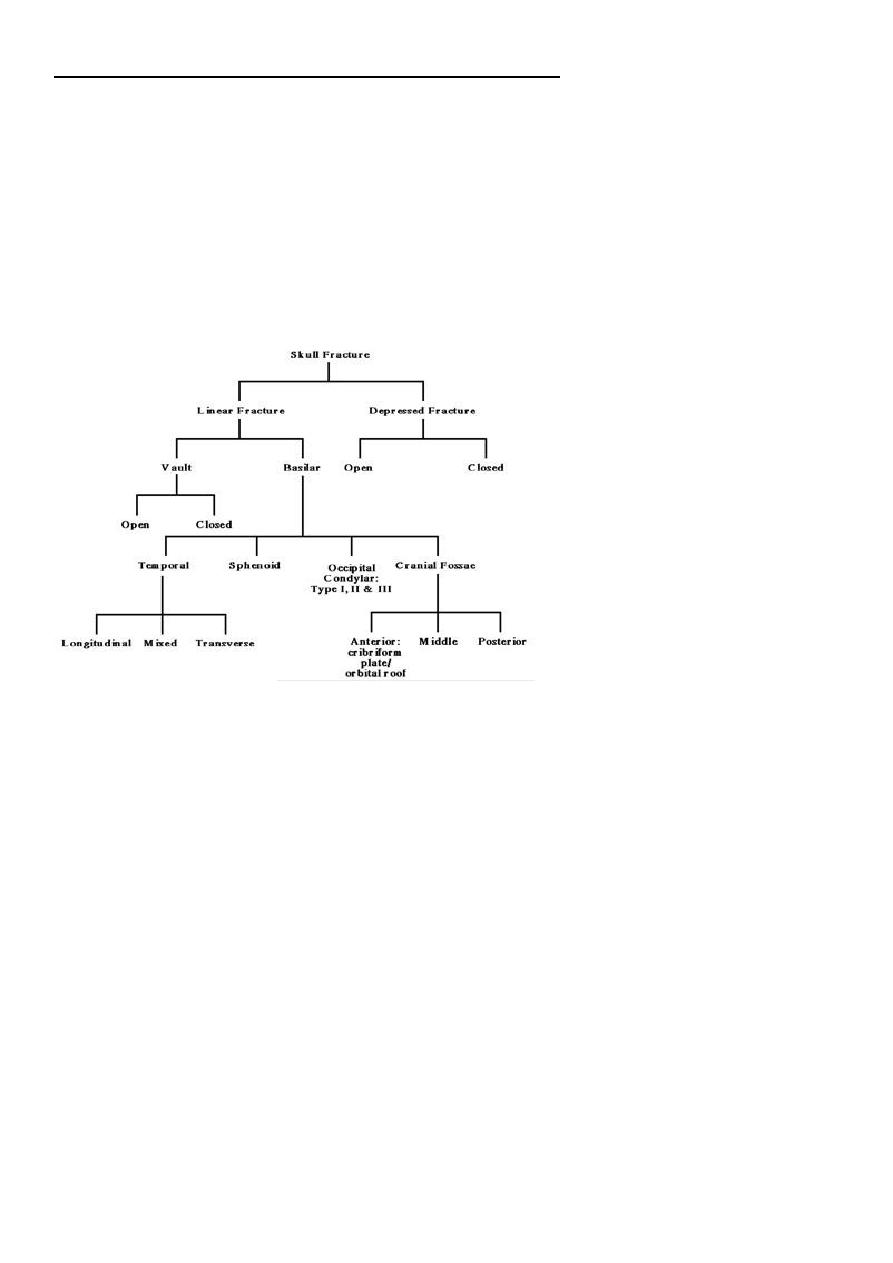
Skull Injuries (Skull Fractures)
1.
Fractures of the Vault
2. Fractures of the base (Basilar skull fractures)
Fractures of the Vault
Simple linear fractures
Depressed skull fractures
Diastatic fractures
Pond (ping pong fractures)
1- Simple linear fractures:
May be closed or opened.
Require no specific neurosurgical management.
Result of blunt trauma.
Usually require computed tomography (CT)
Patient should be admitted for 48 hours of observation.
Fractures crossing the squamous temporal bone may lacerate middle meningeal
vessels and cause extradural haematoma.

5
2- Depressed skull fractures:
Usually result from sharper trauma.
Depressed skull fractures may be:
Closed depressed fractures
Compound depressed fracture (opened)
a- Closed depressed fractures
Rare in adults
The depressed segment rarely causes cerebral compression
Plain X-ray will visualize the depressed segment.
Treatment : usually conservative measures
Indications for surgery to raise the closed depressed fracture
Large depressed segment with possibility of dural tear.
Alleviate mass effect.
Cosmetic purposes.
To prevent secondary infection.
b- Compound depressed fracture
Cause profuse bleeding, leakage of CSF and prolapse of a portion of the brain.
Concussion is slight and there is usually no compression.
The main hazard here is the liability to infection.
Treatment of compound depressed fracture
Foreign bodies are meticulously removed.
The depressed segment is gently elevated to avoid tearing of the dura.
Any prolapsed or necrotic tissue is sucked and haemostasis is performed.
Any dural tear is repaired.
Removed bone segments are cleaned and replaced.
The pericranium and the scalp are sutured.
Prophylactic antibiotics are administered.

6
Complications of depressed fractures
1. Dural tear leading to prolapse of the brain.
2. Infection; may lead to osteomyelitis or meningitis.
3. Epilepsy: either early or late.
4. Cosmetic deformity.
5. Sever bleeding from one of the venous sinuses.
3- Diastatic fractures:
It is separation of a cranial suture line.
It involves the coronal or lambdoid suture.
Diastatic fractures are common in infants under 3 years old and rare in older age
groups except as part of a more extensive skull fracture.
4- Pond (ping pong fractures):
This is a smooth concave depression due to blunt trauma to the cranial vault.
Usually seen in children and also known as ‘ping-pong fracture’, as it looks similar to
a dent in a ping-pong ball.
Fracture will elevate spontaneously if less than 3cm in diameter.
If the fracture is more than 5cm in diameter, it may need surgical elevation.
Fractures of the base (Basilar skull fractures)
These are relatively frequent fractures.
Occult radiologically.
Diagnosed on clinical examination.
They can result in CSF fistula that may persist, but which usually seals off after a few
days.
Aetiology of skull base fractures
most are due to indirect violence on the vault producing deformation of skull, with
compression of skull at one area and giving way or break of skull at other area, with
the base of skull being most vulnerable.
7
The essential features of base of skull fractures
Escape of cranial contents, e.g. blood, CSF, or brain matter.
Injury of cranial nerves.
Signs of brain injury.
Types of skull base fractures
Anterior fossa
Middle fossa
Posterior fossa
a. Anterior fossa basal fractures
May open into the frontal or ethmoidal air sinuses, or run across the cribriform plate.
Clinical presentations:
1. Subconjuctival haematoma.
2. Epistaxis.
3. Anosmia: due to olfactory nerve injury.
4. CSF Rhinorrhoea.
5. Nasal tip parraesthesia: due to injury to the 1st branch of 5th nerve.
6. Periorbital haematoma or ‘raccoon eyes’.
b. Middle fossa basal fractures
Involve the pertrous temporal bone.
Clinical presentations:
1- CSF Otorrhoea.
2- Haemotympanum.
3- Battle sign; discoloration over the mastoid process.
4- VII and VIII cranial nerve palsies.
c. Posterior fossa basal fractures
Boggy swelling or discoloration at the neck due to extravasations of blood in the
suboccipital region.
Injury to cranial nerves: usually involve 9th, 10th, and 11th cranial nerves at the
jugular foramen.
Retraction of the head and stiffness of the cervical muscles due to upper cervical
nerves irritation.

8
Management of skull base fractures
1. Prevention of infection: prophylactic antibiotics.
2. Control of CSF leakage: conservative or surgical intervention.
3. Treatment of associated brain injury.
Indications for surgery(repair of tear)
a. Persistence of rhinorrhoea more than 10 days
b. Presence of a fracture involving the frontal or ethmoidal sinus.
c. Occurrence of meningitis.
