1
Fifth stage
Neuro-Surgery
Lec-7
د. عبدالرحمن
2/5/2016
Intracranial Tumours
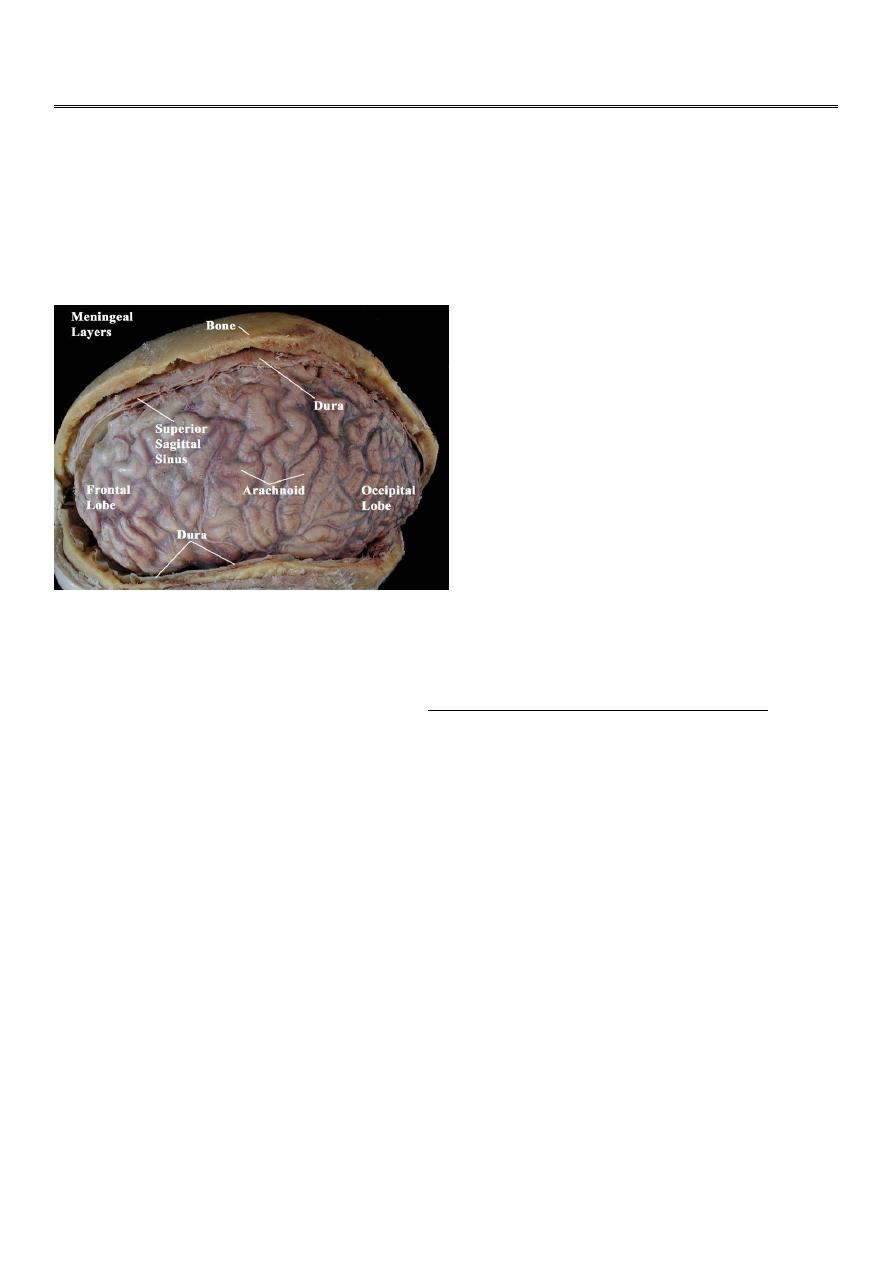
All neoplasms arising from the skull, meninges, blood, blood vessels, pituitary and pineal
glands, cranial nerves, brain tissue, or congenital rests, as well as metastatic tumors.
General Considerations
Although either benign or malignant, almost all brain tumours are malignant in the
sense that they may lead eventually to death if not treated.
Epidemiology
Brain tumors are responsible for 2% of all cancer deaths.
The incidence varies with age.
In adults, metastatic brain tumor is the most common intracranial neoplasm
comprising about 15-20% of them.
Among the primary, the most frequent are gliomas followed by meningiomas.
Glioma more frequent in males and meningiomas are more common in females.
In children, brain tumors are the second most common after leukemia. 70% are
infratentoreal. The most frequent are cerebellar astrocytoma, brainstem glioma,
medulloblastoma and ependymoma.
In neonates and in infants, brain tumors are rare mostly congenital.

2
Classification of brain tumours
The classification of brain tumours is determined by their cell of origin.
Over 50% are neuroepithelial in origin, 15% metastatic, 15% meningioma and 8%
pituitary tumours.
The World Health Organization (WHO) classification of brain tumours
A. Neuroepithelial Tumours:
B. Nerve sheath tumour: acoustic neuroma
C. Meningeal Tumours: Meningioma
D. Pituitary Tumours
E. Germ cell tumours: e.g. Germinoma, Teratoma
F. Lymphomas
G. Tumour-like malformations:
H. Metastatic Tumours
Neuroepithelial Tumours
1) Gliomas:
Astrocytomas
Oligodendrogliomas
Ependymoma
Choroid plexus tumour
2) Pineal Tumours
3) Neuronal Tumours
4) Medulloblastoma
Tumour-like malformations
Craniopharyngioma
Epidermoid tumour
Dermoid tumour
Colloid cyst

3
Aetiology of Brain Tumors
The etiology of brain tumors is still not clearly understood.
Radiation associated with meningioma , glioma and fibrosarcoma
Although there is no genetic predisposition, chromosomal abnormalities have been
noted in many CNS tumors (e.g. von Recklinghausen's).
Viruses, EBV associated with Burkitt s lymphoma and nasopharyngeal carcinoma
Immunosuppression markedly increase the incidence of primary CNS lymphoma.
Mutation in the p53 tumor suppressor gene is the most common gene alteration and
is found in astrocytoma and meningioma
Clinical Features of Brain Tumours
This will result from one or a combination of:
a) Focal neurological deficits
b) Raised intracranial pressure
c) Seizures, and
d) Endocrine dysfunction, or
e) Incidental findings (i.e. symptomless).
a) Focal Neurological Deficits
Frontal lobe lesions: presents with personality changes, gait ataxia, and urinary
incontinence, contralateral hemiparesis if posterior frontal and expressive dysphasia
if involving the dominant inferior frontal gyrus.
Parietal lobe lesions: contralateral sensory impairement, dressing apraxia,
asteriognosis and, if on the dominant side, acalculia, agraphia, left-right
disorientation and finger agnosia.
Temporal lobe lesions: olfactory and auditory hallucination, memory disturbances,
contralateral superior quadrantanopia or hemiparesis and, if on the dominant side,
receptive dysphasia.
Occipital lesions: associated with visual field deficits, most commonly an incomplete
contralateral homonymous hemianopia.
Subfrontal lesions: may involve the olfactory nerves (anosmia).

4
Sellar and parasellar: tumours present with visual field problems due to
compression of the optic chiasm, hypopitutarism and oversecretion syndromes such
as Cushing's disease and acromegaly.
Cerebellar lesions: Tumours involving the cerebellar vermis cause truncal ataxia,
whereas tumours in the hemispheres produce appendicular signs such as
incoordination and nystagmus.
Brainstem and Cerebellopontine angle lesions: may result in cranial nerve palsies,
long tract signs and secondary hydrocephalus.
Ventricular system tumours: may obstruct CSF drainage and result in
hydrocephalus, compounding raised ICP.
b) Raised Intracranial Pressure
Direct mass effect.
Vasogenic oedema.
Obstructive hydrocephalus.
c) Seizures
New onset of seizure in an adult is suggestive of an intracranial mass until proven
otherwise.
The type of seizure may give a clue to the location of the tumour:
Parietal lesions cause simple partial seizures, which may become secondarily
generalized.
Medial temporal lesions will cause complex partial seizures.
Late onset epilepsy, particularly over the age of 30 years, should prompt
investigations to exclude an intracranial neoplasm.
New onset of seizure in an adult is suggestive of an intracranial mass until proven
otherwise.
The type of seizure may give a clue to the location of the tumour:
Parietal lesions cause simple partial seizures, which may become secondarily
generalized.
Medial temporal lesions will cause complex partial seizures.
Investigations of Brain Tumours
Plain Skull x-ray
Computed Tomography (CT-scan)
Magnetic Resonance Imaging (MRI)
5
Angiography
Positron Emission Tomography (PET).
1- Plain Skull x-ray:
May be normal
May show changes due to raised intracranial pressure.
Local changes may occur with specific tumours: like
o Suprasellar calcification in craniopharyngiomas
o Hyperostosis and skull thickening in meningioma.
2- Computed Tomography (CT-scan):
Site and size of the tumour.
Boundaries of the tumour.
If there is surrounding oedema or not.
Shift of the midline structures by the mass.
Associated hydrocephalus.
Bony changes.
Nature of the tumour (solid, cystic, necrotic or calcified), and so its pathology.
3. Magnetic Resonance Imaging (MRI): same as CT
4. Angiography:
Used to evaluate the blood supply and vasculature of the tumor.
5. Positron Emission Tomography (PET): can study the brain metabolism.
Used to characterize the most malignant component of a tumour.
Assess prognosis of brain tumour.
Differentiate recurrent tumour from radiation necrosis.
Management of intracranial tumours
If the patient shows signs of compression, or raised intracranial pressure, treat with
measures that lower ICP.
If an intracranial tumour is associated with hydrocephalus, the hydrocephalus is
dealt with first by a ventriculoperitoneal shunt before surgery.
CT or MRI guided stereotactic surgery : tumour is deeply seated in the brain.
Surgical excision or debulking for accesssible tumours.
6
In cases of malignant brain tumours or metastases : adjunctive therapy :
Radiotherapy and/or Chemotherapy are supplementary to surgical excision.
a. Radiotherapy either conventional radiotherapy or radiosurgery
For small tumor less than 3 cm which is of many types
Linear accelerator
Gama knife
Cyber knife
Metastatic Brain Tumours
Constitute 15% of intracranial tumours.
The commonest sites of origin are the lung (40%) and breast (10-30%), in addition to
melanoma (5-15%), kidney and colon.
In 15% of cases, a primary source is never found.
On CT, they only show well with intravenous contrast.
Steroids may help reduce peritumour oedema.
Surgery may be appropriate for an isolated metastasis.
CSF shunt used for lesions causing Hydrocephalus.
Radiotherapy can be used for multiple metastases.
Gliomas
They are derived from cells of glial origin.
They are the commonest of primary CNS neoplasms.
They form 50% of adult intracranial tumours.
They are of four types: astrocytoma, oligodendroglioma, ependymoma and choroid
plexus papilloma. The most common of which is astrocytoma.
Survival is closely associated with grading.
Treatment involves surgery and radiotherapy and/or chemotherapy.
Meningiomas
These account for 15% of intracranial neoplasms, and are the most common benign
neoplasm.

7
They occur more frequently in women than in men, and their incidence peaks in
middle age.
The tumour arises from meningothelial cells of the arachnoid villi.
They classically arise from a broad base along the dura.
They may invade bone.
They derive their blood supply from the external carotid circulation.
Malignant meningiomas are relatively rare.
The symptoms and signs are related to those of intracranial mass lesions or seizures.
CT scan accurately diagnoses the lesions.
Complete surgical removal usually results in cure.
Pituitary Tumours
Non-functioning pituitary adenomas
Functioning pituitary adenomas
1- Non-functioning pituitary adenomas
Accounts for about 30% of pituitary tumours.
They are often seen in the fourth and fifth decades of life.
Because they are non-functioning, they are not generally diagnosed until they are
very large.
Their presentation is by optic chiasm compression that cause visual field defect
(bitemporal hemianopia).
The usual treatment is microscopic trans-sphenoidal or trans-cranial excision.
2- Functioning pituitary adenomas
Pituitary adenomas are classified according to the hormones they secrete. They
include:
o Prolactin secreting adenomas.
o Growth hormone secreting adenomas that produce acromegaly or gigantism.
o Glycoprotein secreting adenomas that produce excess amount of TSH, LH, or
FSH.
o ACTH secreting adenomas that produce Cushing's disease.
o Some of these secrete more than one hormone, e.g. prolactin-growth hormone
secreting adenomas.
Adenomas may be further divided according to their sizes into Microadenomas that
are less than 1 cm in diameter, and Macroadenomas that have a larger size.

8
Functioning adenomas are diagnosed by:
o Clinical changes.
o Hormone assessment. And
o Radiology by using MRI and CT scan.
Prolactinomas represent 40% of all pituitary adenomas. They cause amenorrhoea,
galactorrhoea, and infertility in women, while in men they cause impotence or may
be asymptomatic.
Bromocriptin (antiprolactin drug) has virtually replaced surgery as the treatment of
choice for prolactinomas.
Surgical excision can preferably done by using the trns-sphenoidal route, whether
sublabial or transnasal, although transcranial approach can also be used.
In case of an invasive tumour with incomplete excision, radiotherapy is required
DO NOT FORGET
The most significant findings pointing to an intracranial tumour on physical
examination are the presence of papilloedema and signs of focal damage to the
nervous system.
If a cerebral tumour is suspected, LUMBAR PUNCTURE IS CONTRAINDICATED as it
may precipitate a fatal coning of the brain stem through the foramen magnum.
