
1
Fifth stage
Surgery
Lec-1
.د
سيف
1/1/2014
Vascular neurosurgery
Subarachnoid hemorrhage
1) Trauma is the most common cause of SAH
2) Spontaneous SAH can be due to
Ruptured aneurysm
Ruptured AVM (arteriovenous malformation)
Vasculitis
Tumor
Coagulopathy
Dural sinus thrombosis
Idiopathic
10 % die before reaching the hospital
10 % die within the first few days
Overall mortality 45 %
Peak age for spontaneous SAH is 55-60 years
Patients more than 70 years having higher incidence and severe neurodeficit
Risk factors include
Hypertension
Cigarette and alcohol consumption
Oral contraception , pregnancy and parturition
Advancing age
Clinical feature
Symptoms
Sudden onset of severe headache (the most common symptom 97% , usually severe
described as the worst headache in my life, this type of headache may clear and called
sentinel hemorrhage or warning headache that could be seen in 50% of patients with
aneurysm
Vomiting, photophobia, diplopia due to 3
rd
nerve palsy from aneurysmal compression and
with more severe cases neurological complication and impaired consciousness
2
Signs
1- Meningismus: positive meningeal signs that often develop in 6-24 hrs and include
1. Nuchal rigidity (neck stiffness) o flexion
2. Kernig sign ( flex the thigh and knee joint to 90 degree, then straighten the knee, pain
in the hamstring muscles will develop)
3. Brudzinski ( involuntary hip flexion on flexing the neck )
2- Hypertension, focal neurological deficit and impaired consciousness
3- Ocular hemorrhage in form of
1. Intraretinal hemorrhage
2. Preretinal hemorrhage
3. Vitrealhemaorrhage ( terson syndrome ) occur in 6-26% most of the cases clear
spontaneously 6-12 months
Diagnosis
Clinical features
Investigations
Non contrast high resolution CT scan which can demonstrate the amount of
blood in the cisterns and fissure, ventricular size, associated intracranial
hemorrhage, infarction and predict the location of aneurysm.
LP (lumbar puncture) if CT scan negative (the most sensitive test for SAH)
Cerebral angiography (the gold standard for evaluation of cerebral angiography)
and can also demonstrate cerebral vasospasm
Differentiating SAH from traumatic LP
Opening pressure : elevated
Non-clotting bloody fluid that does not clear with sequential tubes
Xanthochromia : pink or yellow coloration of CSF supernatant due to broken
RBC , the most important point needing 2-4 hrs to develop
RBC count more than 100.000 RBC/ml
Protein elevated due to broken RBC
Glucose : normal or reduced
Complications
Seizure
Rebleeding, the major concern initially
Hydrocephalus ( usually obstructive by blood clot or communicating type which
develop often late due to toxic effect of blood breakdown)
Cerebral vasospasm
3
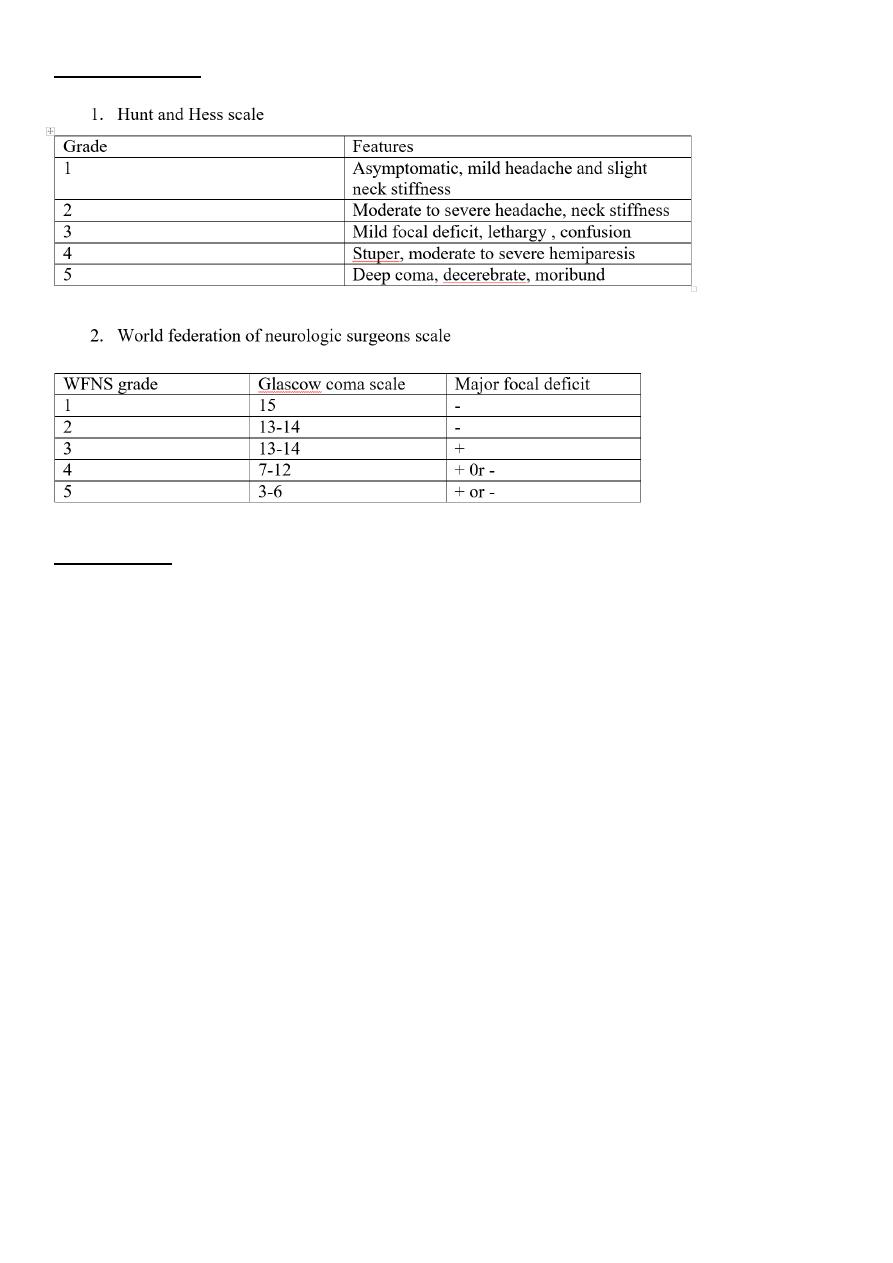
Grading of SAH
Management
Admit to ICU with arterial line, endotracheal intubation for comatose patient, ECG
monitor,folley catheter and intraventricular catheter
Vital signs with neuro check q 1 hr
Head elevation 30 degree
Check fluid input and output
Pneumatic compression stocking
Prophylactic anticonvulsant, phenytoin 17mg/kg loading then 100mg TID or luminal
10 mg/kg loading then 5 mg/kg/day
Sedation with propofol
Analgesia e.g. phentanyl
Decadron
Stool softener
Antiemetic, avoid phenothiazines that lower seizure threshold, use zofran
(ondansetron) 4 mg slow I.V TID
H
2
-blocker, ranitidine ampule 150mg BID or omeprazole or lansaprazole 30mg PO q
day)
Calcium channel blocker with Nimodipine 60 mg 6 times a day PO within 96 hrs
Treatment of underlying aneurysm by
o Surgical clipping
o Endovascular coils application
o Endovascular trapping
o Endovascular balloon therapy
4
Vasospasm:
Angiographic vasospasm: asymptomatic arterial narrowing seen on angiography
Clinical vasospasm : delayed ischemic neurological deficit, manifested clinically as
increasing headache, alteration in the level of consciousness, disorientation,
meningismus or a feature of anterior or middle cerebral artery syndrome
Most significant cause of morbidity, almost never before day 3 post hemorrhage, usually the
onset is between day 6-8 and resolve by day 12
Risk factors for vasospasm include
Increasing age
Female with middle cerebral artery aneurysm
Hypertension
Pial enhancement on CT scan
Hypovolemia
Low GCS on admission
Higher amount of blood within subarachnoid space
Diagnosis
Clinical deterioration
Ruling out rebleeding, hydrocephalus, seizure, cerebral oedema, hyponatremia
Transcranial Doppler, high blood velocity with spasmodic artery , more than 120 cm/s
Cerebral angiography
treatment
Triple H therapy, hypertension, hypervolemia and hemodilusion
Calcium channel blocker, nimodipine
Removing blood clot surgically
Intra-arterial Balloon dilatation
Intra-arterial papaverine injection
Traumatic aneurysm :
Compromise less than 1 % of intracranial aneurysm
Most are false aneurysm (pseudoaneurysm), ruptured all vessel wall layers with the
wall of the aneurysm being formed by surrounding cerebral structures
Rare in children
5
Caused by
o Penetrating trauma
o Closed head injury (more common)
o Iatrogenic , following surgery
Can be presented by
o Incidentally finding
o Progressive headache
o Delayed intracranial hemorrhage
o Progressive cranial nerve palsy
Treated by
o Balloon trapping or balloon embolization
Mycotic aneurysm (infectious or bacterial ):
Compromise 4 % of intracranial aneurysm
Occur in 4-14 % of patient with subacute bacterial endocarditis (SBE)
Usually caused by streptococcus followed by staphylococcus
Treated by antibiotic for 4-6 weeks with angiographic follow up if failure treated
surgically
