
1
Fifth stage
Surgery-Ortho
Lec-6
.د
مثنى
28/4/2016
Fractures of the tibia and fibula
Indirect force: (low energy)
Twisting: spiral fractures of both bones
Angulatory: oblique fractures with butterfly segment.
Direct force:
Transverse (low energy) or comminuted (high energy) fractures usually with skin
and soft tissue damage.
Examine for:
Size of skin and soft tissue damage.
Distal pulses, sensation, movements.
Signs of compartment syndrome.
X-ray must include the knee and ankle.
Management
Objectives:
To limit soft tissue damage and preserve skin cover.
To obtain and hold fracture alignment.
To recognize compartment syndrome.
To start early weight bearing to promote healing.
To start joint movement as soon as possible.
Treatment of low energy fractures
Including closed & Gustilo I & II fractures treated by non-operative methods; MUA for
displaced fractures.
Full-length cast from upper thigh to metatarsal necks with the knee in slight flexion
and the foot plantigrade.
Elevate the leg and observe for 2-3 days for compartment syndrome.
After 4-6 weeks change to below knee functional brace and allow weight bearing and
knee movement.
Healing is complete in 8 wks in children and in 16 wks in adults.

2
Skeletal fixation
Locked intramedullary fixation is the method of choice for diaphyseal (shaft) fractures.
Plate and screws for fractures near bone ends (metaphyseal) and for children with
closed unstable fractures.
Open fractures:
Antibiotics & anti-tetanus.
Debridement; thorough wash with normal saline, removal of dead tissues and debris.
Stabilization preferably using external fixation.
Soft tissue cover using flaps or grafts.
Rehabilitation.
Complications
Vascular injury; popliteal A. injury with proximal tibial frctures requires angiogram,
exploration and repair.
Compartment syndrome; open fasciotomy done with minimum delay.
Infection after open fractures and open surgery.
Malunion: shortening >1.5cm, angulation > 7degrees or rotation should be corrected.
Delayed union and non-union; bone grafting and good fixation is required.
Joint stiffness.
Complex regional pain syndrome.
Ankle ligament injuries
Range from:
Stretching of the ligament.
Partial tear: healing restores full function.
Complete tear: joint instability.
Usually involves lateral ankle ligaments (ant. Talofibular lig., talocalcaneal lig., and post.
Talofibular lig.).
Medial calcaneal lig. (deltoid lig.) can result from abduction or eversion injury.
Clinical features:
Bruising, swelling, tenderness (usually distal and anterior to lat. Maleolus in anterior
talofebular lig. Injury).

3
Treatment
Partial tears: elastic bandage and gentle active exercise.
Complete tears: cast immobilization from below knee to toes for 6 wks then
physiotherapy.
If this regime fails; operative repair is done.
Complications:
Recurrent sprains.
Recurrent giving way or instability.
FRACTURES AND FRACTURE- DISLOCATIONS OF THE ANKLE
Injury may involve one or more of the following structures:
Lateral maleolus.
Medial maleolus.
Tibiofibular syndesmosis.
Lateral collateral ligament (ant. And posterior talofebular lig., and calcaneofibular lig.).
Medial collateral (deltoid) lig.
Tibial articular surface (tibial plafond).
Position of the talus.
Clinical features
History of severe inj. In young athletes or simple inj. In elderly osteoporotic.
Ankle twist.
Intense pain, swelling, inability to stand and deformity.
Look for points of tenderness espetially over medial or lateral malleolus.
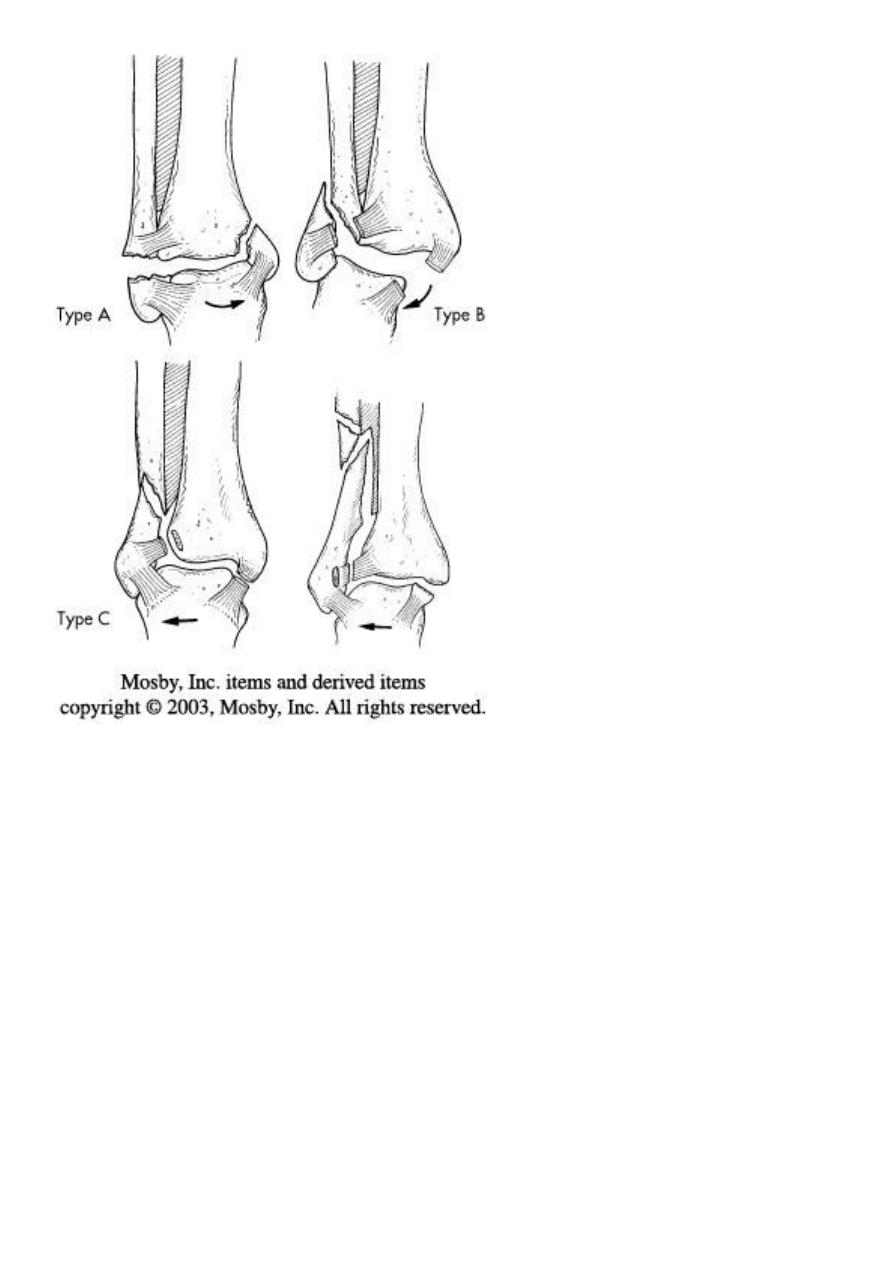
Danis-Weber classification (based on the level of fibular fracture)
Type A: a fibular fracture below syndesmosis and oblique fracture medial maleolus.
Type B: fibular fracture at syndesmosis + disruption of ant. Fibers of tibiofibular lig. +
fracture of medial malleolus or rupture of deltiod lig.
Type C: fibular fracture above syndesmosis+ tibiofibular lig. (syndesmosis) is torn.
Unstable fracture-subluxation of ankle mortise.
4
Principals of treatment
Treatment within hours or after several days until swelling subside by elevation and
splintage.
Anatomical reduction is a must to avoid later osteoarthritis.
Fibular fracture below tibiofibular lig. Ankle jt. is stable; reduce the fracture and
immobilize in a cast.
Fibular fracture above tibiofibular lig. Ankle jt. is unstable; usually need internal
fixation.

5
Postoperative management
Below knee cast for 4 wks in low-level injuries, and 6-8 wks in fractures treated by surgery.
Complictions
Joint stiffness and prolonged swelling. Treat by compression stocking and elevation.
Complex regional pain syndrome.
Osteoarthritis
Comminuted fractures of the tibial plafond (Pilon fracture)
Severe axial compression of the ankle (FFH).
Shattering of ankle joint surface.
Swelling and blistering; treated by elevation and calcaneal traction.
Secondary Osteoarthritis is common.
Fractures of Talus
Rare and usually due to considerable violence- FFH, car accidents,…
May involve the body, neck, head or dislocation of the talus.
Clinical features
Pain, swelling, deformity.
Skin tented or split.
X-ray: difficult to diagnose. May need to repeat several days later to see the fracture.
C-T in difficult cases.
Treatment
Trivial displacement: Below knee plaster with knee plantigrade for 6-8 wks
Displaced fractures or fracture dilocations: urgent reduction by closed manipulation; if
fails, ORIF
Complications
Non-union.
Avascular necrosis of body after fracture of neck.
Oseoarthritis.

6
Calcaneal fractures
Usually after FFH.
Associated injuries: spine, pelvis, hip or base of skull.
Extra-articular fractures: need closed treatment. Have good prognosis.
Intra-articular fractures: involve superior articular surface. May be comminuted.
Special features
Foot painful, swollen, bruised and the heel look broad. Movement is painful.
Signs of compartment syndrome: intense pain and diminished sensation.
Necessary to X-ray the knees, spine, and pelvis.
Treatment
Admit to hospital, elevate the leg and apply ice-packs until swelling subside.
Undisplaced fractures: closed treatment.
Displaced fractures: ORIF with screws.
Complications
Broadening of the heel
Talocalcaneal stiffness and OA
Metatarsal fractures
Mechanism of injury:
Direct blow.
Twisting.
Repetitive stress.
Treatment:
Walking plaster for 3 wks.
Displaced fractures; Kirschner wire fixation.

7
Stress injury (march fracture)
Young adult (often recruit or a nurse)
Painful foot after overuse.
Tender lump in shaft of metatarsal (usually 2
nd
).
X-ray: at first normal but later show hairline fracture and callus.
Radioisotope shows early increased activity.
Avulsion of base of fifth metatarsal
Result from forefoot inversion injury.
Base of 5
th
MT avulsed by peroneus brevis tendon.
Treatment: Below knee walking cast for 3wks.
