1
Fifth stage
Surgery-Ortho
Lec-3
د. هشام القطان
8/3/2016
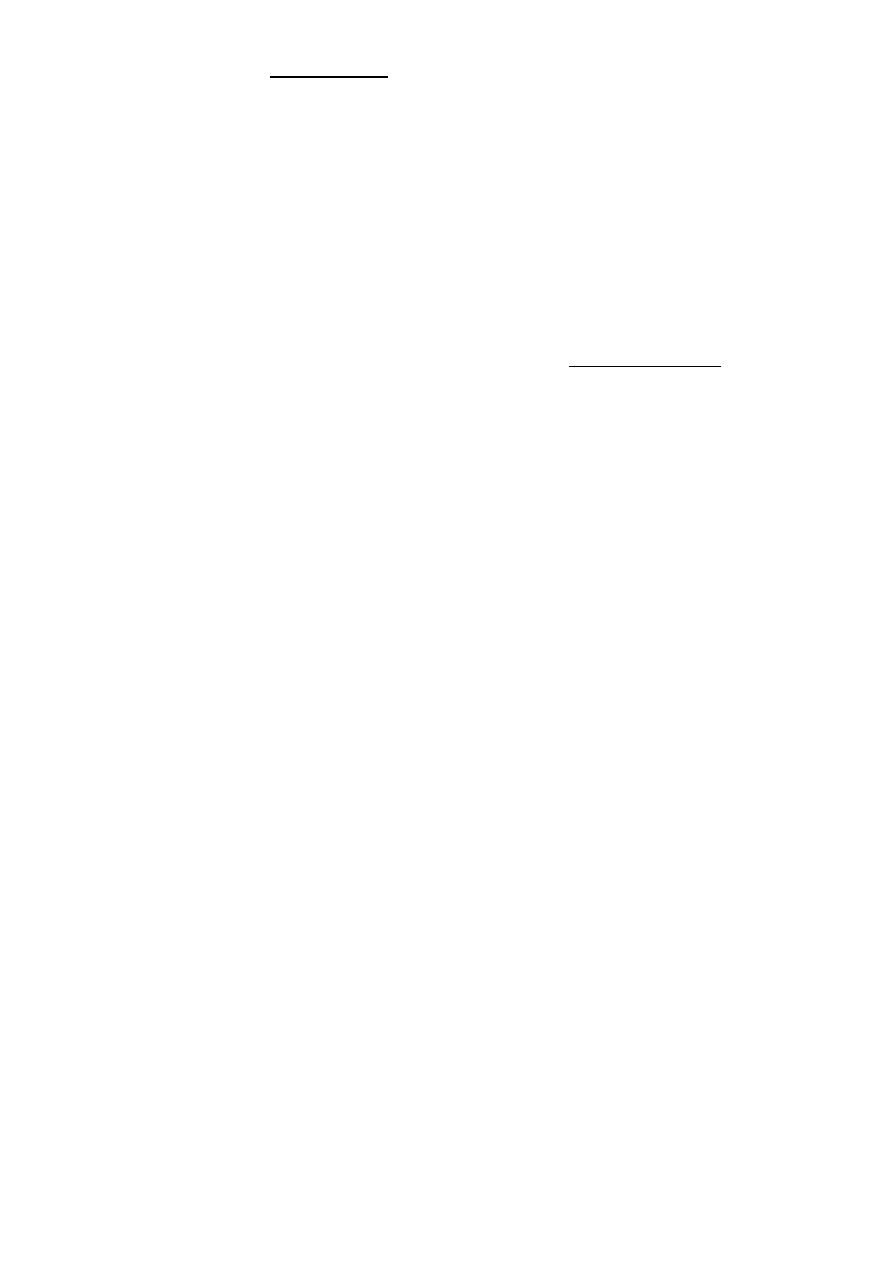
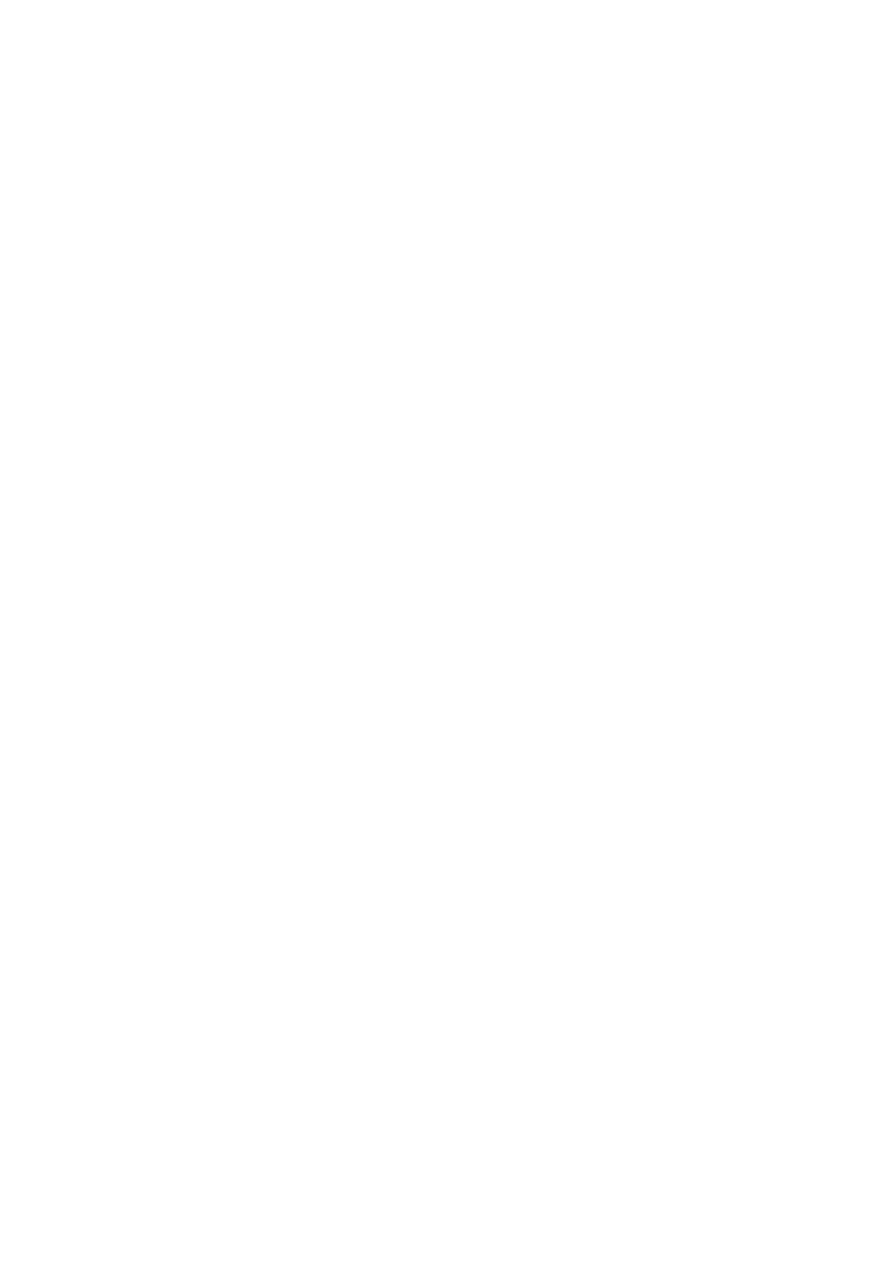
Fractures of the femoral neck
INTRA CAPSULAR FRACTURE
Risk factors
1. Osteoporosis, osteomalacia
2. Diabetes Mellitus
3. Stroke
4. Alcoholism
5. Chronic debilitating disease.
6. Weak muscle and poor balance in old people. parkinsonism)
Mechanism of injury
In elderly
Directly Fall on greater trochanter.
Indirectly. Less force with catching toes in carpet with external rotation of the lower
limb.
In younger individual fall from height or car accident (more sever force).
Pathological anatomy and classification
The most useful is that of garden which is based on amount of displacement apparent in the
pre-reduction x-ray of the neck femur.
1. Stage 1 impacted
2. Stage 2 complete fracture Undisplaced
3. Stage 3 complete with moderate displacement.
4. Stage 4 severely displaced fracture
2
Fracture neck femur has poor capacity for healing because of:
Tearing the capsule vessels.
Intra-articular bone has flimsy periosteum
No contact with soft tissue.
Synovial fluid wash.
Clinically
History of fallen on the ground.
Pain in the hip.
On Examination Limb lies laterally rotation and looks, Short (displaced fracture). In impacted
patient might walk.
Radiological examination
Two questions must be answered.
Is there a fracture?
Is it displaced?
Radiological classification:
GRADE 1: the femoral head is in its normal position or tilted into valgus and impacted
on the femoral stump
GRADE 2: the femoral head is normally placed and the fracture line may be difficult to
diagnosed
GRADE 3: The femoral head tilted out of position and the trabecular marking are not
in line with those of innominate bone.
GRADE 4: The femoral head trabeculae are normally aligned with those of innominate
bone.
Differential Diagnosis
Stress fracture.
Undisplaced fracture.
Painless fracture.
Multiple fractures as with femoral fracture may have neck fracture and missed.

3
Treatment
Surgery mandatory to overcome complications.
Initial treatment
General measure as pain killer.
Temporary limb splintage (skin traction).
Full investigation
Chest x ray
ECG.
F B S.
B urea.
Blood group
Blood preparation for transfusion.
Treatment depend on the type and age of the patient
YOUNGER
Screw
DHS
ELDERLY PEOPLE
Austen Moore
Total hip replacement
Complications
General
DVT
Pulmonary embolism.
Pneumonia.
Bed sore.
Local
A.N. 30% in displaced fracture, 10% in Undisplaced fracture.
Non-union > 30% femoral fracture fails to unite particularly those with sever
displacement. .
Osteoarthritis, avascular necrosis or femoral head collapse may lead after several years
to secondary osteoarthritis.

4
Inter-trochanteric fractures (extracapsular fracture)
It is extra capsular fracture occurs in elderly. Unite quite easily and seldom cause avascular
necrosis.
Mechanism of injury:
Directly on trochanter.
Twisting force indirectly.
The crack runs up between the lesser and greater trochanter.
Pathological anatomy divided into:
Stable
Unstable are those where:
1. Posteromedial cortex is shattered.
2. Poor contact between fracture segments.
Clinically:
Old and unfit
History of trauma.
Unable to stand with pain.
EXAMINATION
The leg is shorter and more externally rotated than intracapsular fracture.
Ecchymosis
Radiological examination
Stable
Unstable
Treatment
Same previous principle almost always treated by early internal fixation to overcome the
possible complications associated with prolonged recumbency and to get the patient up and
walking as soon as possible.
Sliding nail
L-plate
Gamma nail
External fixation

5
PHYSIOTHERAPY
Postoperative exercise is started as early as possible on the day after operation.
Patient is allowed up and partial weight bearing as soon as possible.
Complications
Early
General complications.
Late
Failed fixation.
Malunion.
Rarely nonunion.

6
HIP DISLOCATION
The magnitude of force needed to dislocate the hip joint ((particularly well-contained by
virtue of its bony and soft-tissue anatomy)) is so great that the dislocation is often associated
with fractures - either around the joint or elsewhere in the same limb.
Hip dislocations are classified according to the direction of the femoral head displacement.
Traumatic Dislocations of the hip.
Posterior.
Anterior.
Central.
Posterior dislocation:
Mechanism of injury: 4 out of 5 traumatic hip dislocations are posterior. Usually occur in
road traffic accident when the knee striking the dashboard. The femoral head is forced out
of its socket sometimes associated with fracture.
Clinically:
In a straight forward case the diagnosis is easy.
O\E: Leg is short, internally rotated, adducted and slightly flexed hip.
Sometimes fracture femur associated with, and clinically missed.
Sciatic nerve examination distally is important.
The golden role is to X ray the pelvis in every case of severe injury and with femoral fracture
to include both the hip and knee.
Radiological examinations
X-R AP view we can see the dislocation with or without associated fracture posterior wall of
the acetabulum, or fracture head of the femur and neck of femur.
CT scan is the best way of demonstrating acetabuluar fracture or any bony fragment.
Treatment:
The dislocation must be reduced as soon as possible under general anesthesia. In the vast
majority of cases this is done with closed reduction
U\A on the ground. Pelvic support. In line of the lower limb traction, then gradually flexion
of the patient’s hip and knee in 90 degree.
At 90 hip flexion traction is increased and sometimes little rotation is increased (both internal
and external) to accomplish reduction. Satisfying clunk terminate the procedure.
7
Skin traction 3-6 weeks.
Physiotherapy during and after that.
In complicated dislocation (surgery is indicated).
Complications:
Early
Sciatic nerve injures when there is fracture lead to foot drop in 10%. So nerve function
must be tested and documented before reduction.
Vascular injury mainly for the superior gluteal artery.
Associated fractured femoral shaft. So as a rule the buttock and the greater
trochanter should be palpated.
Late
Avascular necrosis by x-ray appeared between 6weeks- 2 years. It occur in 10% and
raised to 40% if neglected more than 12 hours.
Myositis ossificans.
Osteoarthritis due to fracture acetabulum or femoral head, or a vascular necrosis
Traumatic anterior hip dislocation:
Mechanism:
Road traffic accident, miner, building laborer who is leg wide, knees straight and back bent
forward.
Clinically:
O\E
Leg external rotation.
Abducted and slightly flexed.
Bulging head seen laterally and also feel.
Hip movement impossible.
Neurovascular examination necessary.
Radiological examination:
Hip dislocated either superior, inferior in relation to the acetabulum.
Treatment:
Same principle as posterior while traction of the leg keeping adducted till reduced.
