1
Fifth stage
Surgery-Ortho
Lec-13
د . هشام
1/1/2014
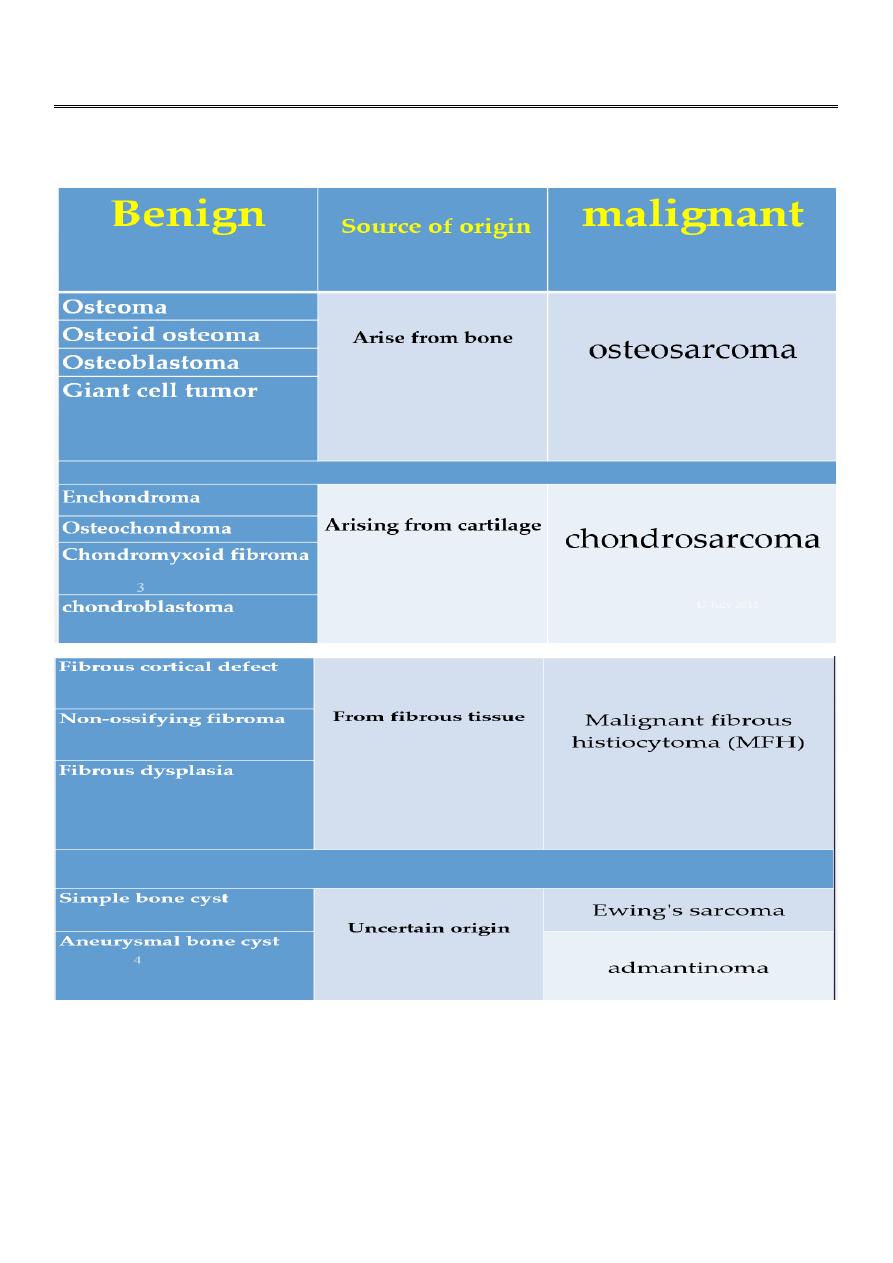
Bone tumor
QUESTIONS TO ASK WHEN STUDYING AN X-RAY
:
is the lesion solitary or are there multiple lesions?
What type of bone is involved?
Where is the lesion in the bone?
Are the margins of the lesion well- or ill-defined?
2
Are there flecks of calcification in the lesion?
is the cortex eroded or destroyed?
is there any periosteal new-bone formation?
Does the tumour extend into the soft tissues?
Osteoid osteoma
This is a benign circumscribed lesion that may arise from the cortex of long bones or
occasionally from the cancellous bone of the spine.
Affect young patients 10-35 years.
3 times common in males than females.
Pathology :
The characeristic features is the formation of a small nidus of osteoid tissue usually less
than 0.5cm diameter, surrounded by a reactive zone of dense sclerotic new bone
formation.
Clinical features
Usually present with increasingly sever but well - localised ,deep aching pain and
sometimes local bone tenderness.
Pain worse at night.
Eased by aspirin or NSAIDS. ( Diagnostic features) .
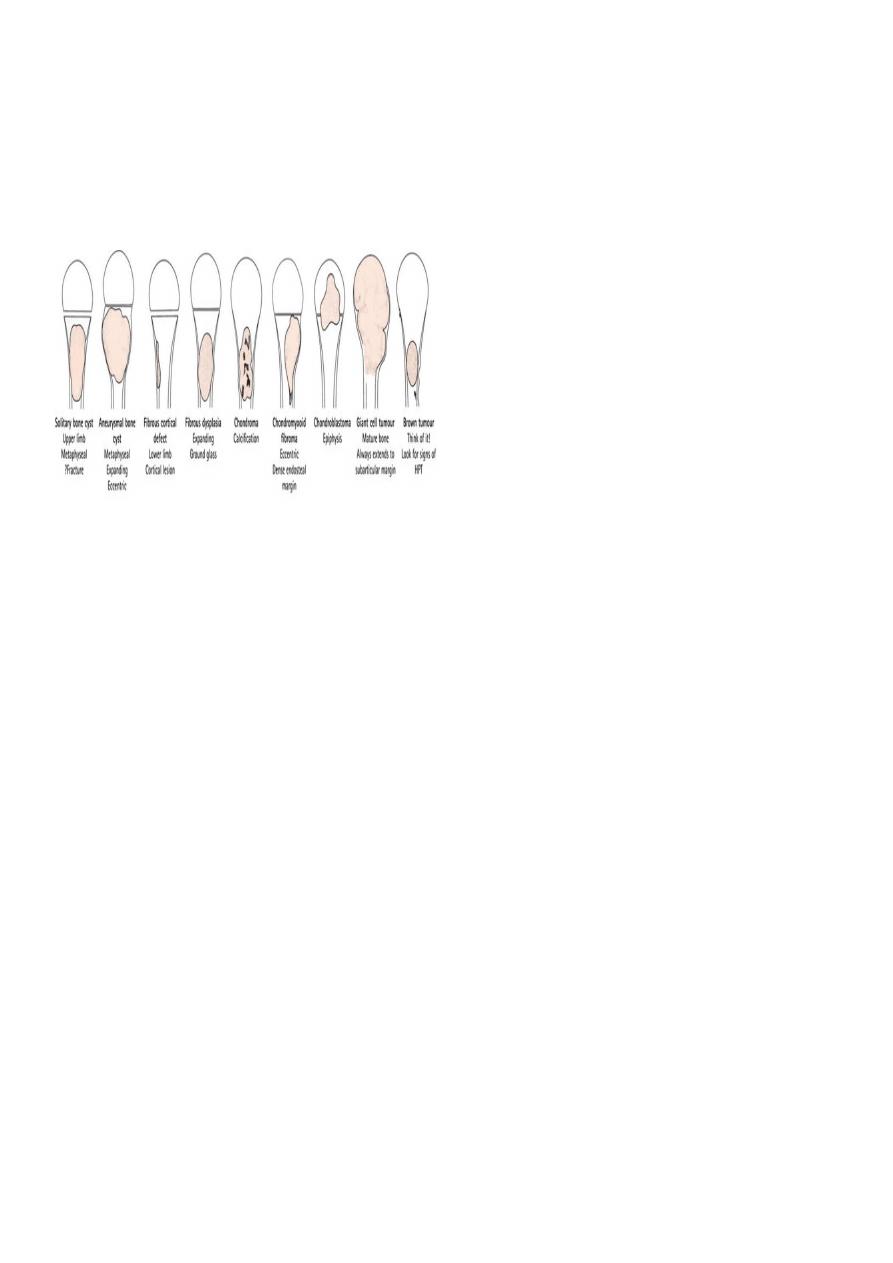
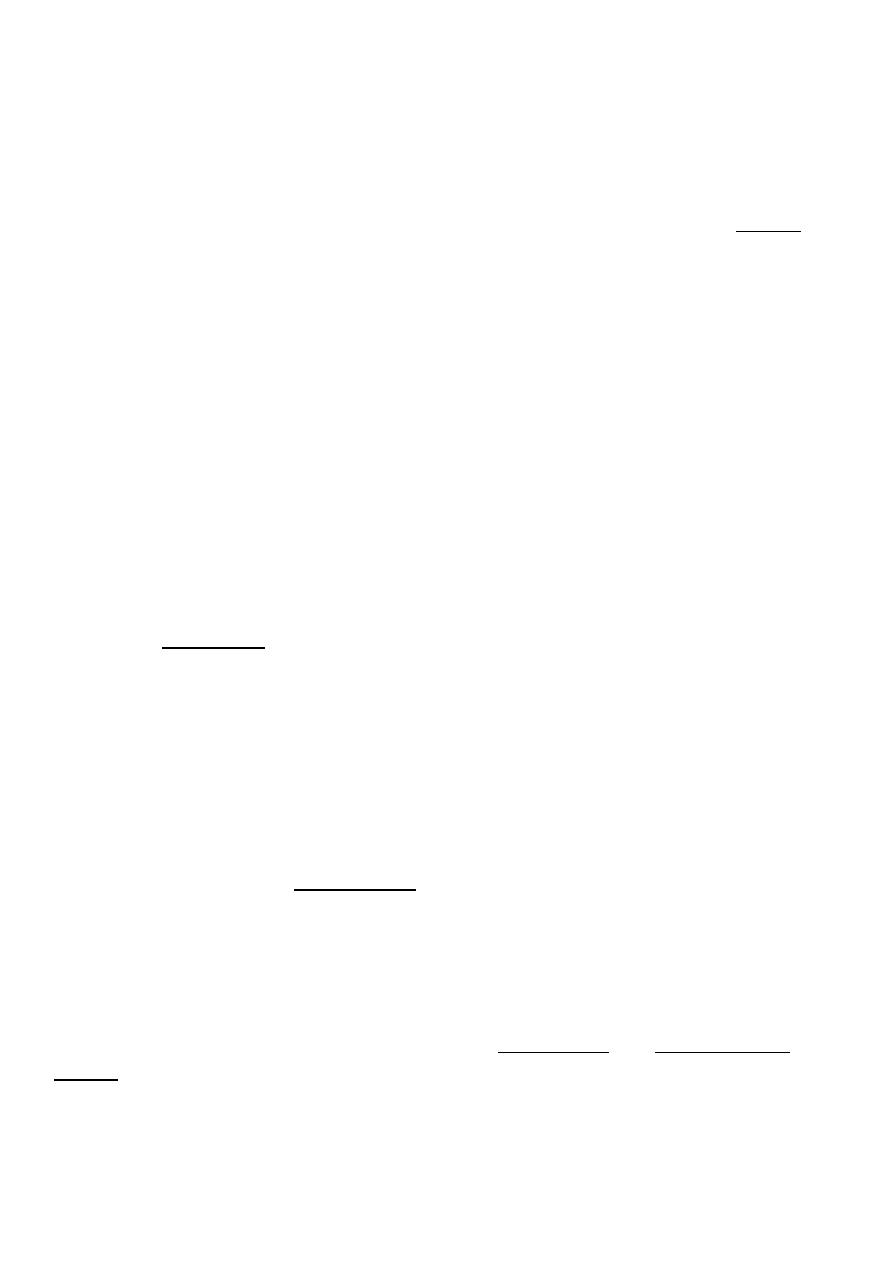
Imaging
Plain x-ray
Show local sclerotic thickening of the shaft that may obscure the small central nidus
within the area of rarefaction.
The nidus is best seen on a fine cut CT scan
Intense uptake on an isotope bone scan.
3
C T scan
Treatment
May resolve spontaneously after several months.
Most require surgery
Removal of the nidus alone produce dramatic relieve and this done by,
Surgical exscion,
curettage.
CT guided needle can be inserted into the nidus and the lesion ablated with
radiofrequency coagulation.
4
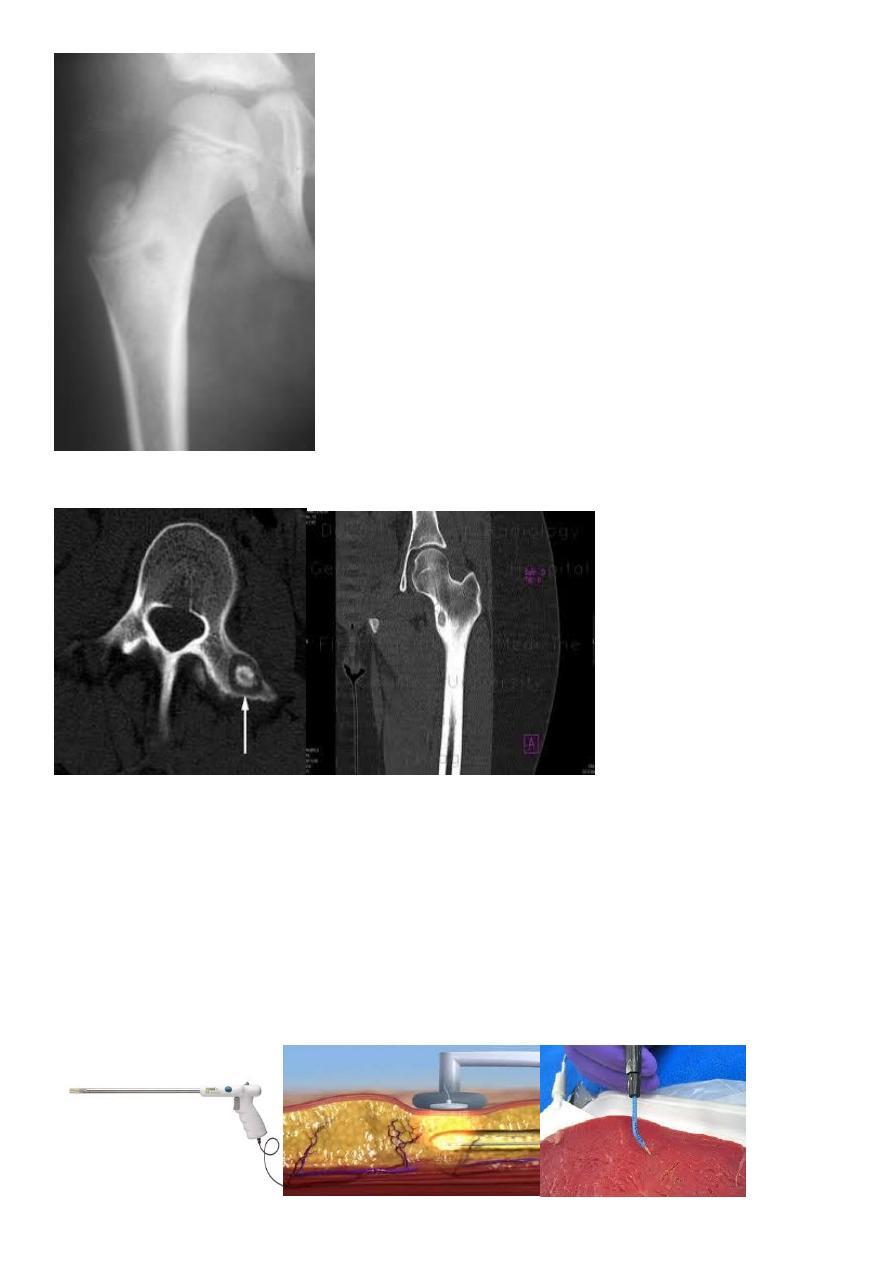
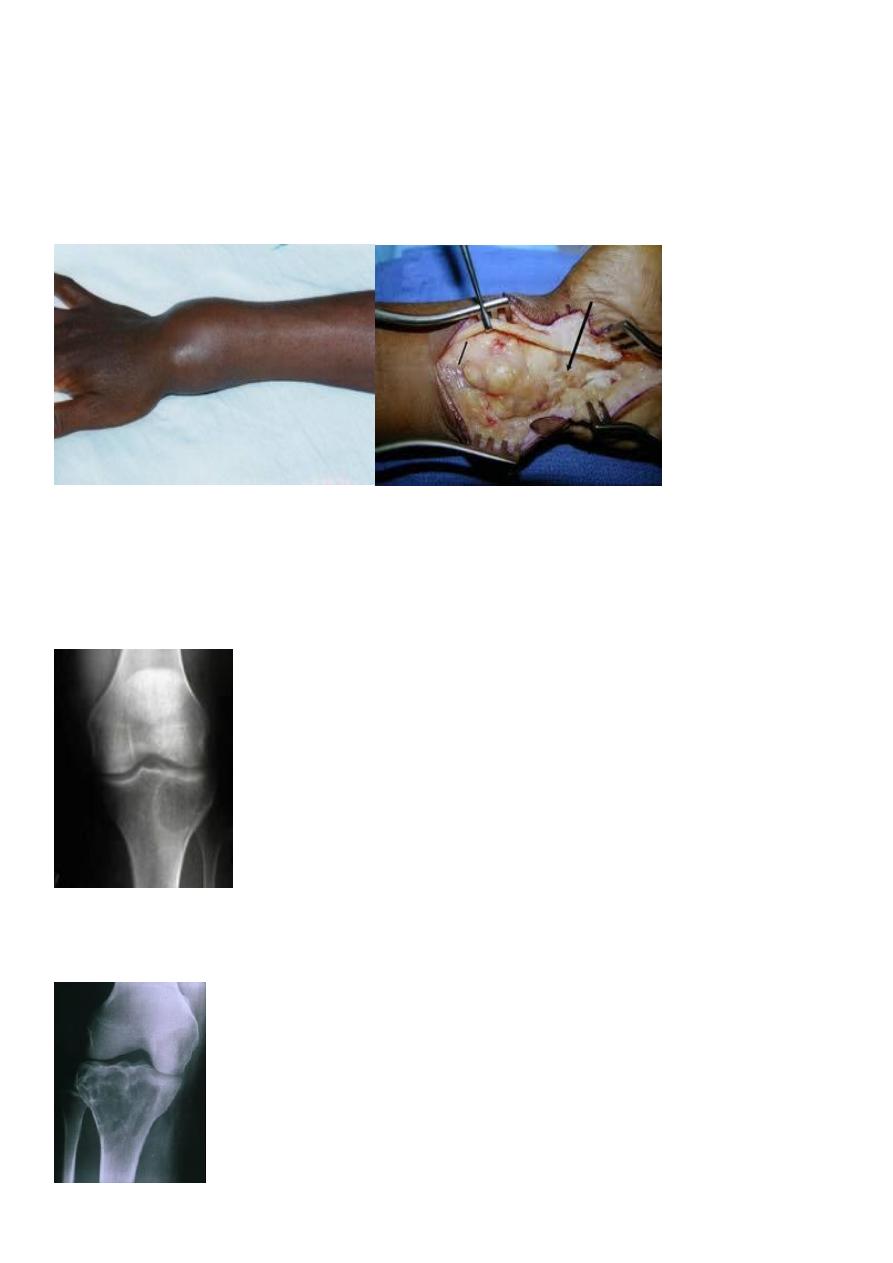
OSTEOCHONDROMA (CARTILAGE-CAPPED EXOSTOSIS)
This, one of the commonest ‘tumours’ of bone, is a developmental lesion which
starts as a small over-growth of cartilage at the edge of the physeal plate.
And develops by endochondral ossification into a bony pro-tuberance still covered by
the cap of cartilage.
commonest sites are the fast-growing ends of long bone. and the crest of the ilium.
Clinical features :
The patient is usually a teenager or young adult when the lump is first discovered.
Occasionally there is pain due to an overlying bursa or impingement on soft tissues, or,
rarely, paraesthesia due to stretching of an adjacent nerve.
Pathology
the cartilage cap is seen surmounting a narrow base or pedicle of bone.
The cap consists of simple hyaline cartilage;
in a growing exostosis the deeper cartilage cells are arranged in columns, giving rise to
the formation of endochondral new bone.
The x-ray appearance
is pathognomonic. There is a well-defined exostosis emerging from the metaphysis,
its base co-extensive with the parent bone.
It looks smaller than it feels because the cartilage cap is usually invisible on x-ray.
5
Ollier disease :
Multiple lesions may develop as part of a heritable disorder – hereditary multiple exostosis
Large lesions may have a ‘cauliflower’ appearance, with degeneration and calcification in
the Centre of the cartilage cap.
Complications
The incidence of malignant transformation is difficult to assess .
Treatment
:
If the tumour causes symptoms it should be excised; if, in an adult, it has recently become
bigger or painful then operation is urgent.
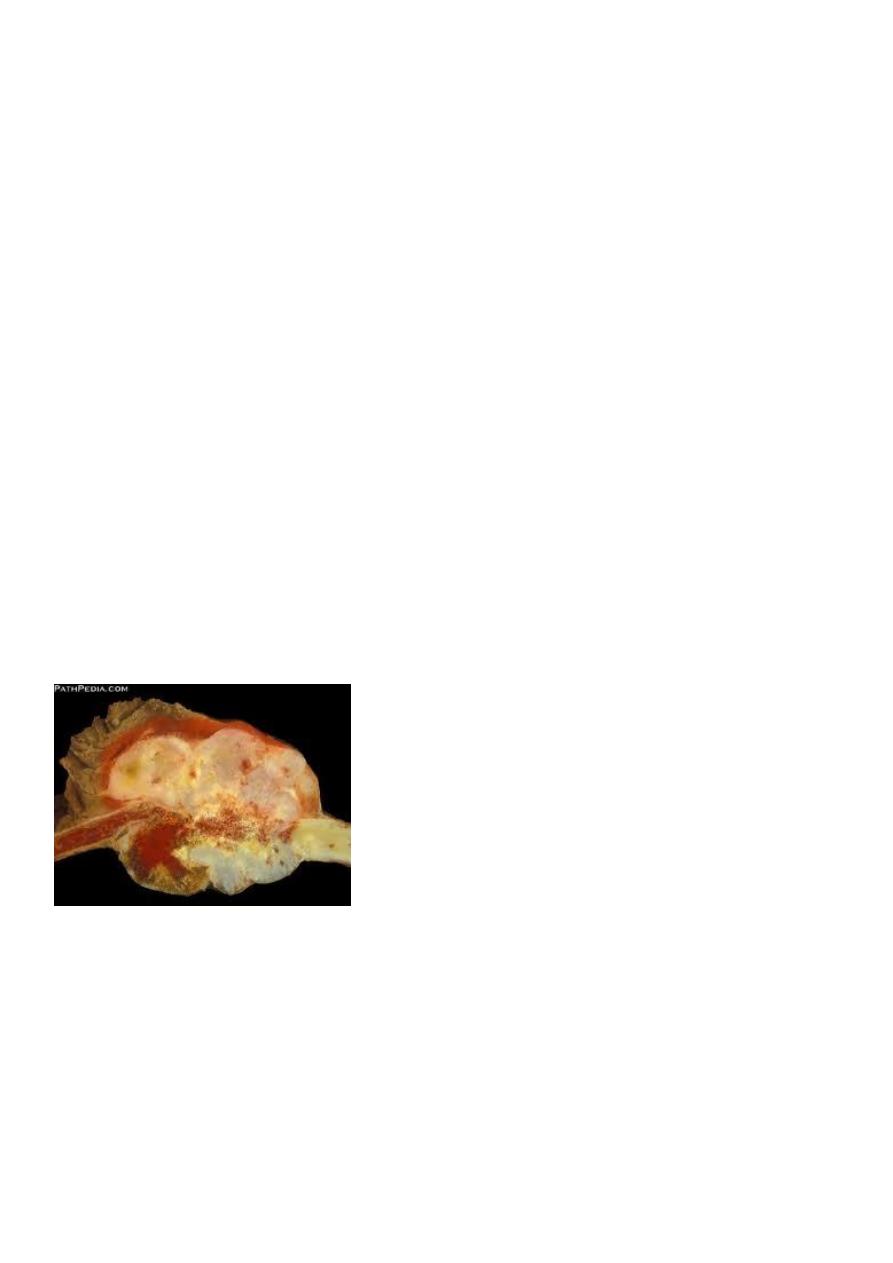
GIANT-CELL TUMOUR osteoclastoma
Pathology
Giant-cell tumour, which represents 5 per cent of all primary bone tumours.
most commonly in the
distal femur,
proximal tibia,
proximal humerus .
and distal radius.
though other bones also may be affected.
It is hardly ever seen before closure of the nearby physis . and 10% behaves as malignant .
characteristically it extends right up to the subarticular bone plate. Rarely, there are
multiple lesions.
Histologically :
Tumor consist abundant of mononuclear stromal cells profusely interspersed with giant
cell.
6
Clinical features
The patient is usually a young adult 20-40 years who complains pain at the end of a
long bone; sometimes there is slight swelling.
A history of trauma is not uncommon.
Some time the patient is made suddenly aware of some thing wrong.
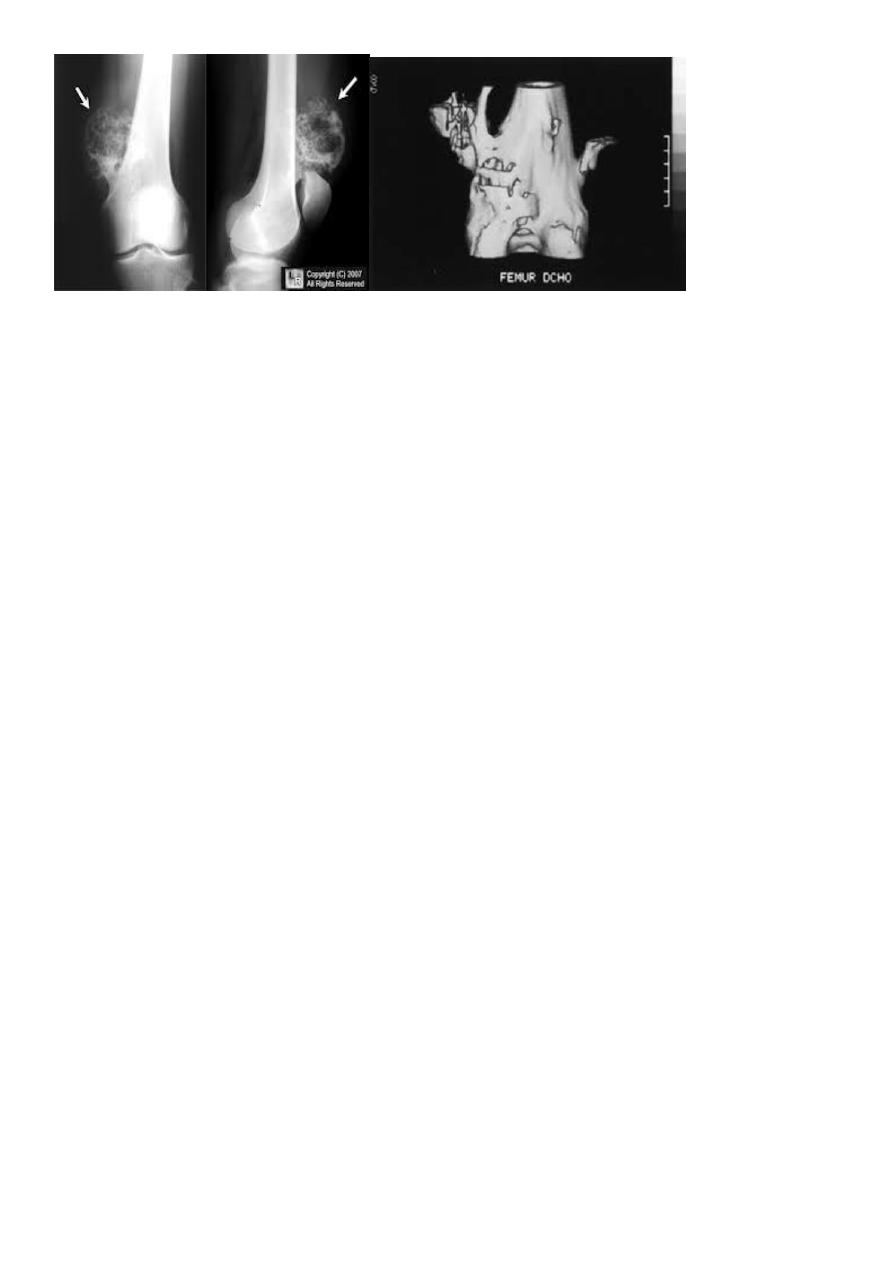
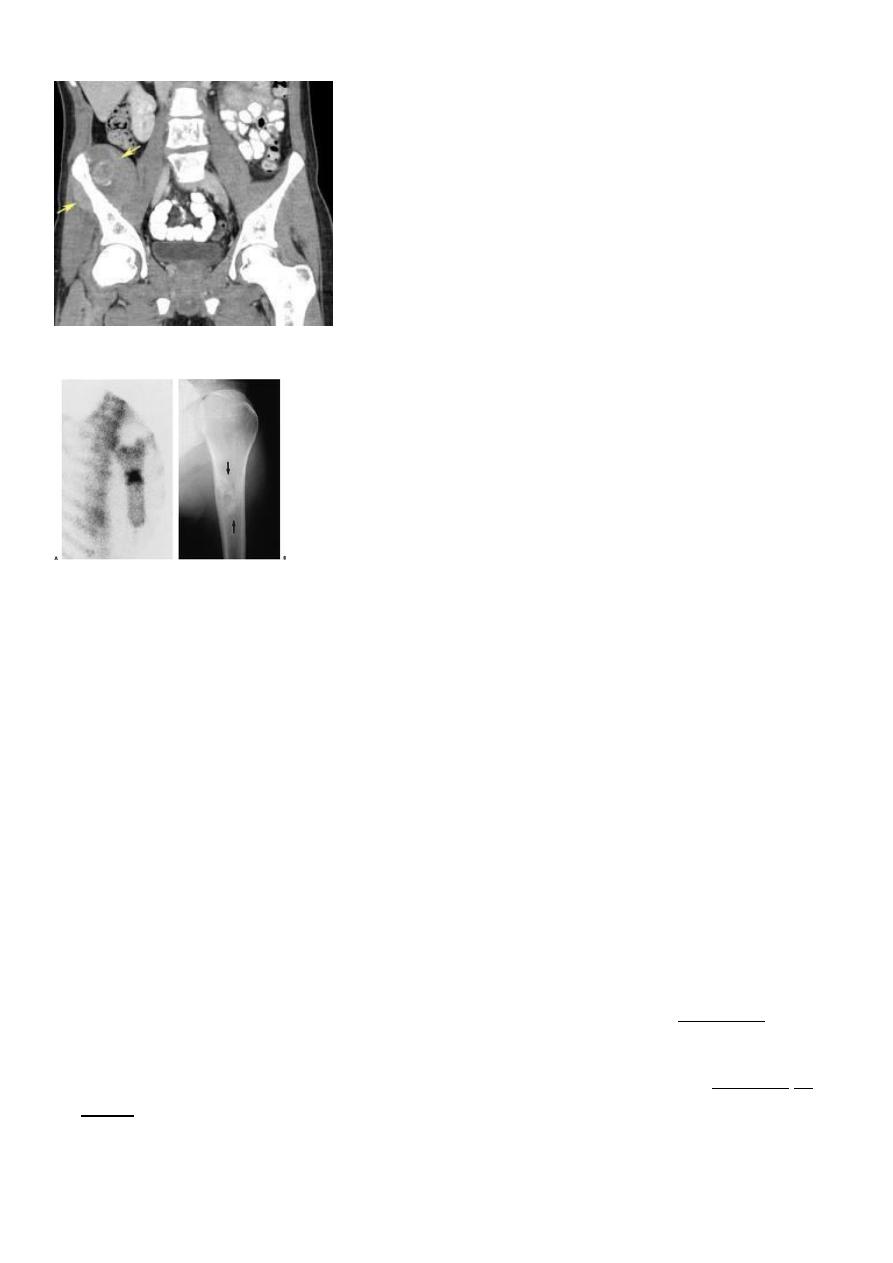
X-rays :
show a radiolucent area situated eccentrically at the end of a long bone and bounded by
the sub- chondral bone plate.
The endosteal margin may be quite obvious, but in aggressive lesions it is ill-defined.
The Centre sometimes has a soap-bubble appearance.
The cortex is thin and sometimes ballooned. aggressive lesions extend into the soft tissue.
7
The appearance of a ‘cystic’ lesion in mature bone, extending right up to the subchondral
plate, is so characteristic
Other investigations :
blood calcium, phosphate and alkaline phosphatase concentrations so as exclude an
unusual ‘brown tumour’ associated with hyper parathyroidism.
CT scans and MRI will reveal the extent of the tumour, both within the bone and
beyond.
Biopsy
:
Is essential. This can be done either as a frozen section before proceeding with
operative treatment or (especially if a more extensive operation is contemplated) as a
separate procedure
Treatment
Well-confined, slow-growing lesions with benign histology can safely be treated by
thorough curettage and ‘stripping’ of the cavity with burrs and gouges, followed by
swabbing with hydrogen peroxide or by the application of liquid nitrogen;
the cavity is then packed with bone chips.
Recurrence about 20-25%
Some time the cavity occupied with bone cement (methyl methacrylate)which is acting
through its exothermic action and mechanical supports to the subchondral bone and
cartilage.
More aggressive tumours, and recurrent lesions, should be treated by excision followed,
if necessary, by bone grafting or prosthetic replacement.
8
Tumours in awkward sites (e.g. the spine) may be difficult to eradicate; supplementary
radiotherapy is sometimes recommended.
but it carries a significant risk of causing malignant transformation
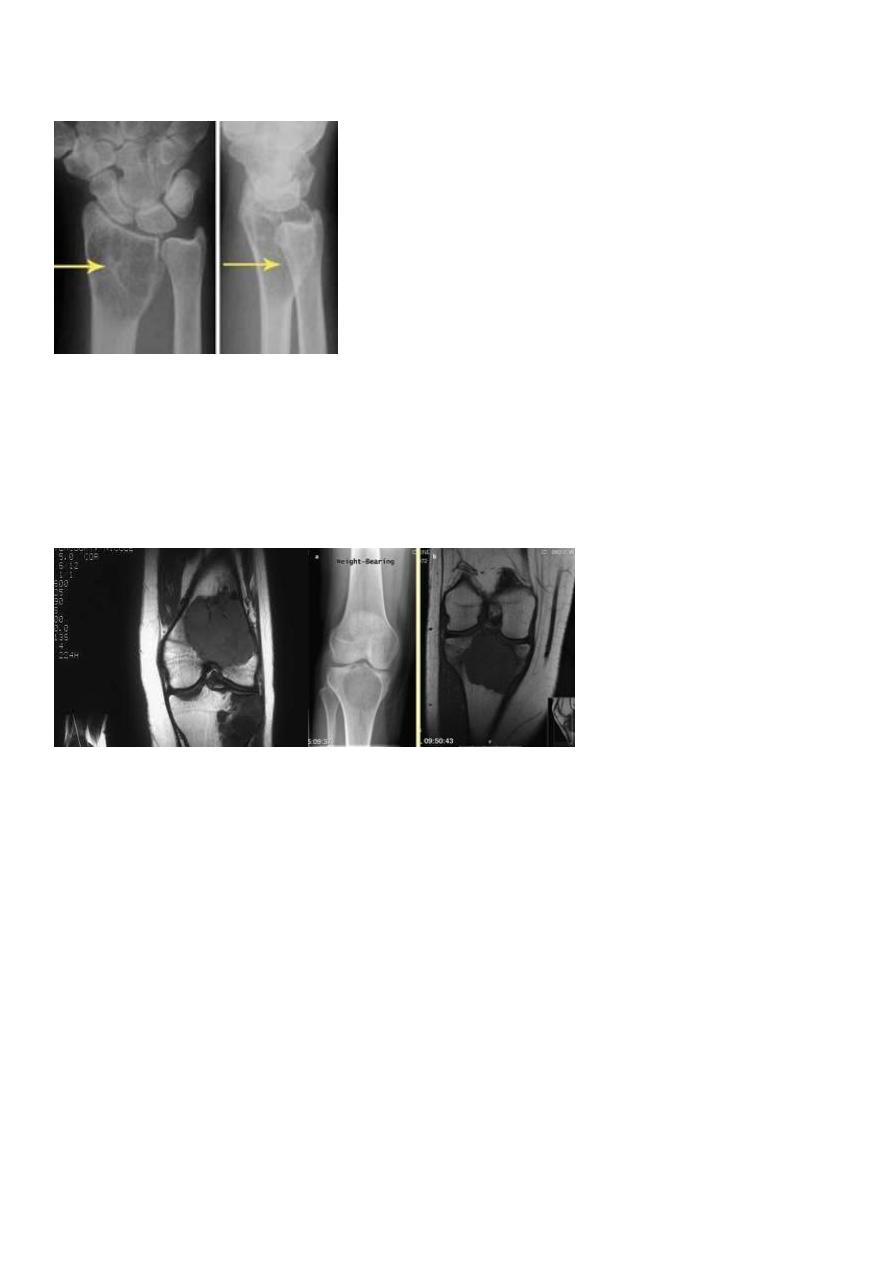
ANEURYSMAL BONE CYST
aneurysmal bone cyst may be encountered at any age and in almost any bone, though
more often in young adults.
Below 20 years age in 75%. 25% in spine. 20% long bones. in the long-bone metaphysis.
Usually it arises spontaneously but it may appear after degeneration or haemorrhage in
some other lesion.
With expanding lesions, patients may complain of pain.
Occasionally, a large cyst may cause a visible or palpable swelling of the bone.
X-rays
show a well-defined radiolucent cyst, often trabeculated and eccentrically placed.
In a growing tubular bone it is always situated in the metaphysis
and therefore may resemble a simple cyst or one of the other cyst-like lesions.
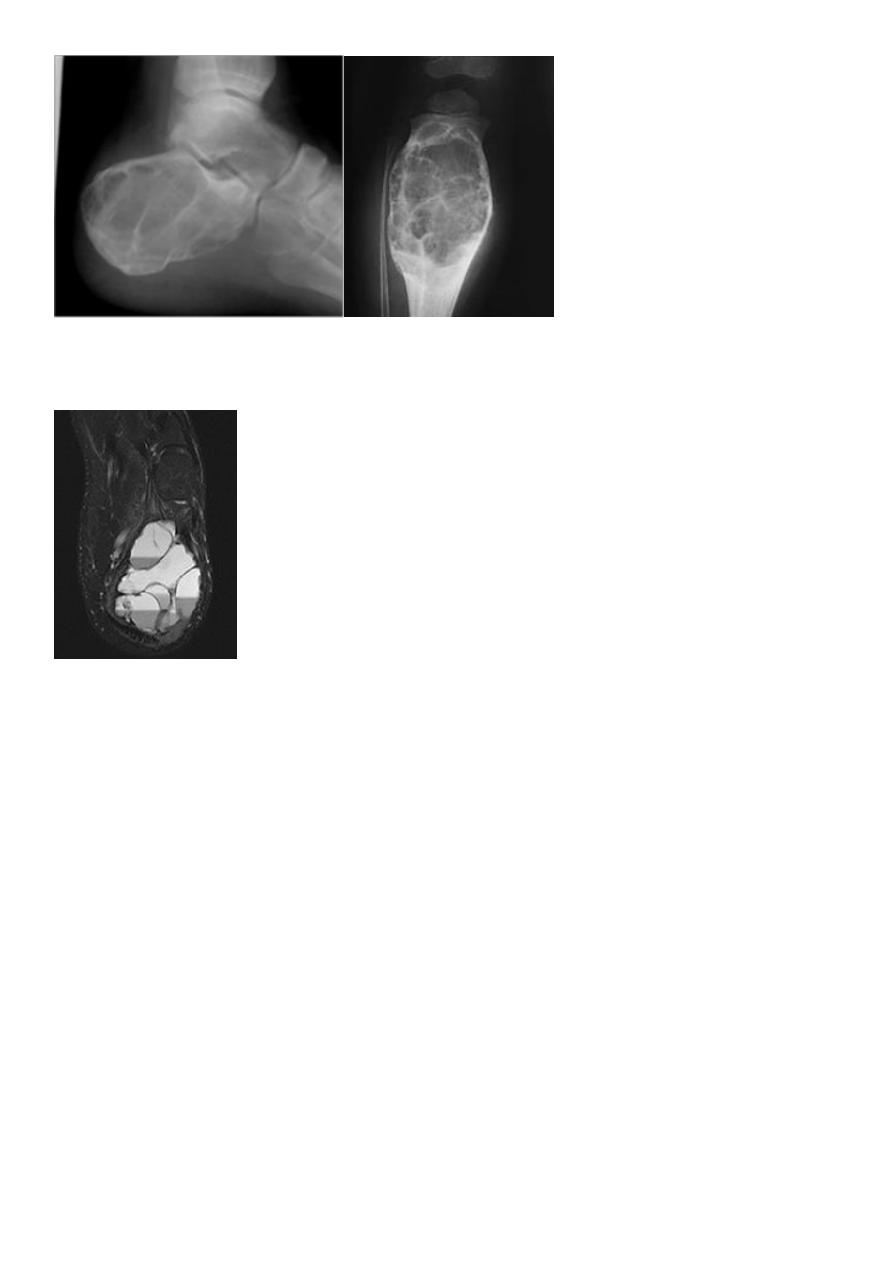
9
•MRI or CT scan ◦will show multiple fluid lines
•Bone scan ◦is warm to hot
Occasional sites include vertebrae. and the flat bones.
In an adult an aneurysmal bone cyst may be mistaken
for a giant-cell tumour
Chondroblastoma
Osteoblastoma
osteosarcoma
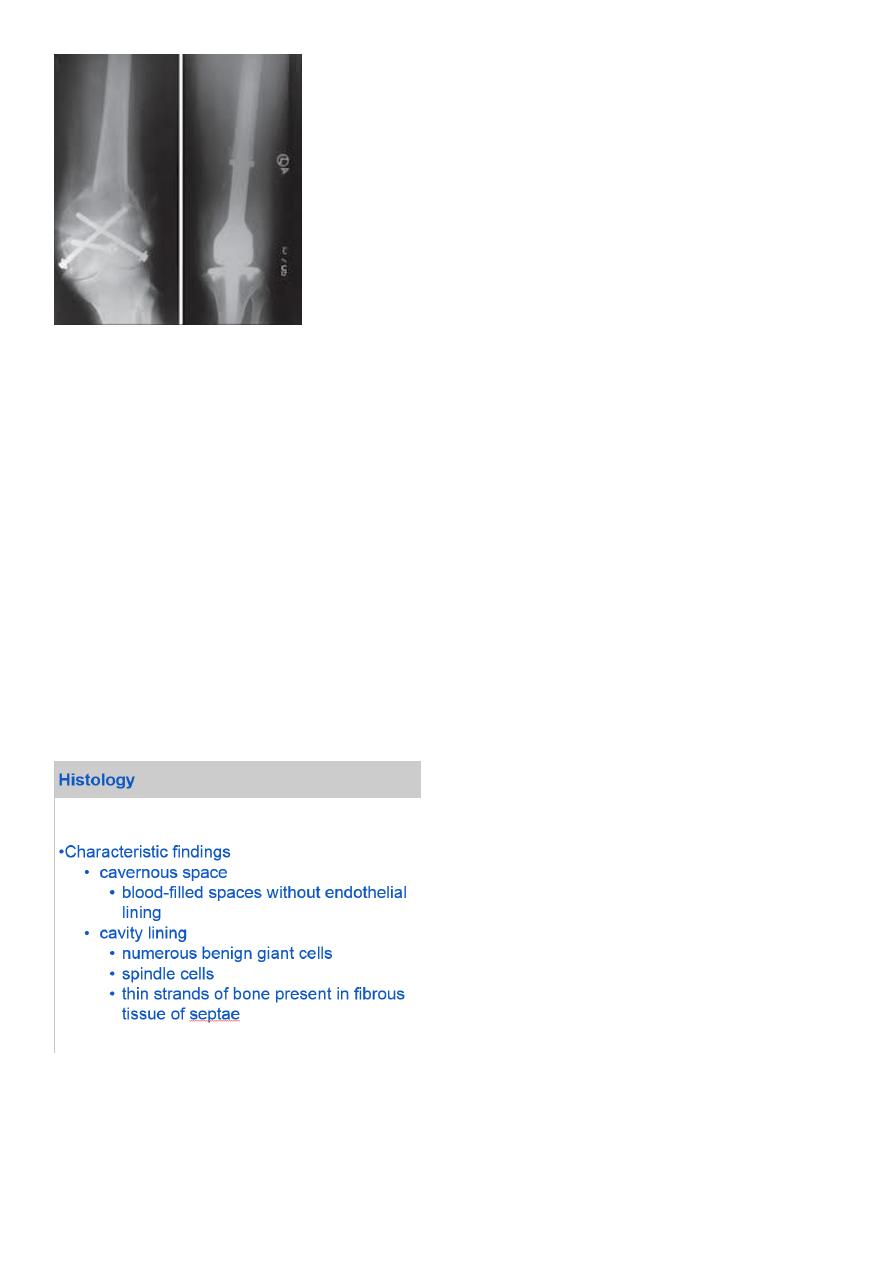
Pathology :
When the cyst is opened it is found to contain clotted blood, and during curettage there
may be considerable bleeding from the fleshy lining membrane.
Histologically
the lining consists of fibrous tissue with vascular spaces, deposits of haemosiderin and
multinucleated giant cells.
Occasionally the appearances so closely resemble those of giant-cell tumour
11
Treatment :
The cyst should be carefully opened, thoroughly curetted and then packed with bone
grafts.
Sometimes the graft is resorbed and the cyst recurs
necessitating a second or third operation.
In these cases, packing with methyl methacrylate cement may be more effective.
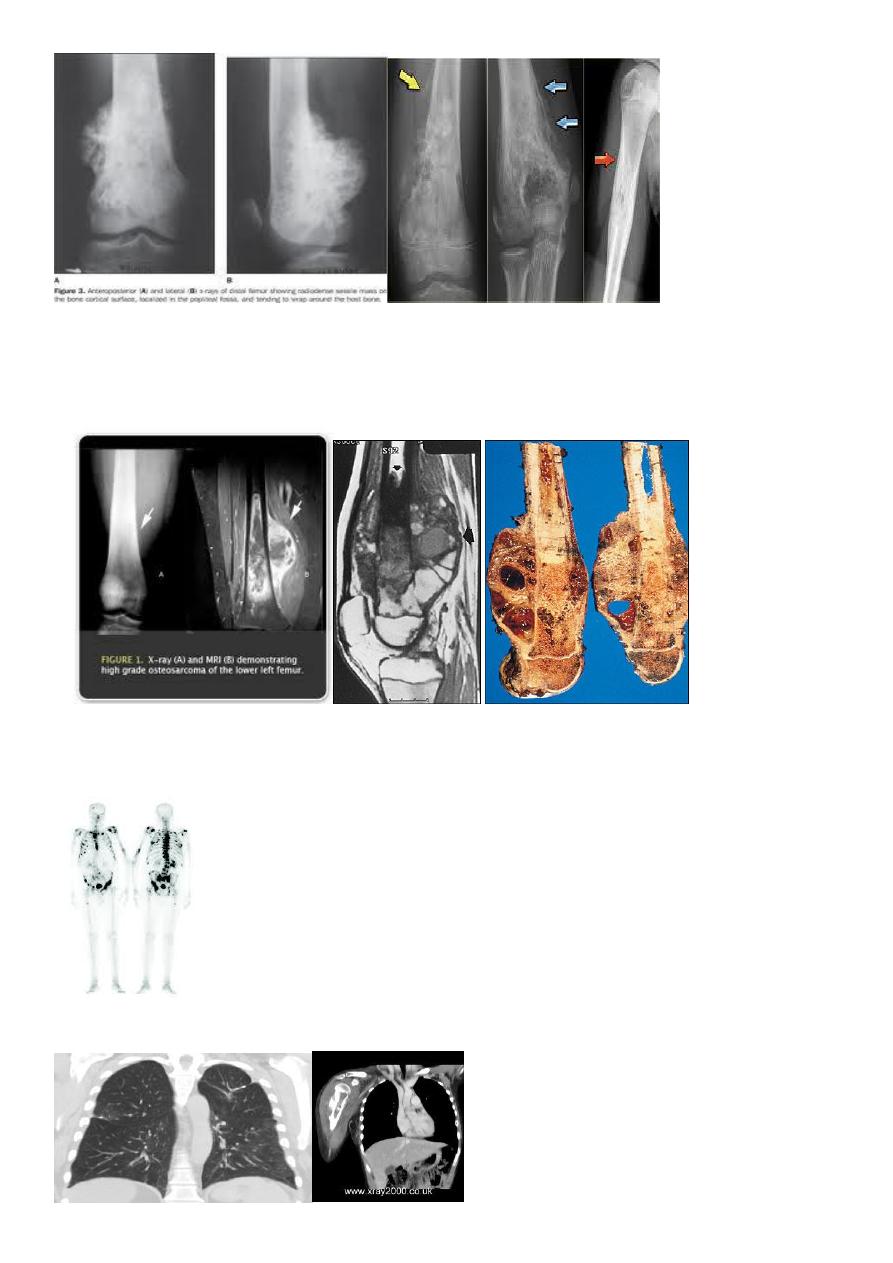
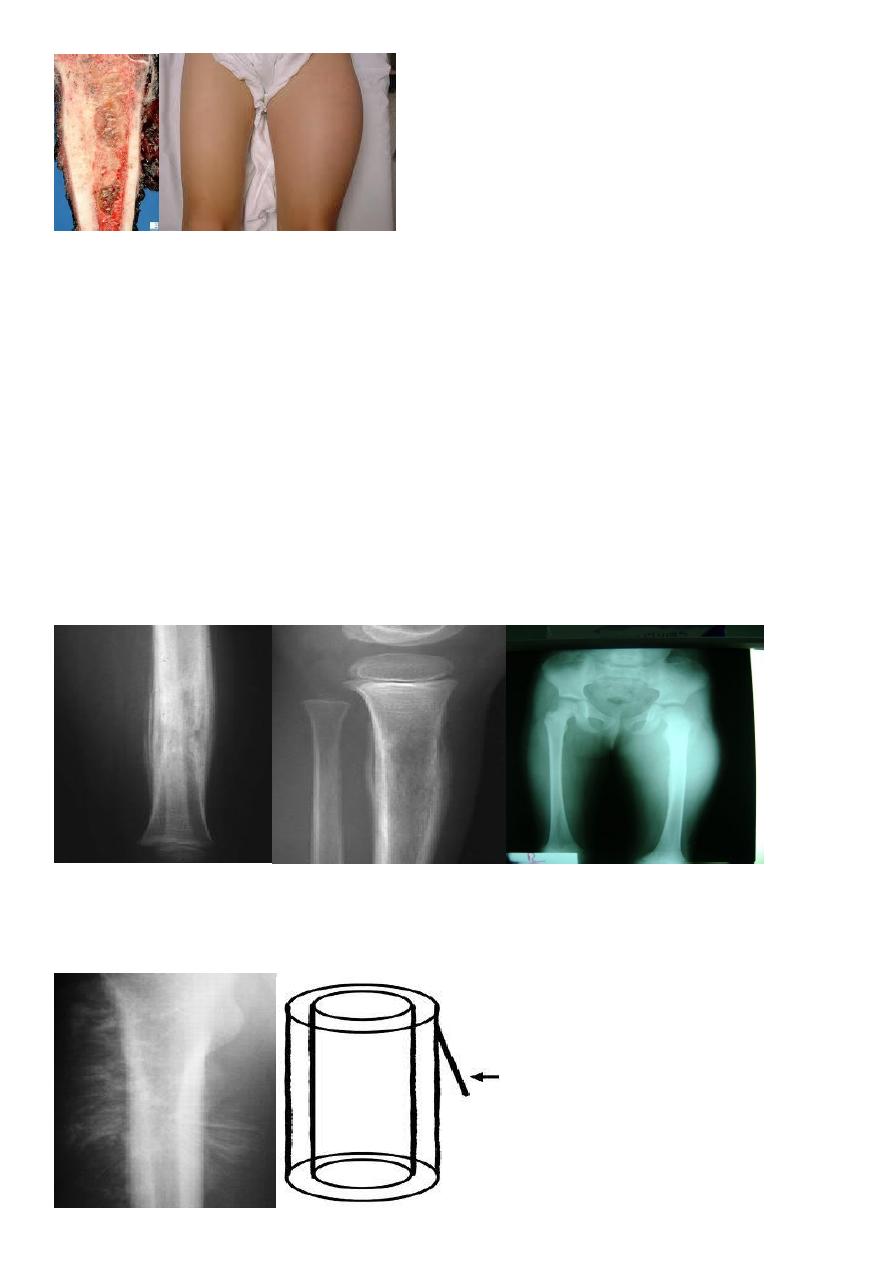
OSTEOSARCOMA}
highly malignant tumour arising within the bone andspreading rapidly outwards to the
periosteum and surrounding soft tissues. It is said to occur predominantly in children and
adolescents, 10-25 years
may affect any bone but most commonly involves the long-bone metaphysis, especially
around the knee and at the proximal end of the humerus.
Pathology
The tumour extend Within the medulla and across the physeal plate.
Obvious spread into the soft tissues with ossification at the periosteal margins and
streaks of new Bone extending into the extraosseous mass.
CLINICAL FEATURES
Pain is usually the first symptom; it is constant, Worse at night and gradually
increases in severity.
Sometimes the patient presents with a lump.
Pathological fracture is rare.
11
On examination
there may be little to find except local tenderness.
In later cases there is a palpable mass and the overlying tissues may appear swollen
and inflamed.
The over lying skin warmer than normal because of its vascularity.
The skin also shiny and stretched.
INVESTIGATIONS
The ESR is usually raised and there may be an increase in serum alkaline phosphatase
X-rays
variable hazy osteolytic . areas may alternate with unusually dense
Osteoblastic areas. The endosteal margin is poorly defined. Often The cortex
is breached .
The tumour extends into the adjacent tissues; when this happens.
Streaks of new bone appear, radiating outwards from the cortex – the so-called
‘sunburst’ effect.
Reactive new bone forms at the angles of periosteal elevation (Codman’s triangle).
12
MRI
Allow accurate delination of the tumor size and the extent of invasion to the near soft
tissue.
Radioactive isotops
Increased uptake. And the extension in to the medullary canal (skipped lesion).
CT and chest radiograph is mandatory for preoperative staging

13
Treatment:
The patient is admitted to a special center for biopsy.
The lesion will probably be graded IIA or IIB.
Multi-agent neoadjuvant chemotherapy is given for 8–12 weeks and then.
Provided the tumor is resectable and there are no skip lesions, a wide resection is
carried.
Replace that segment of bone with either a large bone graft or a custom-made implant;
in some cases an amputation may be more appropriate.
The specimen is examined to assess the response to preoperative chemotherapy.
If tumour necrosis is marked (more than 90 per cent),
Chemotherapy is continued for another 6–12 months;
If the response is poor, a different chemotherapeutic regime is substituted.
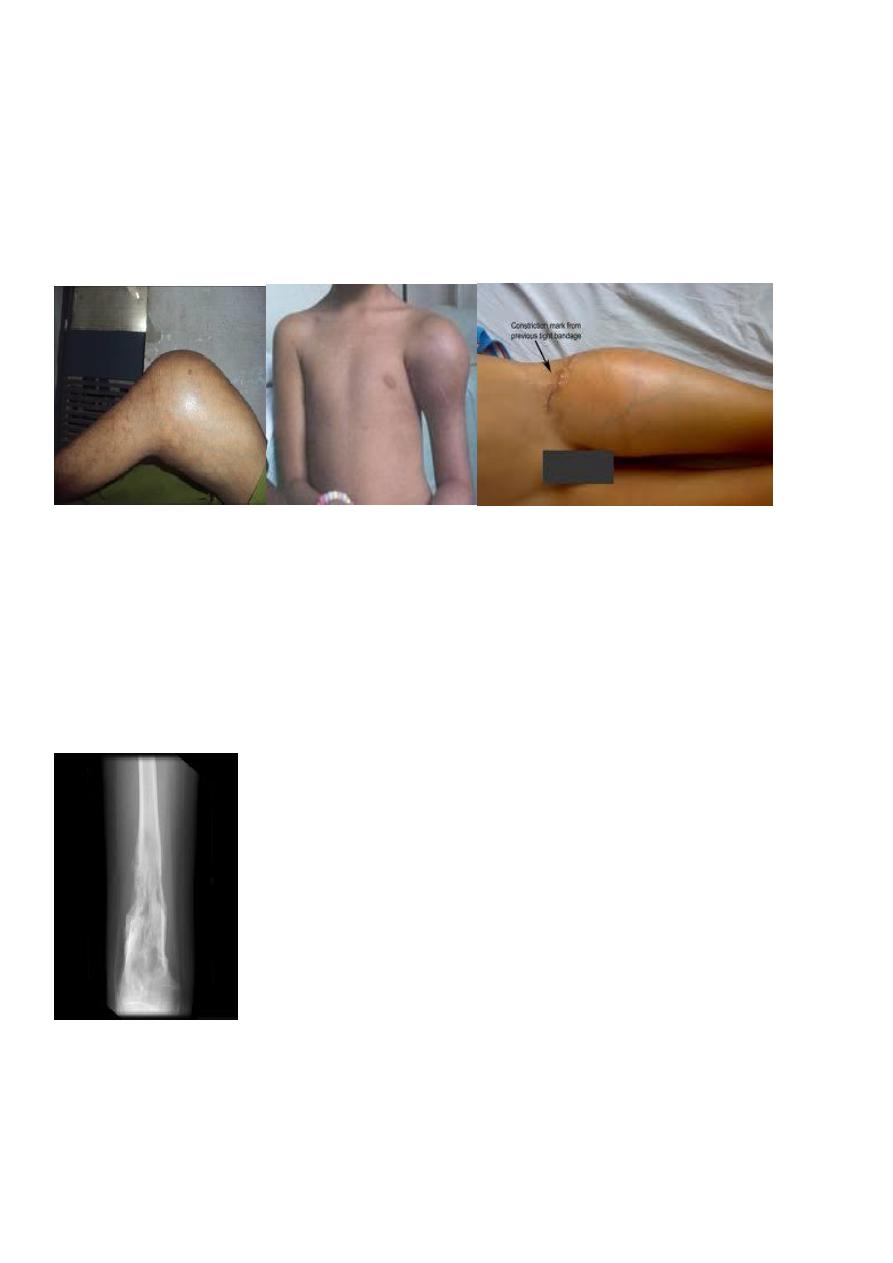
EWING SARCOMA
is believed to arise from endothelial cells in the bone marrow.
It occurs most commonly
between the ages of 10 and 20 years. usually in a tubular bone and especially in the
tibia, fibula or clavicle.
PATHOLOGY :
Macroscopically the tumour is lobulated.
It may look grey (like brain) or red (like redcurrant jelly) if haemorrhage has occurred
into it.
Microscopically, sheets of small dark polyhedral cells with no regular arrangement
and no ground substance are seen.
14
CLINICAL FEATURES
The patient presents with pain – often throbbing in character .
swelling.
Generalized illness .
pyrexia, together with a warm, tender swelling and. a raised ESR, may suggest a diagnosis
of osteomyelitis.
Imaging
X-rays usually show an area of bone destruction in the mid-diaphysis.
New bone formation may appears as fusiform layers of bone around the lesion – the so-
called ‘onion-peel’ effect.
Infiltration into the surrounding soft tissues, with radiating streaks of ossification and
reactive periosteal bone at the proximal and distal margins. These features (the‘sunray’
appearance and Codman’s triangles)
15
CT and MRI reveal the large extra osseous component.
Radioisotope scans may show multiple areas of activity in the skeleton.
Diagnosis
The condition which should be excluded as rapidly as possible is: bone infection.
reticulum-cell sarcoma . and metastatic neuroblastoma.
Treatment
Radiotherapy has a dramatic effect.
Chemotherapy is much more effective,5-year survival rate of about 50 %.
The best results are achieved by a combination of all three methods.
a course of preoperative neoadjuvant chemotherapy; then wide excision .
or radiotherapy followed by local excision if it is less accessible; and then a further
course of chemotherapy for 1 year.
SIMPLE BONE CYST
also known as a solitary cyst or unicameral bone cyst) appears during childhood,
typically in the
metaphysis of one of the long bones and most commonly in the proximal humerus or
femur.
Pathology
The lining membrane consists of flimsy fibrous tissue, often containing giant cells. In an

16
actively growing cyst, there is osteoclastic resorption of the adjacent bone.
Clinical features
The condition is usually discovered after a pathological fracture or as an incidental
finding on x-ray.
it tends to heal spontaneously and it is seldom seen in adults.
X-rays
show a well-demarcated radiolucent area in the metaphysis, often extending up to the
physeal plate.
the cortex may be thinned and the bone expanded.
DDx
Non-osteogenic fibroma,
fibrous dysplasia .
benign cartilage tumours are solid and merely look cystic on x-ray.
Treatment
Treatment depends on whether the cyst is symptomatic, actively growing or
involved in a fracture. Asymptomatic lesions in older children can be left alone.
Active’ cysts
usually abutting against the physeal plate and obviously enlarging in sequential x-rays.
should be treated, in the first instance, by aspiration of fluid and injection of 80–160 mg
of methylprednisolone.
or autogenous bone marrow. This often stops further enlargement and leads to healing
of the cyst.
17
If the cyst goes on enlarging or if there is a pathological fracture. the cavity should be
thoroughly cleaned by curettage and then packed with bone chips.
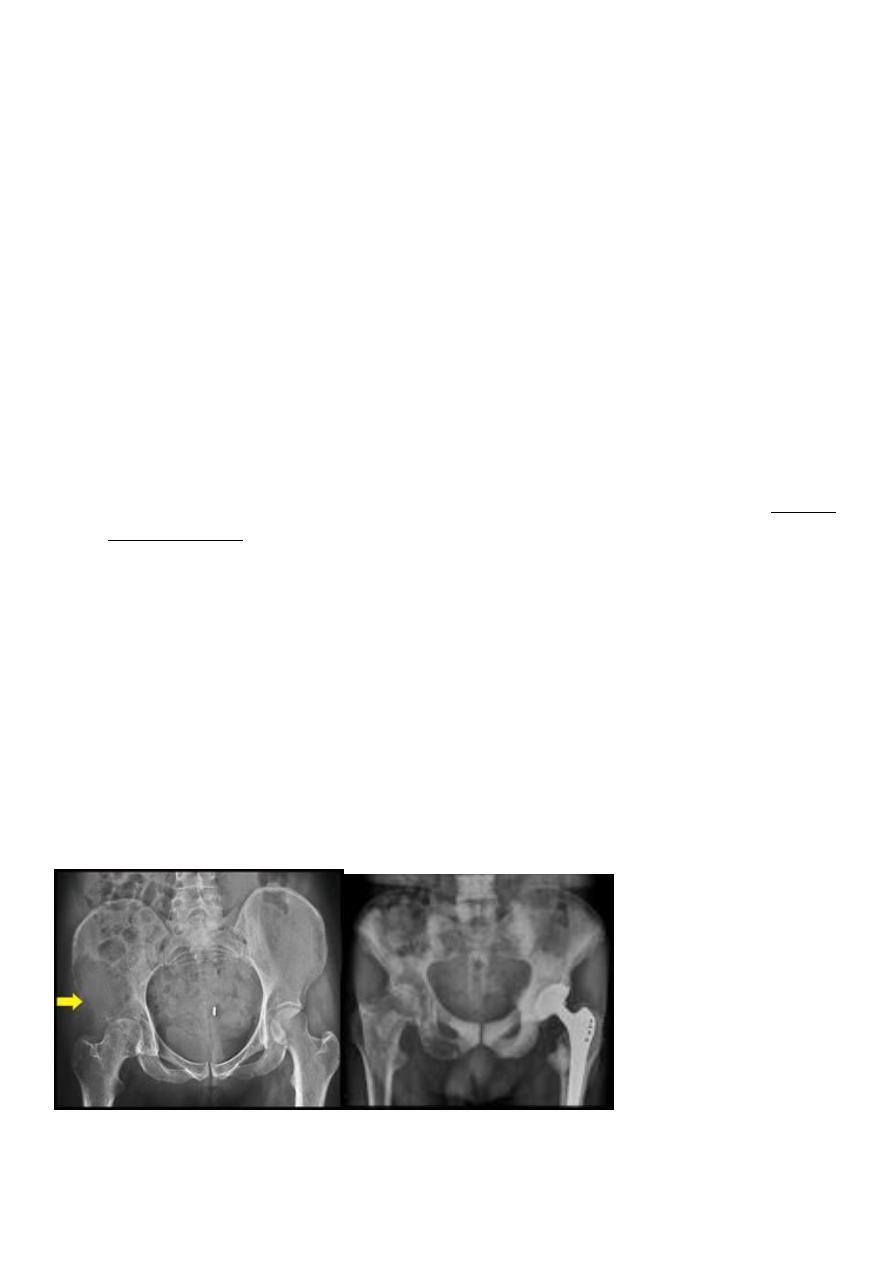
METASTATIC BONE DISEASE
The skeleton is one of the commonest sites of secondary cancer; in patients over 50
years bone metastases are seen more frequently than all primary malignant bone
tumours together.
The commonest source
is carcinoma of the breast;
prostate,
kidney,
lung,
thyroid,
bladder and
gastrointestinal tract.
In about 10 per cent of cases no primary tumour is found.
For bone metastases are the commonest sites
Vertebrae,
pelvis,
proximal half of the femur and
humerus.
Spread is usually via the blood stream;
occasionally, visceral tumours spread directly to adjacent bones (e.g. the pelvis or ribs).
Metastases are usually osteolytic, and pathological fractures are common.
Bone resorption is due either to the direct action of tumour cells or to tumour-derived
factors that stimulate osteoclastic activity.
Osteoblastic lesions are uncommon; they usually occur in prostatic carcinoma.
18
Clinical features
The patient is usually aged 50–70 years; with any destructive bone lesion in this age group,
the differential diagnosis must include metastasis.
Pain is the commonest – and often the only – clinical feature.
The sudden appearance of backache or high pain in an elderly person (especially
some one to have been treated for carcinoma in the past). always suspicious. If x-rays
do not show anything.
Some deposits remain clinically silent and are discovered incidentally on x-ray
examination or bone scanning. or after a pathological fracture. Sudden collapse of a
vertebral body . or a fracture of the mid-shaft of a long bone in an elderly person are
ominous signs;
Symptoms of hypercalcaemia may occur . often missed in patients with skeletal
metastases These include anorexia, nausea, thirst, polyuria
In children under 6 years of age, metastatic lesions are most commonly from adrenal
neuroblastoma.
The child presents with bone pain and fever; Examination reveals the abdominal
mass.
Imaging
Most skeletal deposits are osteolytic and appear as rarified areas in the medulla or
produce a moth-eaten appearance in the cortex.
sometimes there is marked bone destruction, with or without a pathological
fracture.
Osteoblastic deposits suggest a prostatic carcinoma; the pelvis may show a mottled
increase in density which has to be distinguished from Paget’s disease Or lymphoma.

19
Radioscintigraphy
Bone scans with 99mTc-MDP are the most sensitive method of detecting ‘silent’ metastatic
deposits in bone; areas of increased activity are selected for x-ray examination.
Special investigations
The ESR may be increased and the haemoglobin con- centration is usually low.
The serum alkaline phosphatase concentration is often increased, and in acid
phosphatase also is elevated.
Patients with breast cancer can be screened by measuring blood levels of tumour-
associated antigen markers.
Treatment
By the time a patient has developed secondary deposits the prognosis for survival is poor.
Occasionally, radical treatment (combined chemotherapy radiotherapy and surgery).
hormonal manipulation.
