
1
Fifth stage
Surgery-Ortho
Lec- 0
1
د. هشام القطان
1/1/2014
CEREBRAL PALSY
a group of disorders that result from non-progressive brain damage during early
development and are characterized by abnormalities of movement and posture
Causal factors are
:
maternal toxaemia,
prematurity,
perinatal anoxia,
kernicterus and postnatal brain infections
birth injury, though often blamed, is a distinctly unusual cause.
Classification
:
Spasticity , is the commonest muscle movement disorder
and is associated with
damage to the pyramidal
system in the CNS.
Hypotonia , is usually a phase, lasting several years
during early childhood before the
features of spasticity
become obvious
Athetosis. manifests as continuous, involuntary,
writhing movements which may be
exacerbated
when the child is frightened. It is caused by damage
to the extrapyramidal
systems of the CNS.
Dystonia, There is a more generalized increase in muscle tone and abnormal positions
induced by activity.
Ataxia. appears in the form of muscular incoordination during voluntary movements. It
is usually due to cerebellar damage.
Mixed palsy, appears as a combination of spasticity and athetosis
TOPOGRAPHIC DISTRIBUTION
Hemiplegia
Is the commonest. This usually appears as a spastic palsy on one side of the body.
Diplegia
involves both sides of the body, with the
lower limbs always most severely affected

2
Total body involvement
describes a general and often more severe disorder affecting all four limbs
Monoplegia
occasionally appears in an upper limb
Diagnosis in infancy
A history of prenatal toxaemia,
haemorrhage,
premature birth,
difficult labour,
foetal distress or
kernicterus should arouse suspicion
Early symptoms
include difficulty in sucking and
swallowing, with dribbling at the mouth. The mother
may notice that the baby feels stiff or wriggles awkwardly.
Diagnosis in later childhood
Most children presenting to the orthopaedic surgeon have already had the diagnosis
made.
Occasionally, for example with a mild hemiplegia or a symmetrical mild diplegia, the
diagnosis has not been made and the child is simply referred for advice about their gait
or their tendency to trip and fall
Tests for diagnosis in children over 1 year
The primitive neck-righting reflex,
asymmetrical and symmetrical tonic neck reflexes,
the Moro reflex and the extensor thrust
response should all have disappeared at 1 year of age.
Children who retain more than two primitive reflexes
after that age,
3
cannot sit unsupported by 4 years and
cannot walk unaided by 8 years are unlikely ever to
walk independently
Ideally the child should be reviewed by a multidisciplinary
team so that speech, hearing, visual acuity,
intelligence and motivation can also be assessed.
Management
Medical treatment
Baclofen, acts by inhibiting reflex activity
Dantrolene. produces weakness without much reduction in spasticity
Analgesic medication , for the reduction of pain associated with musculoskeletal
problems
Botulinum toxin, This potent neurotoxin is produced by Clostridium botulinum; it acts
by blocking acetyl choline release at the neuromuscular junction. The preparation is
injected into the ‘spastic’ muscle
Physical therapy
Manipulation and serial casting
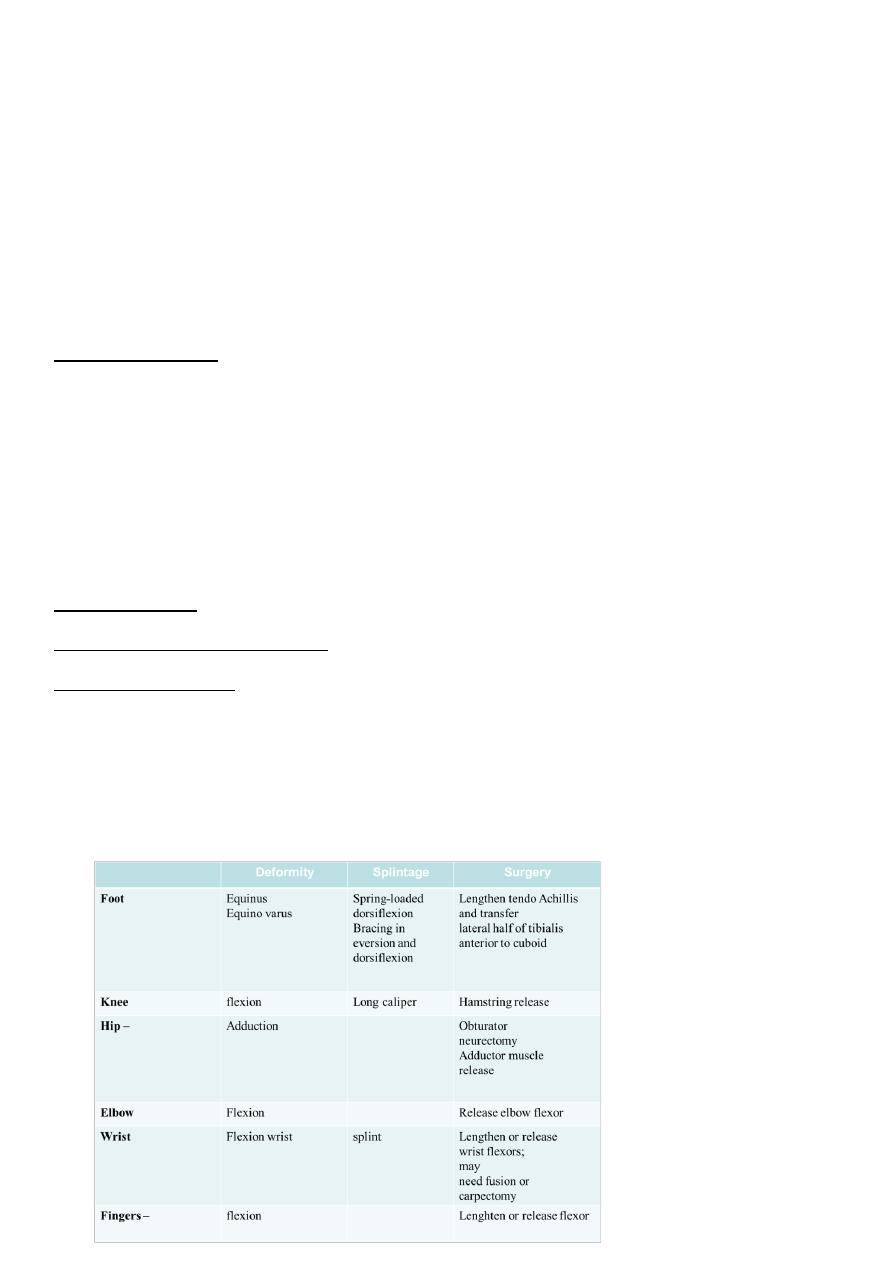
Operative treatment
The indications for surgery are:
(1) a spastic deformity which cannot be controlled by conservative measures;
(2) fixed deformity that interferes with function; and
(3) secondary complications such as bony deformities, dislocation of the hip and joint
instability.

4
POLIOMYELITIS
Poliomyelitis is an acute infectious viral disease,
Spread by the oropharyngeal route, that passes through several distinct phases.
Clinical features
Poliomyelitis typically passes through several clinical phases,
from an acute illness resembling meningitis to
paralysis, then
slow recovery or convalescence
and finally the long period of residual paralysis.
The disease strikes at any age but most commonly in children
The acute illness
Early symptoms are
fever and
Headache.
in about one-third of cases the patient gives a history of a minor illness with sore
throat, mild headache and slight pyrexia 5–7 days before
Paralysis
Soon muscle weakness appears; it reaches a
peak in the course of 2–3 days and may give rise to difficulty with breathing and
swallowing.
Recovery and convalescence
A return of muscle power
is most noticeable within the first 6 months, but there
may be continuing improvement for up to 2 years.
Post polio syndrome
5
Treatment
Depending on the stage .
Stage of onset.
Greatest paralysis.
Recovery.
Residual deformity.
Early treatment
During the acute phase the patient is isolated and kept at complete rest, with
symptomatic treatment for pain and muscle spasm. Active movement is avoided but
gentle passive stretching helps to prevent contractures.
Late treatment
Passively correctible deformity
Residual paralysis
Fixed deformity
Flail joint
Shortening
Vascular dysfunction Sensation is intact but the paralyzed limb is often cold and blue
Operative treatment
Two main group of operations
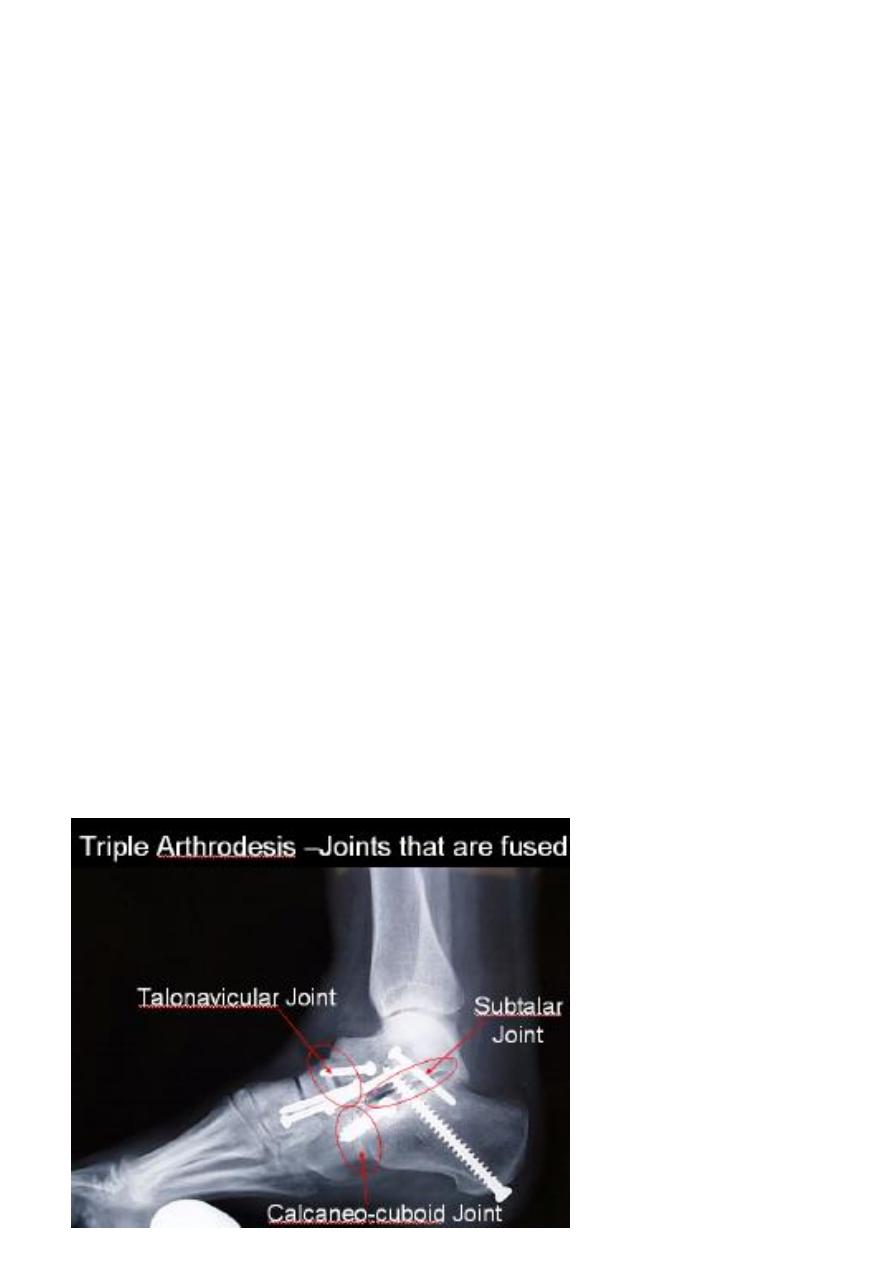
Arthrodesis of joints.
Muscle or tendon transfers.
