1
Fifth stage
Surgery-Ortho
Lec-14
د . هشام
1/1/2014
frcature spine and peripheral nerve
Peripheral nerve lesion
Peripheral nerves are bundles of axons conducting efferent (motor) impulses from cells in
the anterior horn of the spinal cord to the muscles, and afferent (sensory) impulses from
peripheral receptors via cells in the posterior root ganglia to the cord.
They also
convey sudomotor and vasomotor fibers from ganglion cells in the sympathetic chain.
Classifications Seddon's classification
1. Neurapraxia
-- temporary paralysis of a nerve caused by lack of blood flow or by pressure on the
affected nerve with no loss of structural continuity
2. Axonotmesis –
neural tube intact, but axons are disrupted.
nerves are likely to recover.

2
3. Neurotmesis –
the neural tube is severed.
Injuries are likely permanent without repair.
PATHOLOGY
Nerves can be injured by
1.ischaemia.
2.Compression.
3.Traction. 4.Laceration.
5.or burning.
Transient ischaemia
Acute nerve compression causes numbness and tingling within 15 minutes, loss of pain
sensibility after 30 minutes and muscle weakness after 45 minutes. Relief of compression is
followed by intense paraesthesiae lasting up to 5 minutes (the familiar ‘pins and needles’
after a limb ‘goes to sleep’); feeling is restored within 30 seconds and full muscle power
after about 10 minutes.
OBSTETRICAL BRACHIAL PLEXUS PALSY
caused by excessive traction on the brachial plexus during childbirth, e.g. by pulling the
bay’s head away from the shoulder or by exerting traction with the baby’s arm in
abduction.
Three patternsare seen:
(1) upper root injury (Erb’s palsy), typically in overweight babies with shoulder dystocia at
delivery;
(2) lower root injury (Klumpke’s palsy), usually after breech delivery of smaller babies; and
(3) total plexus injury.
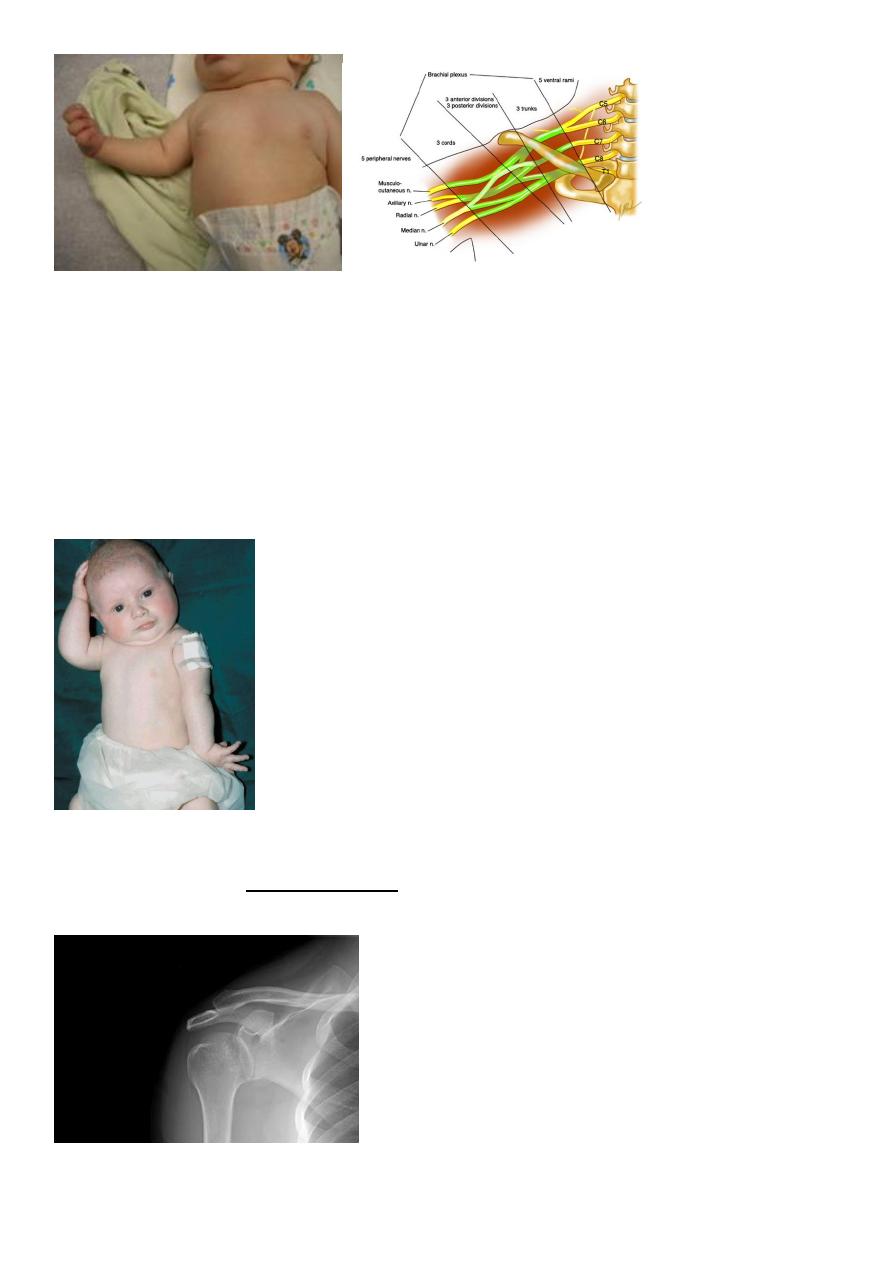
3
Clinical features
Erb’s palsy is caused by injury of C5, C6 and (sometimes) C7. The abductors and external
rotators of the shoulder and the supinators are paralysed.
The arm is held to the side, at birth: after a difficult delivery the baby has a floppy or flail
arm.
internally rotated and pronated.
There may also be loss of finger extension.
Sensation cannot be tested in a baby.
X-rays
should be obtained to exclude fractures of the shoulder or clavicle (which are not
uncommon and which can be mistaken for obstetrical palsy).
Management
4
Over the next few weeks one of several things may happen.
Paralysis may recover completely.
Paralysis may be partially resolve.
Paralysis may remain especially in the presence of a Horner’s syndrome
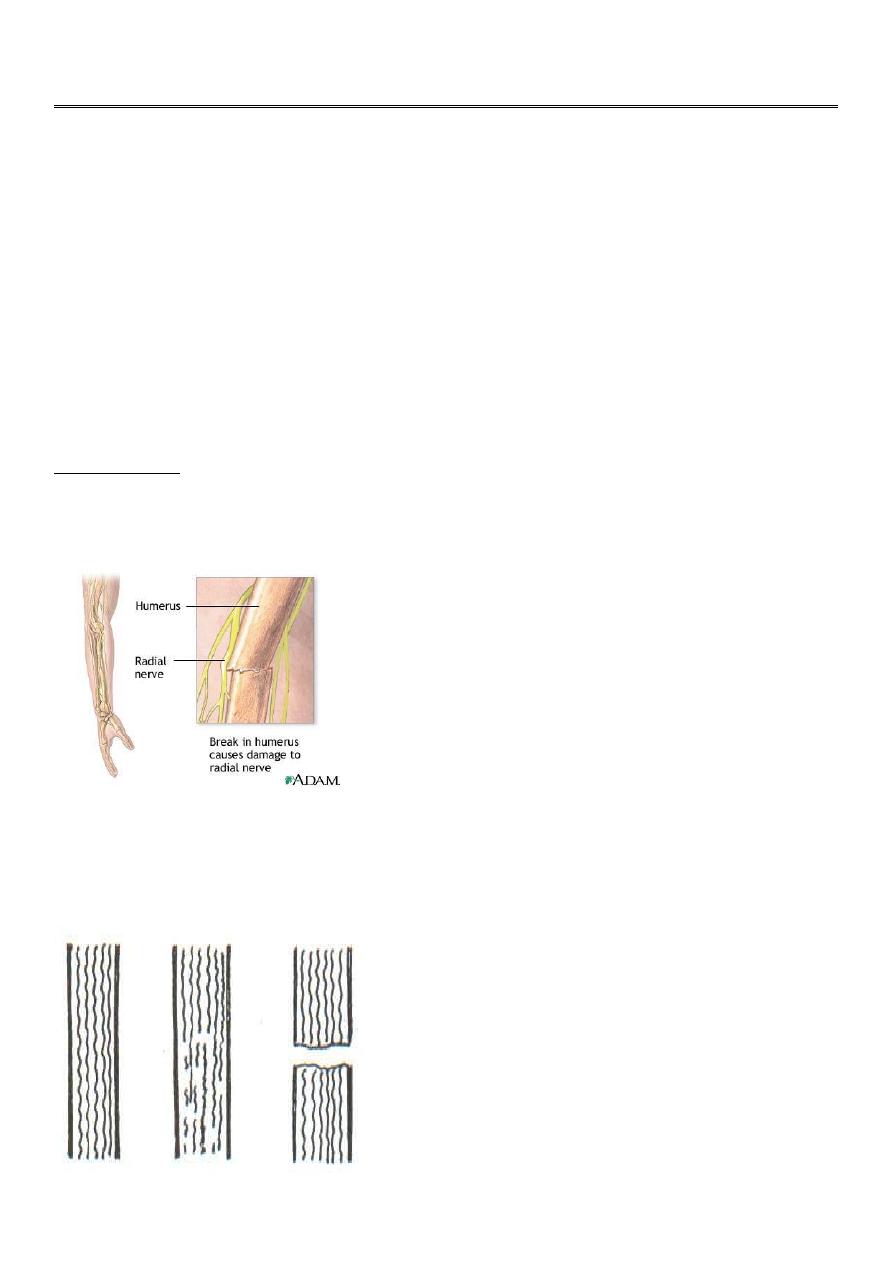
RADIAL NERVE
The radial nerve may be injured at the elbow. in the upper arm or in the axilla.
Clinical features
High and Low lesions are usually due to fractures or dislocations at mid shaft of humerus or
at the elbow, or to a local wound. after operations on the proximal end of the radius.
The patient complains of clumsiness and, on testing, cannot extend the
metacarpophalangeal joints of the hand. In the thumb there is also weakness of extension.

5
Treatment
Open injuries should be explored and the nerve repaired or grafted as soon as possible.
Closed injuries
In patients with fractures of the humerus it is important to examine for a radial nerve injury
on admission, beforetreatment and again after manipulation or internal fixation.
If the palsy is present on admission, one can afford to wait for 12 weeks to see if it starts to
recover. If it does not, then EMG should be performed;
While recovery is awaited,
Physiotherapy
The wrist is splinted in extension. ‘To over come fixed contractures
6
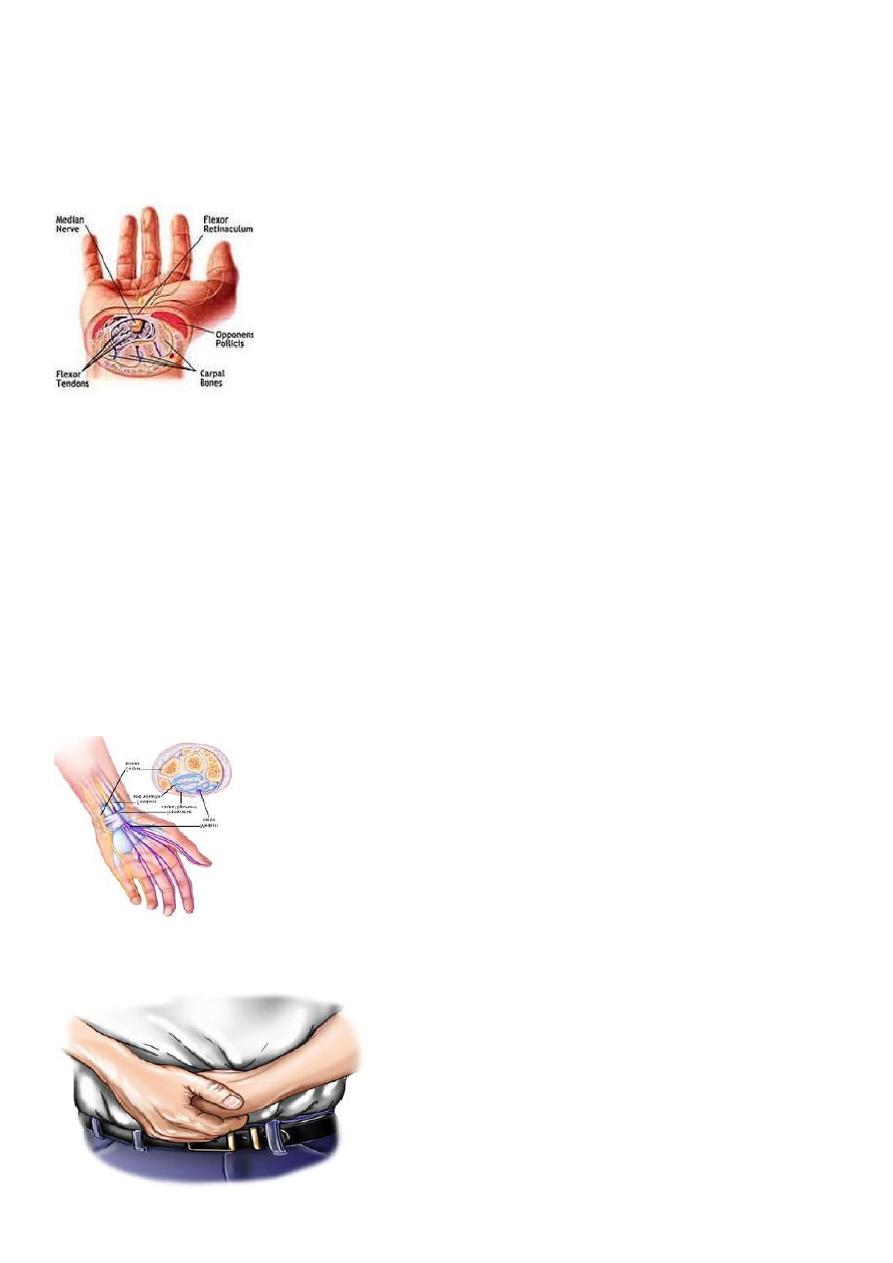
CARPAL TUNNEL SYNDROME
In the normal carpal tunnel there is barely room for all the tendons and the median nerve;
consequently,
any swelling is likely to result in compression and ischaemia of the nerve.
the syndrome is, however, common
• at the menopause.
• in rheumatoid arthritis.
• pregnancy.
• and myxoedema.
Clinical features
The history is most helpful in making the diagnosis.
Pain and paraesthesia occur in the distribution of the median nerve in the hand.
Night after night the patient is woken with burning pain, tingling and numbness.

7
• Hanging the arm over the side of the bed, or shaking the arm, may relieve the
symptoms.
• In advanced cases there may be clumsiness and weakness
The condition is far more common in women than in men.
The usual age group is 40–50 years;
younger patients it is not uncommon to find related factors such as pregnancy, rheumatoid
disease, chronic renal failure or gout.
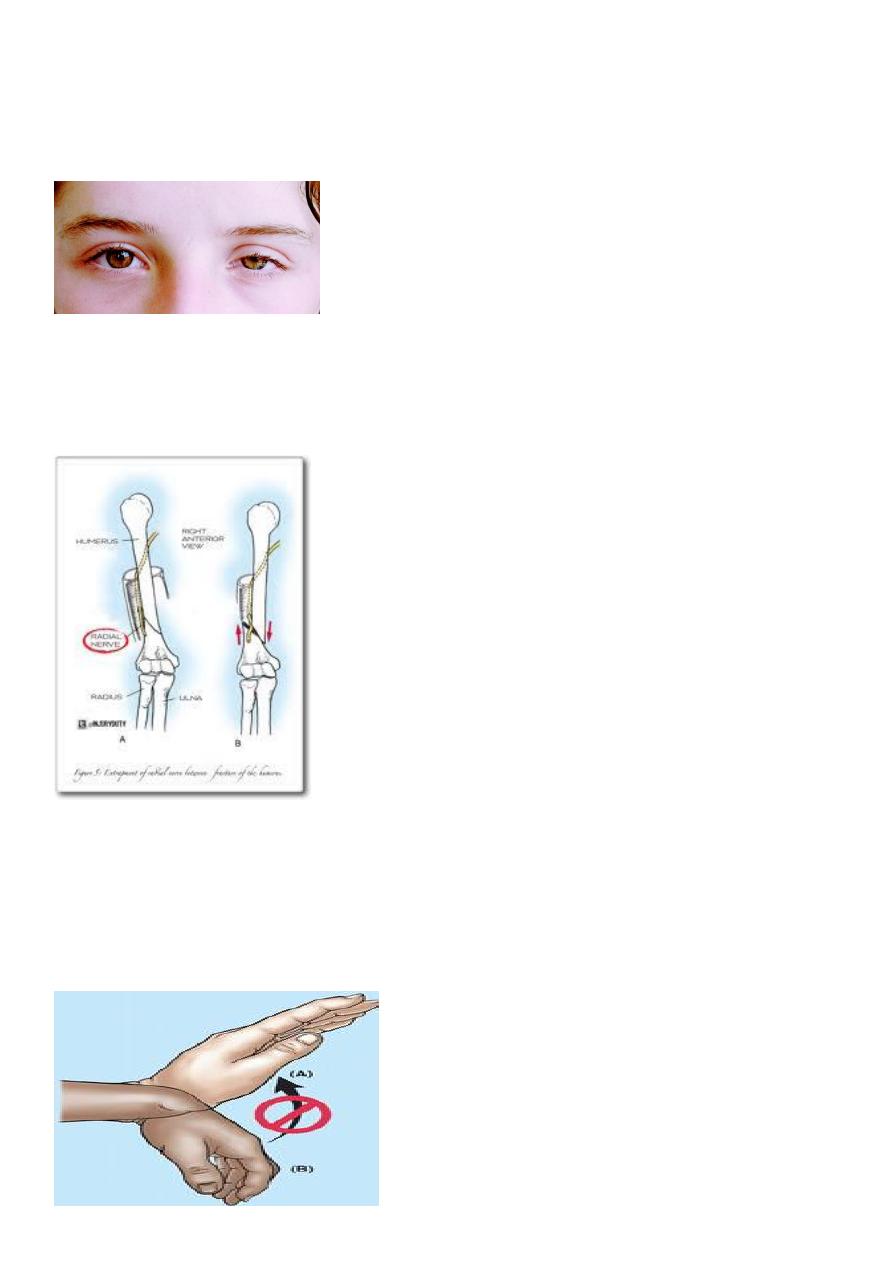
Clinical sign
Sensory symptoms can often be reproduced by percussing over the median nerve (Tinel’s
sign) or by holding the wrist fully flexed for less than 60 seconds (Phalen’s test).
8
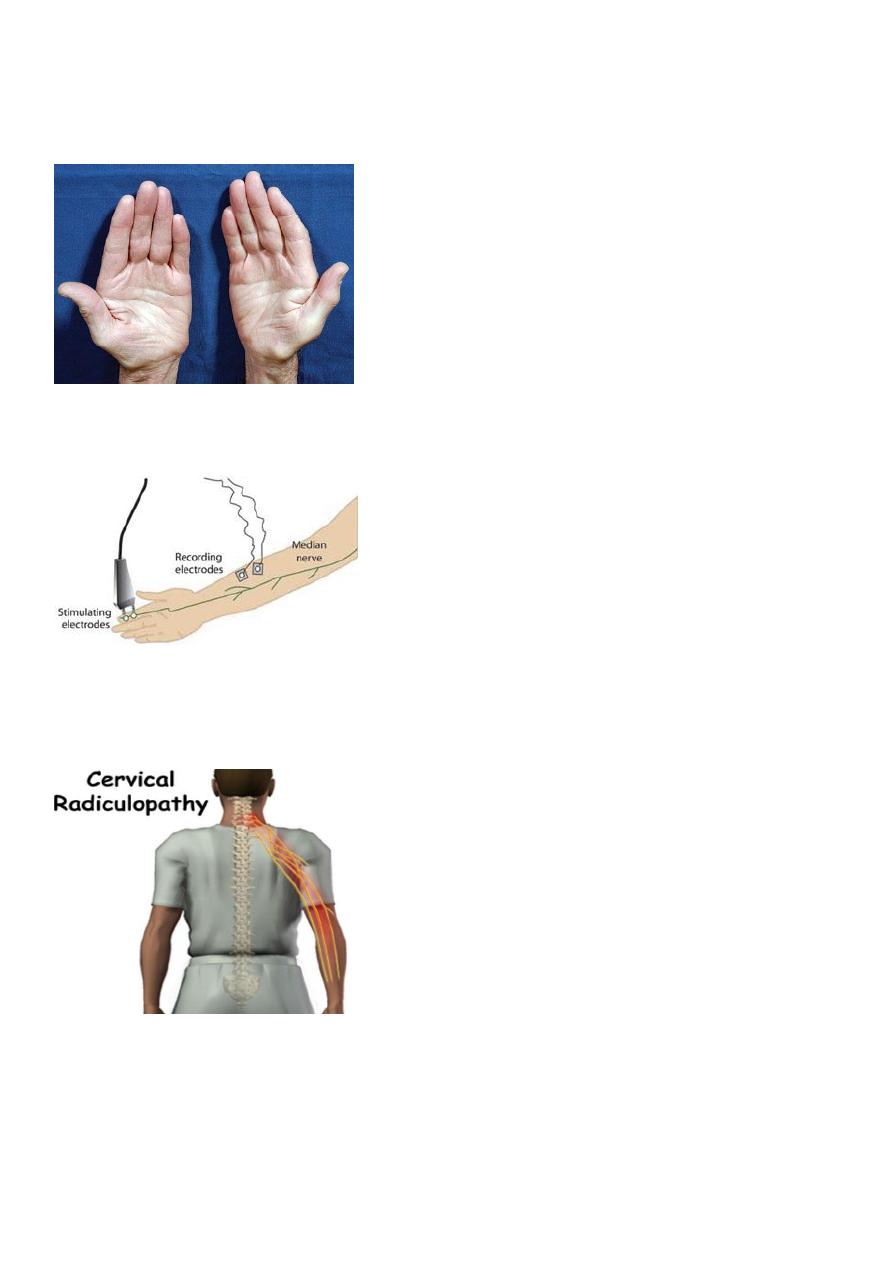
In late cases
there is wasting of the thenar muscles. weakness of thumb abduction and sensory dulling in
the median nerve territory.
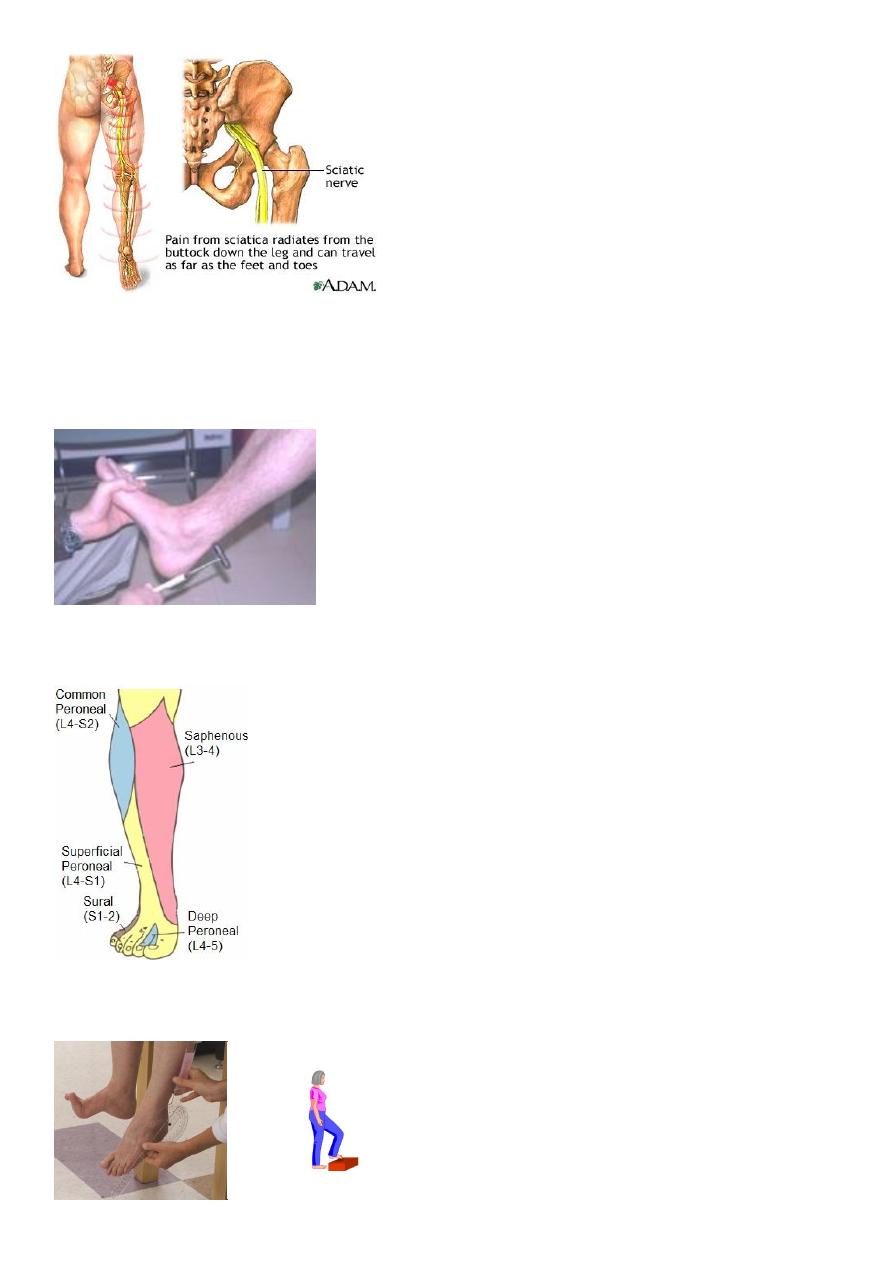
Electrodiagnostic tests
which show slowing of nerve conduction across the wrist
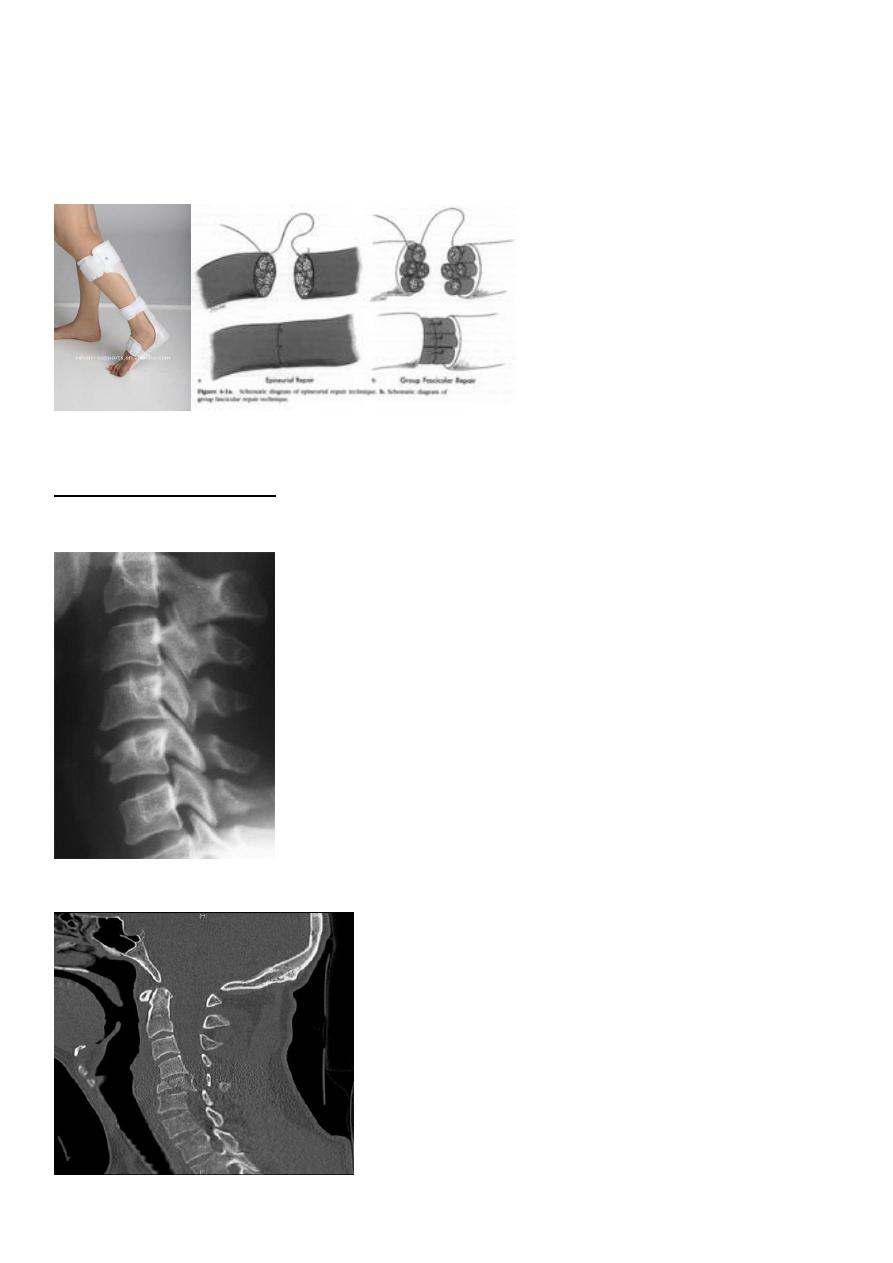
DDx:
Radicular symptoms of cervical spondylosis may confuse the diagnosis and may coincide
with carpal tunnel syndrome.
Treatment
Light splints that prevent wrist flexion can help those with night pain or with pregnancy-
related symptoms.

9
• Steroid injection into the carpal canal, likewise, provides temporary relief.
• Open surgical division of the transverse carpal ligament usually provides a quick and
simple cure.
Endoscopic carpal tunnel release.
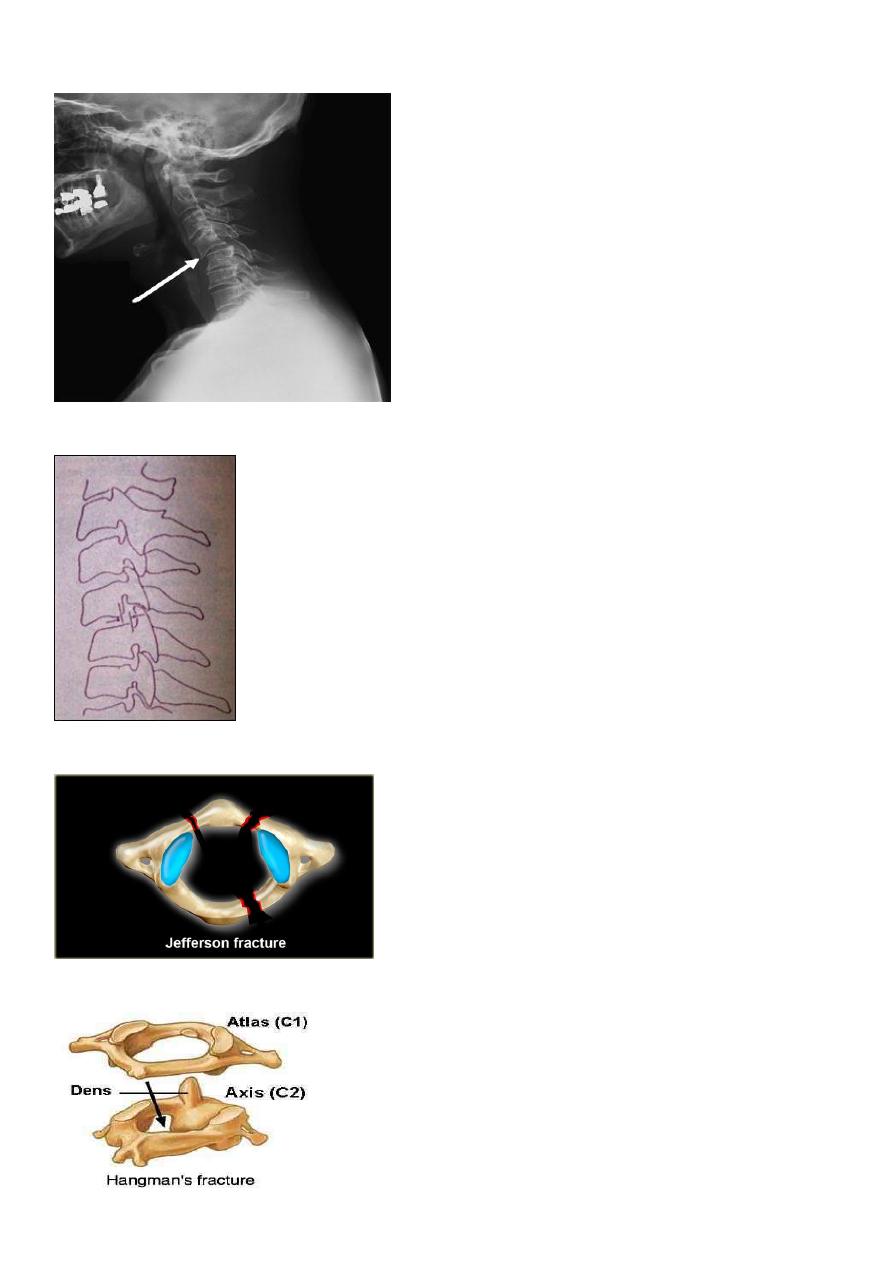
SCIATIC NERVE
• Division of the main sciatic nerve is rare except in
• gunshot wounds.
• Traction lesions may occur with traumatic hip dislocations and with pelvic fractures.
• Intraneural haemorrhage in patients receiving anticoagulants
10
Clinical features
• In a complete lesion the hamstrings and all muscles below the knee are paralysed;
• the ankle jerk is absent.
Sensation is lost below the knee, except on the medial side of the leg which is supplied by
the saphenous branch of the femoral nerve.
• The patient walks with a drop foot and a high-stepping gait to avoid dragging the
insensitive foot on the ground
11
Treatment
• suture or nerve grafting should be attempted ,more than a year for leg muscles to
be re-innervated.
• While recovery is awaited, a below-knee drop-foot splint is fitted.
Spine injuries
Cervical classifications
wedge compression fracture of vertebral body
burst fracture of vertebral body
12
extension subluxation
flexion subluxation
fracture of the atlas
fracture-dislocation of the atlanto-axial joint
13
intraspinal displacement of soft tissue
soft-tissue strain ('whiplash injury')
MECHANISM OF INJURY
Flexion
Flexion-rotation
Extension
Vertical compression.
14
injuries of the cervical spine are usually caused by indirect violence, Such as falls on to the
head or other violent movements transmitted from the skull. i.e in any direction. flexion,
tension, lateral flexion or rotation-or a vertical compression force acting on a straight
spine.
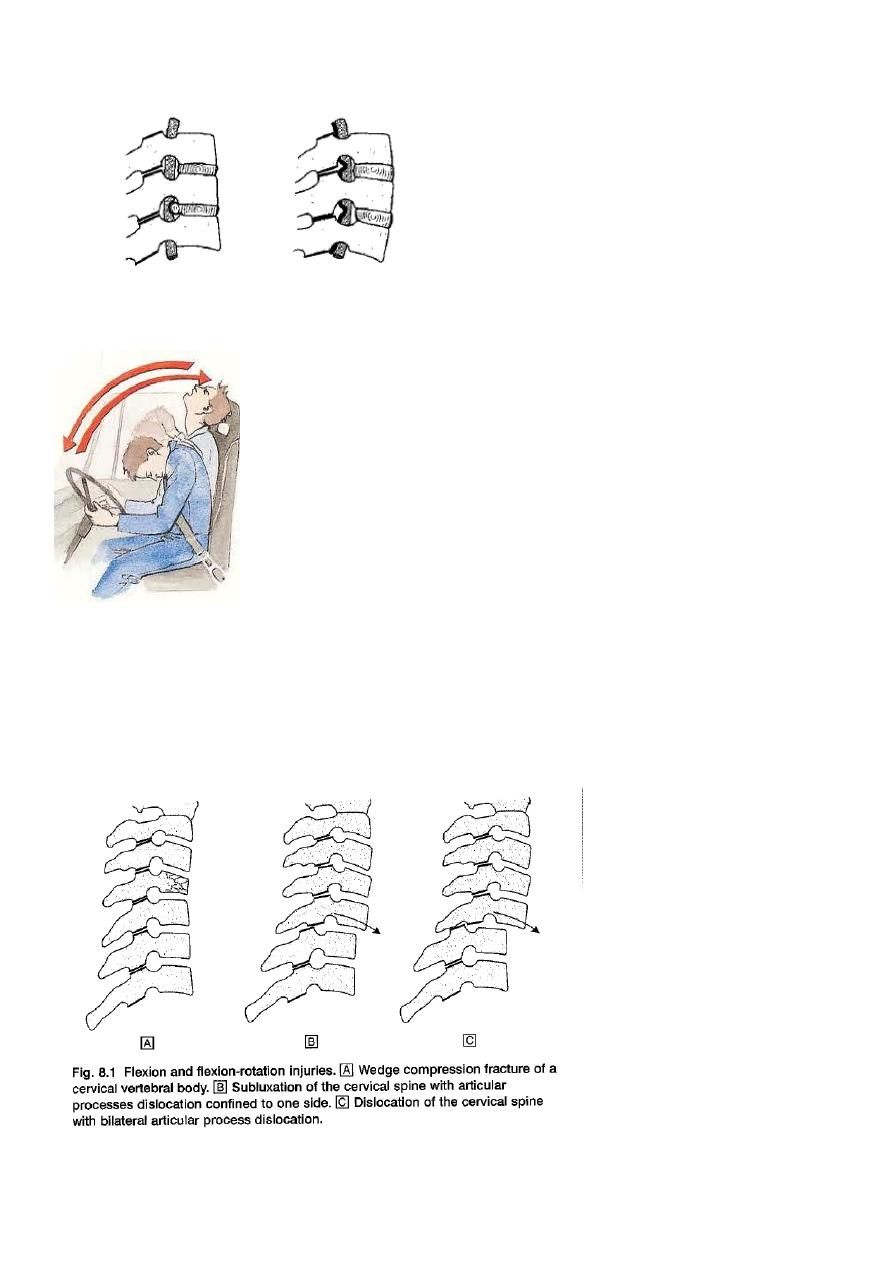
Flexion and flexion-rotation injuries are common: flexion alone tends to a wedge
compression fracture . whereas combined flexion and rotation cause subluxation ,
dislocation or fracture-disIocation.
15
A flexion or flexion-rotation force may also cause massive displacement of an intervertebral
disc, without bone injury
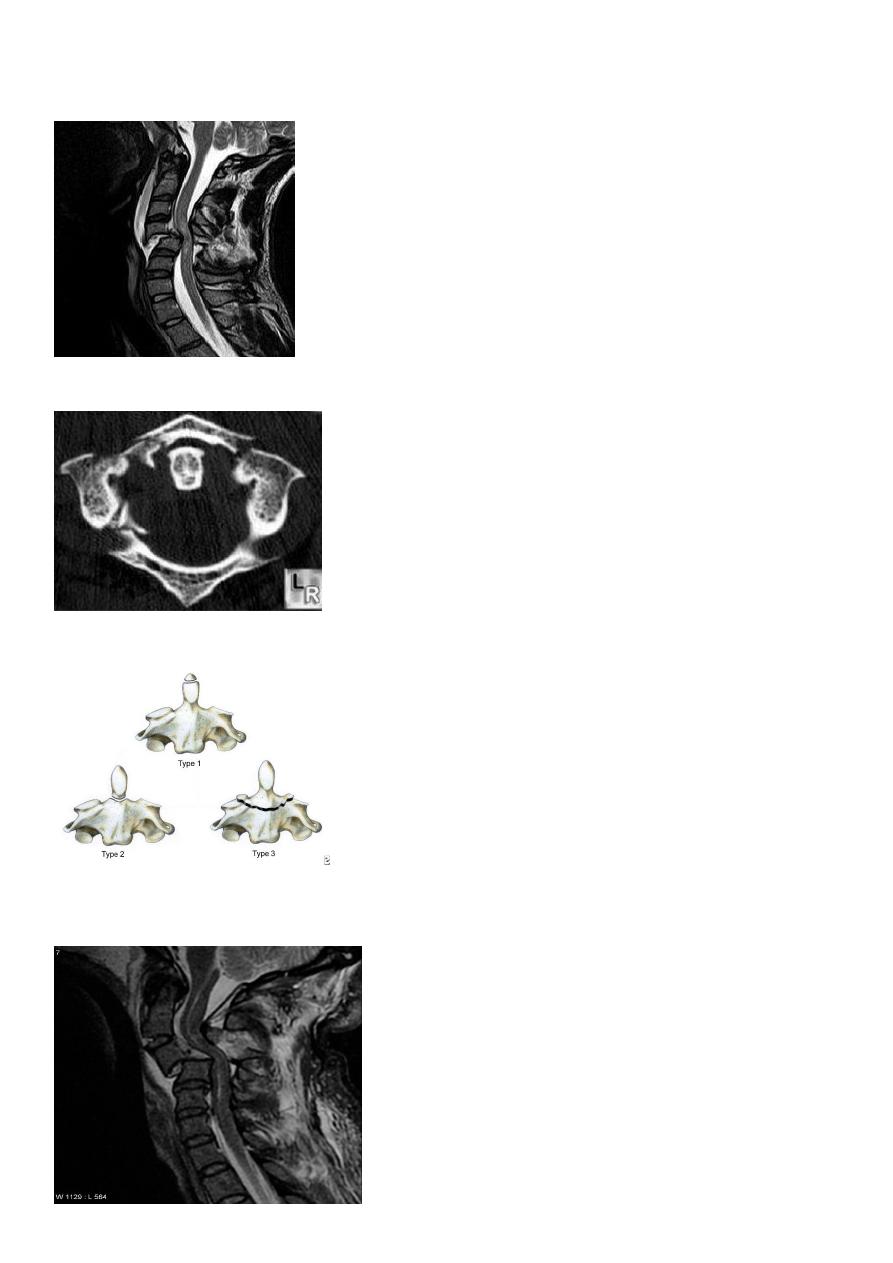
A hyperextension force may fracture the neural arch, especially of the atlas
Or fracture the dens (odontoid process) of the axis.
hyperextension may rupture the anterior longitudinal ligament and the anulus fibrosus,
forcing the vertebral bodies apart anteriorly (extension subluxation) .
16
DIAGNOSIS
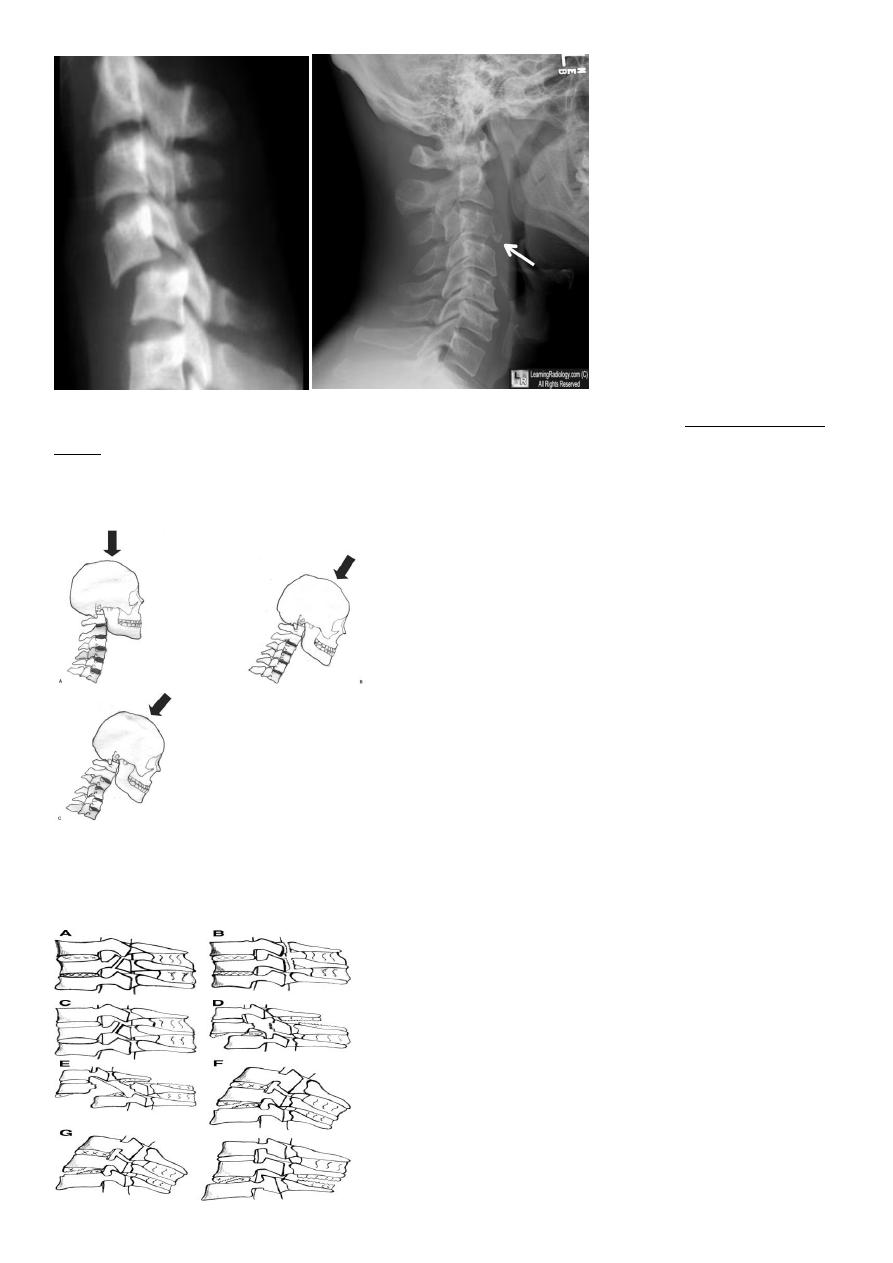
X RAY
Anterio posterior X ray radiograph.
lateral radiographs with the head in flexion and extension may reveal instability that is not
shown in the routine lateral film.
oblique views at 45° are especially helpful
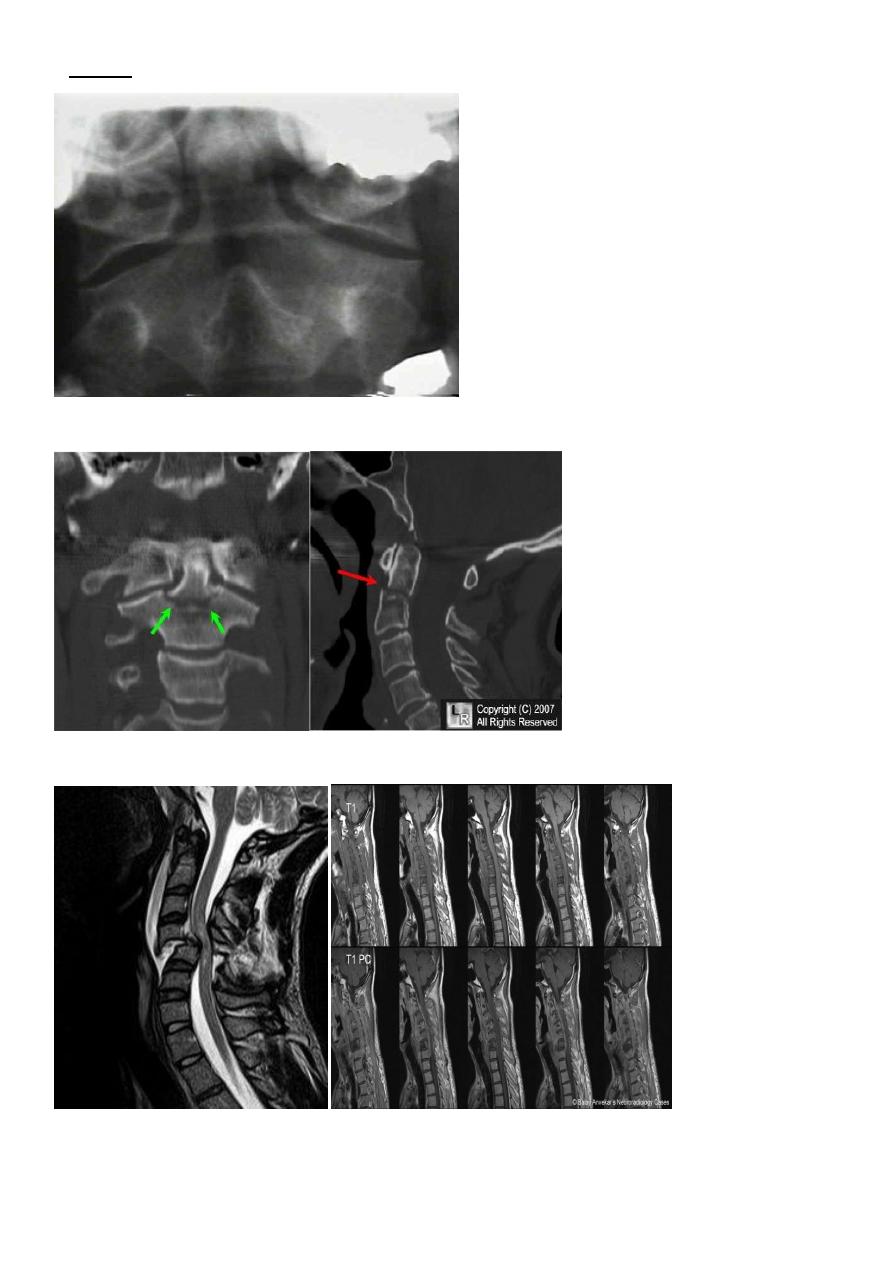
17
a special projection through the open mouth.
Computed tomography (CT)
and magnetic resonance imaging (MRI).
18
Treatment
It is unnecessary to attempt reduction, and all that is required is to support the neck for 2
months to relieve pain. This may be achieved by a rigid plastic Collar. In addition to N S A I
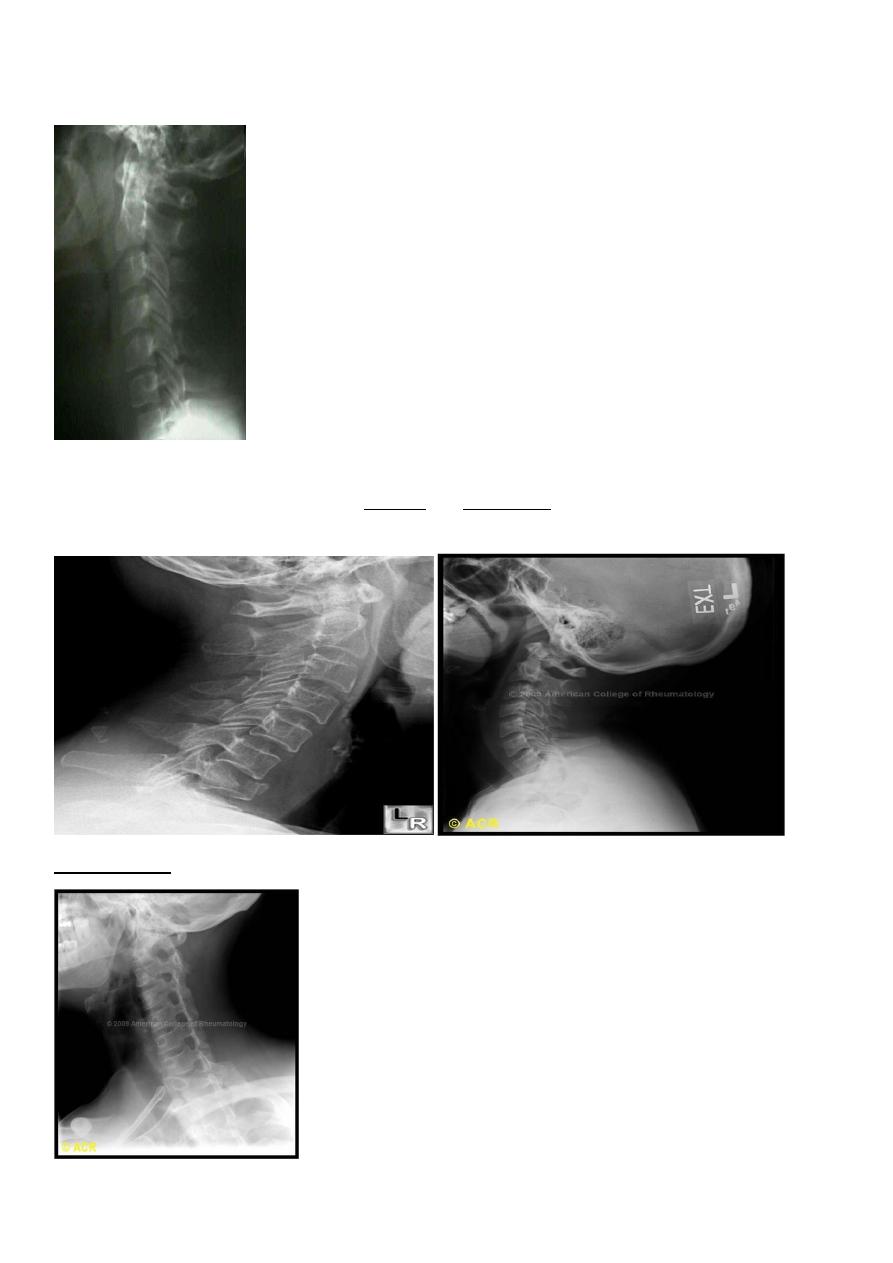
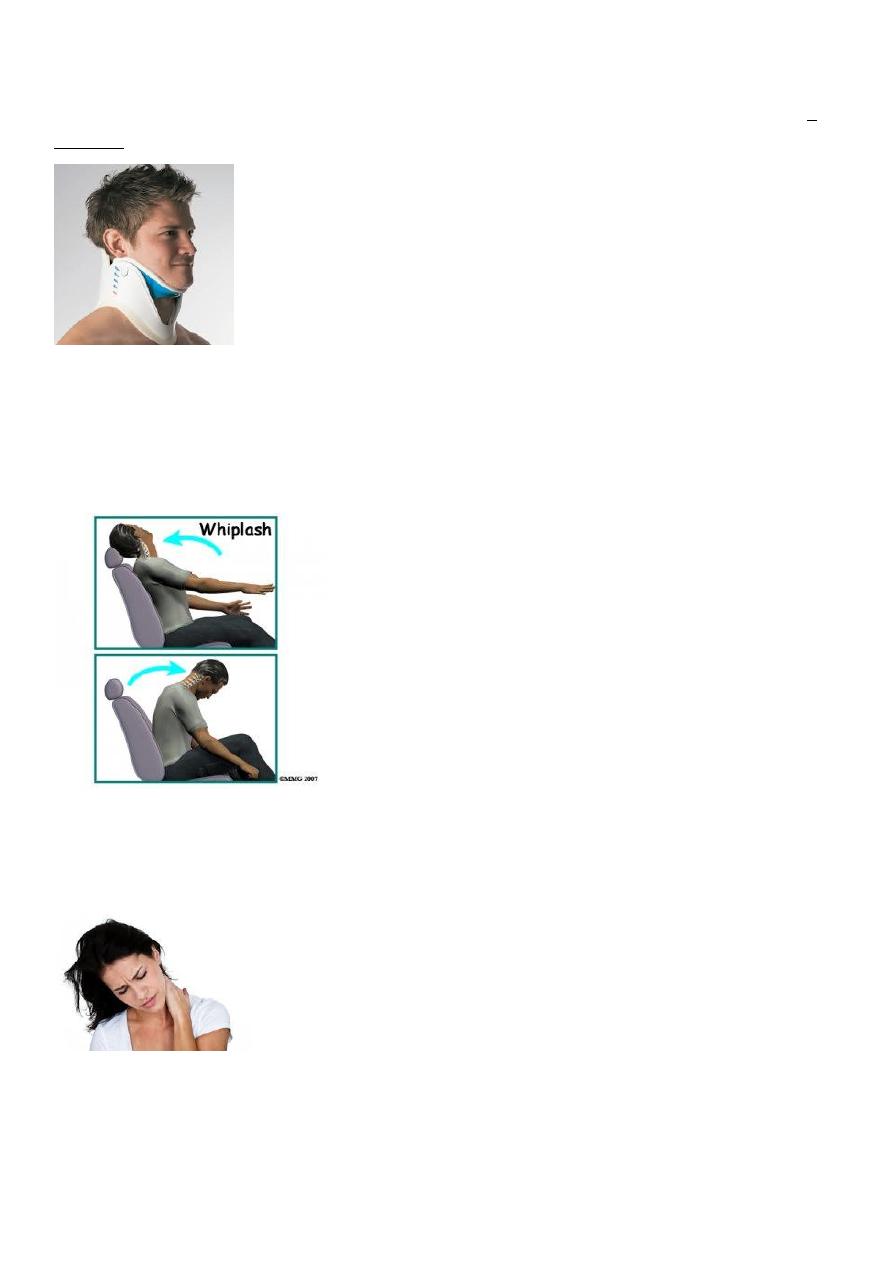
SOFT-TISSUE STRAIN OF THE CERVICAL SPINE
Mechanism of injury and pathology
At the moment of impact, the head is first suddenly jolted forwards followed by rebound
flexion of the spine. And a second by extension of the neck.
Clinical features
At impact, the patient may feel jolting or 'wrenching' of the neck or painful one of the
shoulder,
neck pain is usually accompanied by severe headache, which Examination shows restriction
of the range of movement of the cervical spine, usually in all directions
19
Treatment
In general, the principle to provide support and rest for the neck at First, in the form of a
protective cervical collar.
But after 1or 2 weeks there should be on the restoration of mobility by exercises within the
limits imposed by pain, preferably under the supervision of a physiotherapist.
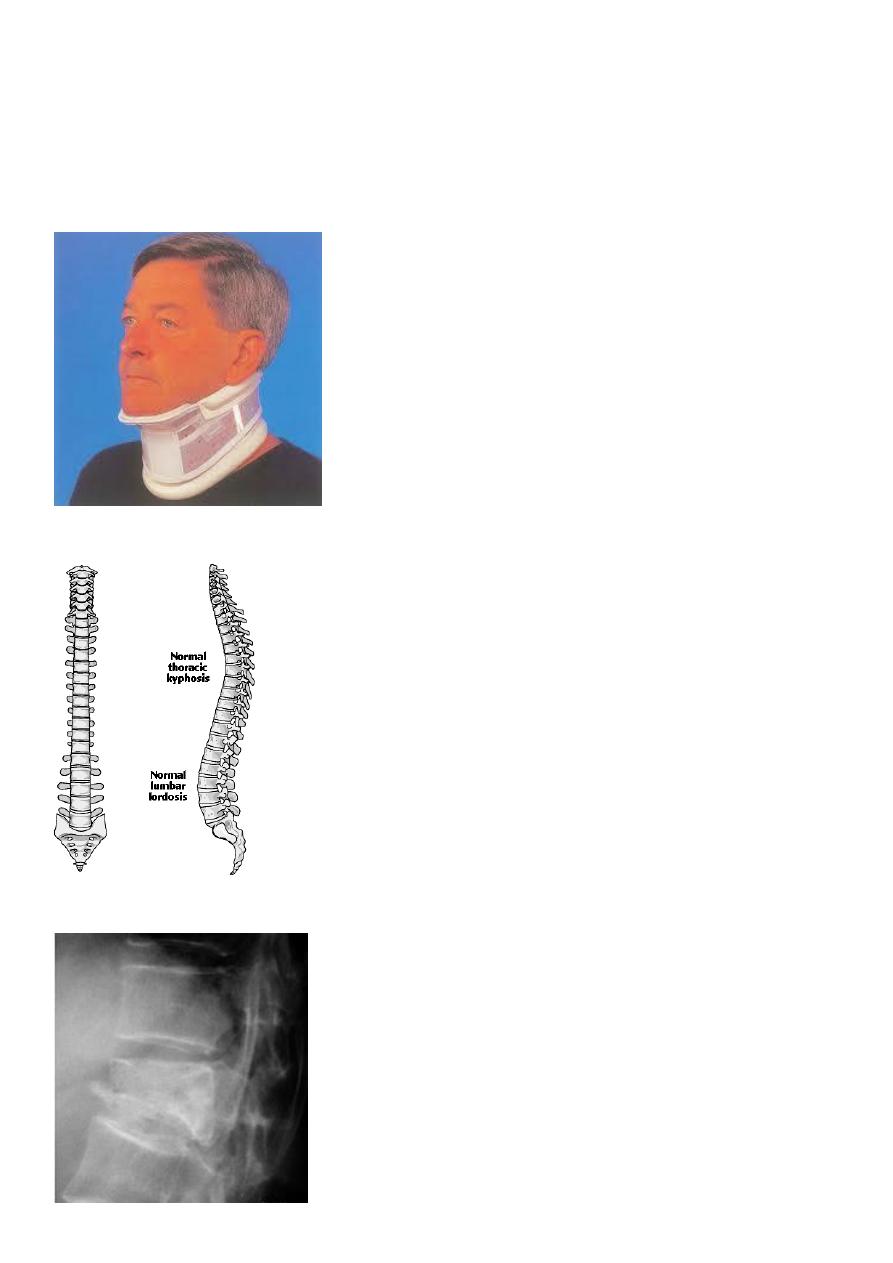
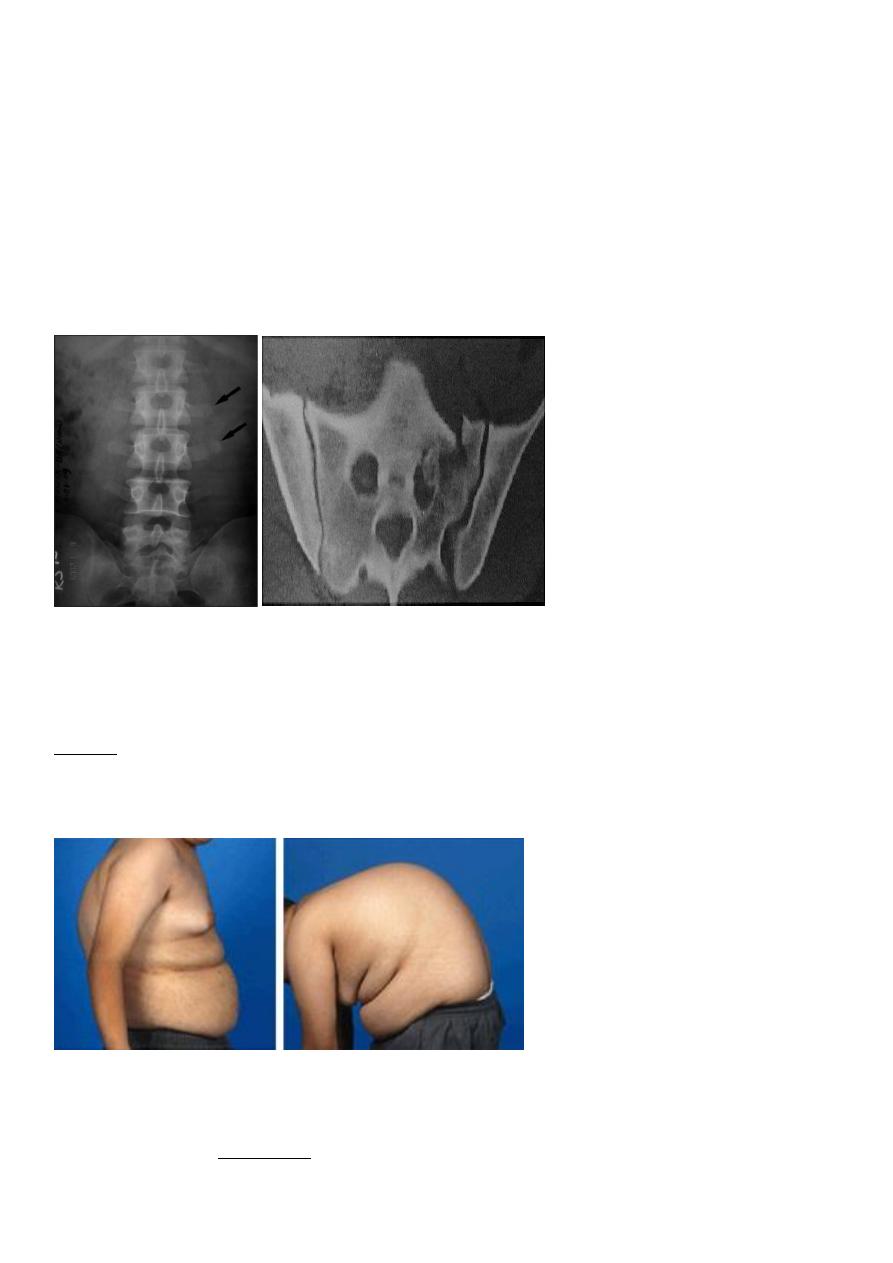
Dorsal and lumbar spine
Wedge compression fracture of a vertebral body.
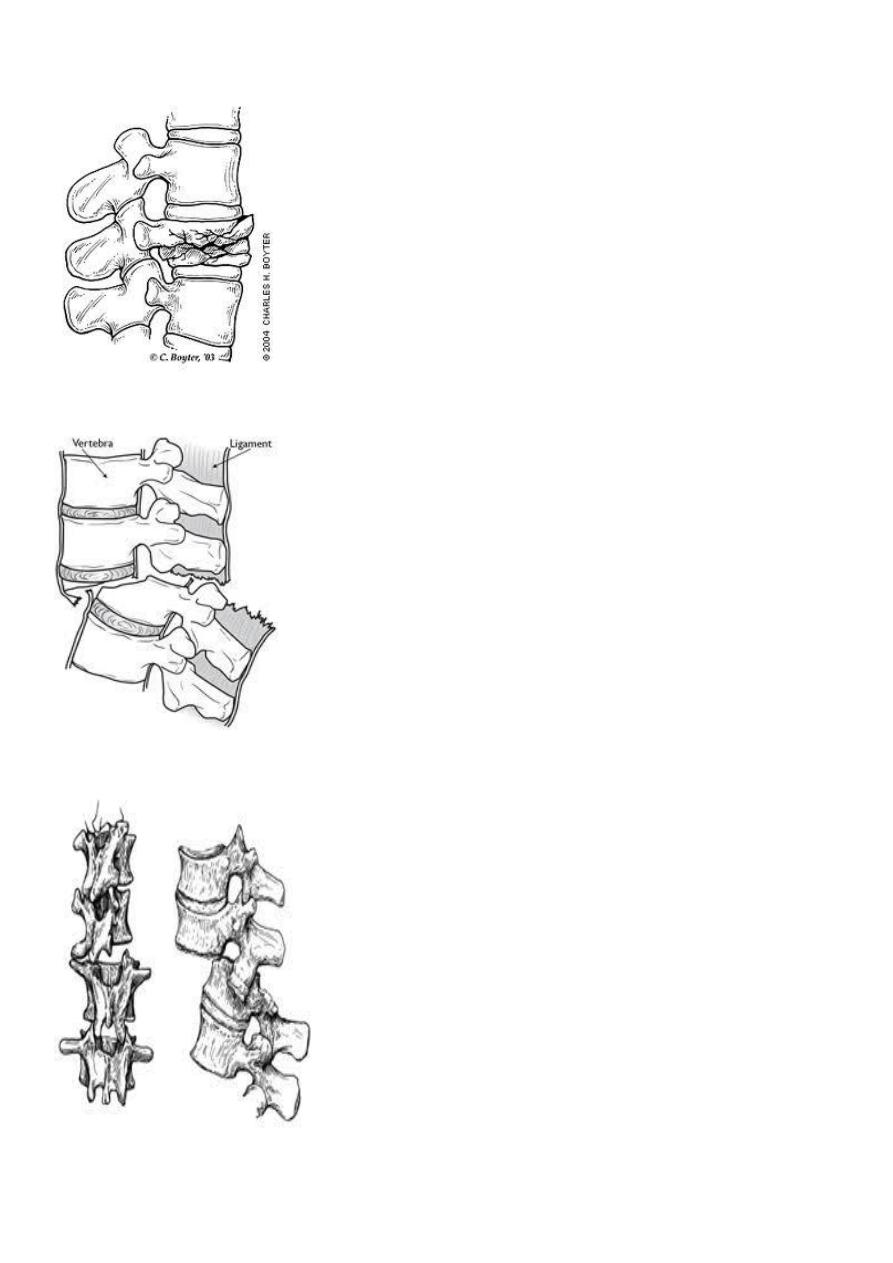
20
Burst fracture of a vertebral body.
Distraction fracture of a vertebral body.
Dislocation and fracture-dislocation
21
Minor fractures of the spinal column
Fractures of transverse processes .
Fracture of the sacrum
Fracture of the coccyx
Fractures of the thoracic cage.
Fractures of the ribs
Fractures of the sternum
MECHANISM OF INJURY
by vertical force acting through the long axis of the spinal column.
This force. may act from above, as when a coal miner is buried by a fall of roof. or from
Below, as by a heavy fall on the feet or buttocks, in high speed motor vehicle collisions
The thoracolumbar junction one or more of the vertebral bodies collapses anteriorly and
becomes wedge-shaped, giving rise to a localized kyphosis.
WEDGE COMPRESSION FRACTURE
Diagnosis . obvious symptoms and signs pointing In cases of major fracture there will be
only between the T11 and L2
22
Treatment
It has been shown that persistent wedging of a vertebral body is compatible. With virtually
normal function.
so correction of the deformity is not essential.
The standard method of treatment may, therefore, be said to be conservative.
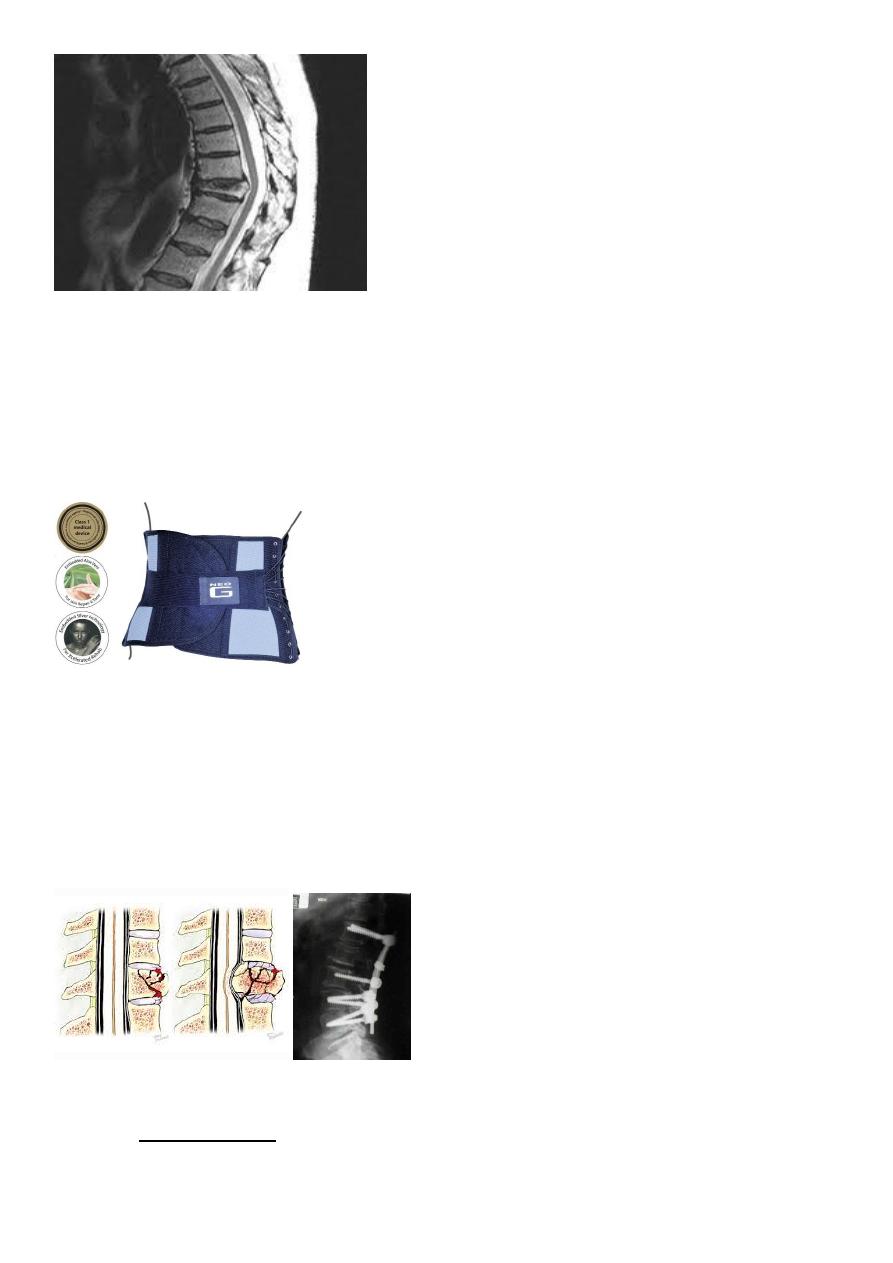
BURST FRACTURE OF A VERTEBRAL BODY
the compression force thus acts vertically in the line of the vertebral bodies.
The intervertebral disc is forced In the affected vertebral body, causing a comminuted
bursting fracture in which fragments are driven outwards in all directions.
Treatment
If there is no neurological impairment, it is permissible to employ Conservative treatment
as for wedge compression fracture, but a rather longer period of recumbency is advisable.
Some surgeon advise surgical fixations.
