1
Forth stage
Surgery
Lec-2
د.هيثم النجفي
1/1/2014
Fate of Appendicitis:
1- The immunity is good, the patient takes antibiotic, acutely inflamed appendix may
resolve.
2- Appendicular mass: the appendix itself is rape, there is good immunity but the
microorganism leaks from the serosa, forming ‘appendicular mass’.
3- Appendicular abscess: slightly, the virulence of the microorganism is powerful, but it
is not powerful enough to perforate rapidly, this will lead to localized abscess.
4- Generalized peritonitis: the virulence of the microorganism is enough to perforate the
appendix.
Management of Appendicular Mass
The patient comes with typical history of appendicitis. On examination, there is mass in the
right iliac fossa, this mass is globular, either mobile or fixed, with smooth surface. Pure mass
is painless, while complicated mass (i.e. with abscess formation) will be tender. Body
temperature within normal limits, and there is no change in constitutional symptoms.
Investigation of appendicular mass:
The most important one is Ultra Sound, show glandular mass in the RIF, other investigation,
GUE, WBC count. Recently CT used.
Treatment of appendicular mass:
1- Small mass (less than 3cm), mobile, and not tender, the treatment is appendicectomy.
2- Large mass (more than 3cm) and fixed, the standard treatment is the conservative
Ochsner–Sherren regimen, this regimen composed of combination of ceftriaxone and
metronidazole, and nothing by mouth. If the patient got severe attack of vomiting
nasogastric tube can be used, if there is no vomiting no need for NG tube. In addition
mapping of the mass should be done plus follow up 4 hourly which involve the
temperature, pulse, blood pressure and evaluation of the signs of the mass.
Q: Outline Differential Diagnosis of a mass in the right iliac fossa?
Children: Female: Adult male
- Intussusception - Ovarian cyst - Tubercles lymph node
- Tumor in the cecum
- Seminoma in the testes
2
Criteria for stopping conservative treatment of an appendix mass
- A rising pulse rate.
- A rising temperature (spiky temperature).
- Tenderness incited.
- Increasing or spreading abdominal pain.
- Increasing size of the mass.
If these criteria doesn’t appear, keep on conservative treatment till the mass disappeared. Ask
the patient to comes again after 2 months to make him appendicectomy, this called ‘interval
appendicectomy.
Management of Appendicular Abscess
Developed either due to low immunity of the patient, virulent microorganism, or pelvic
surgery. The patient will get perforation, and all features of abscess (tenderness, rebound
tenderness…. etc.), the best diagnosis is history, physical examination and ultra sound.
Treatment by drainage, types of drainage are per rectal drainage, suprapubic pfannenstiel
incision and drainage or aspiration. Although per rectal drainage is easy and does not need
general anesthesia, Suprapubic pfannenstiel incision used over per rectal drainage, because
in per rectal drainage you may introduce microorganism which is often not found (most
common clostridium), or the abscess is multilocular or high abscess (paracecal or paracolic),
and specimen cannot be taken, vessels may injured.
N.B: Abscess has more prevalence in children and old age.
Appendicectomy:
When the preoperative diagnosis is considered reasonably certain, the incision that is widely
used for appendicectomy is the so-called gridiron incision (gridiron: a frame of cross-beams
to support a ship during repairs). The gridiron incision at McBurney’s point is muscle
splitting.
Rutherford Morison’s incision is useful if the appendix is para- or retrocaecal and fixed. It is
essentially an oblique muscle cutting incision with its lower end over McBurney’s point and
extending obliquely upwards and laterally as necessary. All layers are divided in the line of
the incision.
For cosmetic purposes, Lanz incision has been used, as the exposure is better and extension,
when needed, is easier. The incision, appropriate in length to the size and obesity of the
patient, is made approximately 2 cm below the umbilicus centered on the midclavicular–
midinguinal line as a transverse skin and muscle cutting incision.
Complication of appendicectomy:
Bleeding : the most early complication, there is blood with the drain, give the
patient fluid and
Wound infection:
Wound infection is the most common postoperative
complication. This usually presents with pain and erythema of the wound on the
3
3
rd
or 5
th
postoperative day, often soon after hospital discharge. Treatment is by
wound drainage and antibiotics when required.
Ileus: A period of a dynamic ileus is to be expected after appendicectomy, and
this may last a number of days following removal of a gangrenous appendix.
Adhesive intestinal obstruction: This is the most common late complication of
appendicectomy. Occasionally, chronic pain in the right iliac fossa is attributed
to adhesion formation after appendicectomy. In such cases, laparoscopy is of
value in confirming the presence of adhesions and allowing division.
Faecal fistula: Leakage from the appendicular stump occurs rarely, but may
follow if the caecal wall was involved by oedema or inflammation.
Occasionally, a fistula may result following appendicectomy in Crohn’s disease.
Portal pyaemia (pylephlebitis): This is a rare but very serious complication of
gangrenous appendicitis. It is caused by septicaemia in the portal venous system
and leads to the development of intrahepatic abscesses (often multiple).
Tumors of appendix:
Carcinoid tumor
Carcinoid tumours (argentaffinoma) arise in argentaffin tissue, it is the commonest site of
GIT to be affected by carcinoid, carcinoid of the appendix is rarely disseminated, and
carcinoid syndrome is rarely to be seen in the appendix, because there is no metastases to the
liver. Tumors of appendix mainly presented as appendicitis.
Appendicectomy has been
shown to be sufficient treatment, unless the caecal wall is involved, the tumor is 2 cm or
more in size or involved lymph nodes are found, when right hemicolectomy is indicated.
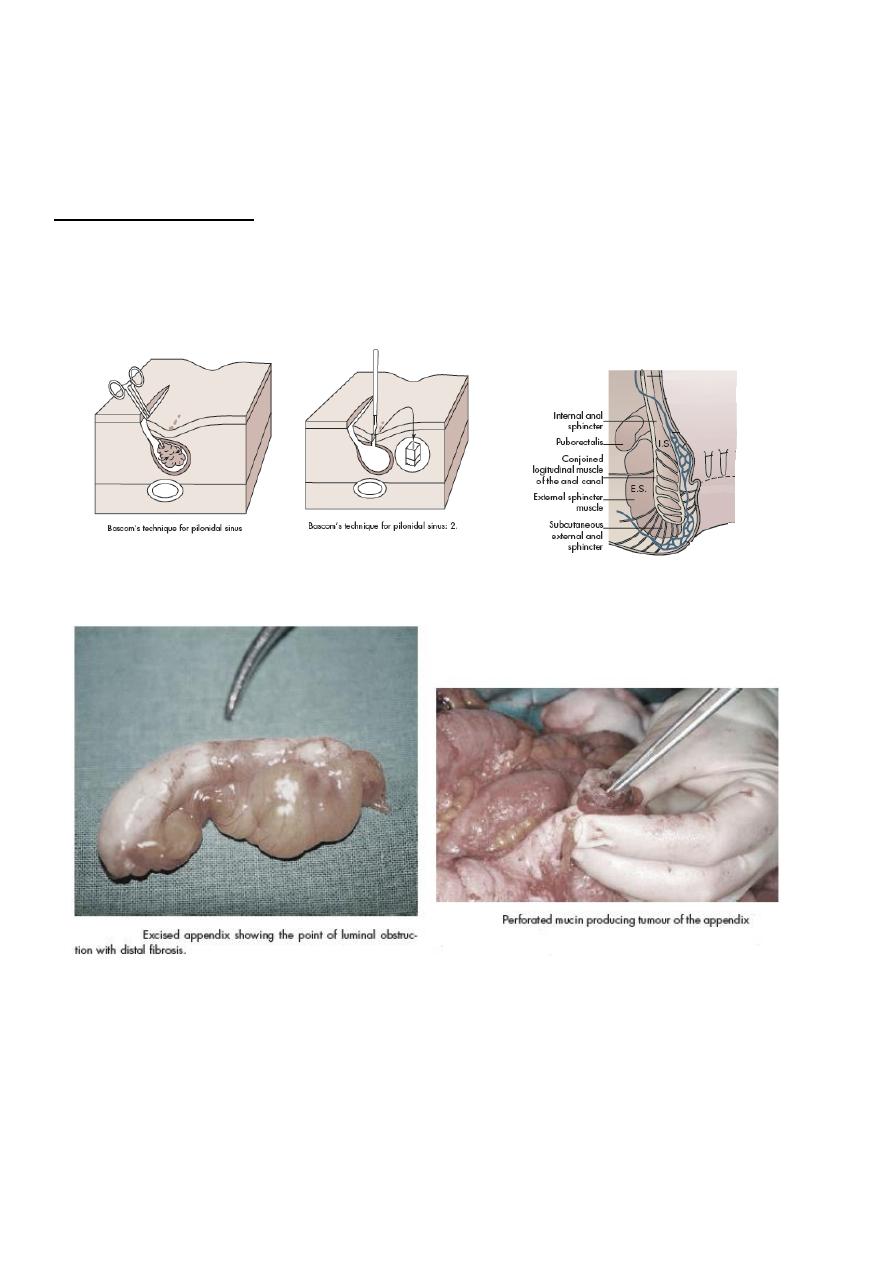
Mucinous cystadenoma
In an inflamed appendix, sometimes the inflammation will resolved but there will be
stricture in the lumen and the appendix will filled and ballooned by mucus material, this is
called mucocele, if it is perforated this will lead to pseudomyxomal
peritoneum, just like
ascites.
Mucus secreting cyst carcinoma (mucus secreting adenocarcinoma), it is presented just like
pseudomyxomal
peritoneum, but here it is malignant, and rupturing of the appendix will lead
to seeding of all malignant cells to the peritoneum and greater omentum, on exploration will
see parietal cells, omentum and crypts are studded with metastatic cells and metastatic tumor
which secret mucus like material.
Treatment consists of radical resection of all involved
parietal peritoneal surfaces and aggressive intraperitoneal chemotherapy (Sugarbaker).
4
Anal Canal
Surgical anatomy
The anal canal commences at the level where the rectum passes through the pelvic
diaphragm and ends at the anal verge. The muscular junction between the rectum and anal
canal can be felt with the finger as a thickened ridge – the anorectal ‘bundle’ or ‘ring’.
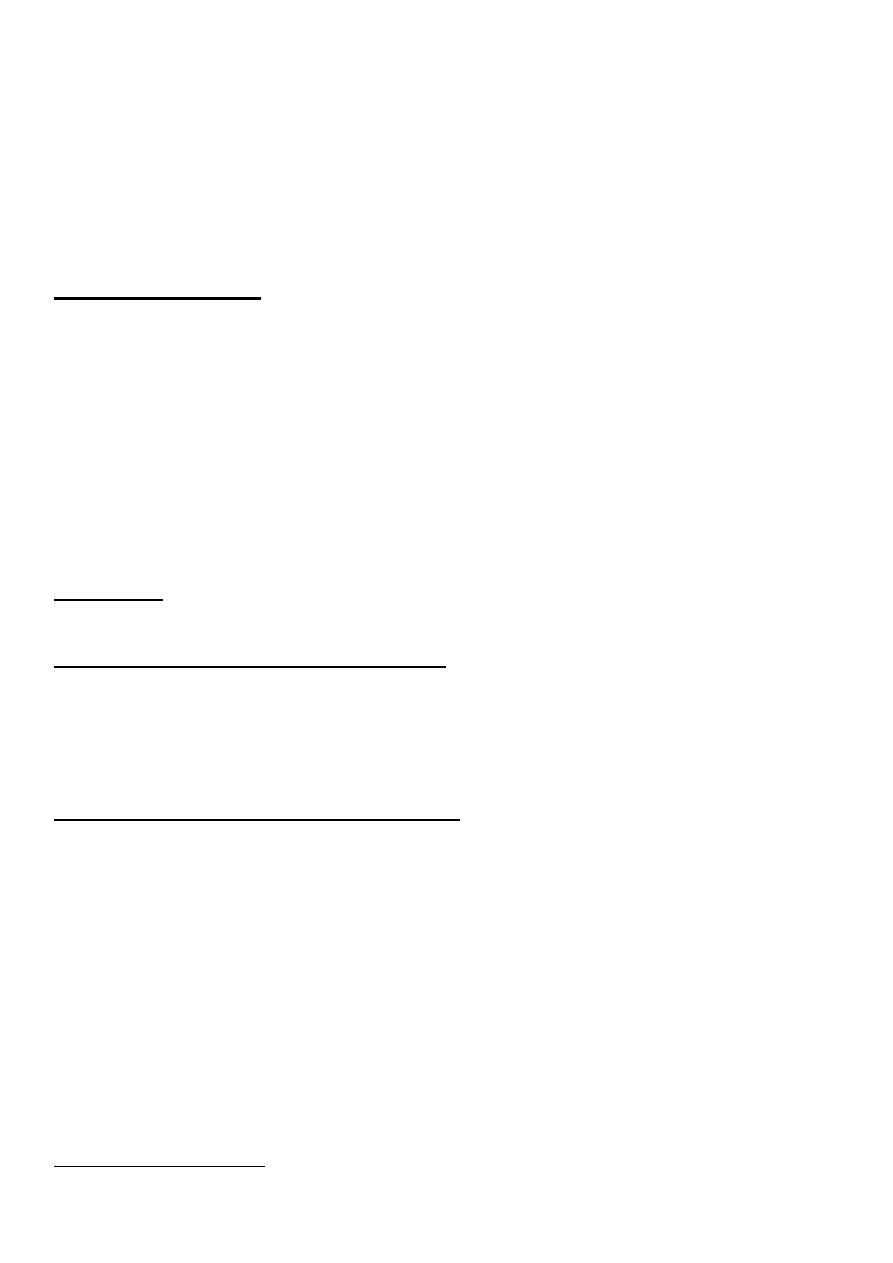
Anal canal anatomy
The anorectal ring marks the junction between the rectum and the anal canal. It is formed
by the joining of the puborectalis muscle, the deep external sphincter, conjoined longitudinal
muscle and the highest part of the internal sphincter. The anorectal ring can be clearly felt
digitally, especially on its posterior and lateral aspects.
The internal sphincter is the thickened (2–5 mm) distal continuation of the circular muscle
coat of the rectum. This involuntary muscle, although innervated by the autonomic nervous
system, it receives intrinsic non-adrenergic and non-cholinergic (NANC) fibers, stimulation
of which causes release of the neurotransmitter nitric oxide, which induces internal sphincter
relaxation.
The external sphincter forms the bulk of the anal sphincter complex. Being a somatic
voluntary muscle, the external sphincter is innervated by the pudendal nerve.
The intersphincteric plane between the external sphincter muscle laterally and the
longitudinal muscle medially exists a potential space. This plane is important as it contains
intersphincteric anal glands.
The importance of this anatomy is to maintain anal continence and defecation.
Pilonidal sinus
The term ‘pilonidal sinus’ describes a condition found commonly in the natal cleft overlying
the coccyx, other sites may be seen in the axilla and chest wall, consisting of one or more,
usually non-infected, midline openings, which communicate with a fibrous track lined by
granulation tissue and containing hair lying loosely within the lumen.
Etiology and pathology
Although acquired theories of development are better accepted than the more historical
congenital theories, exact mechanisms of development are speculative. Evidence that
supports the acquired theory of origin of pilonidal sinuses can be summarized as follows:
Interdigital pilonidal sinus is an occupational disease of hairdressers, the hair within
the interdigital cleft or clefts being from the customers.
The age incidence of the appearance of pilonidal sinus (never present before the ages
of 20 years) is at variance with the age of onset of congenital lesions.
Hair follicles have almost never been demonstrated in the walls of the sinus.
The hairs projecting from the sinus are dead hairs, with their pointed ends directed
towards the blind end of the sinus.
The disease mostly affects men, in particular hairy men.
Recurrence is common, even though adequate excision of the track is carried out.
5
It is thought that the combination of buttock friction and shearing forces in that area allows
shed hair or broken hairs which have collected there to drill through the midline skin, or that
infection in relation to a hair follicle allows hair to enter the skin by the suction created by
movement of the buttocks, so creating a subcutaneous, chronically infected, midline track.
From this primary sinus, secondary tracks may spread laterally, which may emerge at the
skin as granulation tissue lined, discharging openings. A common affliction among the
military, it has been referred to as ‘jeep disease’.
Clincal presentation
Either acute or chronic, acute presentation the patient present with abscess between the level
of the sacrococcygeal joint and the tip of the coccyx, there will be swelling tenderness and
the patient cannot sit on his buttock. While chronic presentation the opening of the sinus is
closed so secretion will accumulated inside lead to abscess formation. Chronic presentation
is the most common presentation, the patient with local discomfort, discharges and the most
important characteristically foul containing hair, other presentation is itching only with no
constitutional symptoms.
On examination, the hole resemble needle hole in size, single or multiple, mostly in the
midline and sometimes it is very obvious (cut of hair)
Treatment
There is no specific treatment for pilonidal sinus
Treatment of an acute exacerbation (abscess)
If rest, baths, local antiseptic dressings and the administration of a broad-spectrum antibiotic
fail to bring about resolution, the abscess should be drained through a small longitudinal
incision made over the abscess and off the midline, with thorough curettage of granulation
tissue and hair. This procedure may or may not be associated with complete resolution.
Surgical treatment of chronic pilonidal disease
The aim of surgical procedures to eradicate pilonidal disease without recurrence, combined
with the lack of prospective trials, attests to the lack of overall superiority of one method
over the others. Time spent off work and perceived recurrence rates, but more usually
surgeon preference, influence the choice of method, which includes the laying open of all
tracks with or without marsupialization, the excision of all tracks with or without primary
closure, and the excision of all tracks and then closure by some other means designed to
avoid a midline wound (Z-plasty, Karydakis procedure). Bascom’s procedure involves an
incision lateral to the midline to gain access to the sinus cavity, which is rid of hair and
granulation tissue, and excision and closure of the midline pits. The lateral wound is left
open. Irrespective of procedure, postoperative wound care is important and centers on
elimination.
Recurrent pilonidal sinus
Three possibilities account for this disappointment:
6
Incomplete resection, part of the sinus complex has been overlooked at the primary
operation;
New hairs enter the skin or the scar;
Midline wound is weak point; in this situation, fracture of this scar and re-embedding
of hair is other cause.
Conservative treatment
As the natural history of the condition is usually one of regression, in those whose symptoms
are relatively minor, simple cleaning out of the tracks and removal of all hair, with regular
shaving of the area and strict hygiene, may be recommended.
This treatment is not effective because there is no way to eradicate the whole tree of hair.
