1
Forth stage
Surgery
Lec-3
د.هيثم النجفي
1/1/2014
Haemorrhoids
Dilatation and tortuosity of venous plexus (internal and external), and sliding of anal mucosa
below anal verge, usually dilatation of internal plexus followed by dilatation of external one.
Primary Internal Haemorrhoid:
Theories of development
1- Portal hypertension theory: haemorrhoid veins are part of portal circulation, which
lack of valves, so any portal hypertension will reflect to the lowest part of the column
of the portal circulation which is the haemorrhoid veins. This theory is no more
dependent, because the researches have seen that the incidence of having
haemorrhoids in patient with cirrhosis, portal hypertension and esophageal varices is
the same of that in normal person.
2- Other vascular causes: Historically, some considered haemorrhoids to be
haemangiomatous or to result from changes in the erectile tissue that forms part of the
continence mechanism, such as hyperplasia of the ‘corpus cavernosum recti’.
3- Infection: Repeated infection of the anal lining, secondary to trauma at defecation, has
been postulated as a cause of weakening and erosion of the walls of the veins of the
submucosa.
4- Diet and stool consistency: role of constipation in the development of haemorrhoids
and, indeed, much of the management of sufferers involves attempts to ‘normalize’
bowel habits. A fiber-deficient diet results in a prolonged gut transit time. The
presence of a hard fecal mass in the rectum could obstruct venous return,
5- Anal hypertonia: The association between raised anal canal resting pressure and
haemorrhoids is well known, but whether anal hypertonia causes symptoms
attributable to haemorrhoids or whether anal cushion hypertrophy causes anal
hypertonia is a subject of debate.
6- Ageing: In contrast to the anal cushion of early life, with age, the supporting structures
show a higher proportion of collagen than muscle fibers and are fragmented and
disorganized.
7- Current view: Shearing forces acting on the anus (for a variety of reasons) lead to
caudal displacement of the anal cushions and mucosal trauma. With time,
fragmentation of the supporting structures (a normal consequence of ageing, but
perhaps accelerated in those with haemorrhoids) leads to loss of elasticity of the
cushions such that they no longer retract following defecation.
2
N.B: All theories except the first one are summarized from the book (Bailey & Love’s short
practice), the first one mentioned as doctor said, the others were not understood and the
doctor didn’t focus on them. You can review all theories in book (pg. 1251).
Secondary Haemorrhoids:
1- Carcinoma of rectum, which may be presented as piles (tumour causing pressure effect
on the anal venous plexus leading to obstruction and piles appear).
2- Pregnancy, due to gravid uterus which press on the pelvic veins with the superadded
effect of estrogen.
3- Big pelvic tumour press on the pelvic veins also.
Q- How piles occur?
A- Dilatation of internal venous plexus followed by external venous plexus with sliding
of anal mucosa outside the anal verge, an embryological anal cushions will appear at
3, 7 and 11 o’clock when patient is lying on lithotomy position lead to pile masses.
B- Haemorrhoids may be observed between the main pile masses which are called
haemorrhoids at secondary position.
Clinical Features of Haemorrhoids:
1- Bleeding: is the earliest and principle symptom of haemorrhoids, the nature of
bleeding is characteristically separated from motion (usually occurs immediately after
defecation), it is associated with significant anemia, because of the chronic blood loss.
2- Prolapse: the patient complain true (piles) lump appear at the anal orifice during
defecation which varies in its reducibility according to the stage of disease.
Stages of haemorrhoids:
Stage 1: bleeding only without prolapse.
Stage 2: bleeding with prolapse but reduced spontaneously.
Stage 3: bleeding with prolapse which should be reduced manually.
Stage 4: bleeding with prolapse that is permanently outside.
3- Pain: pain is not commonly associated with bleeding, and the presence of such a
character of pain should make a clinical alert for possibility of another diagnosis. The
pain pf piles usually arise from the congestion of the venous plexuses below a
hypertonic sphincter.
4- Itching: this is due to irritation of the area which arise from mucus secretion from a
caudally displaced anal mucosa or difficulty in washing the area after defecation
because of irregular anal verge.
On examination: Patient usually presented with anemia due to blood loss, if pain is present,
patient will sit on the edge of the chair trying to avoid the pressure on the haemorrhoid site.
With lithotomy position, three masses of anal cushions will be found at 3, 7 and 11 o’clock
which are plum in color refers to prolapsed haemorrhoid.
3
On PR: The internal piles are not palpable while the external can be felt as small masses,
sometimes felt as firm masses due to engorgement or thrombosis, pain is absent unless
complicated.
Protoscope: Have been pushed into its full extension and then drawn gradually until
reaching the pedicle of internal pile, pile will prolapsed inside the lumen of the protoscope
Sigmoidscope: just to exclude malignancy.
Complications
Profuse haemorrhage is uncommon. The bleeding mainly occurs externally but it may
continue internally after the bleeding haemorrhoid has retracted or has been returned.
In these circumstances, the rectum is found to contain blood.
Strangulation and thrombosis
Ulceration
Gangrene
Portal pyaemia
Fibrosis
Management of Haemorrhoids:
1- Conservative treatment: Exclusion of other causes of rectal bleeding, the aim of
conservative treatment is to normalize bowel and defaecatory habits by: only
evacuating when the natural desire to do so arises, adopting a defaecatory position to
minimise straining, and the addition of stool softeners and bulking agents to ease the
defaecatory act.
2- Minor invasive treatment:
A- Injection sclerotherapy (Mitchell): In those with first- or second-degree piles whose
symptoms are not improved by conservative measures injecting of sclerosing agent
of 5 per cent phenol (5 ml) in almond oil, may be advised. The aim is to create
fibrosis, cause obliteration of the vascular channels leading to its shrinkage. This
procedure is done by Gabriel’s needle, by putting the patient on lithotomy position
(no need for anesthesia) and injecting the substance into the pedicle of the pile
under guidance of protoscope.
Complications:
Injections that are too superficial are heralded by the rapid bulging of the mucosa,
which turns white; this leads to superficial ulceration but rarely serious septic
sequelae. However, injections placed too deeply can have disastrous consequences,
including pelvic sepsis, prostatitis, impotence and rectovaginal fistula.
B- Band treatment: applied for patient with grade 1 and early grade 2 haemorrhoids
which are too large to be handle by injection sclerotherapy, not used for grade 3
because it is very painful. We strangulate the base of the piles by a tight elastic
band (Barron’s bander) by using protoscope, this will cause ischemia to the piles
4
and it will slought off in about 10 days, this procedure can be done for all patient
but avoid doing more than 2 haemorrhoids to avoid mucosal bleeding and sever
mucosal discharge.
C- External infrared: by heating, photocoagulation occurs, leading to construction and
destruction of the pile itself.
D- Laser: also photocoagulation are used, and the results are best.
E- Cryosurgery: (no more in use) by application of liquid nitrogen after doing a local
anesthesia, inserting a probe at the tip of pile, stick and pass the pile and freeze it
by the liquid nitrogen. The danger of this procedure is that the center of the pile
will freeze faster than the surface, so unnoticed ice ball might be formed in the core
of the pile that may extend and affect the anorectal ring producing incontinence.
3- Surgery:
Indications
The indications for haemorrhoidectomy include:
• Third- and fourth-degree haemorrhoids;
• Second-degree haemorrhoids that have not been cured by non-operative treatments;
• Fibrosed haemorrhoids;
• Interoexternal haemorrhoids when the external haemorrhoid is well defined.
• Other strong indication is haemorrhoid bleeding that sufficient to cause anemia.
N.B. if pregnant women presented with haemorrhoids, try to avoid surgery as much as
possible, because haemorrhoids may resolve after pregnancy due to 1- disappearance of the
weight of the fetus, 2- progesterone secretion will be reduced.
N.B. if a pile strangulated without being ischemic, treat it by reducing the pile through
dilating the anus and pushing the pile internally (surgery avoided).
Technique:
It is usual for the patient to have been taking stool softeners in the days before surgery and a
preoperative enema to empty the rectum is administered. The procedure is usually performed
under general or regional anesthesia. The principles of operation is to transfixation, ligation
and excision of the internal and external pile by:
1- Open technique (Milligan–Morgan operation)
Slightly dilate the external sphincter, excise the pile from the pedicle outside through
(U) shaped dissection, then transfixation and ligation is performed, after that we leave
the wound open with good hemostasis, putting packs and gauze to avoid bleeding by
applying pressure.
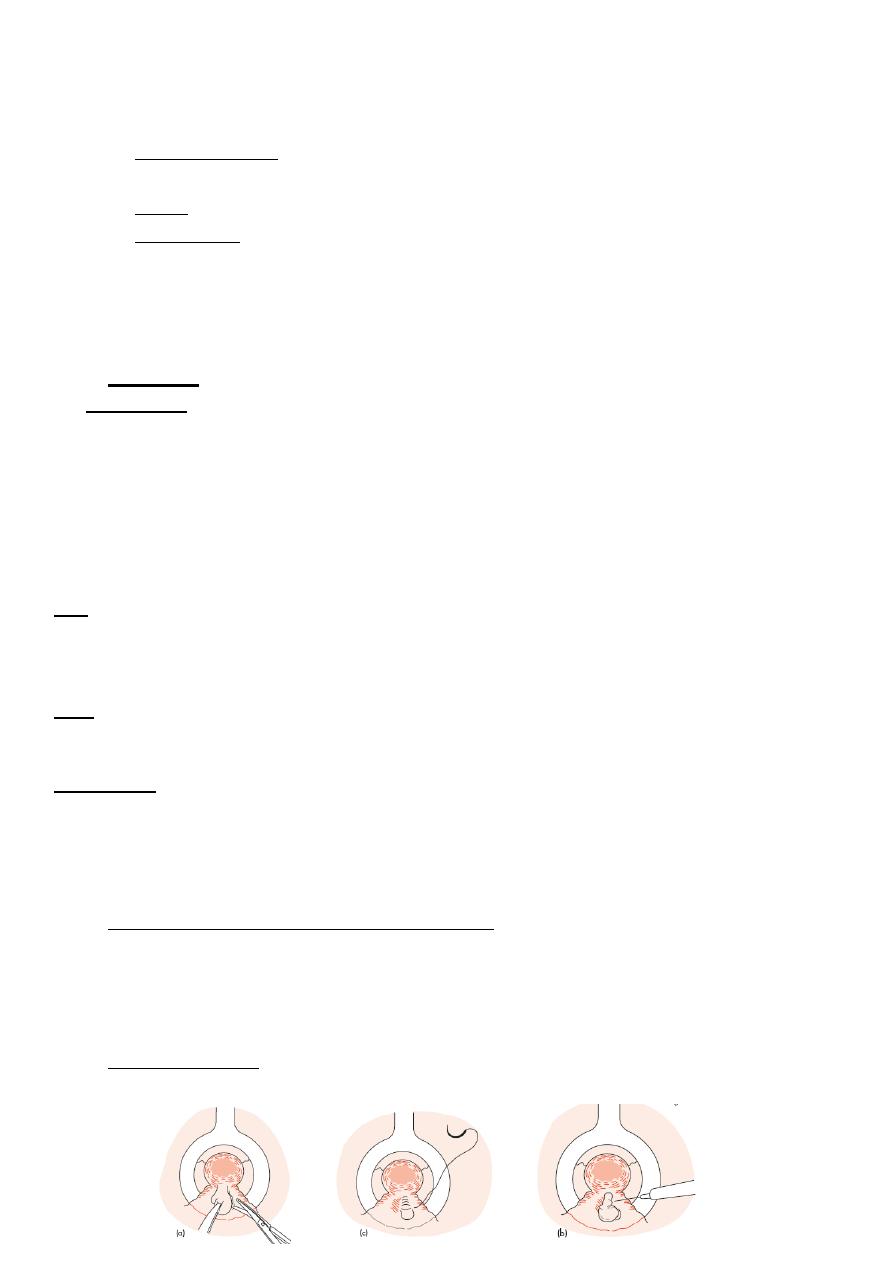
2- Closed technique:
The same as open but suturing of the area after operation should be performed.
5
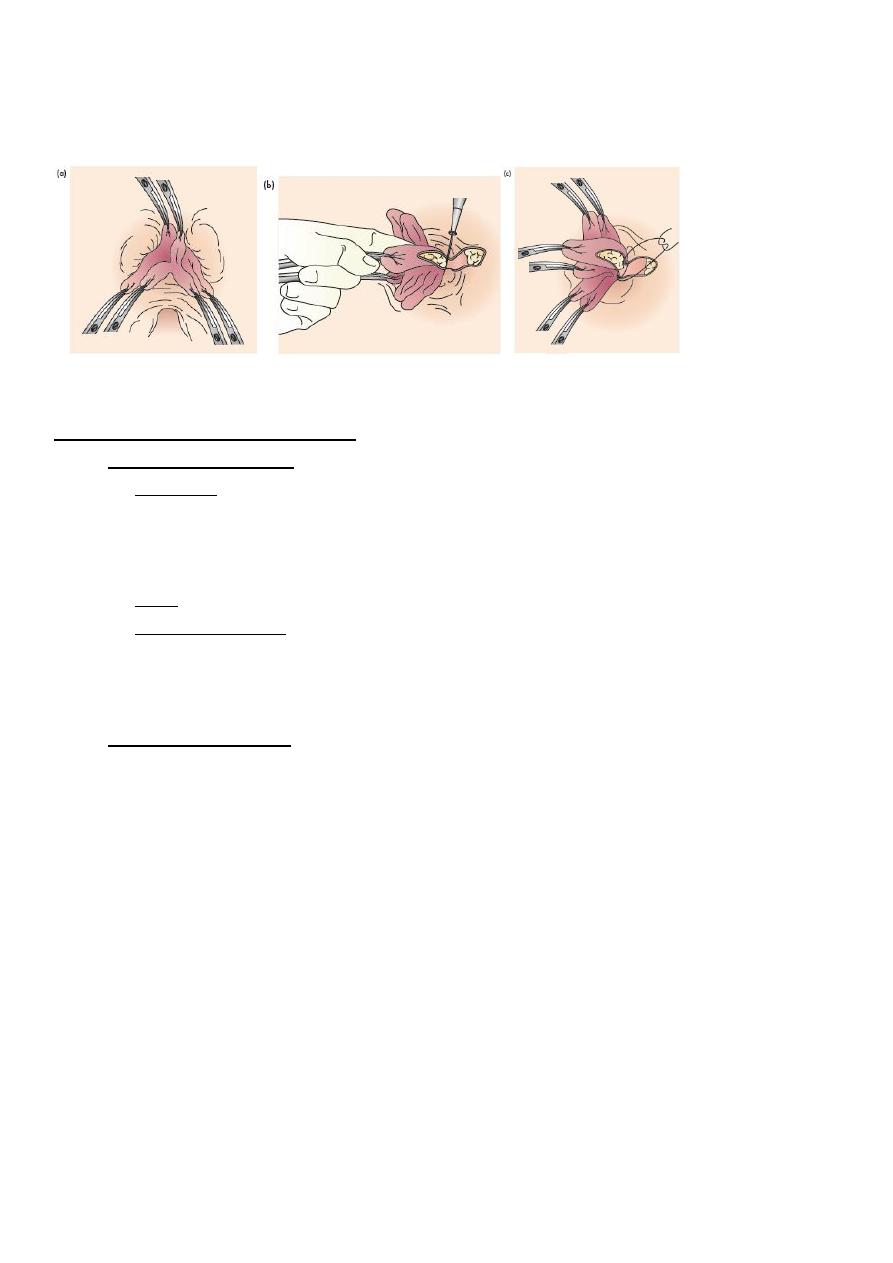
Closed technique of haemorrhoidectomy. (a) The haemorrhoidal tissue is excised. (b) Bleeding is controlled by diathermy.
(c) The defect is closed with a continuous suture after first undermining the anoderm on each side.
Ligation and excision of haemorrhoids. Open technique:
(a) The artery forceps have been applied; (b) dissection of the left lateral
Pedicle; (c) transfixion of the pedicle.
Post-operative Complications
A- Early complications:
1- Bleeding: due to either slipping of the pedicle ligature or band hemostasis, or
reactionary hemorrhage: if the bleeding is mild it may stop spontaneously, but if it
is sever we have to operate upon the patient in order to know the cause of bleeding
and stop it.
2- Pain: common complication and should be relieved by analgesia.
3- Urinary retention: because of pain, a spasm at the area, advice the patient to have
warm bath to induce urination, if it is not useful, then catheterization should be
considered.
B- Late Complications:
1- Anal fissure occur because of stricture which result from excessive removal of the
2- Recurrence: the piles are of 2 types primary one and secondary one, so recurrence
occur by missing excision of the secondary piles or piles not probably excised.
3- Secondary haemorrhage: This is uncommon, occurring about. It is usually
controlled by morphine.
4- Anal stricture: which must be prevented at all costs.
5- Incontinence: especially if there has been inadvertent damage to the underlying
internal sphincter. It is uncommon.
