1
4th stage
Surgery
Lec-4
Dr.Ahmed
4/17/2016
Management Of Haemmorriods
-Exclusion of other causes of rectal bleeding, especially colorectal malignancy, is the first
priority.
-In the absence of a specific cause, important measures:
1. Normalizing bowel and defaecatory habits (only evacuating when the natural desire
to do so arises).
2. Adopting a defaecatory position to minimise straining.
3. Addition of stool softeners and bulking agents to ease the defaecatory act in
constipated patients.
4. Various creams can be inserted into the rectum from a collapsible tube fitted with a
nozzle, at night and before defaecation.
5. Suppositories are also useful.
-Primary haemorrhoids;
In those with first or second degree piles whose symptoms are not improved by
conservative measures ---> injection sclerotherapy ,rubber band ligation , and
photocoagulation are successful .
For third and forth degree haemorroids ---> surgery is recommended.
-Secondary haemorrhoids :
Treatment is directed to the cause .
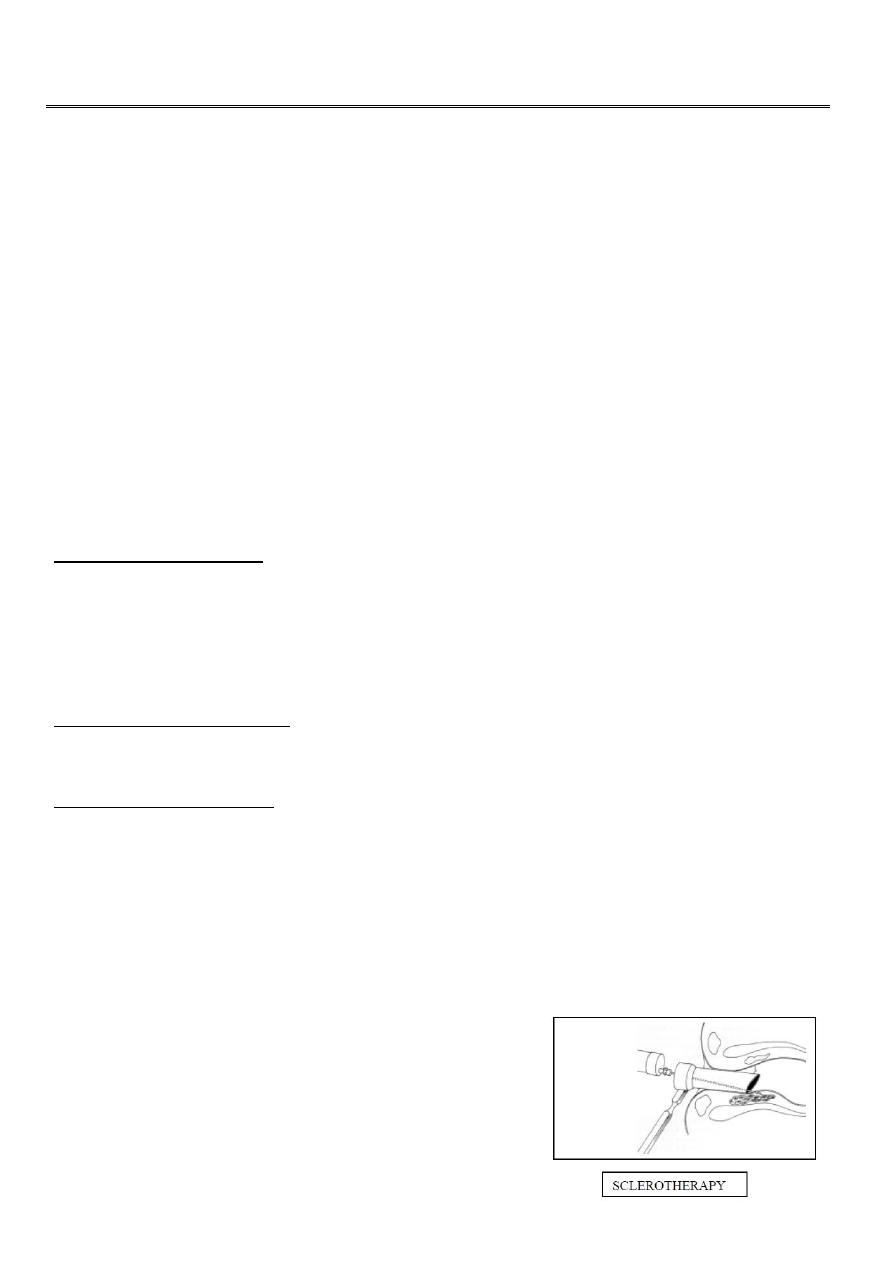
-Injection sclerotherapy:-
Indication for first and second degree piles, the idea is to inject sclerosing agent at
the submucosa at the pedicle of the piles, this lead to fibrosis.
Solution used 3 ml of 5% phenol in almond oil.
3 piles can be injected at the same time and can be repeated after 2-3 weeks.
Complications:-
1. Severe pain .
2. Necrosis of mucosa.
3. Allergic manifestations.
4. Submucous abscess formation.
2
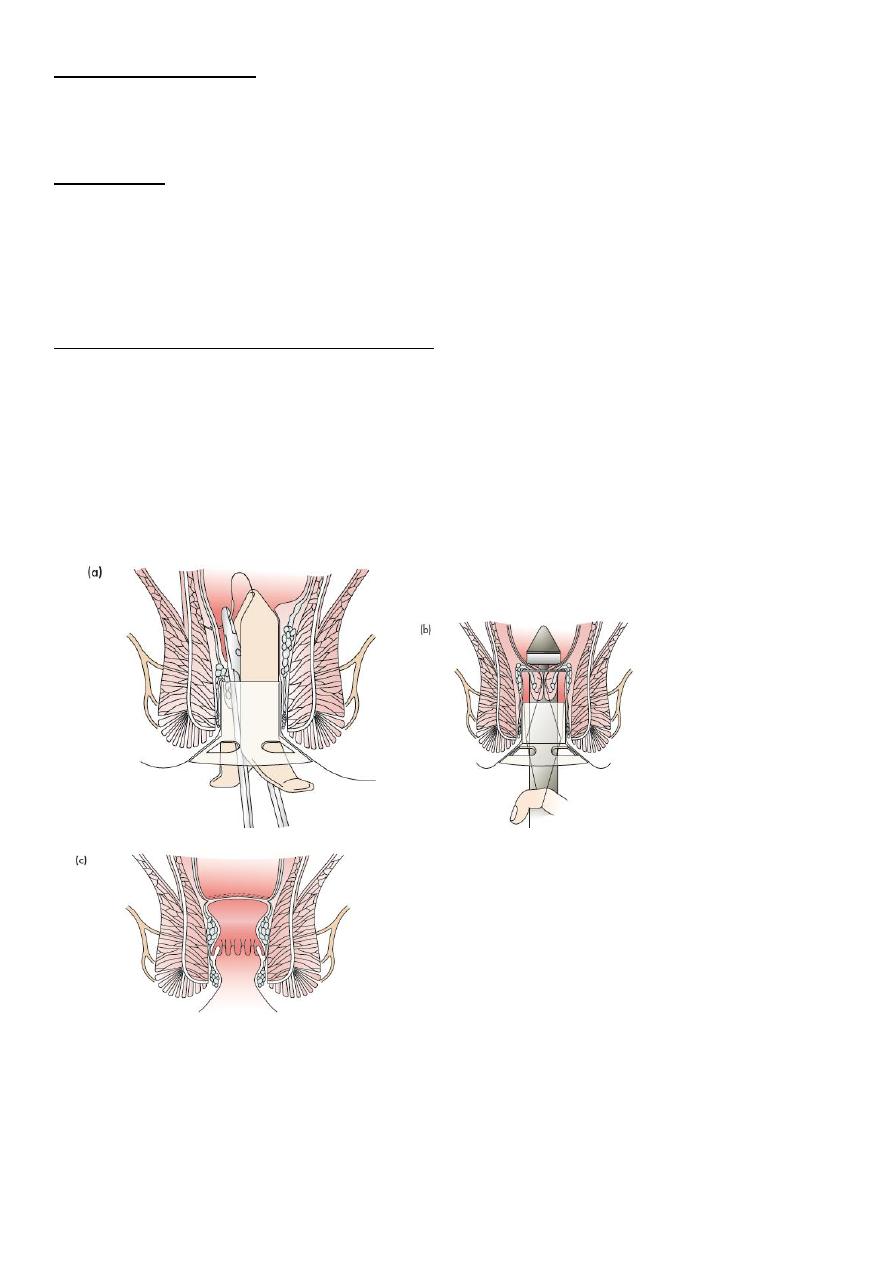
-Rubber band ligation:-
For 2nd and early third degree piles, place rubber band around the pedicle of the pile with
ischemic necrosis.
-Cryosurgery
The application of liquid nitrogen , The extreme cold (-196’C) of the application
causes coagulation necrosis of the piles, which subsequently separate and drop off.
the technique often caused mucus discharge and pain, and has now been
abandoned.
-Transanal Haemorrhoidal Dearterialisation
(THD) is used for the treatment of 2nd and 3rd-degree haemorrhoids.
Some have recently advocated transanal Doppler-guided ligation of those vessels
feeding the haemorrhoidal masses (ultriod), to which others have added suture
‘mucopexy’ to deal with any prolapse.
Longterm outcomes are unknown, but recurrence rates for fourth degree
haemorrhoids are high.
3
Indications Of Surgical Treatment
Cases unsuitable for injection or banding treatment are:
1. Third & 4
th
degree haemorrhoids.
2. Failure of nonoperative treatments of 2nd-degree haem.
3. Fibrosed haemorrhoids.
4. Intero-external haem, when the external haem, is well defined.
Some preoperative treatment is necessary:
The anal region is shaved.
On the morning of the operation the rectum is evacuated with the aid of a
disposable enema.
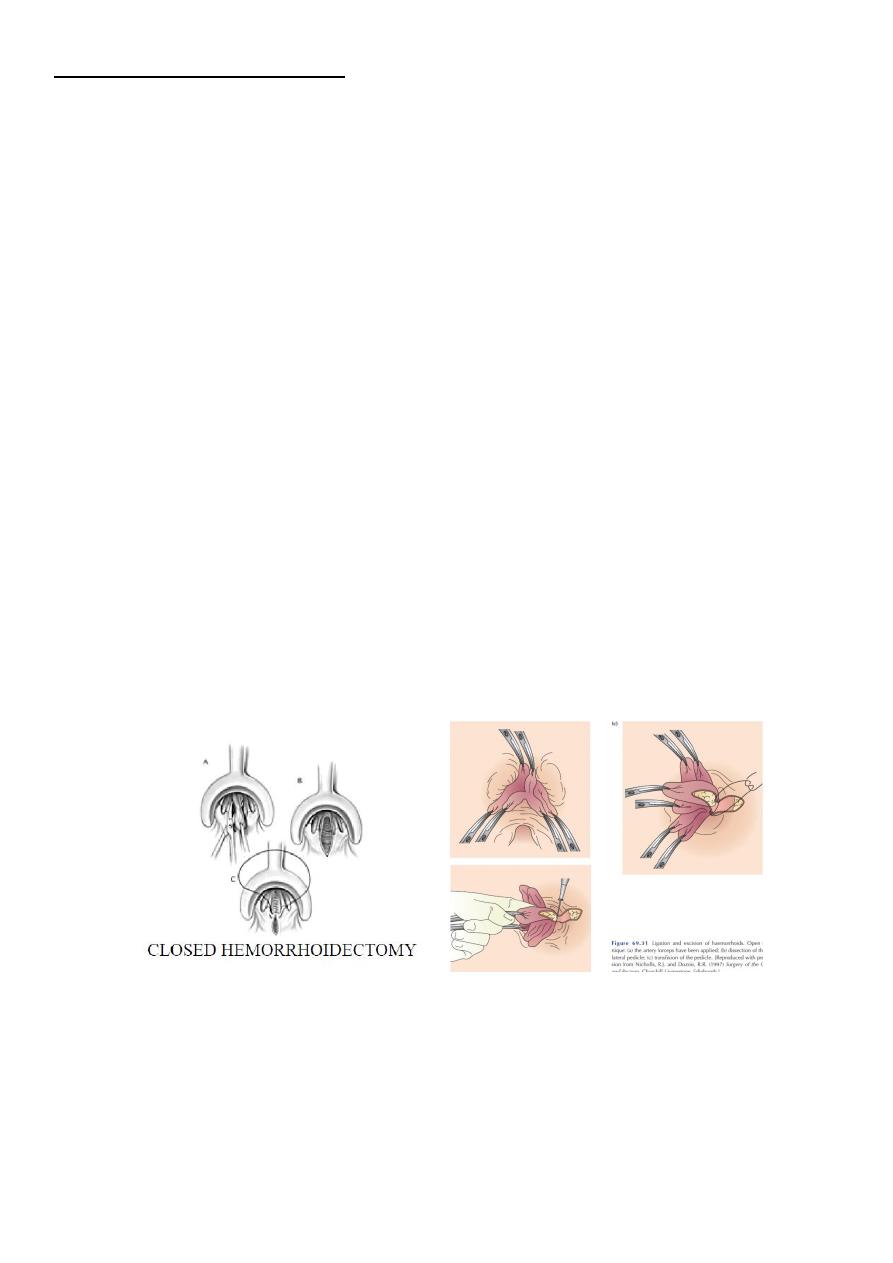
Haemorrhoidectomy
can be performed using an open or a closed technique.
The open
The technique is most commonly used , and is known as the Milligan-Morgan operation
named after the surgeons who described it.
The closed
Both involve ligation and excision of the haemorrhoid, but in the open technique the anal
mucosa and skin are left open to heal by secondary intention, and in the closed technique,
the wound is sutured.
Haemorrhoidectomy
G .A.
Excision of the piles.
Intact skin and mucosa between one pile and an other.
4
Postoperative care:
1. The patient is discharged from hospital within a day or two of the operation and
usually performed on a day care basis.
2. The patient is instructed to take two warm baths a day.
3. Given a bulk laxative to take twice daily.
4. Appropriate analgesia.
5. The patient is seen again 3-4 weeks after discharge and a rectal examination is
performed.
6. If there is evidence of stenosis, the patient is encouraged to use a dilator.
Management of Complications
-Hemorrhage :
Reactionary --> pressure or surgery with analgesia.
Secondary – > antibiotic with pressure and surgery.
-Retention of urine: conservative ---> if fails ---> catheterization.
-Anal stricture: post-operative anal dilatation.
-Recurrence: revision surgery.
-Incontinence : uncommon, serious problem that is difficult to treat.
-Fissure: conservative treatment or sphinctorotomy.

5
Treatment of prolapsed strangulated, thrombosis and gangrene
-Conservative treatment:
Rest in bed.
Antibiotics.
Analgesics.
Frequent bath.
Decongestant ointment : usually cause the pile mass to shrink in 3-4 days.
-surgery:
promote portal pyaemia, but if adequate antibiotic cover is given from the start early
excision can be done .
The other risk if surgery is performed at this stage, is that of postoperative stenosis,
results .
-An anal dilatation technique:
has in the past been used as an alternative treatment to surgery for painful
‘strangulated’ haemorrhoids. However, because of the risk of incontinence this is no
longer advised.
6
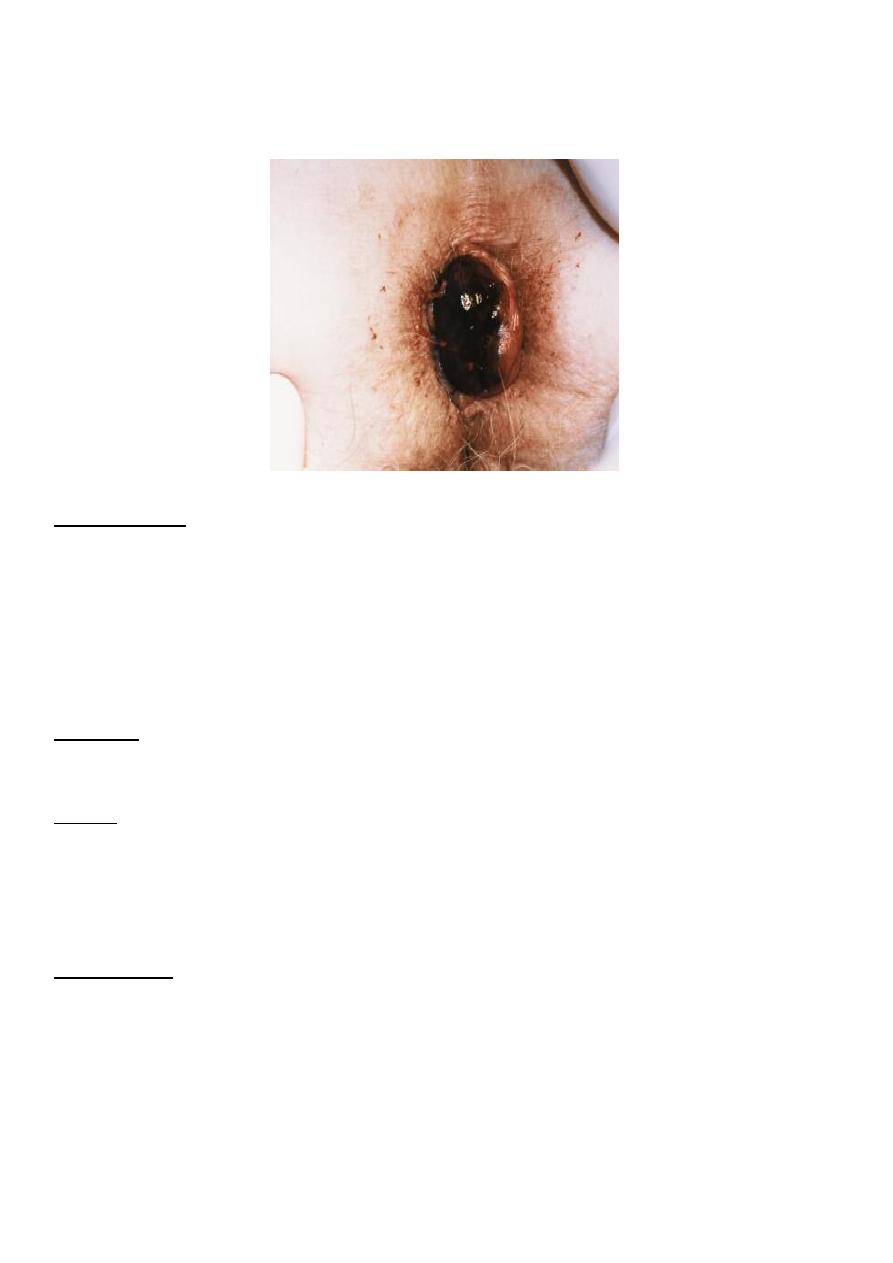
Thrombosed External Hemorrhoids
(Acute Perianal Haematoma)
Pathogenesis
: -
Acute and very painful problem that develops rapidly due to rupture in one of the
subcutaneous or submucosal dilated anal vein secondary to straining on defecation,
coughing or lifting heavy object, it lead to haemorrhage & clot formation usually in lateral
position.
Clinical:-
It appears as tense, tender, bluish swelling covered by smooth shining skin.
Fate: -
-
if untreated haematoma usually resolves, the body will eventually reabsorb the clot, but
might takes weeks
- it may suppurate, ulcerate, clot pass out or fibrosed.
Treatment:-
If patient present early surgical evacuation or excision done.
