1
Forth stage
Surgery
Lec-4
د. زيد
17/3/2016
Salivary Glands
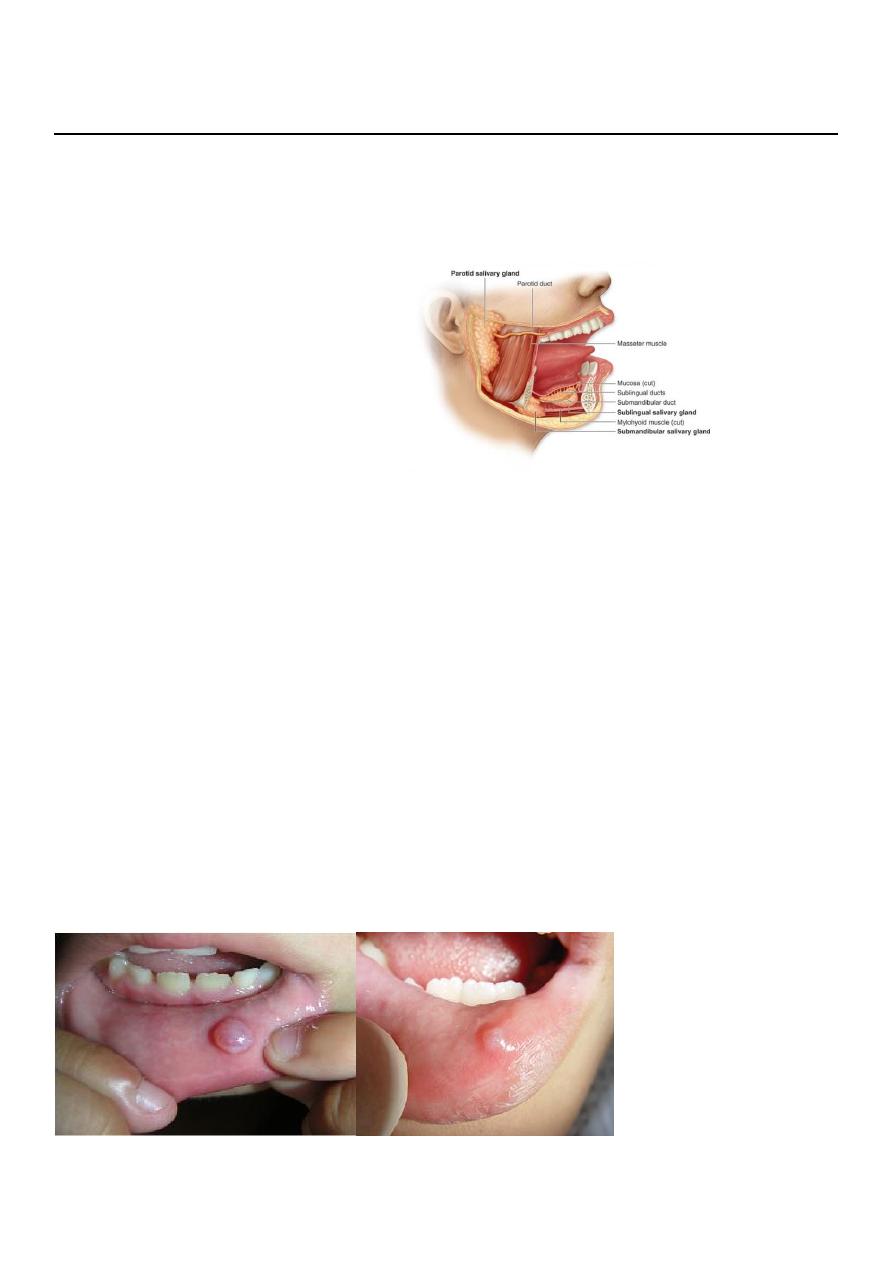
Anatomy of salivary glands:
Two submandibular glands
Two parotid glands
Two sublingual glands
Approximately 450 minor
salivary
glands
Common disorders
of minor
salivary glands
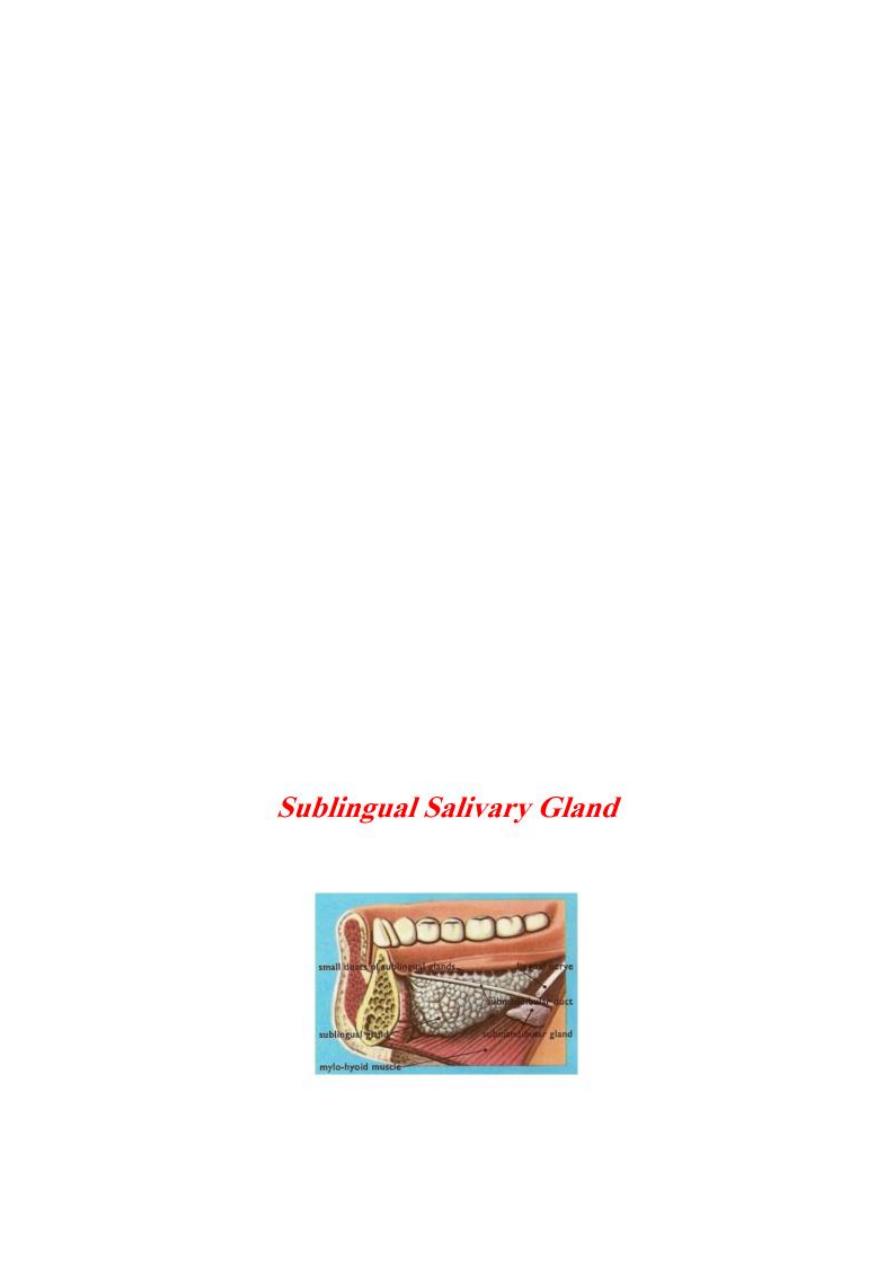
1- Extravasation Cysts
-
Common
-
trauma to the overlying mucosa.
-
affect lower lip producing painless swelling and usually translucent .
-
resolve spontaneously
-
most require formal surgical excision +overlying mucosa +underlying minor salivary
gland.
-
Recurrence is rare.
2
Tumours
of minor salivary glands
90 % malignant.
anywhere in the upper aerodigestive tract
common sites : upper lip, palate and retromolar regions.
Less common sites nasal and pharyngeal cavities.
Benign minor salivary gland tumors present as painless, firm, slow- growing
swellings.
Overlying ulceration is extremely rare.
Treatment: excision of the tumor +overlying mucosa+ primary closure
Malignant minor salivary gland tumours
rare.
Firm
discoloration overlying mucosa (pink to blue or black) .
late necrotic with ulceration.
Treatmentwide excision +/- partial or total maxillectomy + reconstruction.
3
Common disorders of the sublingual glands:
1- Cysts(ranula)
o mucous extravasation cyst that arises from a sublingualgland.
translucent swelling ‘frog’s belly’ .
o resolve spontaneously.
o many require formal surgical excision of the
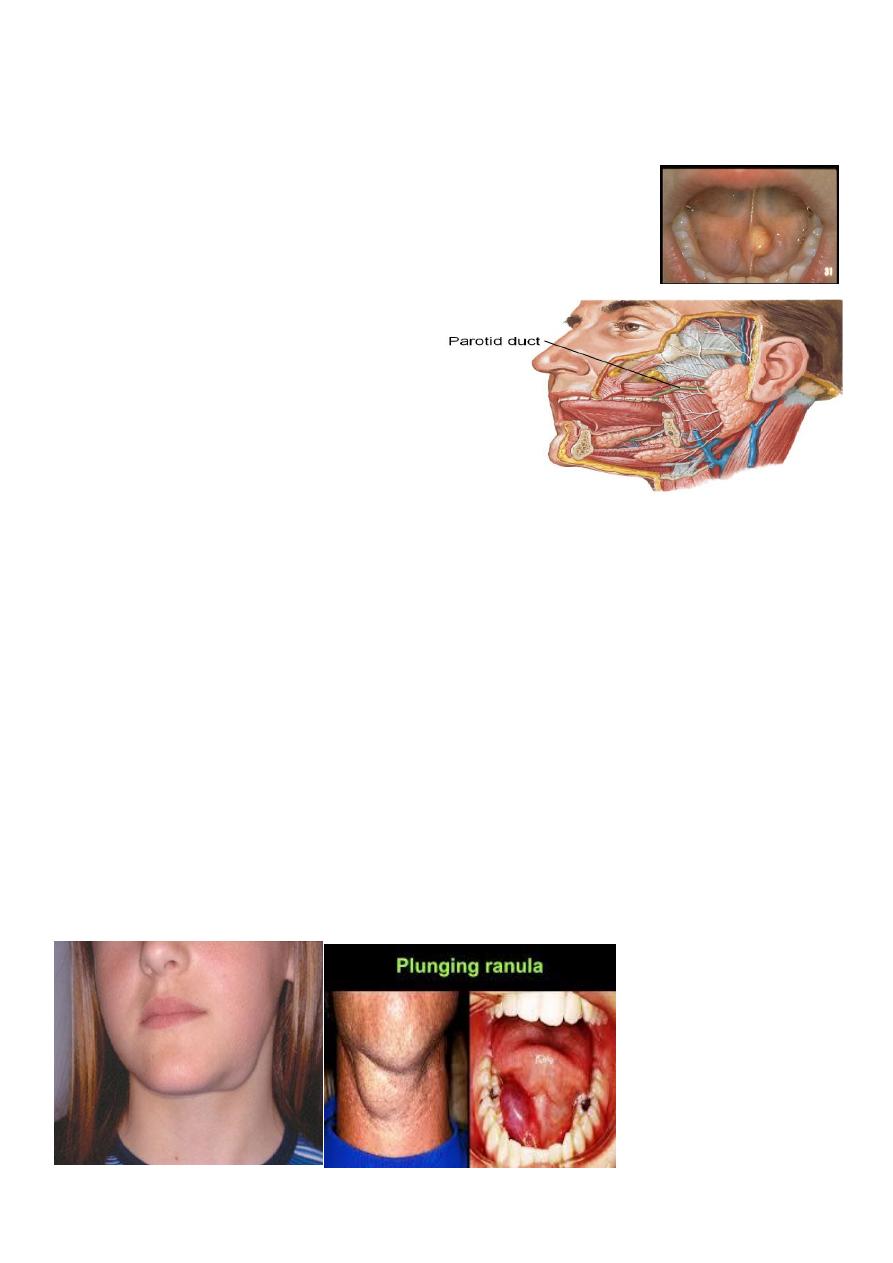
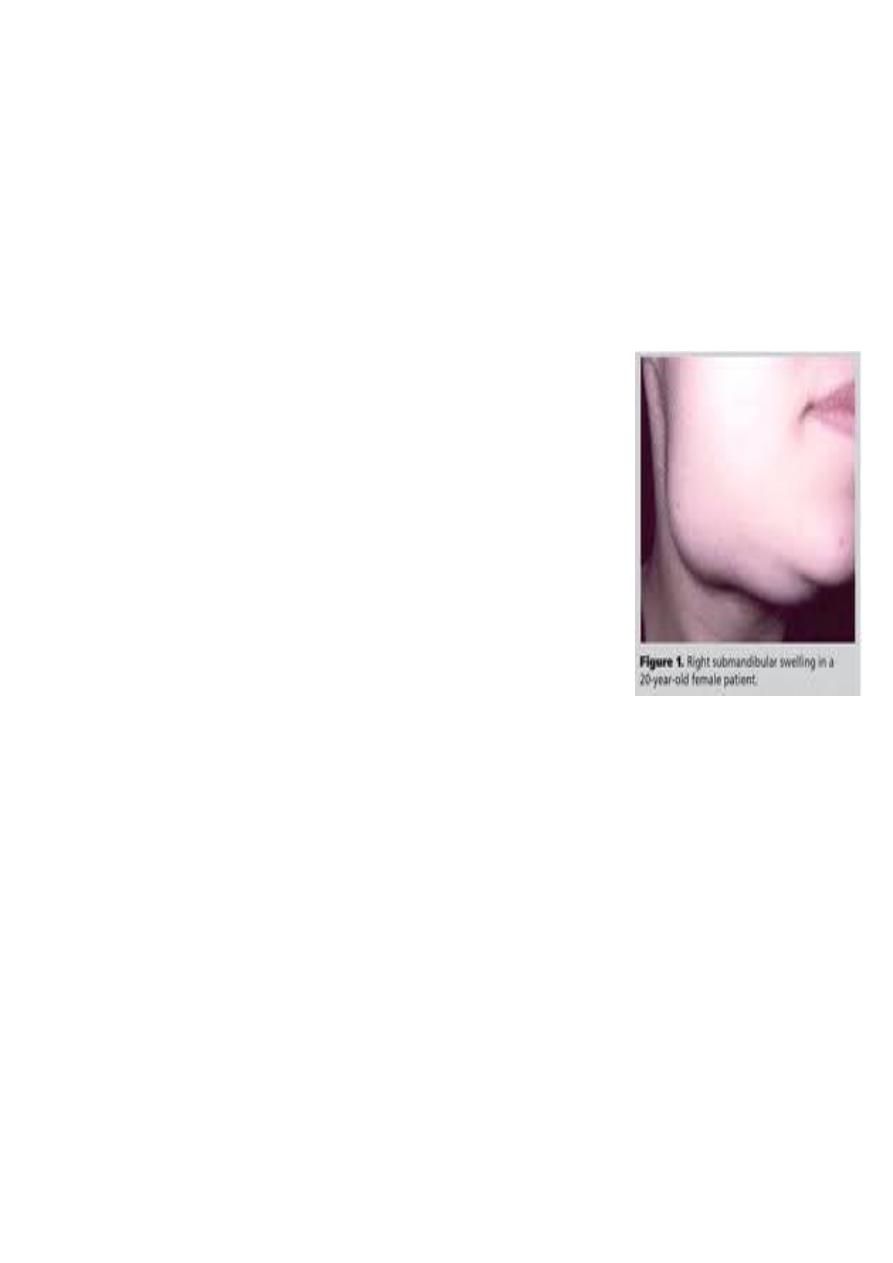
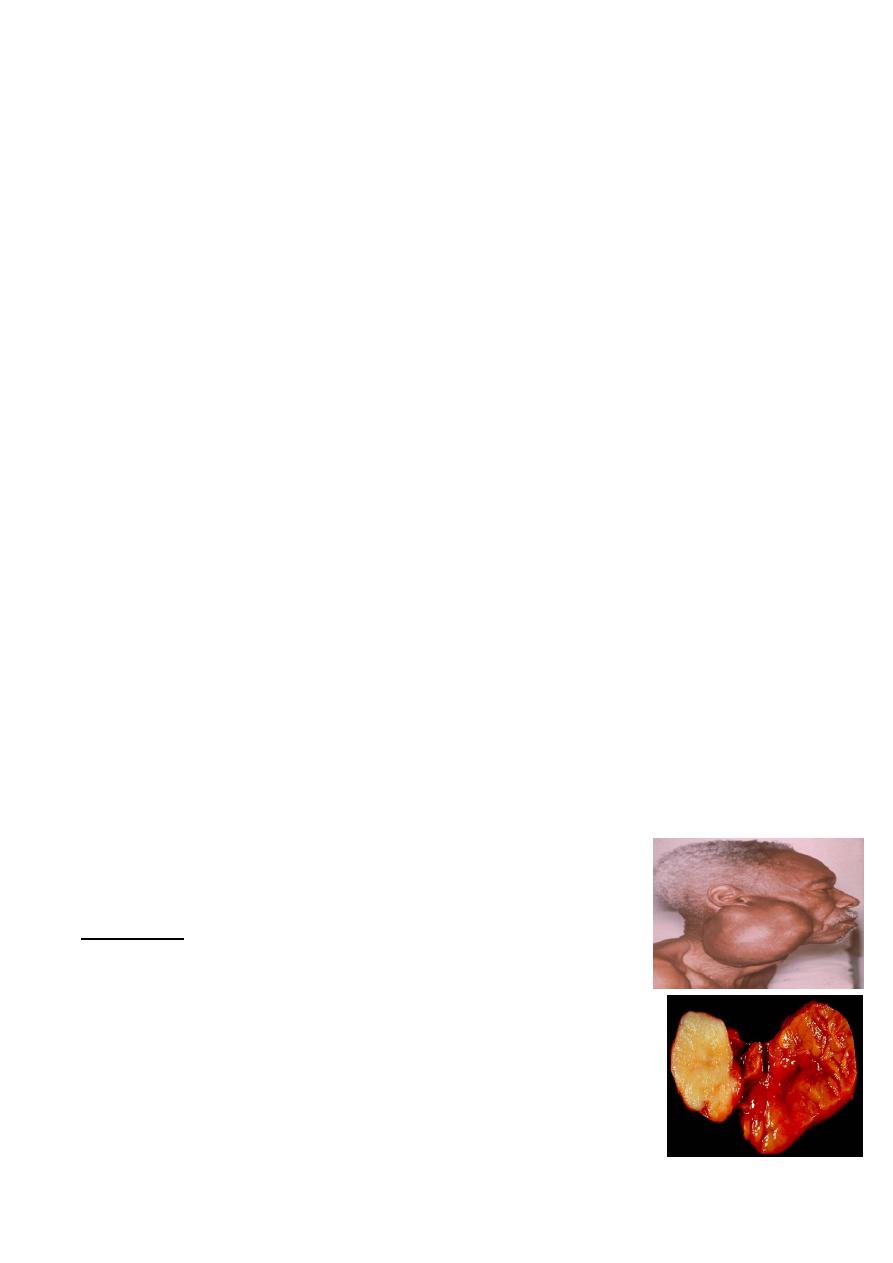
2- Plunging ranula
• rare mucous retention cyst
• arise from sublingual and
submandibular s g.
• Mucus collects within the cyst,
which perforates through the mylohyoid muscle diaphragm to enter the neck.
• dumb-bell-shaped swelling
• fluctuant
• Painless
• Soft
• in the submandibular or submental region of the neck .
• Diagnosis : ultrasound or magnetic resonance imaging (MRI).
• Treatment:
- Excision transcervical ( removing the cyst+ submandibular+ sublingual glands).
- Smaller plunging ranulas transoral sublingual gland excision+/- marsupialisation.

4
Tumors of sublingual:
- extremely rare
-
85 per malignant.
-
hard or firm
-
painless swelling
-
in the floor of the mouth.
-
Treatment:
wide excision + overlying mucosa+ neck dissection. +reconstruction
THE SUBMANDIBULAR GLANDS
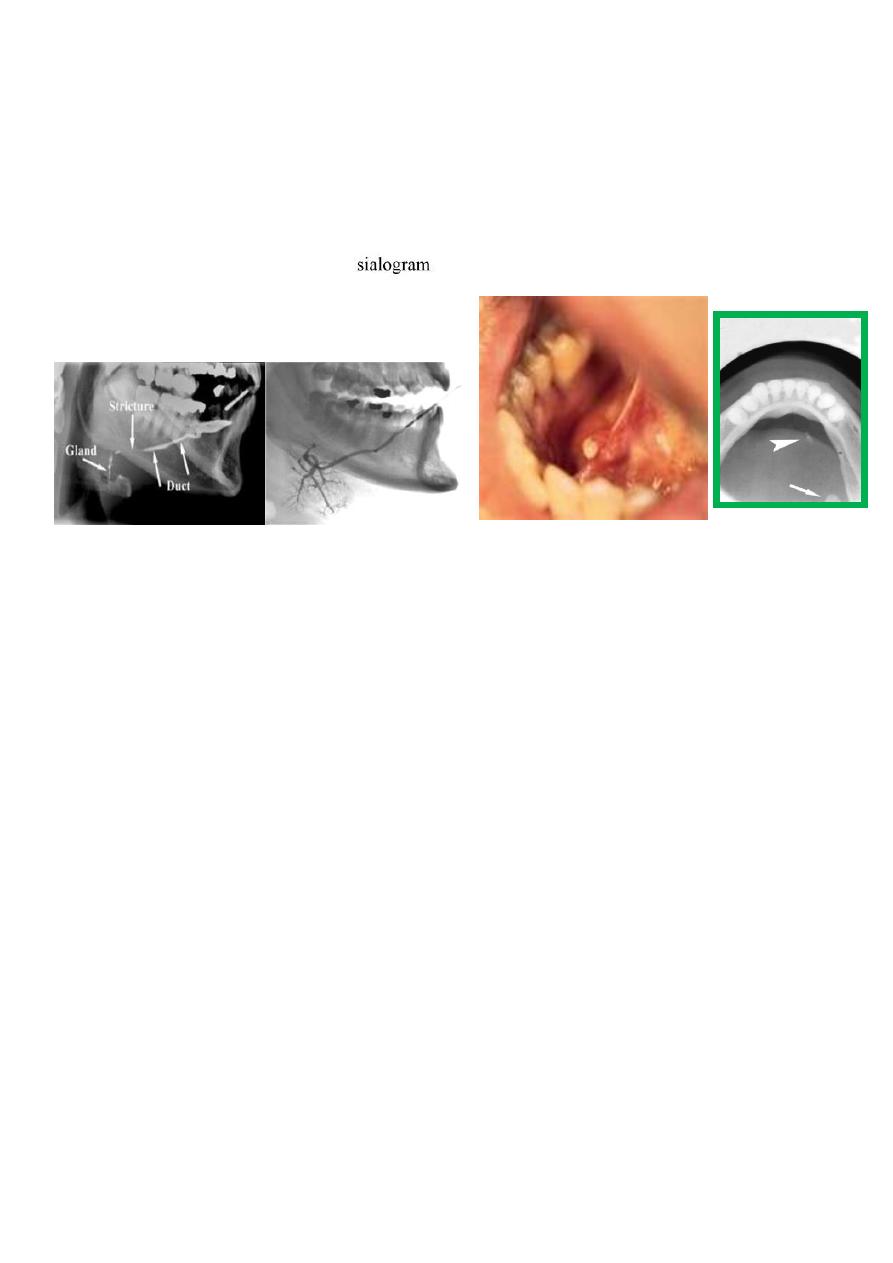
Ectopic/aberrant salivary gland tissue\Stafne bone cyst
- most common ectopic salivary tissue .
-
Asymptomatic
-
clearly demarcated radiolucency of the angle of the mandible.
-
below the inferior dental neurovascular bundle.
-
No treatment is required.
Inflammatory disorders of the submandibular gland(
sialadenitis
)
acute, chronic or acute on chronic.
Common causes are:
Acute submandibular sialadenitis:
1- Bacterial sialadenitis
-
more common than viral sialadenitis
-
secondary to obstruction.
-
antibiotics, if chronically inflamed
formal excision.
2- Viral. The paramyxovirus (mumps)

5
-
Usually parotitis.
-
occasionally submandibular glands
-
painful tender swollen glands.
-
Other viral infections rare.
Chronic submandibular sialadenitis.
Obstruction and trauma to submandibular gland
-
Stone formation (sialothiasis): most common cause of obstruction within the
submandibular gland is within the gland and duct system.
-
80%of all salivary stones occur in the submandibular glands because highly viscous
secretions .
-
80% submandibular stones are radio-opaque
Clinical symptoms
• acute painful swelling in the region of the submandibular gland
• precipitated by eating
-
completely obstruct(less common) opening of the submandibular ductswelling
develop rapidly 1–2 hours after the meal resolves spontaneously
• partial obstruction(more common) (hilum of the gland or within duct in the floor of
the mouth)
- infrequent symptoms
- minimal discomfort and swelling
- not confined to mealtimes.
- examination enlarged firm submandibular gland, tender on bimanual
examination.
-
Pus from the sublingual papilla .
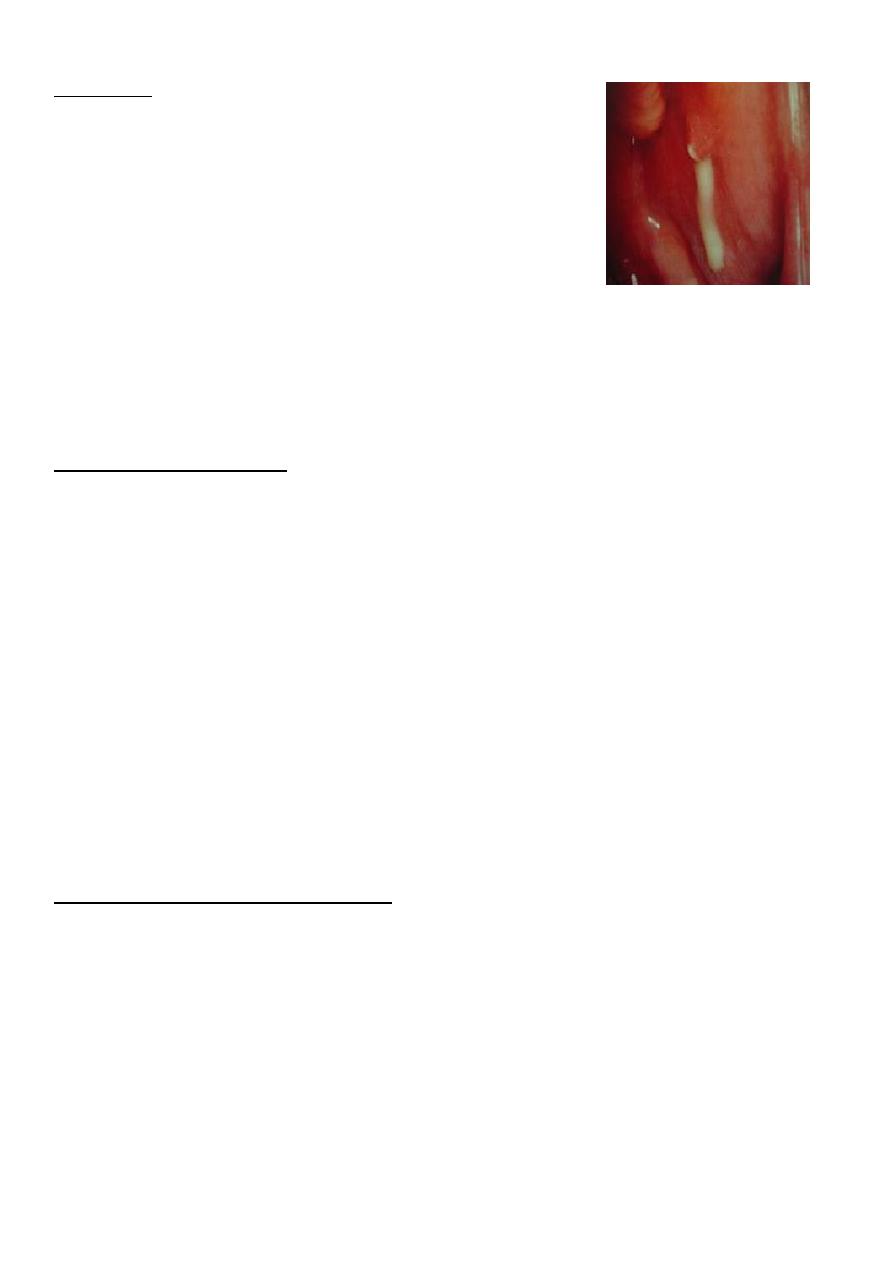
Management
stone within the submandibular duct in the floor of the mouth anterior to the point at
which the duct crosses the lingual nerve (second molar region) incising over the
duct+stone delivered+ leave the wall of the duct
6
stone is proximal to the lingual nervesubmandibular gland excision a removal of the
stone + ligation of the submandibular duct
endoscopic retrieval of stone, lithotripsy(sialadenoscope)
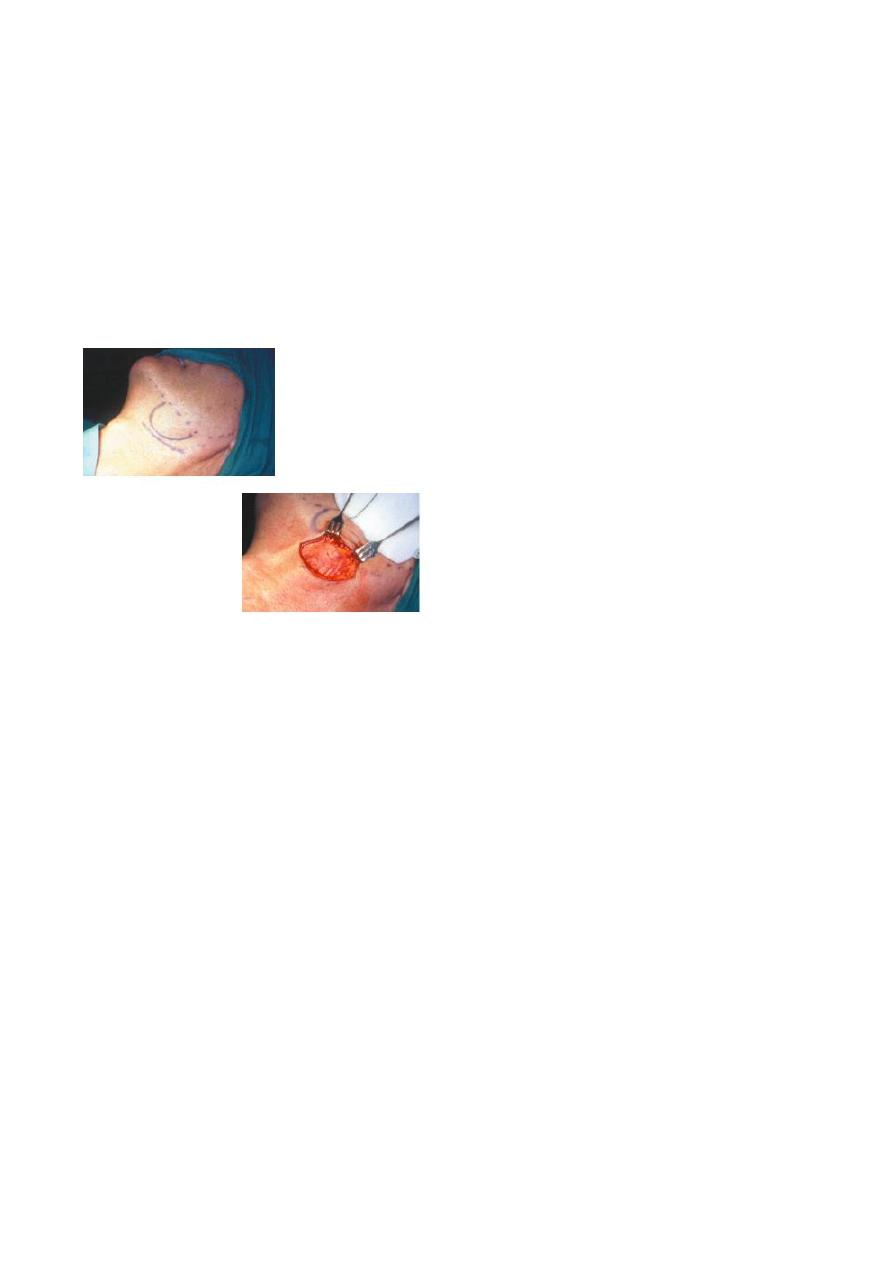
Submandibular gland excision
Indication:
sialadenitis
Salivary tumours.
Complications
:
• haematoma
• wound infection
• marginal mandibular nerve injury
• lingual nerve injury
• hypoglossal nerve injury
• transection of the nerve to the mylohyoid muscle producing submental skin anaesthesia
7
Tumours of the submandibular gland
-
uncommon
-
(benign and malignant)present as a slow-growing, painless swelling within the
submandibular triangle.
-
50 % of submandibular gland tumours are benign.
-
pain is not a reliable indication of malignancy as benign tumours often present with
pain in the affected gland, presumably due to capsular distension or outflow
obstruction.
Clinical features of malignant salivary tumours
• facial nerve weakness
• rapid enlargement of the swelling
• induration and/or ulceration of the overlying skin
• cervical node enlargement.
Investigation
1-Computed tomography (CT) and MRI scanning
the extension, circumscribed (benign, or diffuse, invasive and probably malignant).
2- Biopsy
Open surgical biopsy is contraindicated as this may seed the tumour into surrounding
tissues, making it impossible to eradicate microscopic deposits of tumour cells.
Fine-needle aspiration biopsy : no risk of seeding viable
Management of submandibular gland tumours
surgical excision with a cuff of normal tissue is the goal.
- Small tumor+ localised ( entirely within the submandibular gland parenchyma)
intracapsular submandibular gland excision is
8
- Benign tumors (large and beyond the submandibular gland) suprahyoid neck
dissection
(preserving the marginal mandibular branch of the facial nerve, lingual nerve and
hypoglossal nerves).
- Overt malignancymodified neck dissection /radical neck dissection .
(may sacrifice of the lingual and hypoglossal nerves )
THE PAROTID GLAND
Developmental disorders
-
Rare
-
agenesis, duct atresia and congenital fistula
Inflammatory disorders
Viral infections
Mumps (most common)
-
acute painful parotid swelling
-
Mostly affects children.
-
spread by airborne droplets .
9
-
1–2 days fever, nausea and headache
-
pain and swelling in parotid glands.
-
pain very severe and exacerbated by eating and drinking.
-
Symptoms resolve within 5–10 days.
-
Treatment : regular paracetamol + adequate oral fluid intake.
-
Complications
orchitis, oophoritis, pancreatitis, sensorineural deafness and
meningoencephalitis are rare.
Other viral agents that produce parotitis include: Coxsackie A and B, parainfluenza 1 and 3,
Echo and lymphocytic choriomeningitis.
Bacterial infections
Acute ascending bacterial sialadenitis
dehydrated elderly patients following major surgery
Reduced salivary flow ascending infection.
-
Staphylococcus aureus /Streptococcus viridans
-
Can occur with no obvious precipitating factors.
-
presentation tender, painful parotid swelling that arises over several hours .
-
generalised malaise, pyrexia and occasional cervical lymphadenopathy.
-
The pain is exacerbated by eating or drinking.
The parotid swelling may be diffuse/localises (lower pole
of the gland)
Pus may exuding from the parotid gland papilla
11
Treatment:
- intravenous antibiotics.
abscess drainage (large bore needle aspiration / drainage
under general anaesthesia.
Chronic bacterial sialadenitis is rare in the parotid gland.
- Recurrent parotitis of childhood
- Obstructive parotitis
Papillary obstruction
-
less common than obstructive submandibular sialadenitis
-
caused by trauma to the parotid papilla
-
overextended upper denture flange or a fractured upper molar tooth.
-
inflammation and oedema obstructs salivary flow(mealtimes)
rapid onset pain and swelling at mealtimes.
-
untreated progressive scarring and fibrosis in and around the parotid duct papilla
will produce a permanent stenosis.
-
Treatment: papillotomy(under either local or general anaesthesia).
Stone formation(Sialolithiasis)
- less common in the parotid gland (20 %)(submandibular gland (80 %).
- Parotid duct stones radiolucent.
- Stone either proximal in the collecting duct or distal near the papilla.
- Diagnosis: Parotid gland sialography.
- Treatment: stone located in the collecting duct or within the gland endoscopic
retrieval, lithotripsy or rarely parotidectomy.

11
Tumours of the parotid gland
- The parotid gland is the most common site for salivary tumors.
-
Most tumors arise in the superficial lobe
-
80–90 % of tumours of the parotid gland are benign
-
the most common is pleomorphic
-
Slow growing, painless swellings below the ear, in front of the ear or in the upper
aspect of the neck.
- Less commonly, tumors in accessory lobe persistent swellings in the cheek.
- Rarely, tumours in deep lobe as parapharyngeal massesdifficulty in swallowing
and snoring.
Malignant salivary gland tumours are divided into two distinct subgroups:
1- Low-grade malignant tumours, e.g. acinic cell carcinoma,
are indistinguishable on clinical examination from benign
neoplasms.
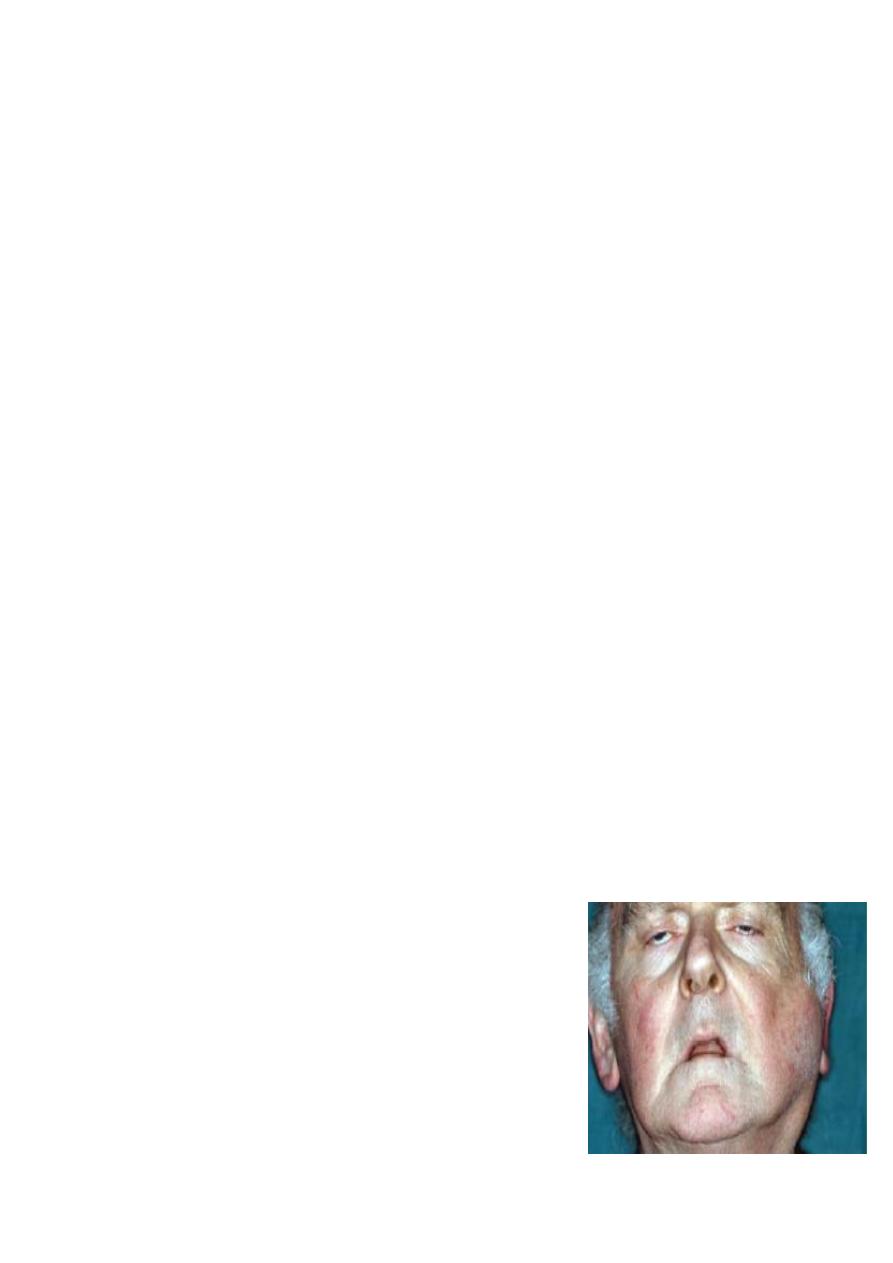
2- High-grade malignant tumours :
-
Rapidly growing
-
painless swellings
-
discrete mass with infiltration into the overlying skin
-
or diffuse + hard swelling + no discrete mass(advanced disease)
- Cervical lymph node metastases.
Investigations
CT and MRI scanning
Fine-needle aspiration biopsy
(open surgical biopsy is contraindicated )
(no enucleation even if a benign lesion is suspected)

12
Treatment of parotid tumor
Superficial parotidectomy
for Superficial lobe tumor
The aim of superficial parotidectomy is to remove the tumor with a cuff of normal
surrounding tissue.
Low-grade malignant tumours superficial parotidectomy.
Radical parotidectomy
Indicated in high-grade malignant tumour(squamous cell carcinoma)
Radical parotidectomy = removal of all parotid gland tissue +sectioning of the facial nerve+
ipsilateral masseter muscle +/- neck dissection(if positive LN mets.)
Complications of parotid gland surgery:
• haematoma formation;
• infection
• temporary facial nerve weakness
• transection of the facial nerve and permanent facial weakness
• sialocoele
• facial numbness
• permanent numbness of the ear lobe associated with great auricular nerve transection;
• Frey’s syndrome.
13
Frey’s syndrome
:Frey’s syndrome (gustatory sweating)
-
damage to the autonomic innervation of the salivary gland with inappropriate
regeneration of parasympathetic nerve fibres that stimulate the sweat glands of
the overlying skin.
-
sweating and erythema over the region of surgical excision of the parotid gland as
a consequence of autonomic stimulation of salivation by the smell or taste of
food.
-
Dgxstarch iodine test.
-
Rx
antiperspirants( aluminium chloride)
denervation by tympanic neurectomy; botulinum toxin injection into the affected skin.
Pleomorphic adenoma
-
Benign Tumor
-
- On gross inspection : tumors is smooth and lobular and demonstrates a well
defined capsule
-
On microscopic examination : both epithelial and mesenchymal elements are
present
-
MOST COMMON NEOPLASM IN THE PAROTID GLAND ACCOUNTS FOR 65% OF ALL
OF THE PAROTID TUMORS.
-
The most common salivary T.
-
In middle aged & more in woman than in men,
-
Slowly growing
Treatment :
-
Superficial parotidectomy
-
WIDE RESECTION OF THE TUMOR
-
AVOID SHELLING OUT THE LESION
-
RECURRENCE: PRIMARY DUE TO INADEQUATE RESECTION
-
LESIONS ARE MORE AGGRESSIVE WHEN THEY RECUR

14
WARTHIN’S TUMOR (ADENOLYMPHOMA)
-
SECOND MOST COMMON PAROTID TUMOR
-
MALE : FEMALE 5 : 1
-
BILATERAL 10%
-
May (MULTICENTRICITY).
-
TREATMENT: superficial parotidectomy
-
90%CURED WITH RESECTION
-
10%RECUR DUE TO MULTICENTRICITY OR INADEQUATE RESECTION
Malignant neoplasm
-
Mucoepidermoid carcinoma
-
Adenoid cystic carcinoma
-
Acinic cell carcinoma
-
adeno carcinoma
-
Carcinoma Ex. Pleomorphic adenoma or malignant mixed tumor
-
Squamous cell carcinoma
-
Undifferentiated carcinoma
-
Miscellaneous
Other diseases of salivary glands
A-Granulomatous sialadenitis:
-
Mycobacterial infection
-
Sarcoidosis
B-Tumour-like lesions
-
Sialadenosis
C-Degenerative conditions
- Sjögren’s syndrome
autoimmune condition causing progressive
destruction of salivary and lacrimal glands.
- Benign lymphoepithelial lesion
Xerostomia(decrease salivary flow)
Sialorrhoea(increase salivary flow)
