1
Forth stage
Surgery
Lec-5
Dr.Samer
28/2/2016
Stomach & Duodenum
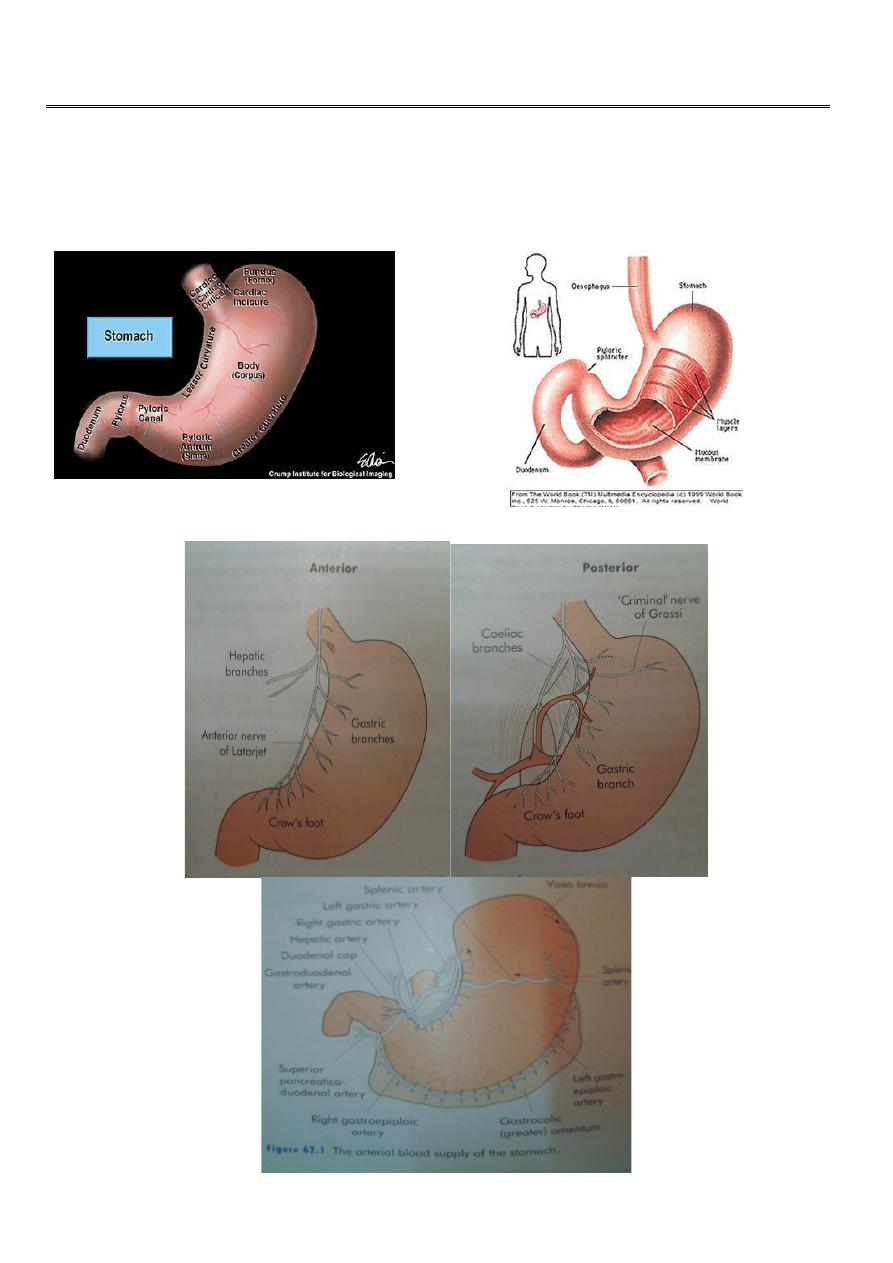
Gross anatomy of stomach
2
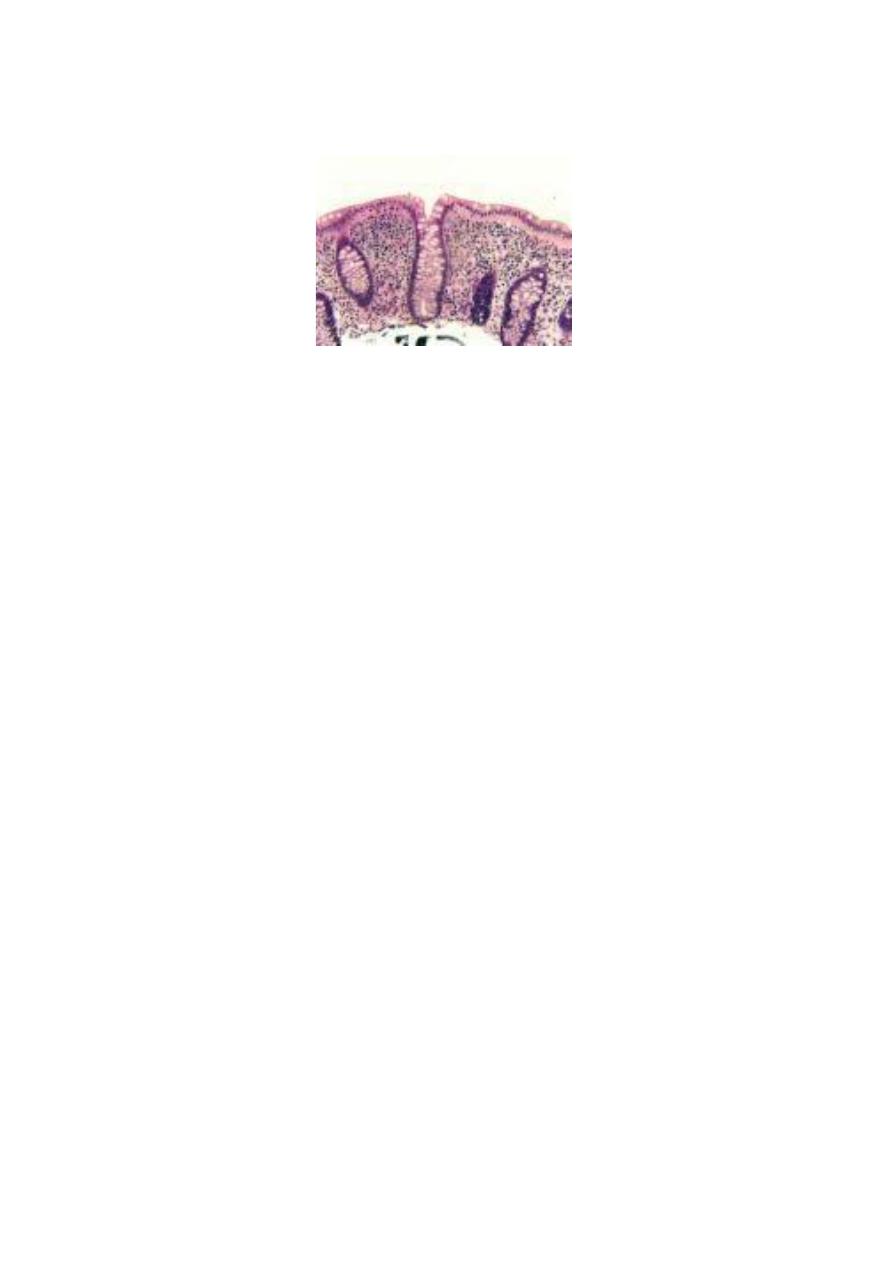
Microscopic anatomy :
The gastric epithelial cells are mucus producing and turned over rapidly
In the pyloric part , mucus secreting glands are found
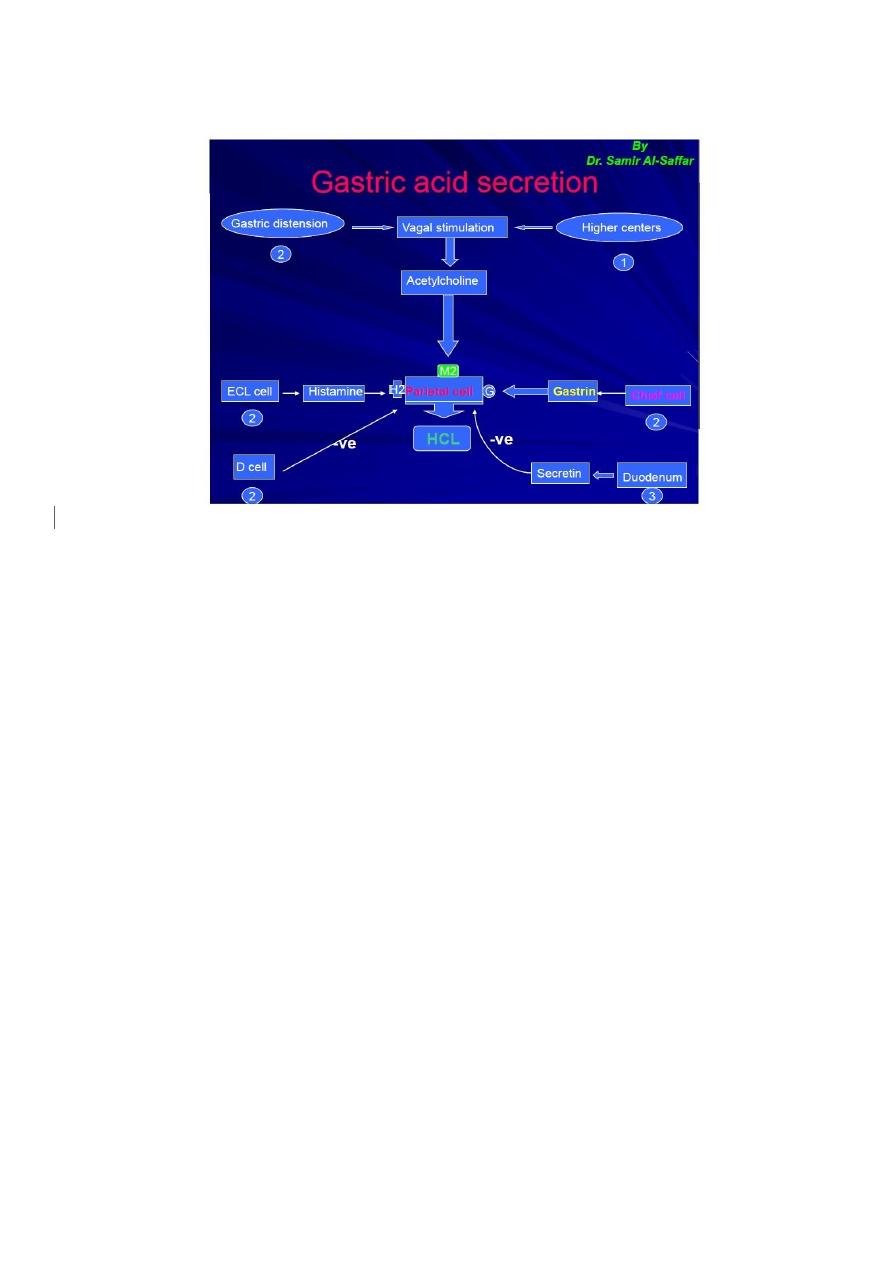
Parietal cells : Present in the body”acid-secreting” of stomach , Responsible for acid
secretion
Chief cells : Pepsinogen
Endocrine cells :
G cells; in the gastric antrum---gastrin
Enterochromaffin-like (ECL) cells ---Histamine
D cells ---somatostatin
Microscopic anatomy of Duodenum :
Lined by mucus secreting columner epithe
Brunner’s glands
Endocrine cells----cholecystokinin secretin
Physiology :
Storage “reservoir”
Mechanical break up of ingested food
Production of chyme by the actions of acid and pepsin
Programmed passage of contents into duodenum
3
Gastric acid secretion :
Investigation of stomach and duodenum :
Flexible Endoscopy:
Is more sensitive than conventional radiology in the assessment of the majority of GD
conditions, e.g. peptic ulceration, gastritis, and duodenitis.
Upper GIT bleeding
Early gastric cancer
Diagnostic:
Visual
Biopsy
Endoluminal Ultrasound
Therapeutic:
Control of bleeding, inj. Laser, diathermy
Endoscopic gastro-cystostomy
Endoscopic Gastrostomy
Removal of Foreign bodies
Disadvantages:
Invasive, discomfort
Perforation, of pharynx, oesophagus
Miss-diagnosis,early gastric cancer.

4
Contrast radiology
Less commonly asked for
Of value in;
Hiatus Hernia specially of the rolling type
Volvulous of stomach
Linitus plastica
Ultrasonography
Conventional US
Detection of large gastric tumor
Metastases to liver
Endoluminal US
Depth of wall invasion” T staging”
Local LN
Liver metastases
Laparoscopic US
CT scan and MRI
CT scan
In Gastric malignancy
Miss smaller lesions
Less accurate in T staging
Less easy to detect small liver metastases
MRI
Higher sensitivity for detection of gastric cancer liver metastases
Laparoscopy
Well used for assessment of patients with gastric cancer
Particularly for detection of peritoneal seedlings
Other investigations
Gastric emptying studies
Angiography
Measurement of gastric acid secretion
Gastric motility
Plasma gastrin

5
Paediatric Disorders :
1. Hypertrophic pyloric stenosis of infancy
Aetiology:
3:1000 births
4:1 male to female
Familial
Pathology:
Hypertrophy of musculature of pylorus and adjacent antum
Clinical features :
Commonly present at 4 wks of age
Vomiting of milk without bile---2-3 days become forcible and projectile
Immediately after vomiting, the baby is usually hungery
Wt loss---emaciation, dehydration
Diagnosis
Test feed
Imaging:
Ultrasonography Olive mass
Contrast radiology no longer necessary
Differential Diagnosis
Gastro-oesophageal reflux
Feeding problems
UTI
Raised intracranial pressure
Treatment
Correction of dehydration and electrolyte abnormalites; by using Dextrose
saline plus potassium
Followed by Operation “ Ramstedt’s”

6
2. Duodenal Atresia
Occur at the point of fusion between the foregut and midgut, in the neighbourhood
of the ampulla of Vater.
Other defects
Antenata Dx : US
The child vomits from birth and the vomitus is bile stained
Differential DX. : High intestinal obstruction , Pyloric stenosis
Treatment : Duodenoduodenostomy
3. Helicobacter Pylori
Proved its importance in the aetiology of ch.gastritis, peptic ulceration,and cancer
Waren and Marshal in 1980 proved casual relation between HP and Gastritis
HP is spiral shaped, able to hydrolyse urea to ammonia “a strong alkali”
Spread Feco-oral
Incidence 80 –90 %
Pathogensis
o Antral gastritis---relase of ammonia---decrease in acidity---G cell stimulation--
increase gastrin----increase in HCL
o Disruption of gastric mucosa through a number of cytotoxins
Diagnosis of HP infection
o Brith test
o CLO
o Histological examination of biopsy
o Serological tests
Treatment
Eradication therapy :
o Combination of antibiotics like : Metronidazol + Amoxil or Claithromycin +
Amoxil
o With the use of proton pump inhibitor like : Omerprazol, Lansoprazol
7
Gastritis
Type A gastritis :
----achlorhydria
----hypergastrinaemia----
Hypertrophy of ELC
Type B gastritis :
Reflux Gastritis:
ectomy
Treatment:
Erosive gastritis:
alcohol.
SAID act as anti inflammatory without affection on gastric
barrier
Stress gastritis
8
May lead to stress ulceration that may bleed
Treatment: Prevention; routine use of H2 antagonists, + -mucosal barrier agents
like sucralfate
Peptic Ulcer
Not related to pepsin
Can occur in the:
1. 1stpart of duodenum,
2. lesser curve of stomach
3. stoma of gastrojejunostomy,
4. oesophagus,
5. Meckel’s diverticulum
Aetiology:
ollinger-
Ellison syndrome”
9
Duodenal Ulceration
Incidence
:
rease in its incidence
Pathology
:
Penetrates the mucosa and into the muscle coat
Histopatholgy:
uscular coat
Gastric Ulcers
Incidence
:
ents
11
Aetiology
:
Pathology:
Lesser curve of the stomach
Malignancy in gastric ulcers:
il proved otherwise usually by
well targeted multiple biopsis “as many as10”
Clinical features of peptic ulcers
Pain: epigastric, gnawing, may radiate to back, eating may relieve the discomfort,
intermittent
Periodicity:intermittent, spring and autmen
Vomiting:indicates stenosis
Alteration in weight: wt loss or gain may occur ,,, wt loss more with GU
Bleeding: all may bleed; may be: chronic anaemia acute presentation with
hematemesis and melaena
Clinical examination
c tenderness
Investigation :
11
Treatment of peptic ulceration :
Medical treatment:
except in patients with :
Zollinger-Ellison syndrome
Surgical treatment of uncomplicated DU ulceration :
Operations for duodenal ulcer
1. Truncal vagotomy and drainage
2. Highly selective vagotomy
3. Truncal vagotomy and antrectomy
4. Billroth II gastrectomy
Protocol for GU :
-8 wks later
If un-healed ------Surgery
Operations for gastric ulcer :
1. Billroth I gastrectomy
2. Billroth II gastrectomy
3. Vagotomy, pyloroplasty and ulcer excision
12
Sequelae of peptic ulcer surgery :
Bile vomiting
Post-vagotomy diarrhoea
Complications of peptic ulceration
Perforated peptic ulcer
Epidemiology:
Pathology:
The ulcers that are liable for perforation are:
Clinical features
:
Sudden onset of severe generalised abdominal pain
Board like rigidity
13
Investigations:
Air under the diaphragm in about 50
–70 % of cases
--free peritoneal leak
Treatment:
Laparotomy
Laparoscopy
14
Upper GIT Bleeding
Haematemesis and Melena
Is a common emergency
A mortality of 5%
Bleeding peptic ulcer, gastric erosions, Mallory-Weiss and oesophageal vavices.
Medical treatment is ineffective
Therapeutic endoscopy
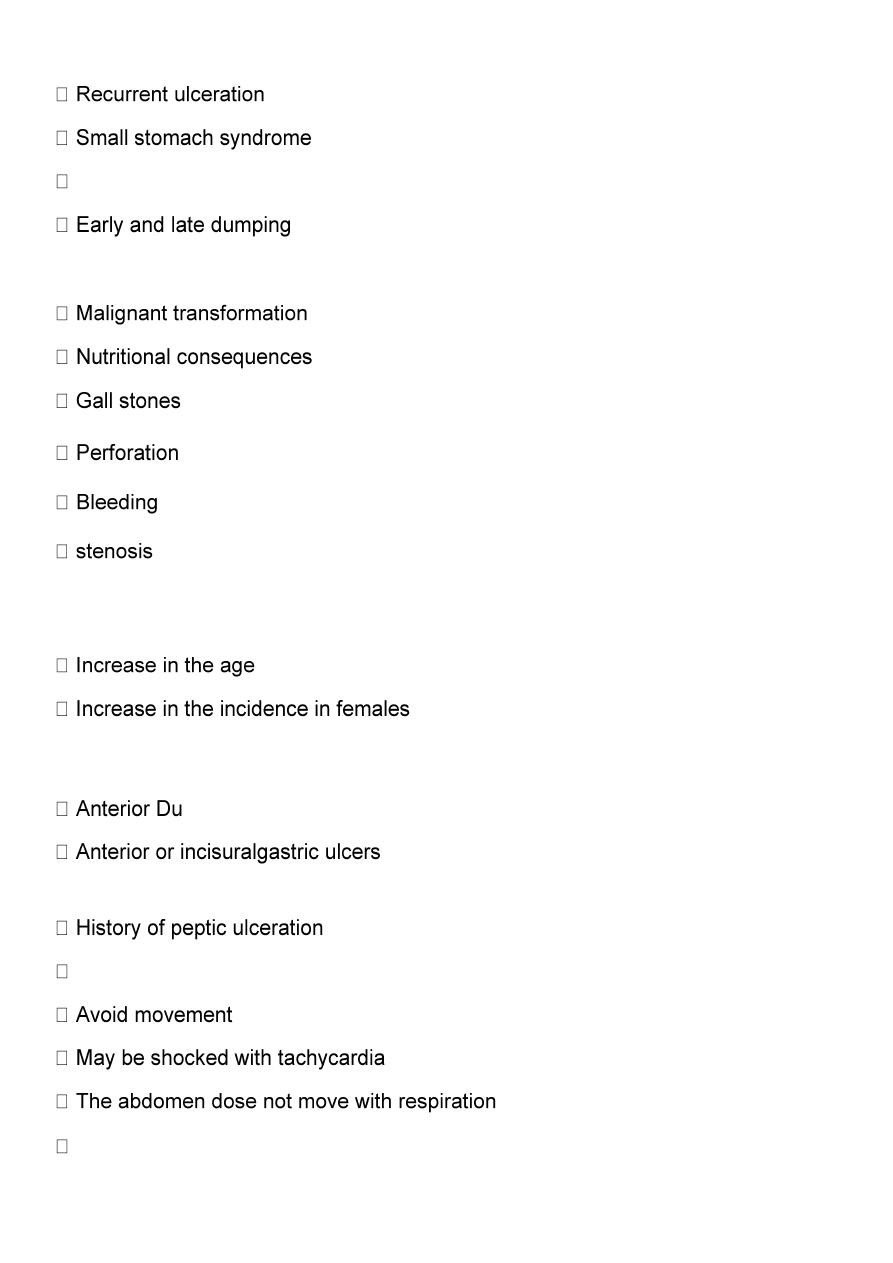
Causes of GIT bleeding
Principles of management:

15
Bleeding peptic ulcers
Epidemiology;
Affect much older persons
Commonly associated with NSAIDs
Diagnosis:
Endoscopy
Goal of treatment:
1. Control of bleeding
2. Prevention of rebleeding
Options to control bleeding
1- Medical treatment
H2 antagonist
Proton pump inhibitors
Tranexamic acid; fibrinolysis inhibitor
2
-
Minimal invasive treatment
;
Therapeutic endoscopy:
Injection, epinephrine
Thermal , electrocoagulation
Laser, APC
3- Surgical treatment
Criteria for surgery:
1. Patients who continue to bleed
2. Significat rebleeding
3. A patient who required >6 units of blood / 24h
4. Elderly patients
Certain endoscopic features;
Visible vessel in the ulcer base
Spurting vessel
Clot cover the ulcer
Its Aim is to stop bleeding By Minimal surgery
Definite acid lowering surgery is not required
Mallory-Weiss tear
Longitudinal tear below the gastro-oesophageal junction
Induced by repetitive and strenuous vomiting
Diagnosis by OGD –difficulty and easily missed
Surgery may be needed to stop the bleeding

16
Dieulafoy
’s disease
Gastric arterial venous malformation
Difficult to diagnose Treatment:
Endoscopic----injection of sclerosant
Surgery—local excision
Tumors
Chronic or acute
Not torrential
Common presentation of gastric smooth muscle tumors
Gastric outlet obstruction
The two most common causes:
Pyloric stenosis
Gastric cancer
Clinical features
In pyloric stenosis
:
Long history of peptic ulcer disease
Unremitting pain
Unpleasent vomiting that lacking bile
Contain foodstaff taken several hours previously
Loss of wt.
On examination
:
Dehydrated, loss of wt.
Distended stomach, succussion splash
Metabolic effects:
Hypochloraemic alkalosis
Initially the urine contain low chloride and high HCO3, then dehydration---Na retention
with excessive K and H ions excretion resulting in paradoxical acid urine
Alkalosis-----decrease in ionized Ca---tetany
Management
Diagnosis
: usually by
Endoscopy
Contrast radiology
Treatment:
Correction of dehydration and metabolic abnormalities by using IV isotonic saline with K
Correction of mechanical problem: Usually needs Surgery:

17
Prior to surgery;
Wide bore NG tube
Gastric antisecretory agents
Surgical treatment:
1. Gastro-enterostomy
2. Vagotomy
Endoscopic treatment by balloon dilatation
Disadvantages:
Applicable for early cases
Repeated courses
Perforation
Gastric polyps
Accidental finding at endoscopy
May be premalignant
Must be biopsied
Types of gastric polyps:
Metaplastic related to H.pylori infection
Inflammatory
Fundic gland polyp; associated with proton pump inhibitors and familial polyposis
Adenoma premalignant
Gastric cancer
Is the major cause of cancer mortality
Poor prognosis
Early detection
The aetiology is multifactorial, but H. pylori is an important factor.
Epidemiology:
The incidence is highest in Japan and some areas of China; >70 per 100000
Men more than female
Incidence increase with age
Increase incidence of tumors affecting the proximal part of stomach
Proximal gastric cancer dose not seem to be associated with H.pylori
Aetiology
:
Multifactorial disease
H.pylori
Risk factors
:
Pernicious anaemia and gastric atrophy
Peptic ulcer surgery
Cigarette smoking

18
Diet, N-nitros compounds, excessive salt intake
Alcohol
Genetic
Clinical features
Early gastric cancer
Advanced gastric cancer
Early gastric cancer:
Non-specfic symptoms; dyspepsia
Liberal use of gastroscopy in patients with dyspepsia (Open access gastroscopy)
Antisecretory agents can improve the symptoms of gastric cancer
Advanced gastric cancer:
Early satiety, bloating, distension and vomiting
Bleeding, mild and chronic
Obstruction,:
proximal---dysphagia
Distal ---------gastric outlet obstruction
Non-metastatic effects:
Thrombophlebitis (Trousseau’s sign)
Deep vein thrombosis
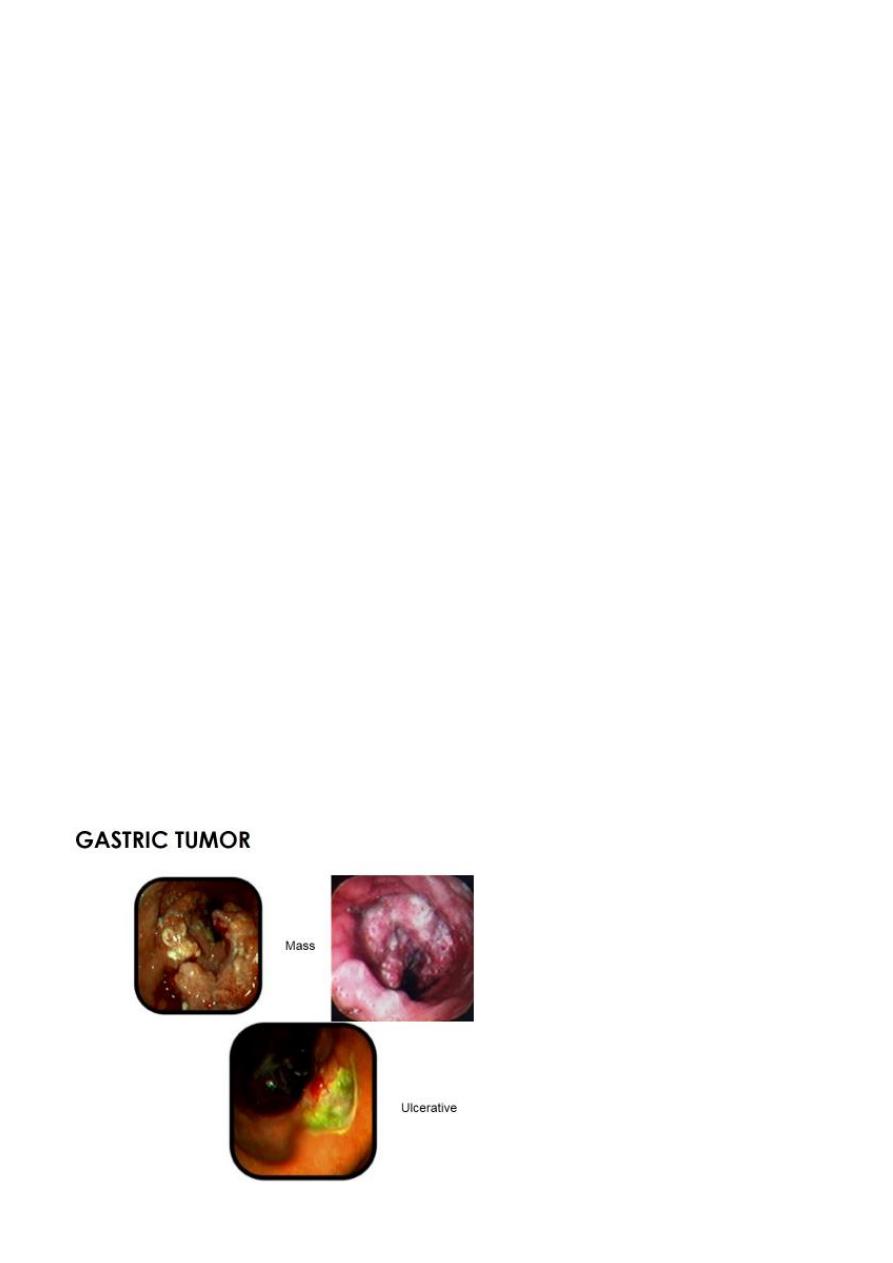
Pathology
Lauren classification: Intestinal gastric cancer
Intestinal metaplasia
Polypoid or ulcer Diffuse gastric cancer
Deep infiltration no obvious mass
Poorer prognosis Mixed
Early gastric cancer (90% five years survival)
Cancer limited to mucosa and submucosa with or with out LN involvement ( T1,any N)
Advanced gastric cancer: ( < 30% five years survival)
Involve the muscularis
Spread of gastric cancer
Direct spread
:
Penetrates the mucsularis, serosa, and ultimately adjacent organs
Lymphatic spread
Both by permeation and emboli
Distant nodal; supraclavicular (Troisier’s sign)
Blood borne metastases:
First to liver and then other organs like lung and bone
Transperitoneal spread:
Involve anywhere in the peritoneal cavity
Ascites

19
Krukenberg’s tumours
Tumour shelf
Sister Joseph’s nodule
Laparoscopy and cytology
Gastric cancer
The prognosis of operable cases of gastric carcinoma depends on whether or not there is
histological evidence of regional LN involvement.
International Union Against Cancer (UICC) staging of gastric cancer
T1 Tumour involves lamina propria
T2 Tumour invades muscularis or subserosa
T3 Tumour involves serosa
T4 Tumour invades adjacent organs
N0 No lymph nodes
N1 Metastasis in 1–6 regional nodes
N2 Metastasis in 7–15 regional nodes
N3 Metastasis in more than 15 regional nodes
M0 No distant metastasis
M1 Distant metastasis (this includes peritoneum and distant lymph nodes)
Staging
IA T1 N0 M0
IB T1 N1 M0
T2 N0 M0
II T1 N2 M0
T2 N1 M0
21
T3 N0 M0
IIIA T2 N2 M0
T3 N1 M0
T4 N0 M0
IIIB T3 N2 M0
IV T4 N1–3 M0
T1–3 N3 M0
Any T Any N M1
Diagnosis
Clinical Signs
Investigations:
For Dx.:-----Endoscopy, with biopsy
For extend and operability “Staging”:
Ultrasound
Endoluminal
Laparoscopic
Conventional
CT scan
For assessment:
21
Treatment
Surgery:
Radical
Palliative
Operability
Radical surgery:
Palliative surgery:
Partial gastrectomy
Gastroenterostomy
Gastric exclusion oesophagojejunostomy
Partial gastrectomy Gastrojejunostomy
Subtotal gastrectomy
Total gastrectomy

22
Postoperative complications of gastrectomy
Leakage; from oesophagojejunostomy
Leakage from duodenal stump
Biliary peritonitis
Secndary haemorrhage
Long term complications
Nutritional deficiencies
Dumping
Diarrhoea
Other treatment modalities
Chemotherapy:
Improvement in the survival of several months
Combination cytotxic chemotherapy
Radiotherapy:
Disappointing except for bony metastases
Other gastric tumours
GASTROINTESTINAL STROMAL TUMOURS(GIST)
Previously Called Gastric Leiomyoma and Leiomyosarcoma
Distniction between them difficult
Associated with a mutation in the tyrosine kinase c-kit oncogene.
Peritoneal and liver metastases
spread to lymph nodes is extremely rare.
Clinical features
Non specific symptoms
Bleeding
23
Difficult to detect by endoscopy
TREATMENT
wedge excision
GASTRECTOMY
lymphadenectomy is not required
imatinib before operation
Gastric Lymphoma:
Primary
Part of generalized lymphoma
Clinical features:
Similar to gastric cancer
Diagnosis is by endoscopic biopsy
Ct scan for staging
Treatment:
Primary lymphoma: surgery + - chemotherapy
Systemic lymphoma chemotherapy
GASTRIC OPERATIONS FOR MORBID OBESITY
Obesity when the BMI of the person is
more than 25
BMI = (Weight in kg)/(Height in m)
2
Normal weight when BMI between 18 –
24.9
Over weight when BMI 25 – 29.9
Obesity when BMI > 30
Morbid obesity when BMI >45
24
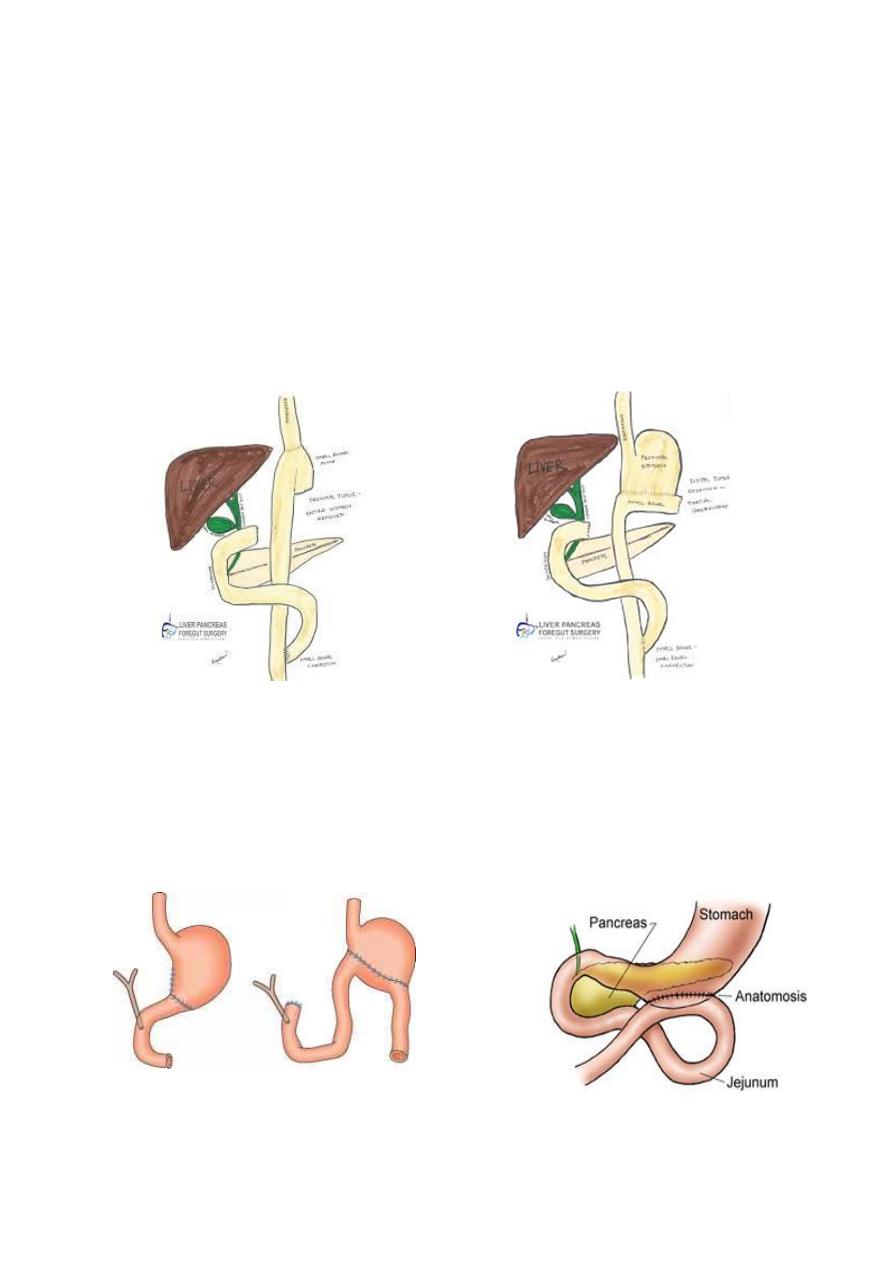
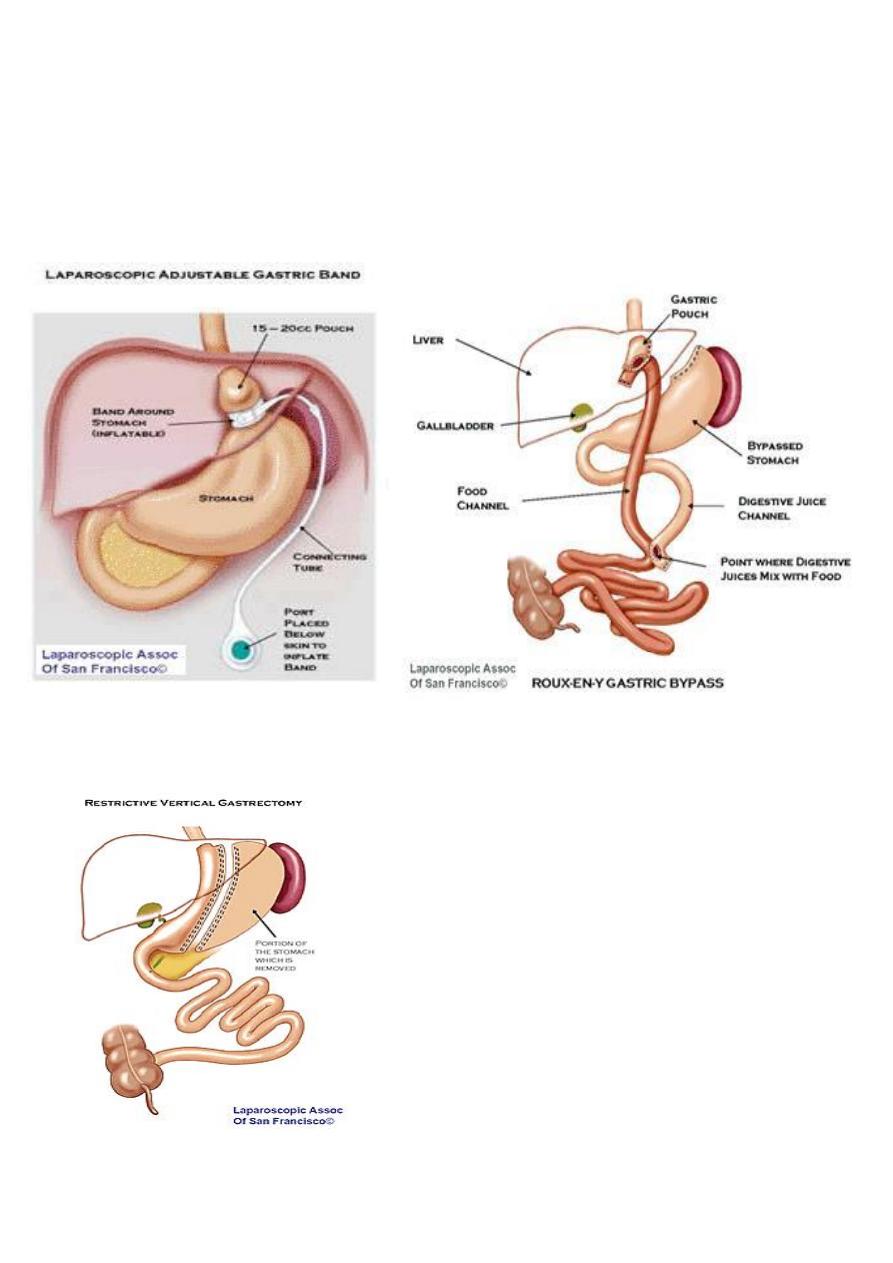
Bariatric Surgical procedures
1. Laparoscopic gastric Band procedure
2. Laparoscopic gastric bypass
3. Laparoscopic sleeve gastrectomy
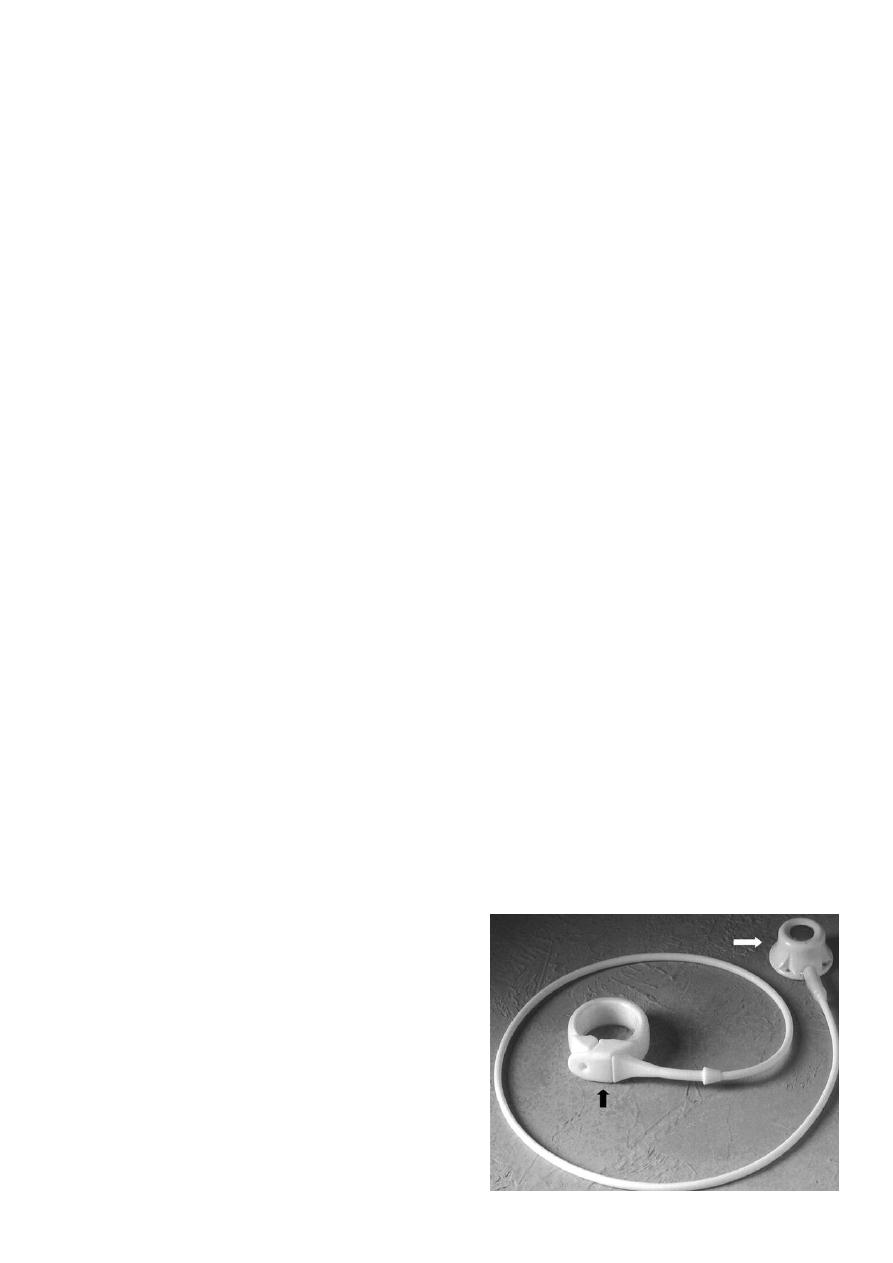
1-Lap Band procedure
2-Gastric bypass
3-Lap sleeve gastrectomy
Intragastric balloon

25
Zollinger- Ellison syndrome
Gastrin producing endocrine tumour
Head of pancreas
Duodenal loop
Effects; persistant peptic ulceration
Treatment:
Total gastrectomy in the past
Proton pump inhibitor
OTHER GASTRIC CONDITIONS
Acute gastric dilatation
Trichobezoar and phytobezoar
Foreign bodies in the stomach
Gastric volvulous
Total gastrectomy
