
1
Forth stage
surgery
Lec-6
د.سمير الصفار
4/10/2015
The Esophagus
Introduction
Anatomy
Physiology
Clinical features
Investigations
Diseases of esophagus
Surgical anatomy
The esophagus is a muscular tube approximately 25 cm long.
The musculature of the upper 5%, including the upper esophageal sphincter,
is striated; the middle 40% has mixed striated and smooth muscle, the distal
55% is entirely smooth muscle.
The parasympathetic nerve supply is mediated by the vagus.
There are an upper and lower esophageal sphincters.
Physiology
The main function of the oesophagus is to transfer food from the mouth to
the stomach.
The initial movement of food from the mouth is voluntary.
The upper esophageal sphincter is normally closed at rest and serves as :
1. A protective mechanism against regurgitation of esophageal contents into
the respiratory passages.
2. Also it serves to stop air entering the esophagus.
The lower esophageal sphincter(LOS) is a physiological sphincter, about 3-4
cm in length and has a pressure of 10-25 mmHg.
The tone of it is influenced by many things including food, gastric distension,
smoking, and GI hormones.
Its main function is to prevent gastric and duodenal contents from refluxing
into the lower esophagus.

2
Clinical features:
Symptoms
Dysphagia:
Is the term used to describe difficulty, but not necessarily pain, on swallowing.
The type of dysphagia is important; it may be dysphagia for solids or fluids,
intermittent or progressive.
Odynophagia
It refers to pain on swallowing.
Regurgitation and reflux
Regurgitation strictly refer to the return of esophageal contents from above
an obstruction in the esophagus.
Reflux is the passive return of gastroduodenal contents to the mouth.
Chest pain
Chest pain similar in character to angina pectoris may arise from an esophageal cause.
Other symptoms of esophageal disorders include; loss of wt, anemia, cachaxia,
change of voice, and cough.
Investigations
A- Radiography
1- Plain X ray; may show opaque foreign bodies.
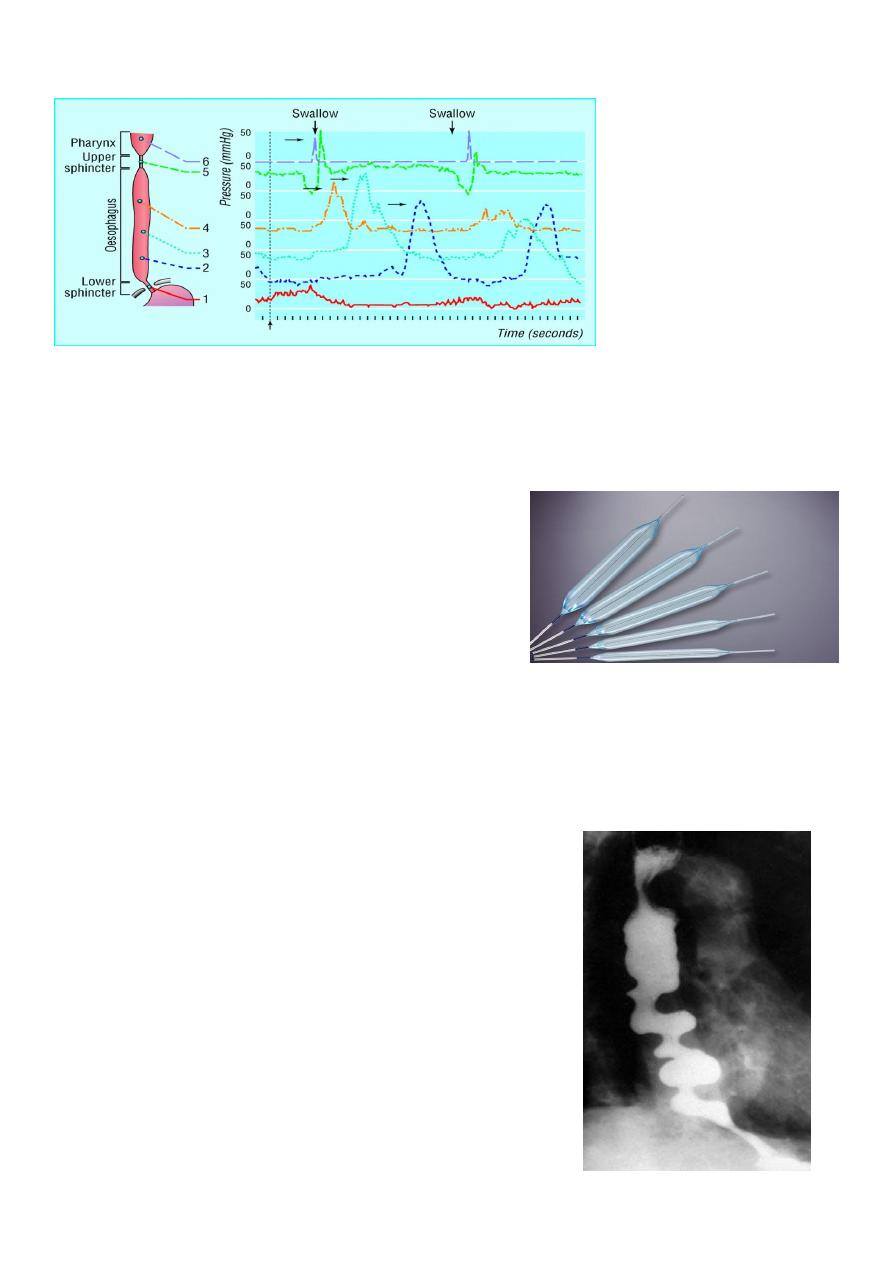
2- Contrast radiography (Barium swallow) is a useful investigation for
demonstrating narrowing, space-occupying lesions, anatomical distortion or
abnormal motility.
B- Endoscopy
Is the investigation of first choice for most oesophagial disorders.
It is either for diagnostic or for therapeutic purposes.
Diagnosis is by visual inspection of the inside of oseophagus and also by
taking a biopsy or cytology specimen.
For therapy, can be used for;
Removal of FB
Dilatation of strictures
Oseophagial varices

3
There are two types;
1- Rigid oesophagoscopy; which is now virtually obsolete.
Disadvantages:
Needs general anesthesia, difficult to introduce, and carry high risk of
perforation
2- Fibre-optic endoscopy
It has virtually supplanted the rigid instrument.
It is done under local anesthesia on an out-patient basis, easy to enter, and
carry low risk of perforation.
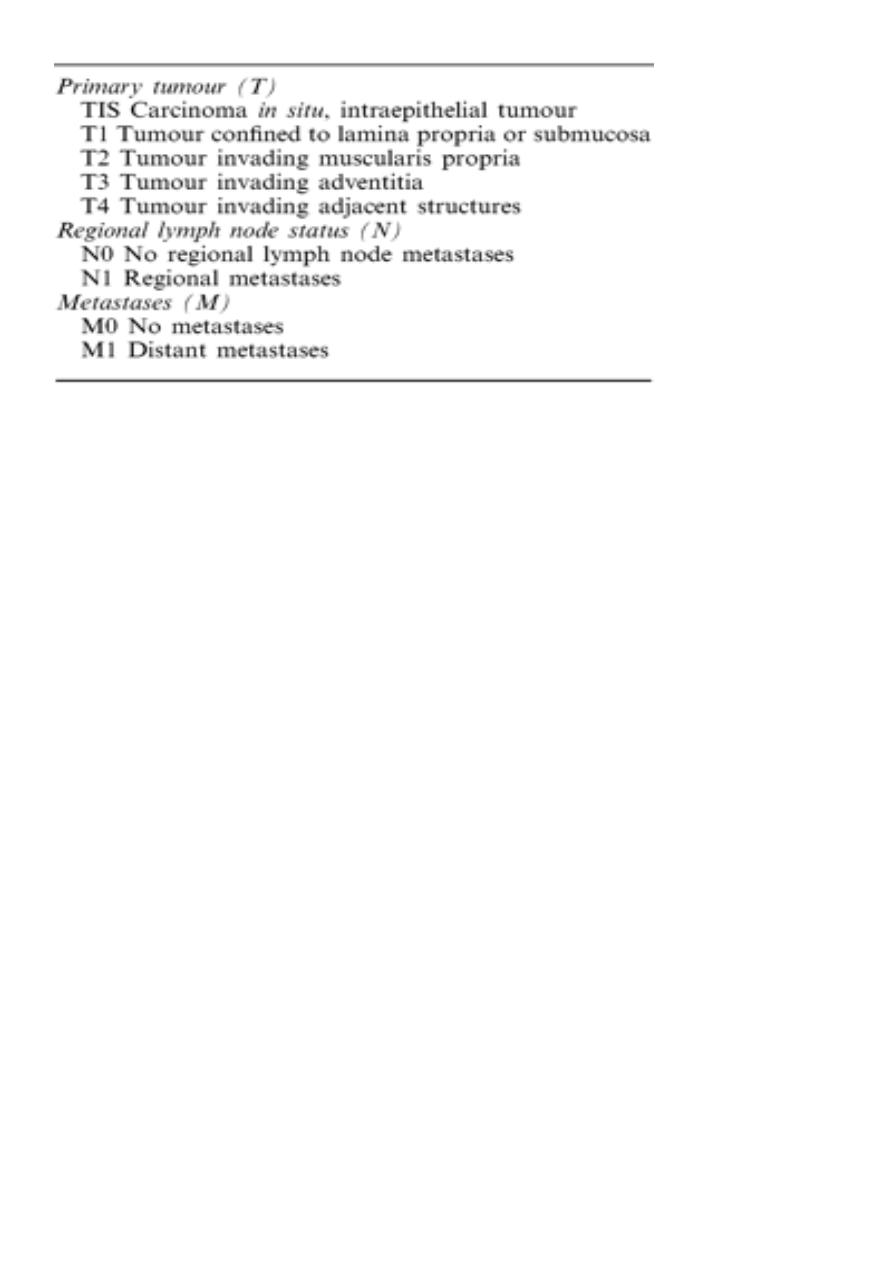
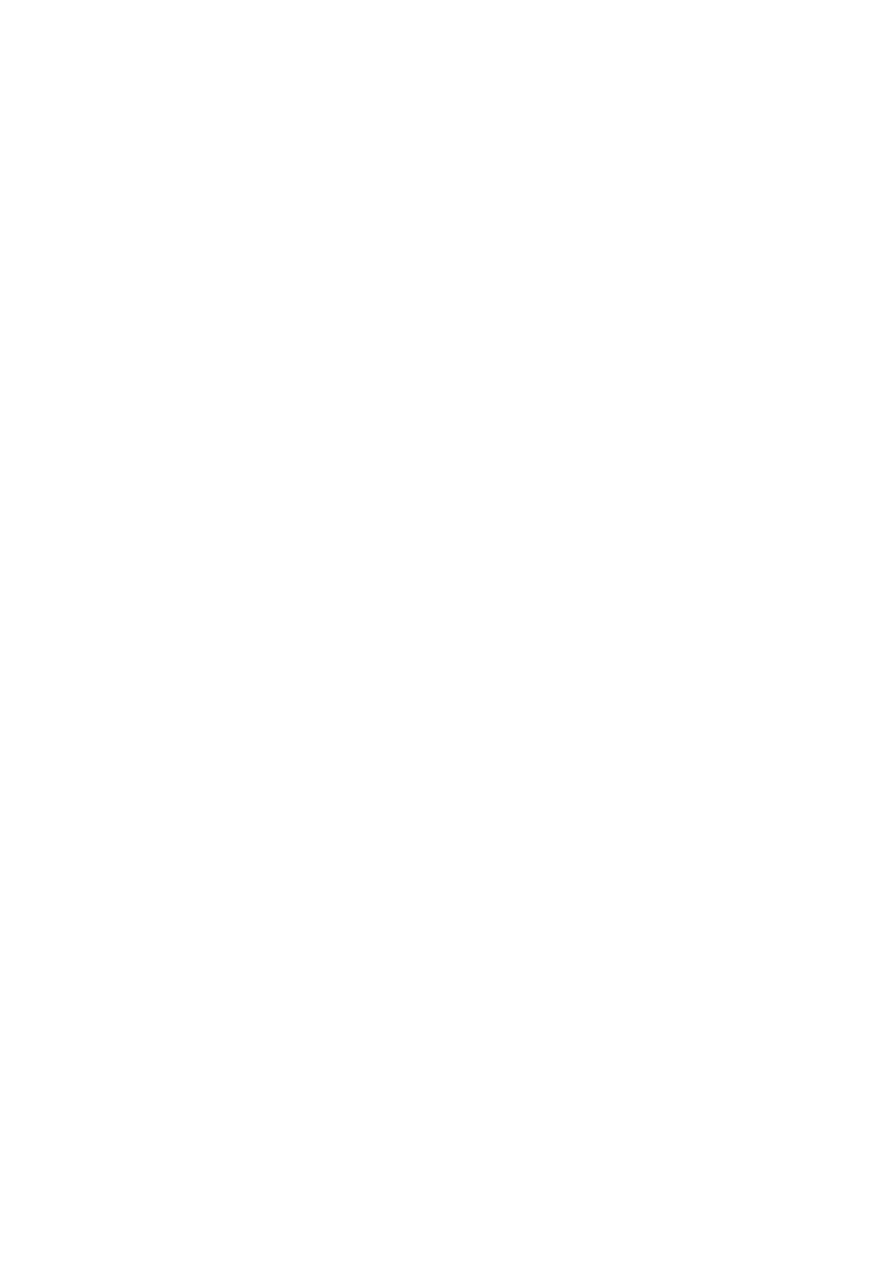
C- Oesophageal manomerty
Is widely used to diagnose esophageal motility disorders.
Recordings are usually made either by;
1- Multilumen catheter 2- Catheters with solid-state transducer
D- 24-hour PH recording
Prolonged measurement of esophageal pH is now accepted as the most accurate
method for the diagnosis of gastro esophageal reflux.
Diseases of the esophagus
Congenital abnormalities
Atresia and tracheo-oesophageal fistula
Oesophageal stenosis
Dysphagia lusoria
Foreign bodies in the oesophagus
A lot of things may become arrested in the oesophagus such as coins, pins,
dentures. The commonest impacted material is food.
Plain radiographs are the most useful examination.
Endoscopy is good tool for the dx specially of non-opaque FB.
Treatment:
Flexible endoscopy is now the method of choice and the majority
of objects
can be extracted with suitable grasping forceps, a snare or a basket.
An impacted food bolus will often break up and pass on if the patient is given
fizzy drinks and confined to fluids for a short time

4
Perforation of the oesophagus
Perforation of the oesophagus is a serious condition that requires prompt diagnosis
and treatment
Causes:
A)
Barotrauma _ Boerhaave’s syndrome
So-called “spontaneous” perforation of the oesophagus is usually due to severe
barotrauma when a person vomits against a closed glottis.
Usually at the lower third
The clinical history is of severe pain in the chest or upper abdomen following a
meal or a bout of drinking.
B) Pathological perforation
Perforation of ulcers, such as a Barrett’s ulcer or tumours.
Penetrating injury
Foreign bodies
Instrumental perforation
Diagnosis
Beware and beware of perforation
Chest pain
Subcutaneous emphysema in the neck
Emphysema around the pericardium can be detected on auscultation as a
mediastinal crunch
Chest XR may show gas in the mediastinum
Contrast swallow using barium suspension
Treatment
Prompt dx and treatment is essential for the best results
There are two options:
Operative
Non-operative

5
Management options in perforation of the oesophagus:
Factors that favour
Nonoperative
Operative
Small septic load
Large septic load
Minimal CV upset
Septic shock
Perforation confined to
Pleura breached
Mediastinum
Endoscopic perforation
Boerhaave syndrome
Perforation of cervical
Perforation of abdominal
Oesophagus
oesophagus
Nonoperative management
Analgesia
Nil by mouth
Antibiotics
General supportive care…IV fluids
When stable…enteral or paenteral nutrition
Nasogastric tube is not recommended
Operative management
It involves thoracotomy and repair of the perforation
This is best done within a few hours of perforation
Corrosive injury
Sodium hydroxide
Sulphuric acid
Drug induced injury
Antibiotic tab
Potassium tab
Gastro-oesophageal reflux disease
Pathophysiology
Competence of the gastro-oesophageal junction is dependent into:
Physiology of LOS;
Basal tone, length, intra-abdominal length
Anatomy of the cardia
Diaphragmatic hiatus-Sliding hiatus hernia

6
Gastro-oesophageal reflux
Physiological reflux After meals
Physiological reflux occurs during transient lower oesophageal sphincter
relaxations (TLOSRs)
Pathological reflux
Gastro-oesophageal reflux disease
Is by far the commonest condition affecting the upper GI tract.
Its incidence increased during the last years;
*Improvement of socioeconomic conditions ↓ H.pylori ↓ DU
Obesity
GORD
Reflux oesophagitis
is a complication of GORD that occur in a minority of sufferers
Clinical features
Retrosternal burning pain( heartburn)
Epigastric pain
These are usually provoked by food, particularly fatty food.
Unpleasant acidic taste
In advanced cases there is a history of pain and reflux when lying flat or on
stooping.
Odynophagia
Less typical symptoms;
Angina-like chest pain
Pulmonary or laryngeal symptoms
Dysphagia

7
Diagnosis of GORD
In the majority of cases the dx is assumed rather than proven and treatment
is empirical
1- Endoscopy;
To exclude: serious pathology
Reflux oesophagitis
Peptic stricture
Barrett’s oesophagus
2- Oesophageal manometery
3- 24-hours oesophageal pH recording
Is the gold standard for the dx of GORD
4-
Barium swallow and meal;
Gives the best appreciation of G-O anatomy but it is not important for the dx of GORD
Differential Dx
Achalasia and GORD are easily confused
Management of uncomplicated GORD
Non-operative management
Medical management
Simple medications; like
Antacids, H2 receptor antagonists
Simple measures; like
Advice about wt. loss, smoking, excessive consumption of alcohol, tea or
coffee, and a modest degree of head up tilt of the bed
Proton pump inhibitors;
Omeprozole, Lansoprazole and pantoprazole are by far the most effective
drug treatment for GORD
Operative managemen
t
Surgery
Indications:
1. In uncomplicated GORD-
2. Failure of medical therapy..PPI
3. Patient choice
Disadvantages of surgery:
Mortality (0.1-0.5%)
Failed operation (5-10%)
3-Side effects; dysphagia, gas bloat(5-10%)
8
What operation
There are many antireflux operations for GORD;
1.
Total fundoplication …Nissen 360
Disadvantage of Nissen:
Over competent cardia….Dysphagia, gas bloat syndrome
2.
Partial fundoplication …Belsy 240
Disadvantage; high recurrence rate….Hill operation
Other antireflux procedures
Angelchik prosthesis
Silastic prosthetic collar
Partial gastrectomy with Roux-en Y reconstruction
What operative approach
Abdominal
Thoracic
Minimal access surgery…Laparoscopic approach
Laparoscopic Fundoplication
Complications of GORD :
1.Reflux oesophagitis : is a complication of GORD that occur in a minority of sufferers .
2. Stricture : reflux induced stricture,,Usually affect middle aged and elderly.
D.Dx from malignant stricture.
Treatment:
a) Dilatation
b) Long-term PPI
c) In younger and fit patients May consider Antireflux surgery.
9
3. Oesophageal shortening : Reflux oesophagitis…longitudenal contraction…secondary
hiatus hernia.
The main problem is during antireflux operation
Collis gastroplasty which produce neo-oesophagus around which a fundoplication can be
done (Collis-Nissen operation)
4. Barrett’s oesophagus : (columnar-lined lower oesophagus)
is a metaplastic change in the lining mucosa of the oesophagus in response to chronic
gastro-oesophageal reflux .
Risk of Barrett’s oesophagus :
- Barrett’s ulcer
- Dysplasia…Carcinoma
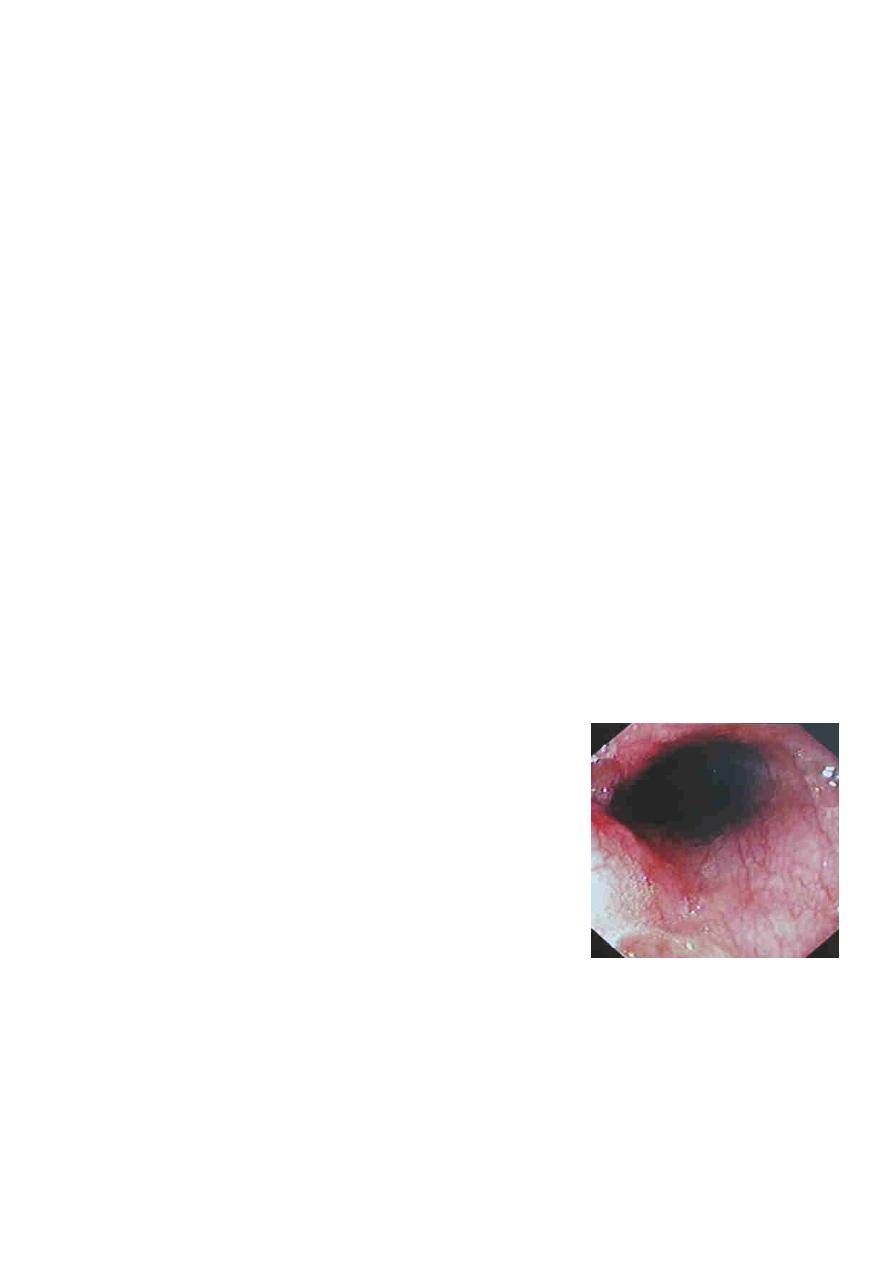
Diagnosis of Barrett’s :
OGD with biopsy
Dull red of the metaplastic columnar epithelium contrasts sharply with the pale glossy
normal squamous lining.
Treatment of Barrett’s oesophagus :
The primary aim is to prevent Barrett's oesophagus from turning into oesophageal cancer.
Of the underlying GORD
Ablation of abnormal mucosa by :
Laser
Photodynamic therapy
Argon beam plasma coagulation
Follow up: yearly OGD
Barrett’s ulcer :
- Is an ulcer in the columnar-lined portion of a Barrett’s oesophagus.
- Barrett’s ulcers may be deep and prone to bleeding or, rarely, perforation.
11
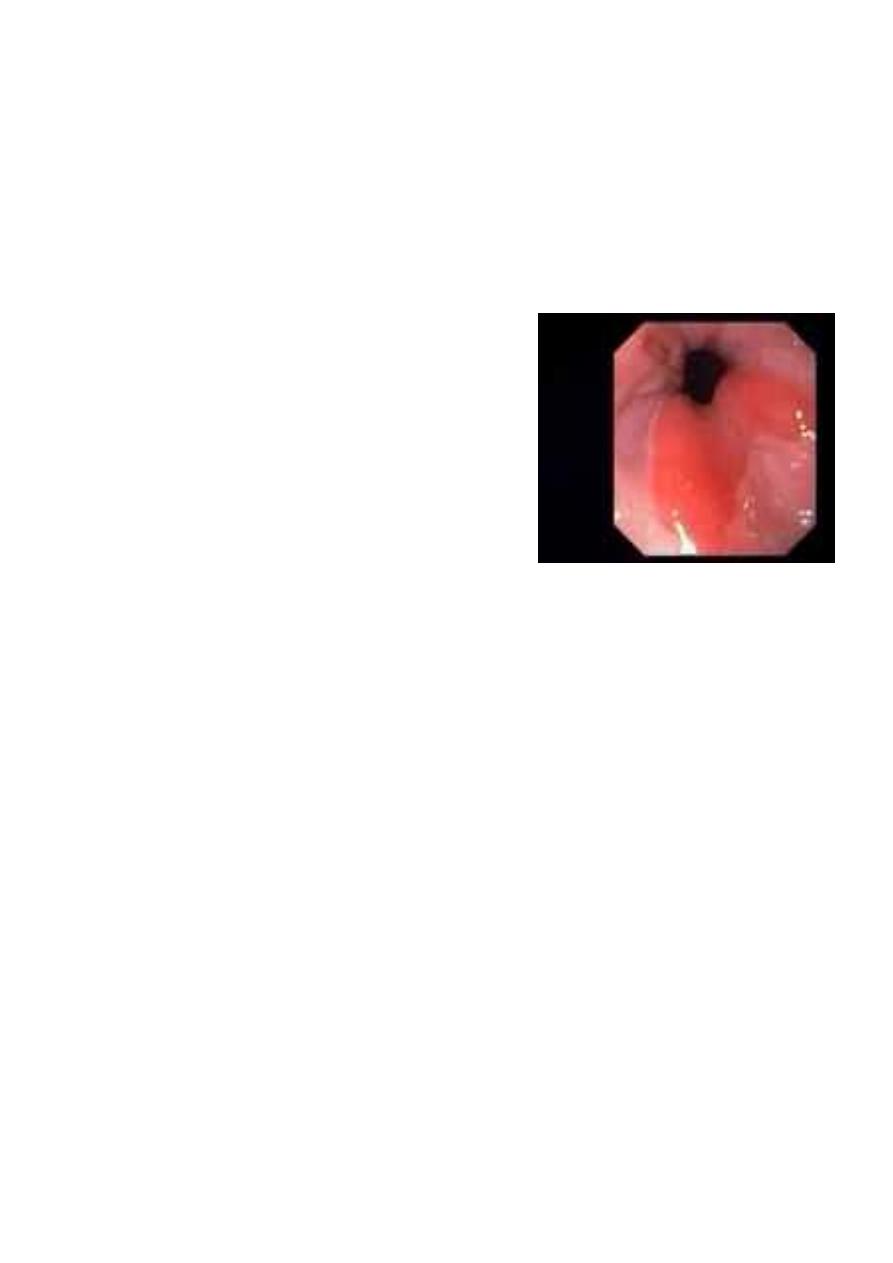
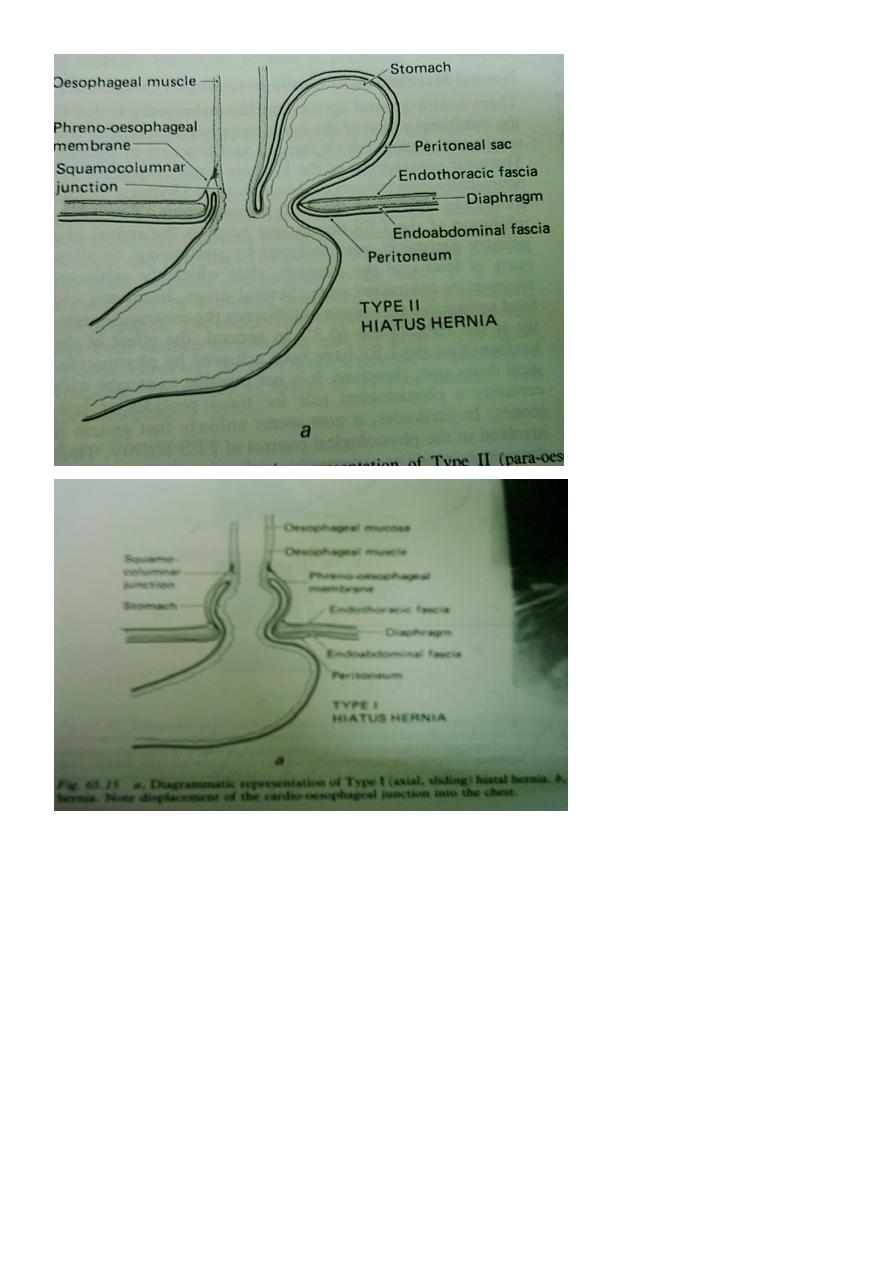
Paraoesophageal (rolling) hiatus hernia :
- Is a true hernia that is prone to complications
- True(pure) paraoesophageal hernia
- Mixed paraoesophageal hernia
- Sometimes the whole of the stomach lies in the chest and may undergo volvulus with
perforation or gangrene.
Clinical features:
- Commonly occurs in the elderly, but it also may occur in young fit people
symptoms :
- Dysphagia
- Chest pain
- Symptoms of GORD
Investigations :
- Plain X-ray of the chest
- Barium meal
- Endoscopy
Treatment :
- Rolling hernias always require surgical repair as they are potentially dangerous.
- The principle of surgery is :
Reduction of the hernia
Gastropexy
- Some surgeons may perform a fundoplication
Neoplasms of the oesophagus :
- Benign tumours
- Malignant tumors :
Primary
Secondary
Benign tumours :
- are rare
- Leiomyoma is the commonest
- Oesophageal polyps
11
Squamus cell polyp
Malignant tumours :
1. Sarcoma are rare
- Leiomyosarcoma
- Rhabdomyosarcoma
2. Malignant melanoma
-Is rare
- May be secondary
- Poor prognosis
3. Carcinoma of the oesophagus
- Is the sixth most common cancer in the world.
- A disease of mid to late adulthood
- Carry a poor prognosis, 5-year survival is only 5-10%
Pathology :
Histologic types:
Squamous cell carcinoma (95%)
- World-wide is the commonest tumour
- Affect the upper 2/3rd
Adenocarcinoma (4%)
- 70% from
- Is the commonest in westernised countries accounts for 60-75% of all
oesophageal cancers.
- Affect the lower 1/3rd
Radiological types:
polypoid/fungating form (most common)
- sessile/pedunculated tumor with lobulated surface
12
-"applecore" lesion
ulcerating form
infiltrating form
-gradual narrowing with smooth transition (DDx: benign stricture)
varicoid form: superficial spreading carcinoma
-thickened nodular tortuous longitudinal folds (DDx:
The poor prognosis of oesophageal cancer is proof of its ability to spread
This may be locoregional or systemic
Aetiology
:
Epidemiology
-South africa
-Northren Iran and china
The cause in endemic areas
-Fungal contamination of food….carcinogenic mycotoxin - -- -
Nutritional deficiences
In non-endemic areas
-Tobacco and alcohol are the major factors in the occurrence of squamous
cancer.
High risk factors for oesophageal carcinoma :
1. Alcohol and smoking
2. Long history of dyspepsia
3. Barrett’s oesophagus
4. Achalasia cardia
5. Stricture “ Corrosive,radiation”
6. Scleroderma
7. Plummer-Vinson syndrome
8. Hyperkeratosis(tylosis)
Clinical features :
1. Patients with early disease may present with rather nonspecific dyspeptic
symptoms or a vague feeling of “something that is not quite right” during
swallowing.
2. Features of advanced disease
3. Dysphagia, is the usual presenting feature

13
4. Loss of weight
5. Hoarsenece of voice
6. Haematemesis or melaena
7. Palpable cervical lymphadenopathy
Diagnosis :
Endoscopy; is the most important diagnostic tool and its widespread use is the major
contributor to early diagnosis;
when the disease at a relatively early stage
when the chances of cure are greater.
It should be emphasised that biopsies should be taken of all lesions no matter how
trivial they appear.
Contrast radiology “Barium swallow” :
The tumour appears as a filling defect in the lumen of oesophagus.
Not helpful for the diagnosis of early disease.
Gives a good assessment of the length of the lesions.
Staging
:
Once a diagnosis of oesophageal carcinoma is made, staging of the disease is
necessary to establish the appropriate method of treatment.
A careful search for metastatic disease
- Chest X-ray
- Ultrasonography
- CT scan of chest and abdomen
- MRI
- Endoscopic ultrasonography
- Bronchoscopy
- Laparoscopy
Staging system:
- TNM classification system
- T for tumour extent
- N for lymph nodes assessment
- M for distant metastases
14
General assessment:
- Assessment for fitness
- Nutritional assessment
Treatment of oesophageal cancers :
- The treatment depends on:
the staging of the disease
the general condition of the patient.
The treatment options available are:
Surgerical excision
Radiotherapy
Chemotherapy
Intubation
Laser coagulation
Combined modality treatment
The treatment is either Radical or Palliative :
A) Radical treatment:
-Indicated for potentially curable disease in fit patients
-Curative treatment involves;
15
Radical surgery
Radical radiotherapy
Radical Surgical Resection:
Is the treatment of choice for tumours of the lower two-thirds of the oesophagus provided:
1. The patient is fit for major surgery
2. Preoperative staging tests indicate that the tumour is resectable and there is no
metastatic disease.
The principle of surgical treatment:
-Resection of the tumour with safety margins.
-Restoration of the continuty, usually gastro-oesophageal anastomosis.
Radical Radiotherapy:
Radiotherapy may be a useful alternative to surgery especially in unfit patients.
- 5year survival 9-19%(average10%) while following surgical treatment 20-35% (20%)
Chemotherapy:
- Improved after the introduction of newer drugs like cis-platinum.
- Chemotherapy never cures the disease
- Best results are seen in SCC
Multimodality treatment:
- Adjuvant radiotherapy either pre- or post- operative
- Radiochemotherapy
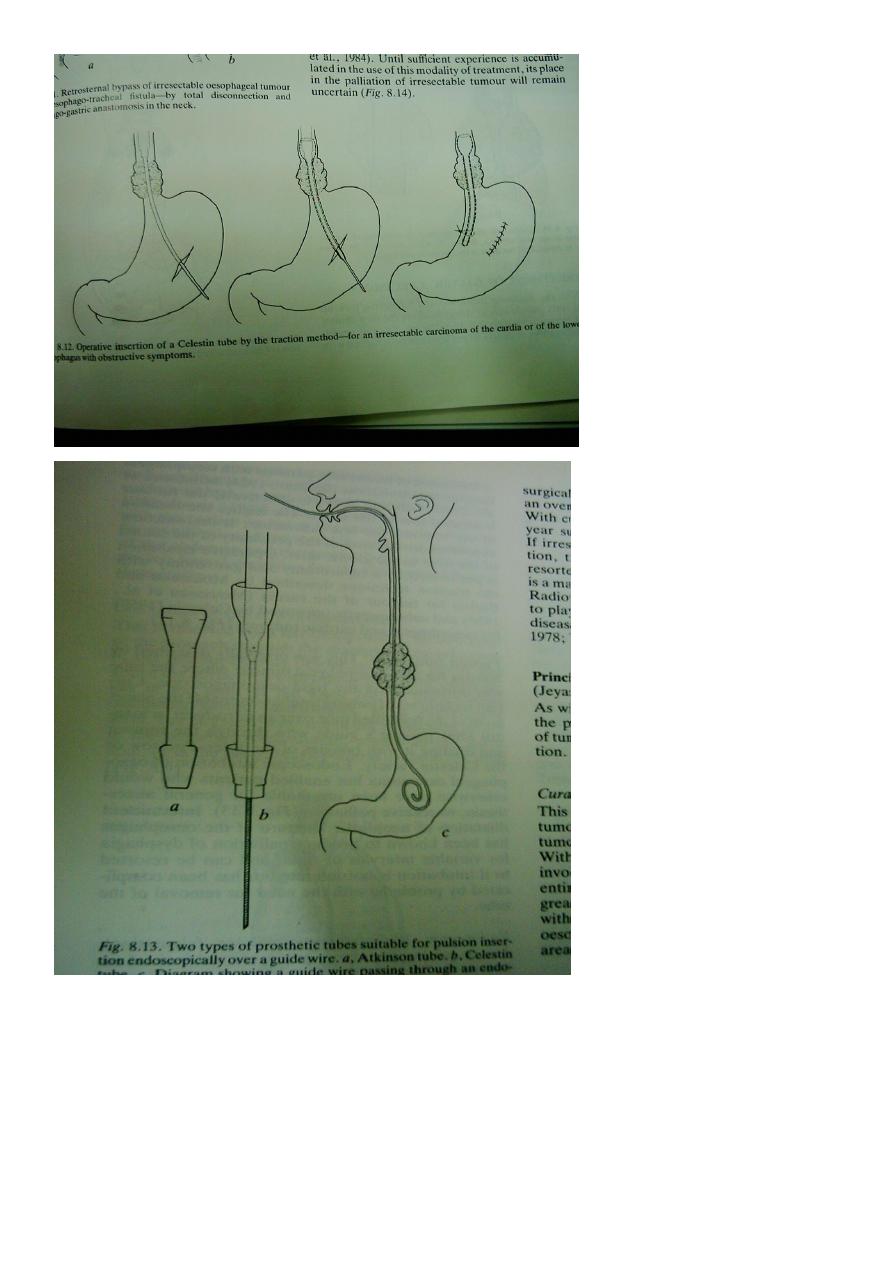
B) Palliative Treatment:
Simple procedures that will produce worthwhile relief of dysphagia with minimal
disturbance to the patient
1. Intubation:
-Traction tubes ( Celestin )
-Pulsion tubes ( Atkinson tube ,, Metal slent )
2. Endoscopic Laser:
-Used to core a channel through the tumour
3. Brachytherapy : intraluminal radiation

16
Carcinoma of the oesophagus :
- Squamous cell usually affects the upper two-thirds
- adenocarcinoma usually affects the lower third
- Common aetiological factors are tobacco and alcohol
(squamous cell) and GORD (adenocarcinoma)
- The incidence of adenocarcinoma is increasing
- Lymph node involvement is a bad prognostic factor
- Dysphagia is the most common presenting symptom, but
is a late feature
- Accurate pretreatment staging is essential in patients
- thought to be fit to undergo ’curative’ treatment
Oesophageal Motility disorders :
1. Achalasia
Pathology: Loss of the inhibitory ganglion cells in Auerbach’s plexus.
Aetiology
:
- Unknown
- Neurotropic viruses, Varicella zoster
- Trypanosoma Cruzi cause Chagas disease
- Incomplete or absent relaxation of the lower oesophageal sphincter and absent peristalsis
in the body of oesophagus.
- It results in :
1. Retension of food in oesophagus
2. Dilatation….Megaoesophagus
Clinical features :
- Is commonest in middle life
- Typically presents with dysphagia
- Long standing cases…overspill into the trachea at night Retrosternal discomfort
Diagnosis :
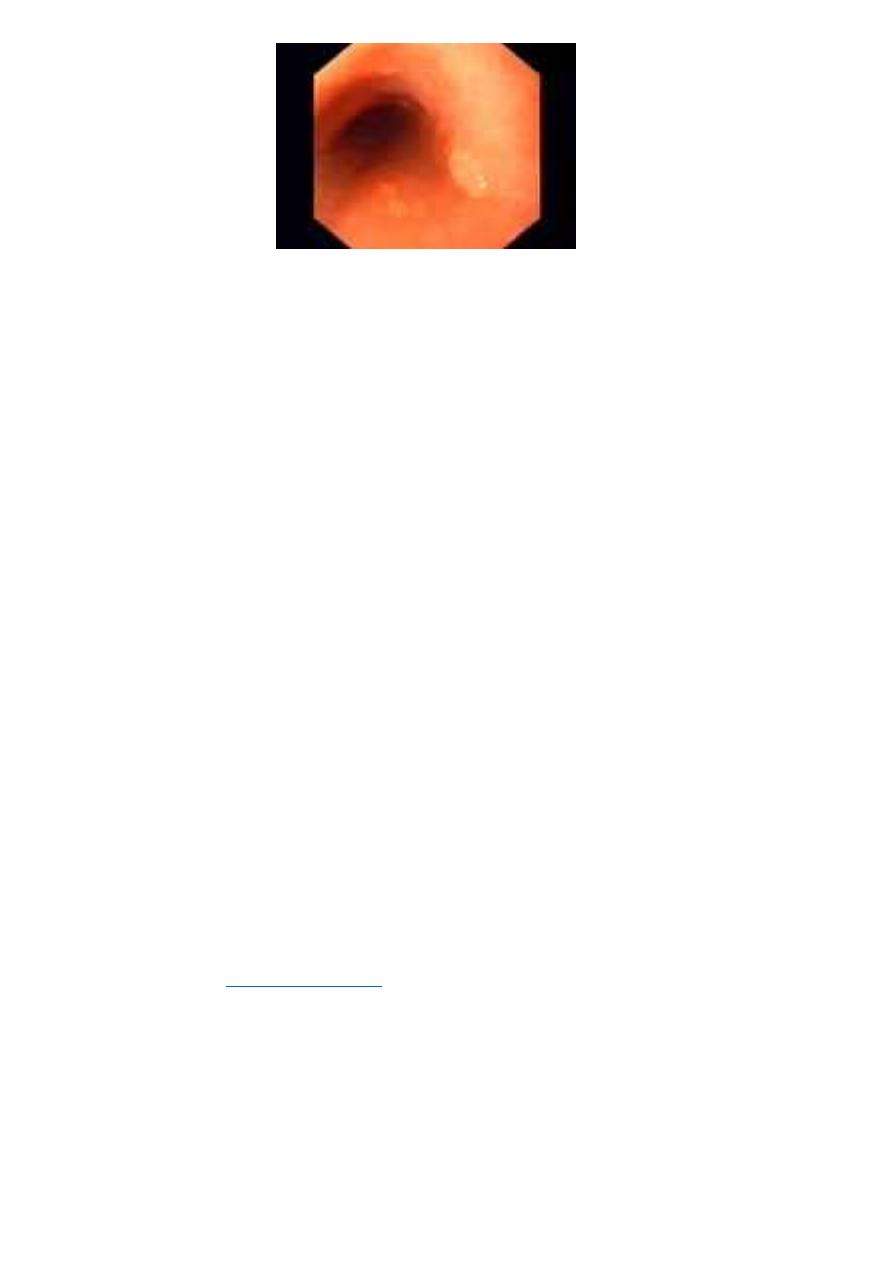
1. Endoscopy
2. Contrast radiology:
- Dilated oesophagus
- Tapering stricture…bird’s beak
- Absent gas bubble
17
3. Oesophagial Manometry
Treatment :
1. Forceful dilatation
Disadvantages:
-Perforation
-Reflex
-Repeated sessions
2. Heller’s cardiomyotomy
a. Open Laparotomy
b. Laparoscopic
3. Botulinum toxin
4. Drugs : Calcium channel antagonists
Other oesophageal motility disorders :
- Cricopharyngeal achalasia
- Diffuse oesophageal spasm
- Nutcracker oesophagus
- Eosinophilic oesophagitis
Oesophageal diverticula :
- Pulsion diverticula
- Traction diverticula
18
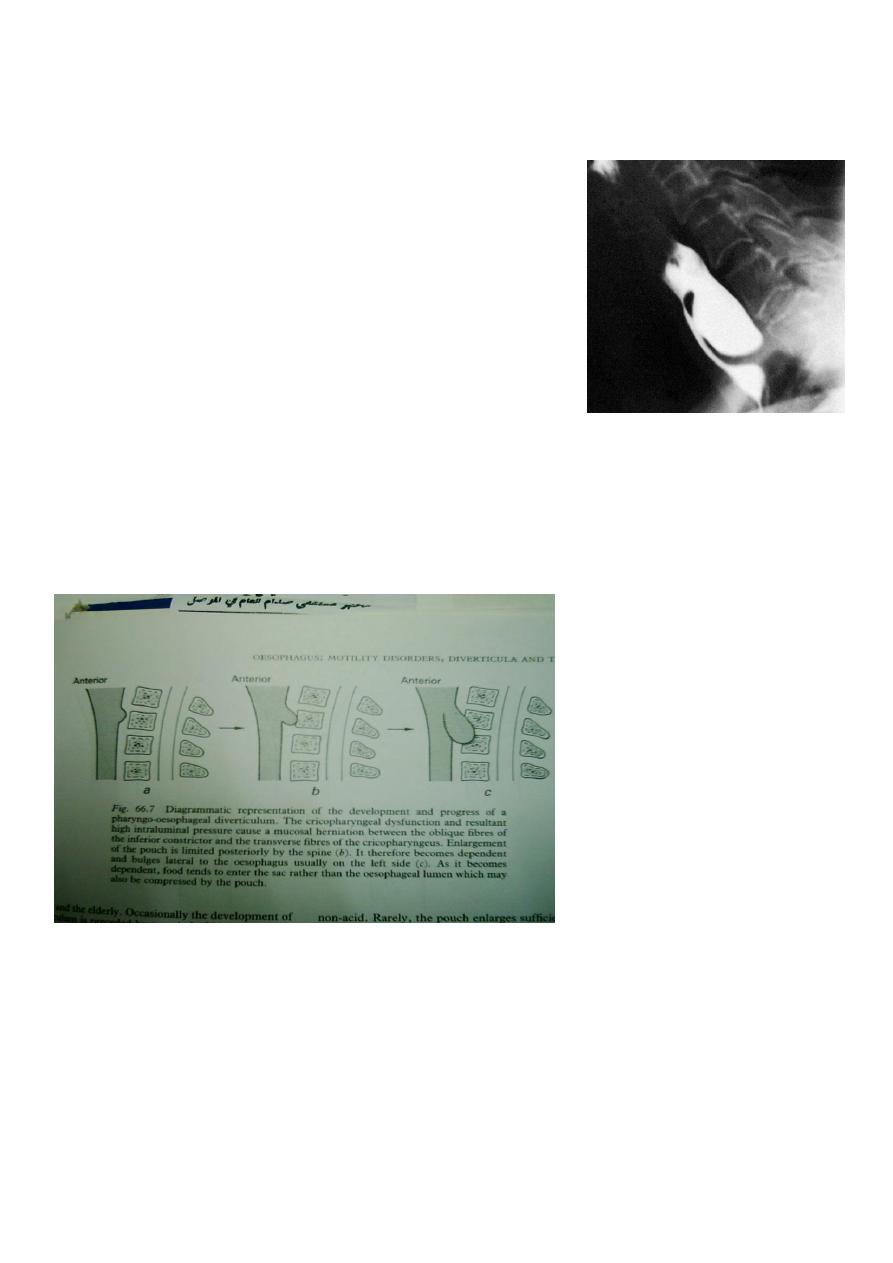
Zenker’s diverticulum (Pharyngeal pouch)
it protrudes posteriorly above the cricopharyngeal sphincter through the natural weak
point (the dehiscence of Killian) between the oblique and horizontal (cricopharyngeus)
fibres of the inferior pharyngeal constrictor
Symptoms:
- Pharyngeal dysphagia
- Halitosis
- Oesophagial Dysphagia
Diagnosis:
- Endoscopy
- Barium swallow
Treatment:
- Endoscopic: stapler creating diverticulo-oesophagostomy
- Open surgery:
Pouch excision
Pouch suspension
Myotomy
19
21
