1
Forth stage
Surgery
Lec-3
Dr.Samer
16/12/2015
Spleen
Embryology
mesodermal condesation in the dorsal mesogastrium
Anatomy
It weighs 75 – 250 g
It lies in the left hypochondrium
Along the line of tenth rib
Its hilum lies in the angle between the stomach and kidney, and is in contact with the tail
of pancreas
There is a notch in its inferolateral border.
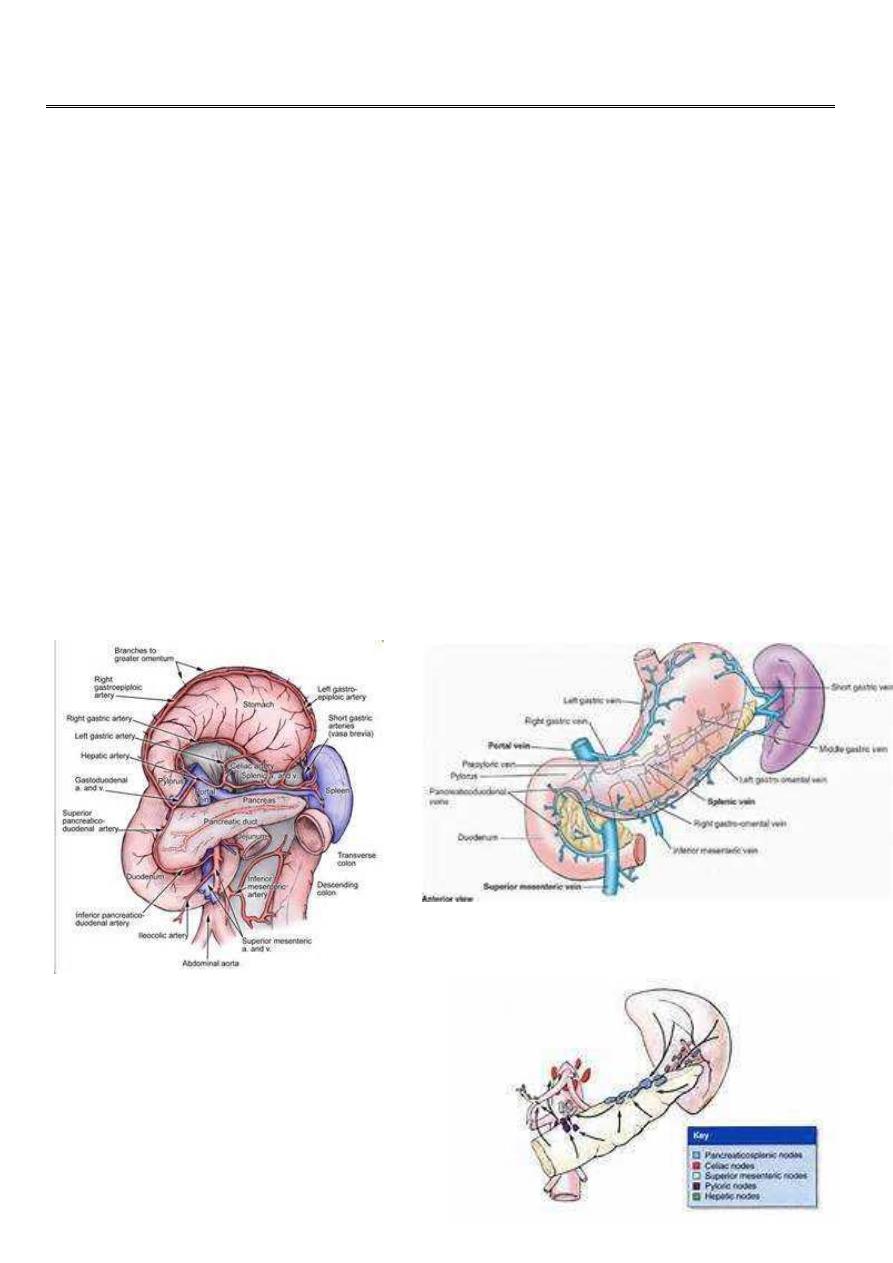
Blood supply
Lymphatic dranage
2
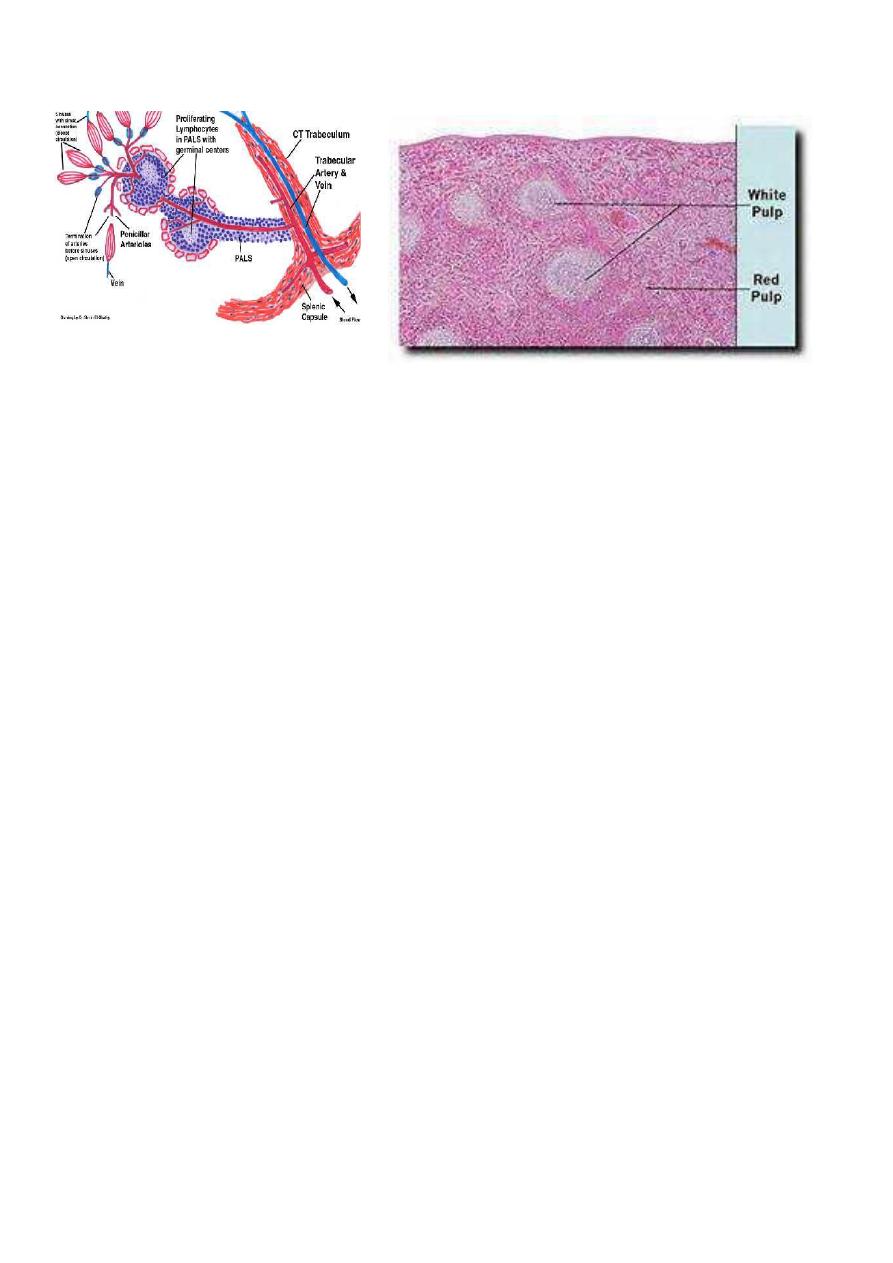
histology
Function of spleen
Immune function
Major site of IgM production
Opsonins, tuftsin, and properdin
Filter function
Macrophages in the reticulum capture cellular and non-cellular material from the
blood and plasma.
Effeet platelets & RBCs
Bacteria, pneumococci
Pitting
Removal of particulate particles from RBCs, like the Howell-Jolly & Heinz bodies.
Reservoir function
It is less marked but dose the spleen Contain approximately 8% of the red cell mass.
Cytopoiesis
Haemopoiesis during fetal life.
Proliferation of T & B cells and macrophages following antigenic stimulation.
Investigation of spleen
Imaging:
Plain radiology:
Rarely used, but incidental finding of calcification of the splenic artery __splenic
artery aneurysm
calcification of spleen__an old infarct, a benign cyst or Hydatid cyst.
multiple calcifications__tuberculosis
Ultrasonography;
Determine the size & consistency
SOL, cystic or solid
3
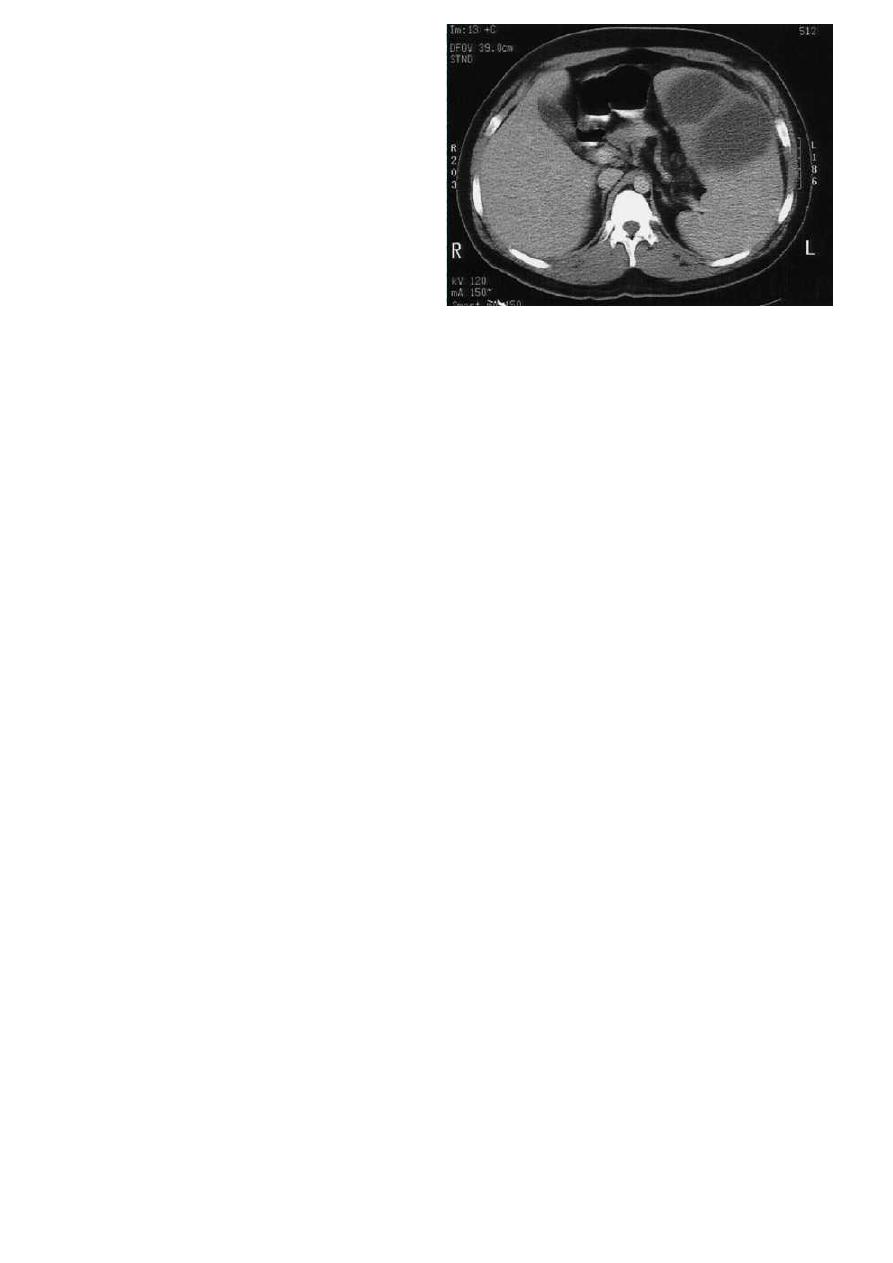
CT scan;
Better in determing the nature of suspected splenic pathology.
MRI
scan similar value to CT scan
Radioisotope:
Less commonly requested
Technetium99mm-labelled colloid is restricted to determine whether the spleen is a
significant site of destruction of RBCs.
Disease of spleen
Congenital abnormalities of the spleen:
Splenic agenesis
is rare but present in 10% of children with congenital heart
disease.
Polysplenia
is a rare condition resulting from failure of splenic fusion.
Splenunculi:
Are single or multiple accessory spleens that are found in approximately 10-30% of
the population.
Located near the hilum in 50%,
Related to the splenic vessels or behind the tail of pancreas in 30%.
Remainders are located in the mesocolon or the splenic ligaments.
Hamartomas:
Are rarely found in life
Non-parasitic cysts:
Are rare True cysts form embryonal rests.
Splenic rupture
Aetiology:
Blunt abdominal trauma, splenic injury should be suspected in any case of blunt abdominal
trauma,
Particularly when the injury occurs to the left upper quadrant of the abdomen.

4
And specially if there are fractures of the overlying ribs ( 9th ,10th ,11th).
Penetrating abdominal trauma:
Stab and missile injury
Iatrogenic:
Splenic injury is a frequent complication of any surgical procedure, particularly those in the
left upper quadrant.’
Presentation:
may present in three ways
The patient succumbs rapidly
Initial shock, recovery, signs of late bleeding
The delayed case
Clinical signs of ruptured spleen:
General signs of internal hge
Left upper quadrants guarding and tenderness.
Kehr’s sign
Shifting dullness
Fullnes in the pelvis
Diagnosis:
Abdominal ultrasonography (FAST)
CT scan
Management:
Conservative: applied in blunt trauma
Only in Haemodynamically stable patients
Minimal or no abdominal findings
CT scan *isolated injury. * absence of hilar involvement or massive disruption of
spleen
Immediate laparotomy:
Obvious evidence of continuous blood loss despite adequate resuscitation.
Strong suspicion of trauma to other organs
Splenic preservation should be considered wherever possible.
Persons with splenomegaly like in malaria are more liable to splenic rupture after
trivial trauma.
Trend for early splenectomy Delayed Rupture of the Spleen
May arise from:
Infected splenic embolus
In association with typhoid and paratyphoid fever, osteomyelitis, otitis media, and
purperal sepsis.
Pancreatic necrosis
In association with intraabdominal infection.
Complications:
Rupture:
Subphrenic abscess
5
Peritonitis
Splenic abcess
Diagnosis:
Ultrasound
CT scan
Treatment
:
Underlying cause
drainage
Tuberculosis of spleen
Considered in young patients with:
Splenomegaly, asthenia, loss of weight, and fever.
Complications:
Cold abscess
Portal hypertension
Treatment
:
Anti-TB drugs
Splenectomy
Tropical splenomegaly
Splenic enlargement, frequently massive, found in the tropics attributed to; malaria,
schistosomiasis, and kalaazar. Occasiosionally attributed to malnutrition.
Removal of spleen is frequently required.
Schistsoiasis
Prevalent in Africa, Asia, and South America.
S.mansoni 75%,S.haematobium 25%
Pathogenesis: enlargement of spleen arise either as a result of ;
Hepatic fibrosis portal hypertension
Or splenic enlargement may result from hyperplasia induced by phagocytosis.
Diagnosis:
Exam. of urine & faeces for ova
Abnormal liver function test
Hypochromic anaemia
Treatment:
Medical not helpful for regression of splenic enlargement
Usually removal of spleen is needed.
6
Idiopathic thrombocytopenic purpura
Pathogenesis:
ABs .That damage the patient’s own platelets
It is of two types
Acute in childhood
Chronic in adults
Acute in childhood usually follows an acute infection and has a spontaneous resolution
within 2 months.
Chronic in adults seen in associated with other conditions, including systemic lupus
erythematosus, chronic lymphatic leukaemia and Hodgkin’s disease.
Clinical features
:
Adult type Affects female 15-50 years
Purpuric patches in the skin and mucous membrane spontanous or after trivial
trauma.
Hemorrahage from the urinary tract and GIT and haemoarthrosis are rare.
Intracranial hge is uncommon but it is the most common cause of death.
Signs:
o Ecchymosis
o Tourniquet test
o Palpable spleen in less than 10%
Investigations:
Prolonged bleeding time
Clotting and prothrombin time normal
Reduced platelets count
( usually (usually < 60*10^9/litre)
Bone marrow aspiration ;plentiful platelet -
producing megakaryocytes.
Treatment:
Medical ;steroids ,good prognosis in pediatrics with 75 %
incidence of spontaneous
regression
Splenectomy:

7
Is indicated when;
The patient develops two relapses on steroid therapy.
Low platelets in spite of steroid therapy.
When ITP persisted for
< than 6-9months.
Splenectomy: will lead to;
cure in up to two-thirds of patients,
15 %
of patients show improvement
The remainder show no benefit.
Preoperative:
Fresh blood transfusion
Platelet concentrate.
Splenectomy:
Indications:
Urgent
Splenic injury ,accidental or iatrogenic
Ellective
1
-
Oncological
:
Part of en bloc resection
Diagnostic
Therapeutic
2
-
Haematological
ITP
Haemolytic anaemias
1 -Hereditary spherocytosis
2 -Acquired autimmune haemolyic anaemia.
3
- Thalassaemia
4 -
Sickle cell anaemia
Hypersplenism
8
3-Portal
hypertension
Variceal surgery.
Preoperative preparation:
I -
Normalization of coagulation profile:
In the presence of bleeding tendency;
Transfusion of blood
Fresh-frozen plasma
Cryoprecipitate
Platelets
III-
Vaccination; against
Pneumococcus (those over 2 years)
H. influenzae ( for all ages )
Meningococcus ( recommended in high risk areas )
Influenza virus.
Note: in trauma victim, vaccination can be given in the postoperative period.
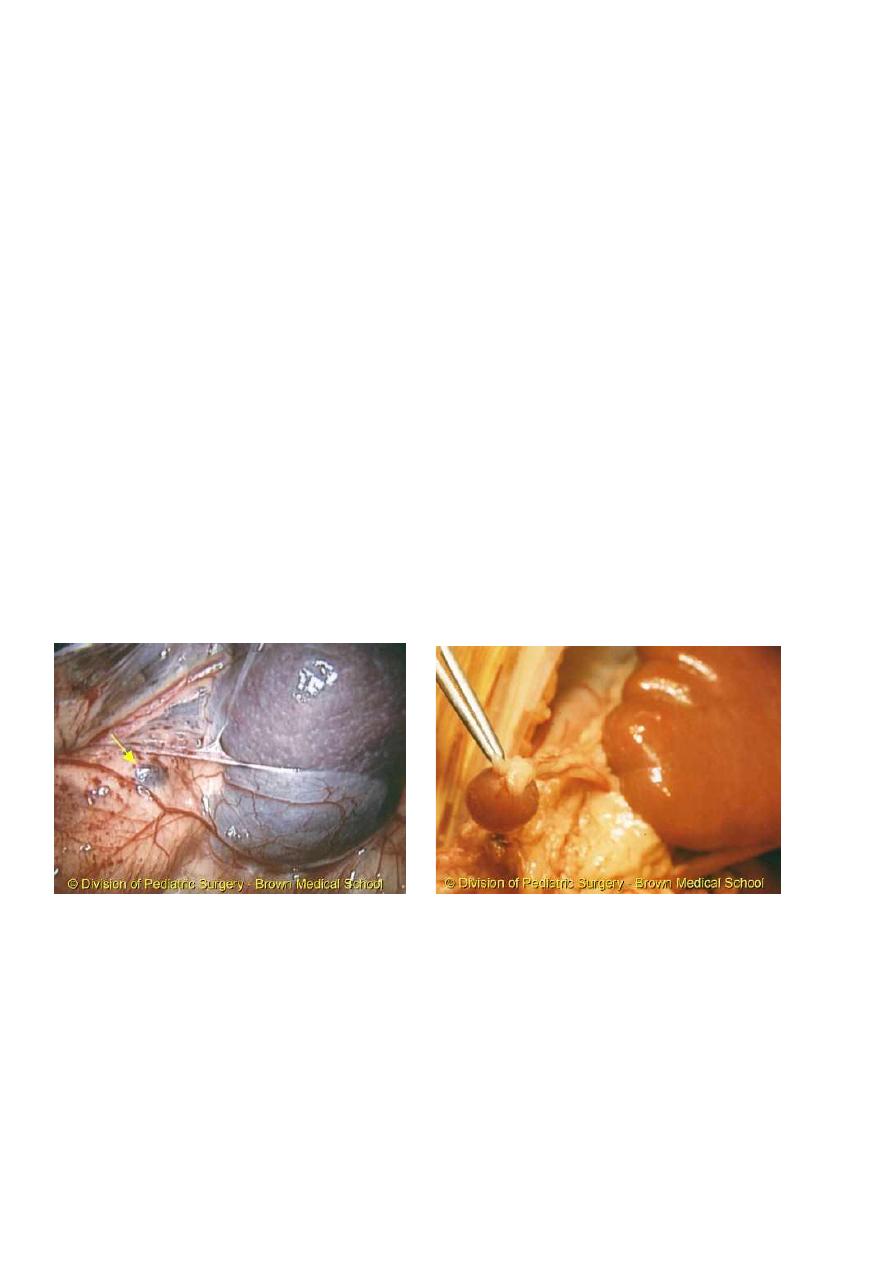
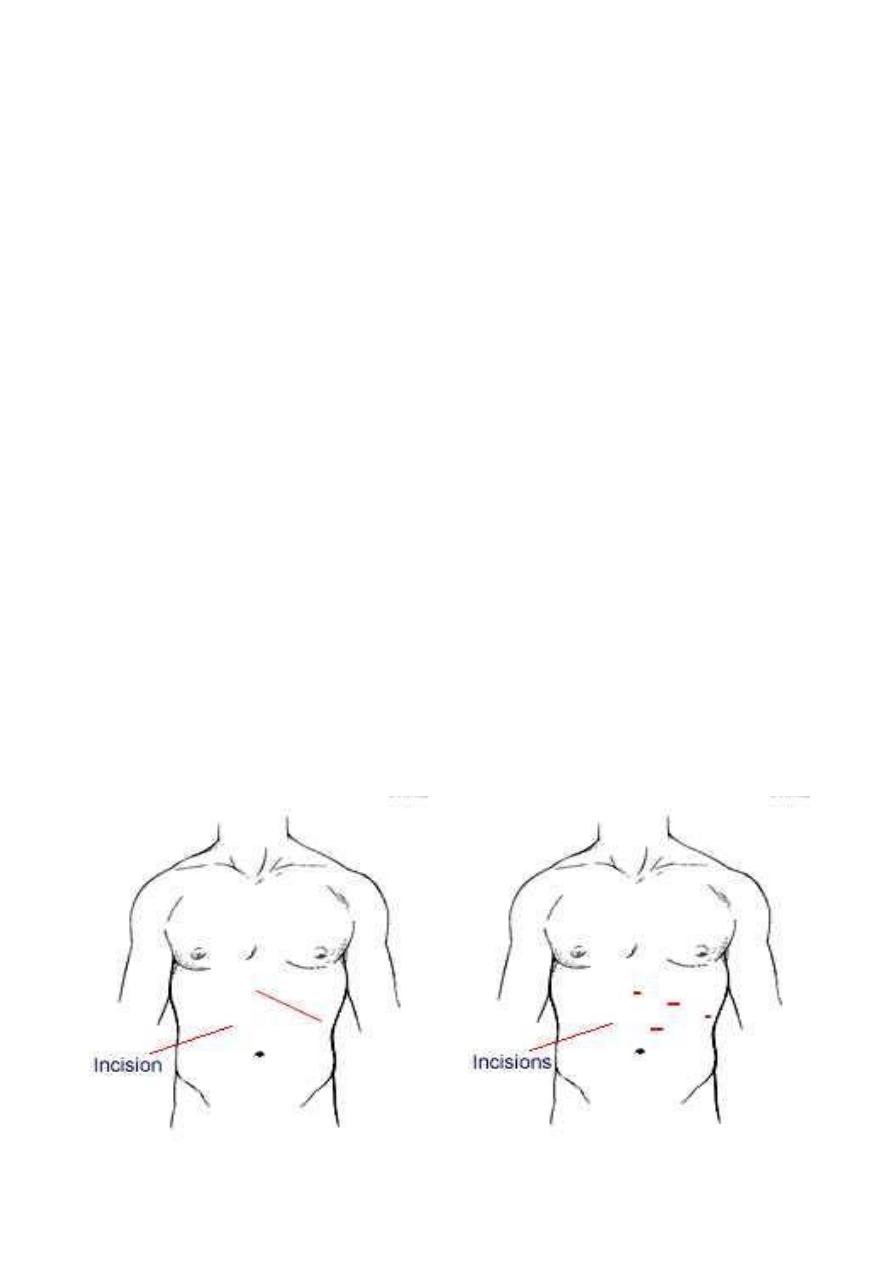
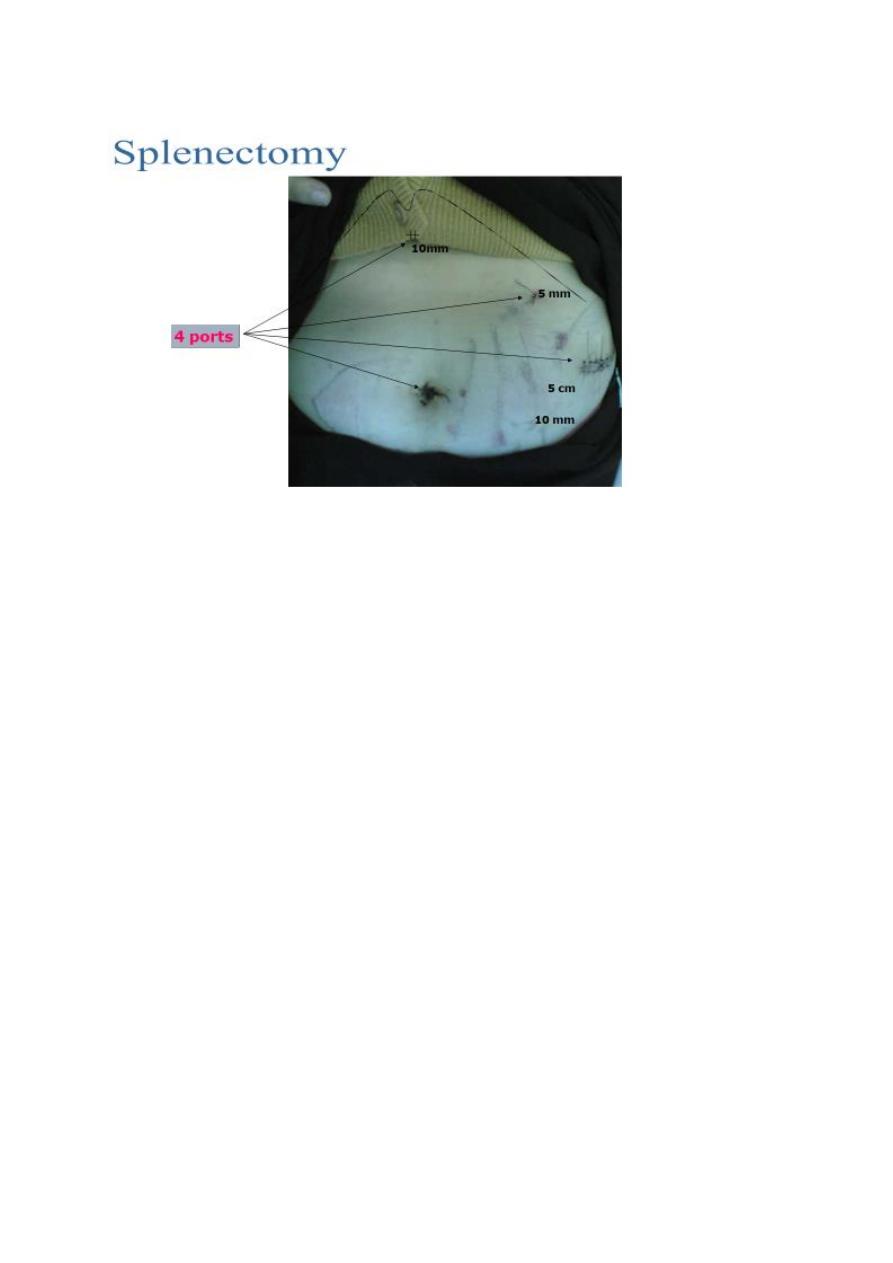
Technique:
Open splenectomy
Laparoscopic splenectomy
Open splenectomy
Laparoscopic splenectomy
9
Postoperative complications:
Local:
Haemorrhage
Haematemesis
Gastric dilatation
Iatrogenic injury to adjacent organs ;like
1 -
Pancreas ;
may lead to:
Pancreatitis
Local abscess
Pancreatic fistula
2 -
Stomach ;
a fistula may result from damage to the greater curvature
during ligation of short gastric vessels.
3 -
Colon , splenic flexure
Systemic:
1 -
Left basal atelectasis.
2 -
Pleural effusion.
3 -
Thrombocythemia;
Prophylactic aspirin is recommended if platelet count exceeds one million per
millilitre ,to prevent axillary or other venous thrombosis.
4 -
Post-splenectomy septicaemia.
5 -
Opportunist pos-splenectomy infection.
May result from S .pneumonia ,N .meningitidis ,H .influenzae, and E .coli.

11
Is a major concern for children who undergone splenectomy before the age
of 5 years.
Systemic:
The risk is increased in:
Young patients
Chemotherapy
Splenectomy for haematological disorders.
How do we can decrease the risk:
Vaccination
Prophylactic antibiotics
Postoperative recommendation
II- Antibiotic prophylaxis;
Daily oral penicillin, or erythromycin, or amoxicillin, or co-amoxiclav until the age of 10
years for those children who have undergone splenectomy before the age of 5
years.
For older children and adults is controversial; but since the risk of overwhelming sepsis is
greatest during the first 2 – 3 years of splenectomy it seems reasonable to give
prophylaxis antibiotics during this time.
Hereditary spherocytosis
Autosomal dominant
Defect in cell membrane ;increased permeability to Na.
Increased entry of H2O inside the RBC spherocytic RBC.
Spherocytic RBCs are fragile and need increased energy and O2 to pump sodium
outside the cell.
Spherocytic RBCs are destroyed in the spleen,
.indirect bilirubin .liver .excretion of bilirubin with bile .bile pigments stones
Clinical features:
Presentation generally in childhood
Intermittent jaundice, associated with anaemia ,splenomegaly and gall stones.
Haemolytic crisis; characterised by the onset of pyrexia ,abdominal pain, nausia
and vomiting and extreme pallor followed by increased jaundice.
Examination:
Pallor ,mild jaundice, leg ulcers

11
Splenomegaly
Normal color urine
Investigation:
Increased indirect bilirubin
Anaemia ,immature reticular cells
Increased urobilinogen in faeses and urine
Increased fragility test of RBCs;
Normal RBCs begin to haemolyse in 0.47 %
saline
In HS aemolysis occur in 0.6 %
saline
Any child with gall stone disease should be investigated for hereditary spherocytosis
and a family history sought.
Radioactive chromium (51Cr) labelling of the patient’s own RBC
Decreased life span of RBCs
Increased sequestration of RBCs in spleen.
Ultrasound examination:
Splenomegaly
Gall stones
Treatment:
Splenectomy;
In young children it is preferable to delay splenectomy until 6 years of age to
minimise the risk of post-splenectomy sepsis.
NEOPLASMS
Haemangioma
Lymphoma is the most common cause of neoplastic enlargement
The spleen is rarely the site of metastatic disease
Cysts of the Spleen
Non parasitic
Embryonal cysts
Parasitic
Hydatid cyst
Selected nonparasitic cyst may be managed by aspiration
Splenectomy should be performed for all large cyst and those with an uncertain
diagnosis.
