1
Forth stage
Surgery
Lec-1
د
.
ليث
الحرباوي
1/1/2014
Principles of colonic surgery
Colonic anastomosis
is more liable for : disruption , leakage & peritonitis because of the followings:
1-the highly infective aerobic &anaerobic organisms in the colon.
2-constant gaseous distention.
3-Incomplete serous coat.
4-the terminal arteries poorly connect with each other.
Preoperative preparation for colonic surgery
•
Patient counseling
•
Improving nutritional status
•
Bowel preparation
In order to reduce the risk of leakage &wound sepsis:
The bowel must be empty at the time of operation
The bacterial flora of the colon is reduced
In elective cases the bowel is empty &clean ,so primary resection
(i.e. Resection &anastomosis at the same session)
Mechanical preparation:
1- Standared preraration
non-residue diet for 4 days before the operation
enemas & mild laxatives 2-3 days before the operation
2- rapid preparation: is an alternative that can be performed one day before surgery
by one of the following methods:
a- whole gut irrigation using 2-3 L/hour of a balanced
crystalloid solution passed through a nasogastric tube
until the patient passes clear fluid per rectum.
(This method is not used in patients with cardiac ,renal
diseases &in those with partially obstructed colon)
b-Mannitol: one liter of flavoured Mannitol is given orally or by nasogastric tube.
Metachlopromide may be administered to inhibit vomiting.
2
Chemical preparation:
intestinal antiseptics administered orally help to reduce the density of colonic
bacteria
Combination of Neomycin & Metronidazole (Flagyl) for 2 days will cover
the gram
–ve bacilli and anaerobes which are normal residents in the large
intestine
Prophylactic parenteral Antibiotics:
To minimize septic complication following colonic surgery ,systemic
antibiotics are administered immediately before surgery & are continued for
1 day postoperatively ,this is termed ''perioperative antibiotic prophylaxis'‘
and is usually a combination of Cephalosporin or an aminoglycoside with
either metronidazole or clindamycin .
Operative Procedure
Resection:
The extent of resection is governed by the arterial blood supply &by the
disease process
In radical surgery for malignant tumors ,it is essential to remove the draining
lymphatics
Division of the peritoneal attachments allowsadequate mobilization of the
bowel on its mesentery.
Anastomosis:
For a successful anastomosis the two bowel ends should be adequatly
vascularize and should be sutured without tension
An intestinal anastomosis can be done in one of 2 methods:
Hand suturing
is commonly done in 2 layers of interrupted sutures .
The first layer induces the whole wall thickness .
while the second incorporates the serosa and muscle only .to invert & seal
the suture line .The defect in the mesentery is closed to prevent an internal
hernia .
-
Mechanical staplers
are increasingly used ,They are faster but more coasty
3
Emergency Surgery:
In patients with obstruction ,,perforation ,toxic dilatation .or massive bleeding
from the colon
→emergency surgery may be required.
In clinically ill obstructed cases ,a temporary Proximal colostomy to
decompress the colon is done ,postponing resection to a later date.
If the patient's condition allows resection of the diseased colon should be
carried out in the course of the emergency operation
After exision of the diseased segment,
the surgeon is faced with a colon that is heavily loaded with stools and
bacteria ,the decision for further management depends on the site of the
resected part .
with right colon resection ,restoration of the bowel continuity by primary
anastomosis is feasible. The ilium is anastomosed to the transverse colon (ilio-
transverse anastomosis)
With emergency excision of the other parts of the colon ,primary anastomosis
is avoided because of the high possibility of disrupted suture line &leakage .The
options are:
a-the proximal colon end is opened to the skin as a temporary colostomy .and the
distal end is closed by sutures and replaced in the abdomen (Hartmann's
procedure) ,both ends are opened to the skin ,the proximal one as a temporary
colostomy ,
2.distal one as a mucous fistula ,
In either case,a second operation is needed to restore bowel continuity within few
weeks
This second elective operation should be preceded by proper bowel preparation ..
Intestinal stomas
Intestinal stomas
ileostomy
Indications
Proctocolectomy for ulcerative colitis or familial polyposis coli.
Conventional ileostomy
The stoma is fashioned so that a nipple of ileum protrudes from the skin,
facilitating direct delivery of the irritant small bowel con-tent into an appliance.
Conventional ileostomosis are incontinent.

4
Continent ileostomy
A continent ileostomy may be done by fashioning a valve with an underlying
reservoir (Kock pouch) which the patient regularly evacuates by passing a tube.
Colostomy
A colostomy is an opening of the colon to the skin.
Indications:
Temporary colostomy
1. To relieve large bowel obstruction in patients with:
•
High anorectal malformations.
•
Hirschsprung disease.
•
Inflammatory stricture.
•
Carcinoma of the colon.
After the obstruction is relieved, the colon is prepared and the cause is corrected.
Later, the colostomy is closed. This is called three-stage management of acute
colon obstruc-tion.
2. Injuries of the colon. The injured segment is either exterior-ized as a colostomy,
or is closed and a proximal diverting colostomy is performed.
3. To protect a distal doubtful colonic or rectal anastomosis.
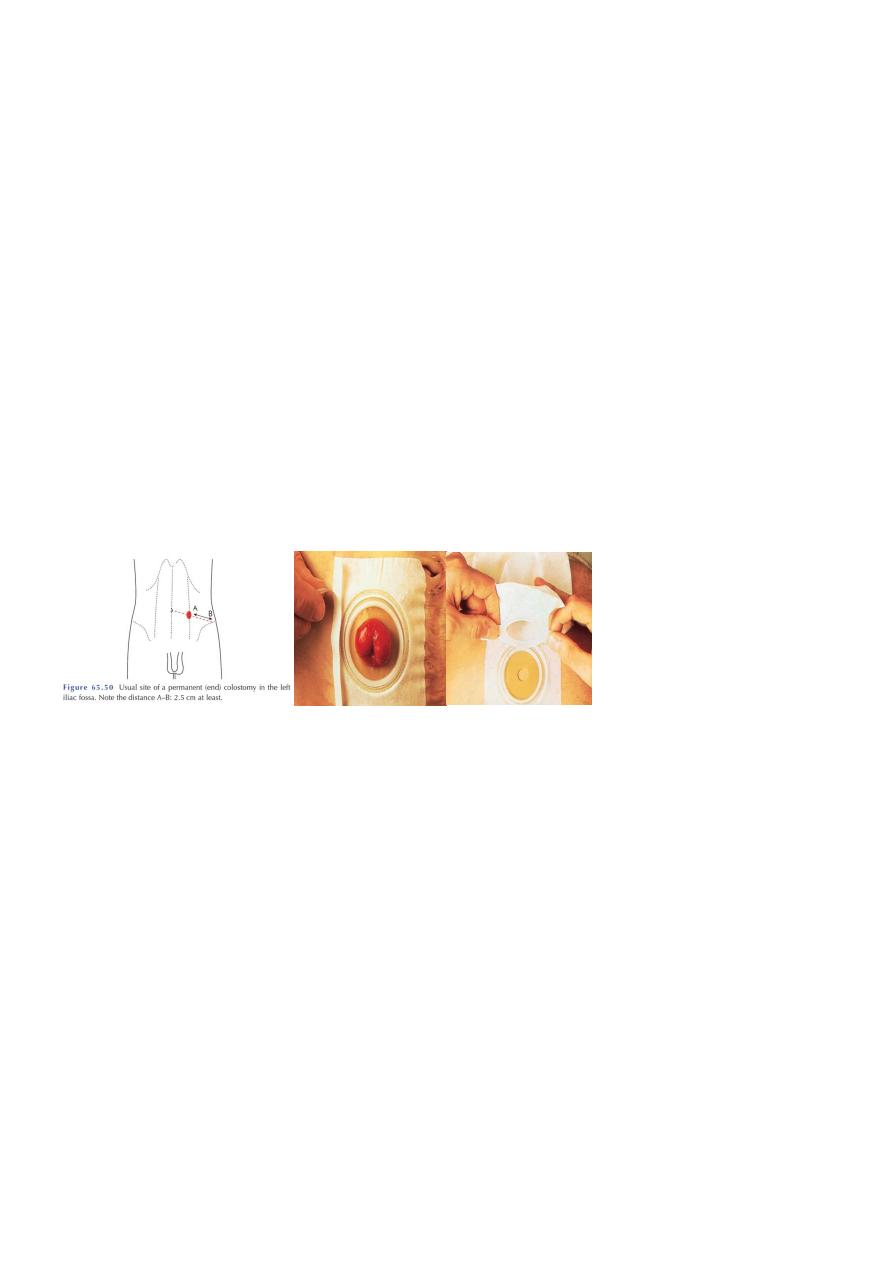
Permanent colostomy
After abdomino-perineal resection.
Irresectable carcinoma of the large bowel with obstruction.
Incurable cases of anal incontinence.
High anal fistulae that is not amenable to surgery.
5
Types:
Loop colostomy is usually temporary and is usu-ally done in the right side of
the transverse colon (transverse colostomy). This part is brought to the
surface, fixed to the ab-dominal wall, opened along one of the taeniae coli,
and then stitched to the skin. A rod is passed beneath the loop to pre-vent
retraction, and is removed after one week.
End colostomy may be permanent or temporary. It is com-monly constructed
in the left or the sigmoid colon (iliac colos-tomy) by bringing the divided end of
the bowel to the surface.
The lateral space between the exiting colon and the parietal peritoneum is closed
to prevent an inter-nal hernia. The colon is fixed to the abdominal wall muscles
and is then stitched to the skin.
3. Caecostomy is occasionally used for temporary decompres-sion of the colon but
it is not as effective as the loop colostomy. Caecostomy is done by inserting a
wide bore tube into the caecum.
Colostomy care
A colostomy is an incontinent opening on the abdominal wall.
An iliac colostomy is easy to manage, as by time it functions once or twice a
day. The patient usually uses a colostomy ap-pliance and evacuates its plastic
bag when it is full .An alternative method is to wash out the colon through the
colostomy once every morning. As the colostomy does not act during the rest
of the day, a simple dressing is all that is neces-sary.
A transverse colostomy is wet, i.e., it discharges semi-liquid stools frequently,
and, therefore, requires an appliance.
Complications of colostomy
The following complications can occur to any colostomy but are more common after
poor technique or siting of the stoma:
prolapse;
retraction;
necrosis of the distal end;
fistula formation;
6
stenosis of the orifice;
colostomy hernia;
bleeding (usually from granulomas around the margin of the
Colostomy)
colostomy
‘diarrhea’: this is usually an infective enteritis and will respond to
oral metronidazole 200 mg three times daily.
Many of these complications require revision of the colostomy.
Sometimes, this can be achieved with an incision immediately around the stoma
but, on occasion, reopening the abdomen and freeing up the colostomy may be
necessary. Occasionally, transfer to the opposite side of the abdomen may be
necessary.
