1
Forth stage
Surgery
Lec-7
د
.
ليث
الحرباوي
4/18/2016
Hirschsprung's disease
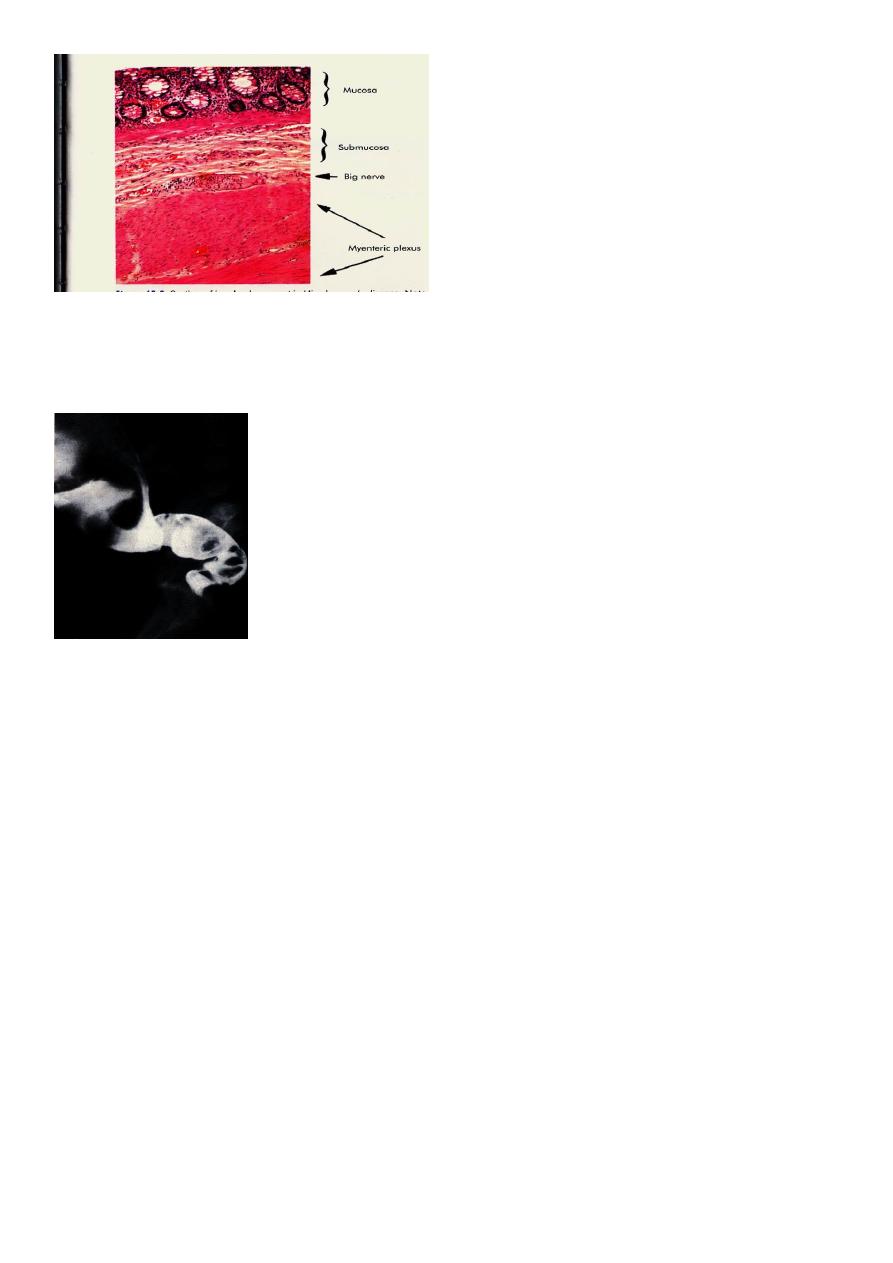
- Caused by an absence of ganglia in the myenteric plexus usually of the distal hind
gut.
- May affect a short or long segment.
Usually presents in neonatal life with large bowel obstruction.
-
-Milder forms may be missed at birth and present in later childhood with severe
constipation.
Diagnosis depends on a full thickness rectal biopsy.
-
-Treatment usually requires on emergency defunctioning stoma shortly after birth
and a major reconstructive procedure later.
Clinical features:
Hirschsprung's disease occurs in approximately one in 4500 lived births, It shows a
familial tendency and is more common in males than in females.
In over 10% of patients, it is associated with Down syndrome.
The clinical picture varies from acute intestinal obstruction in neonates to chronic
constipation in later life.
Diagnosis:
Rectal biopsy
2
Anorectal Manometry
Radiology:
Treatment :
1.Duhamel operation
2.Swenson's procedure
3.Coloanal anastomosis
4.Restorative Proctocolectomy
Colon Diverticula:
Diverticula of the colon are acquired herniations of colonic mucosa, protruding
through the circular muscle at the points where the blood vessels penetrate the
colonic wall. They tend to occur in rows between the strips of longitudinal muscle,
some-times partly covered by appendices epiploicae. The condition is most
commonly found in the sigmoid colon, hut the caecum can also be involved,
and on occasion the entire large bowel can be affected. The rectum with its
complete muscle layers is not affected. In 90% of cases, the sigmoid colon, is
involved and is almost always the site of inflammation, i.e. diverticulitis. Some 5% of
patients have associated gallstones and hiatus hernia (Saint's triad).
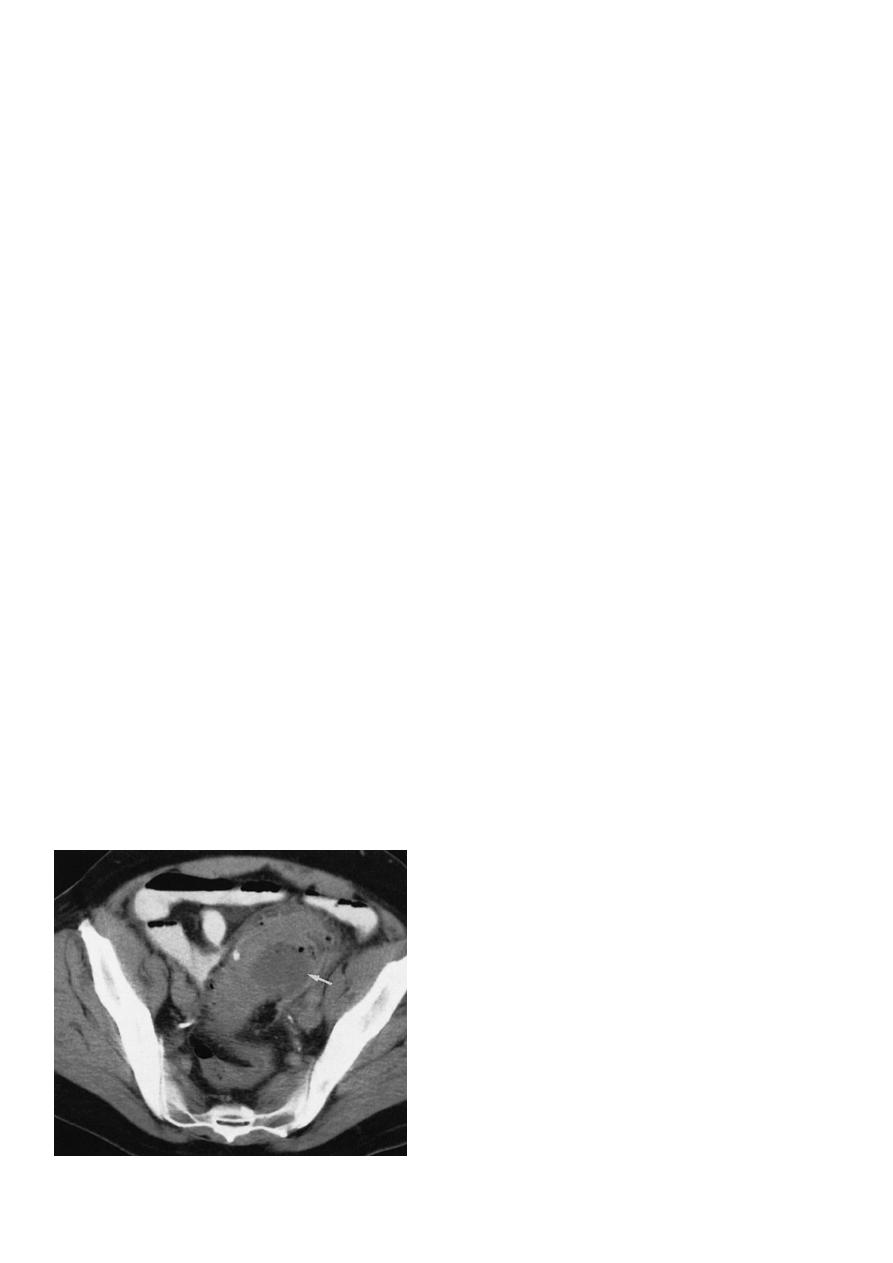
Barium enema showing sigmoid
diverticular disease ‘saw-teeth’ and
diverticula

3
Diverticular disease is rare in Africans and Asians, who eat a diet that contains
natural fibre. In Western countries, where the roughage has been removed from
flour and refined sugar forms a large part of the diet, divcrticula are found in 25% of
patients over the age of 40 receiving barium enemas, and the incidence increases
with age.
Diverticulosis:
It is important to distinguish between diverticulosis and the pres-ence of diverticula,
which may be asymptomatic, and clinical diverticular disease in which the diverticula
are causing symp-toms. Diverticula probably arise as a result of muscular
incoordination and spasm, resulting in increased segmentation and intraluminal
pressures.
Excessive segmentation in response to food, prostigmine and morphine is found in
colonic motility studies, and this exaggerated response is more apparent in
symp-tomatic than in asymptomatic individuals. On histological inves-tigation, the
diverticulum consists of a protrusion of mucous membranes covered with
peritoneum. There is thickening of the circular muscle fibres of the intestine, which
develops a con-certina or saw-tooth appearance on barium enema .
Diverticulitis
Diverticulitis is the result of inflammation of one or more diver-ticula, usually with
some pericolitis. Episodes of diverticulitis may be followed by years free of
symptoms, but the condition is essentially progressive - the longer the duration the
worse the symptoms and the greater the risk of complications. Diverticulitis is not a
precancerous condition, but cancer may coexist
Complications of diverticular disease
1.Diverticulitis
2.Pericolic abscess
3.Peritonitis
4.Intestinal obstruction
5.Haemorrhage
6.Fistula formation
Clinical features:
4
Diverticulosis may be asymptomatic, but the disordered colonic function may cause
symptoms of distension, flatulence and a sensation of heaviness in the lower
abdomen, all of which may be indistinguishable from the symptoms of irritable bowel
syndrome.
Excessive colonic segmentation can cause severe pain in the left iliac fossa, but this
must be distinguished from episodes of often subclinical inflammation in the sigmoid
colon as a result of diverticulitis.
Persistent lower abdominal pain, usually in the left iliac fossa, with or without
peritonitis, in patients of either sex over the age of 40, could be caused by
diverticulitis.
Fever, malaise and Leucocytosis can differentiate diverticulitis from painful
diverticulosis. The patient may pass loose stools or may be constipated; the lower
abdomen is tender, especially on the left, but occasionally also in the right iliac fossa
if the sigmoid loop lies across the mid-line.
The sigmoid colon is often palpable, tender and thickened. Rectal examination may,
but does not usually, reveal a tender mass. The condition has been likened to left-
sided appendicitis. Any urinary symptoms may-herald the formation of a vesicocolic
fistula, which leads to pneumaturia (flatus in the urine) and even faeces in the urine.
Diagnosis:
Radiology
Diverticulosis, like 'irritable bowel' syndrome, is a diagnosis of exclusion, and
symptoms should not be attributed to diverticulosis unless other diseases have been
excluded by barium enema, sigmoidoscopy or colonoscopy. Although the diagnosis
of acute diverticulitis is made on clinical grounds, it can be confirmed during the
acute phase by (CT).
5
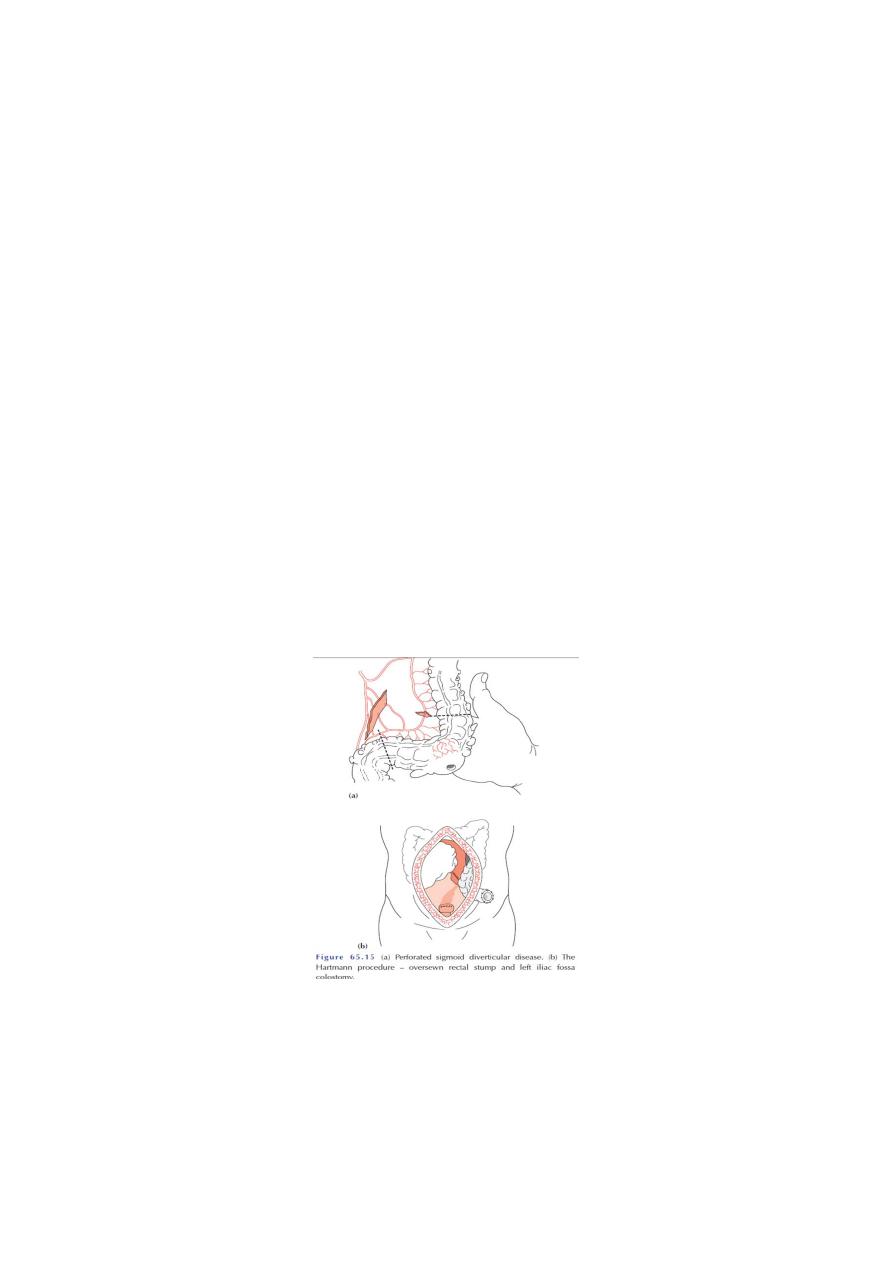
Computerized tomography scan showing a segment of thickened sigmoid colon with
a paracolic abscess (arrow) in a patient with diverticulitis.
This will demon-strate not only the diverticula but also any associated pericolic
abscess .Barium enemas & sigmoidoscopy are usually reserved for patients who
have recovered from an attack of acute diverticulitis, for fear of causing perforation
or peritonitis.
Water-soluble contrast enemas may, however, be helpful in sorting out patients with
large bowel obstruction. Barium radiology is carried out to exclude a carcinoma and
to assess the extent of the disease. Where the sigmoid colon is thickened and
narrowed, a 'saw-
tooth’ appearance may be seen.
Some strictures can be very difficult to distinguish by radiology alone, and in those-
circumstances colonos-copy will be necessary to rule out a carcinoma.
Vesicocolic fistulae should be evaluated with cystoscopy and biopsy in addition to
colonoscopy. Plain abdominal radiography may show gas within the bladder, and
contrast examinations may show the fistula itself. The differential diagnosis for
vesicocolic fistulae (and other fistulae) includes cancer, radiation damage, Crohn's
disease, tuberculosis and actinomycosis. The surgical approach, to each of these
may differ substantially, reinforcing the need for tissue diagnosis where possible.
Operative procedures for diverticular disease
