1
4th stage
Surgery
Lec-
Dr.Mohamad
fawzi
20/12/2015
Bladder tumor
Facts
•
Bladder cancer is the second most common cancer of the genitourinary tract.
•
Bladder cancer three times more common in men .
•
The average age at diagnosis is 65 years.
•
At the time of diagnosis , approximately 75% of bladder cancers are localized to the
bladder; 25% have spread to regional lymph nodes or distant sites.
Risk Factors & Pathogenesis
1) Cigarette smoking
2) Occupational exposure . Workers in the chemical, rubber, petroleum, leather, and
printing industries
3) Pelvic Irradiation.
4) Cyclophosphamide.
5) physical trauma to the urothelium induced by infection, instrumentation, and calculi .
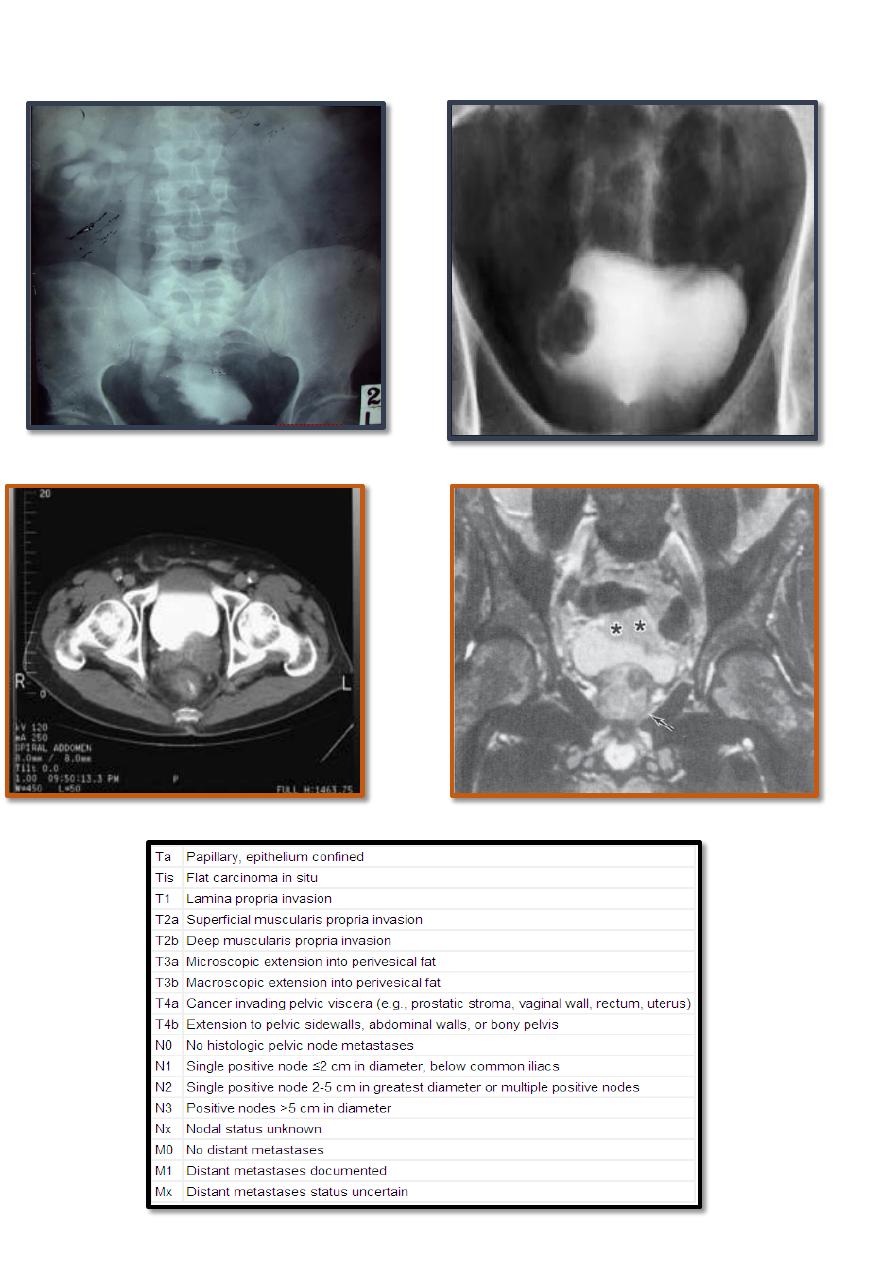
Histopathology
Ninety-eight percent are epithelial , with most being transitional cell carcinomas
1- Transitional Cell Carcinoma (TCC):
•
commonly appear as papillary, ; less commonly, sessile or ulcerated.
•
Carcinoma in situ (CIS) is recognizable as flat, anaplastic epithelium.
2- Adenocarcinoma: account for <2% .
3-squamous cell carcinoma (SCC)
2
Secondary bladder tumors:
•
Cancers of the prostate, cervix, and rectum may involve the bladder by direct extension.
•
The most common tumors metastatic to the bladder include melanoma, lymphoma,
stomach, breast, kidney, lung and liver .
Clinical Findings
A. SYMPTOMS:
•
Hematuria 85–90% of patients with bladder cancer usually painless.
•
Symptoms of advanced disease include bone pain from bone metastases or flank
pain from retroperitoneal metastases or ureteral obstruction
B. LABORATORY FINDINGS
1. Routine testing
GUE…….. Hematuria most common …. , pyuria,.. from concomitant UTIs
•
Azotemia in patients with ureteral occlusion owing to the primary tumor or
lymphadenopathy.
•
Anemia may be a presenting symptom owing to chronic blood loss, or replacement of
the bone marrow with metastatic disease.
2. Urinary cytology
3. Other markers: Commercially available tests include, the BTA test and NMP22.
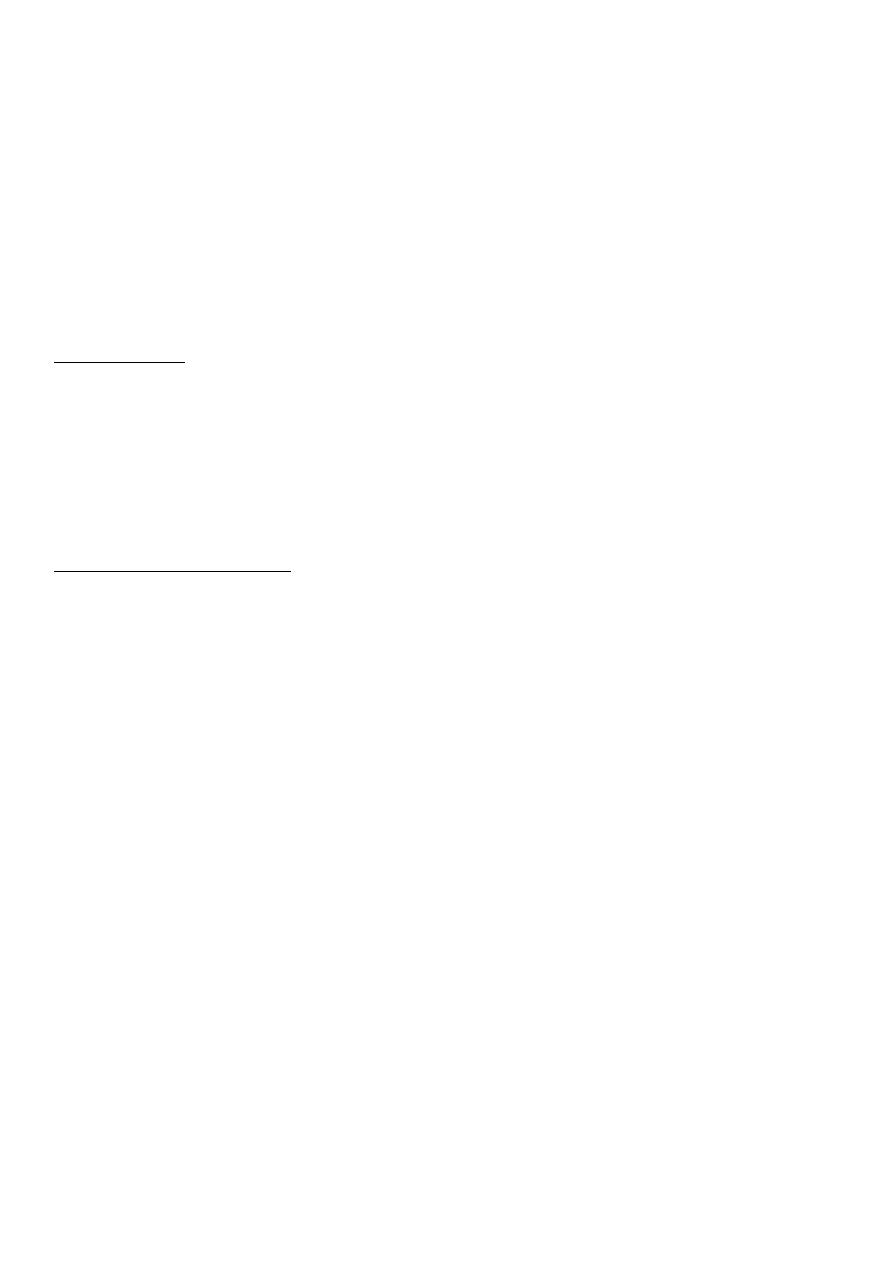
4- Imaging Studies:
A- IVU.
B- U/S.
C- CT. SCAN , MRI.
D- chest x-ray and radionuclide bone scan.
5..difinit diagnosis by cystoscopy and biobsy
3
4
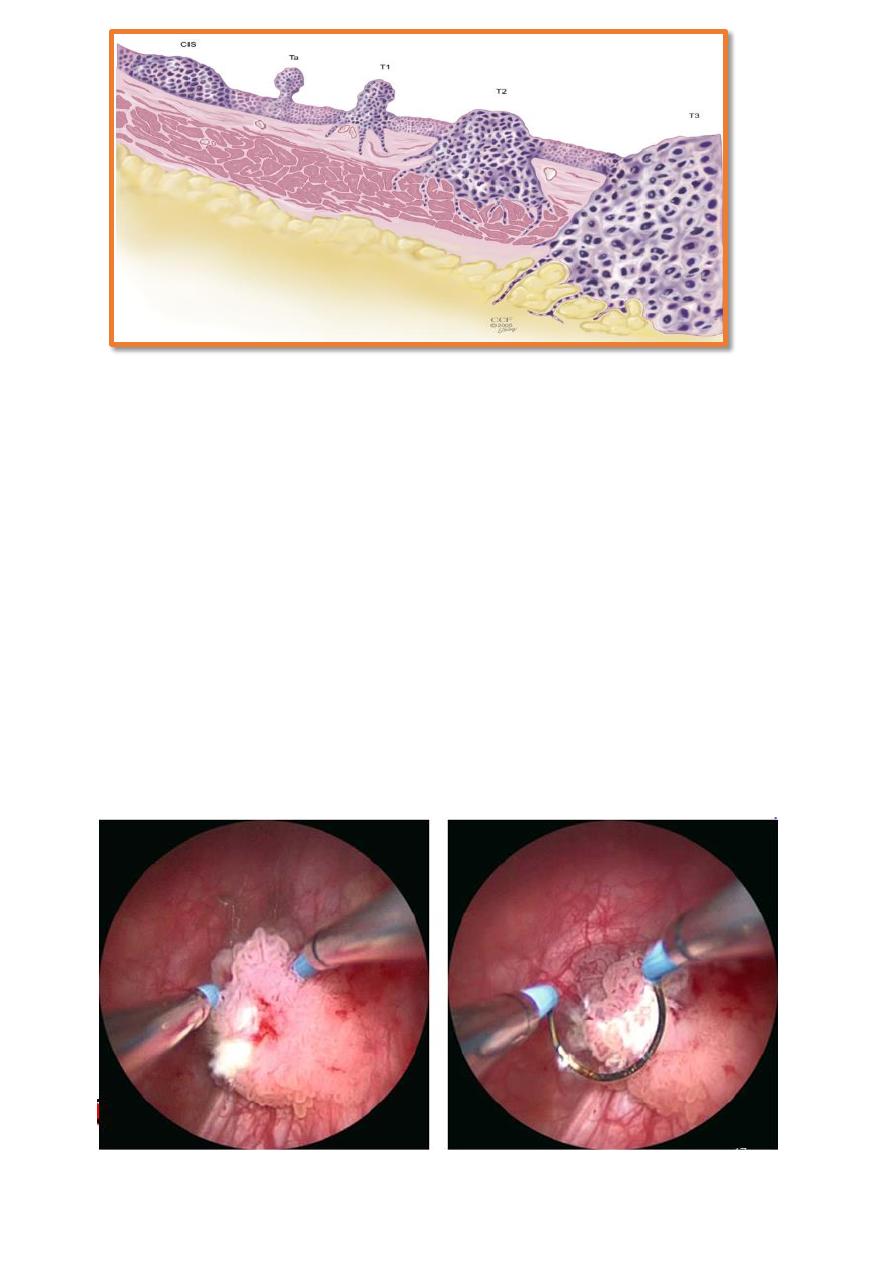
TREATMENT
•
Once a tumor is visualized or suspected, the patient is scheduled for examination under
anesthesia and TURT and biopsy of the suspicious lesion.
•
The objectives of TURT are
1. tumor diagnosis,
2. assessment of the degree of bladder wall invasion (staging),
3. and complete excision of the lesions.
TURT
5
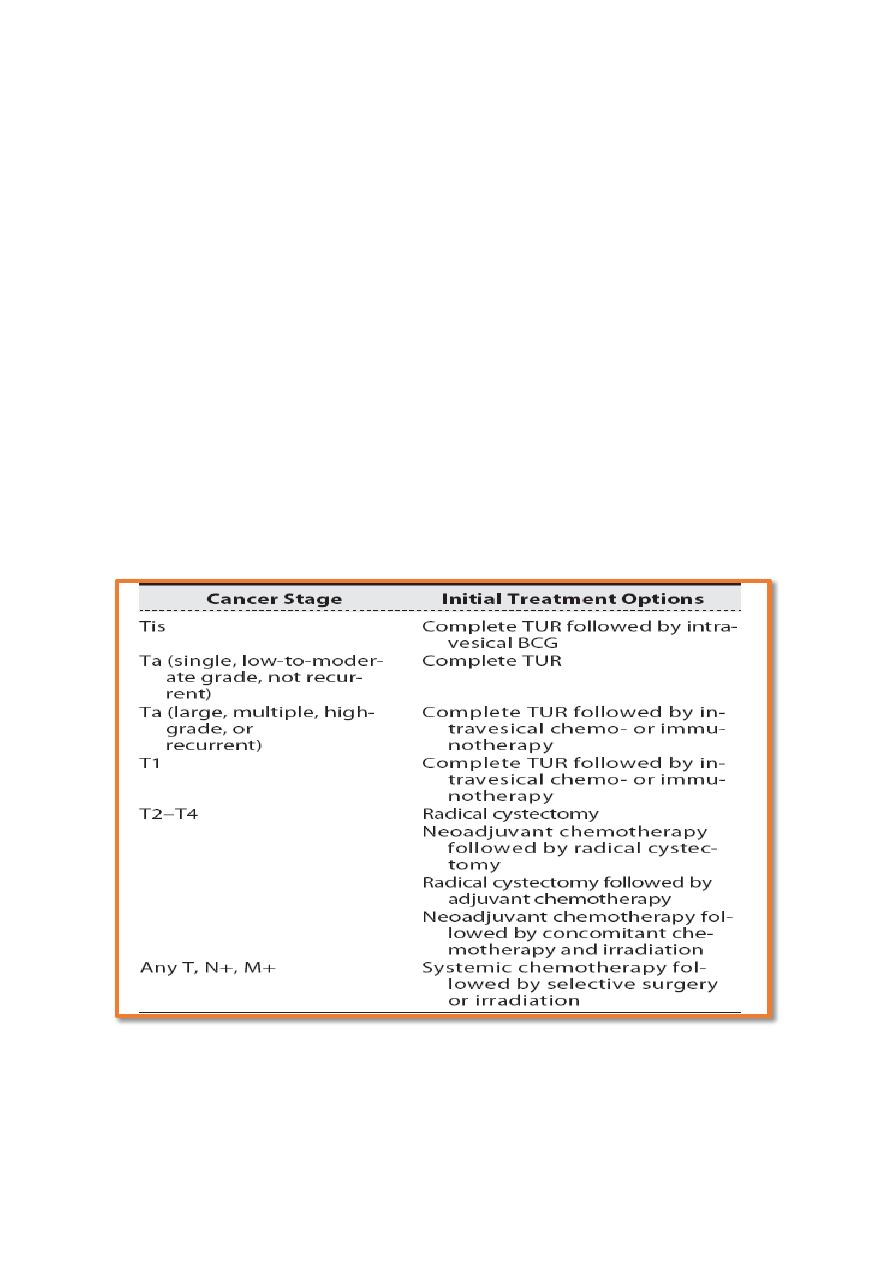
TREATMENT
SUPERFECIAL BT (Ta , T1 )
<<
Small,low grade ,single,
TURT then check scope every three months
SUPERFECIAL BT (Ta , T1 )
<< large, multiples ,high grade ,associated CIS, recurrent
TURT,intrasical chimotherapy ,and check scope every three months
DEEP BT (T2-T4)
Radical cystectomy with urinary diversion
(radiotherapy for unfit patient)
METASTATIC TUMOR
Systemic chimotherapy

6
intravasical chemotherapy
•
Immunotherapeutic (Bacillus Calmette-Guérin BCG) or chemotherapeutic agents
(mitomycin C, thiotepa , and Gemcitabin) can be instilled into the bladder directly
via catheter, thereby avoiding the morbidity of systemic administration in most cases.
•
Most agents are administered weekly for 6 weeks .
SURGERY
1. TURT : is the initial form of treatment for all bladder cancers. It allows a reasonably
accurate estimate of tumor stage and grade and the need for additional treatment.
•
Patients who presented initially with multiple or higher grade lesions (or both) and
those who have recurrences at 3 months require more careful surveillance. In such
patients, cystoscopy at 3-month intervals is necessary.
Complications of TURBT:
•
Bleeding , Clot Retention And Bladder Perforation.
2. Partial cystectomy:
•
Patients with solitary, infiltrating tumors (T1–T3) localized along the posterior lateral
wall or dome of the bladder are candidates for partial cystectomy, as are patients
with cancers in a diverticulum.
3. Radical cystectomy and Urinary diversion:
•
implies removal of the anterior pelvic organs: in men, the bladder with its
surrounding fat and peritoneal attachments, the prostate, and the seminal vesicles;
•
in women, the bladder and surrounding fat and peritoneal attachments, cervix,
uterus, anterior vaginal vault, urethra, and ovaries.
•
This remains the “gold standard” of treatment for patients with muscle invasive
bladder cancer

7
CHEMOTHERAPY
•
15% of patients who present with bladder cancer have regional or distant
metastases.
•
The regimen of methotrexate, vinblastine, doxorubicin (Adriamycin), and cisplatin
(MVAC) has been the most commonly used.
