
1
Forth stage
Surgery (Urology)
Lec-11
د.محمد فوزي
10/3/2015
Neurogenic bladder
-The urinary bladder is probably the only visceral smooth muscle that is under complete
voluntary control from cerebral cortex
-It has both somatic & autonomic innervations
-The functional features include:
1. A normal capacity of 400 – 500 ml
2. Sensation of fullness
3. Volume change without change in intraluminal pressure
4. Initiation & maintenance of contraction until bladder is empty
5. Voluntary initiation or inhibition of voiding
The sphincteric unit:
In both male & females, two sphincters:
1. Internal : involuntary smooth muscle sphincter, at bladder neck
2. External : voluntary striated muscle sphincter, from the prostate to membranous
urethra in males & at mid urethra in females
Innervation :
Parasympathetic : S 2 – 4
Symp. : T10 – L 2
Somatic motor innervation :S 2 – 3 though the pudendal N.
Classification of neurogenic bladder
• Upper motor neuron , spastic , uninhibited ((injury above spinal cord micturition
center))
• Lower motor neuron, flaccid , atonic, areflexic ((injury in the pelvic nerves or spinal
micturition center))
2
N.B. :Spinal shock
- Immediately after injury, regardless of the level, there is a stage of flaccid paralysis with
numbness below the level of the injury that lead to bladder overfilling to the point of
overflow incontinence & rectal impaction.
-It last few weak up to 6 months during this the bladder should be drained by a catheter
Clinical picture
-UMNL : reduced capacity , involuntary detrusor contraction , high intravesical detrusor
pressure , spasticity of pelvic striated M. , autonomic dysreflexia in cervical cord lesions
-LMNL : large bladder capacity, lack of voluntary detrusor contraction, low intravesical
pressure, deceased tone in external sph.
N.B.: full neurologic examamination Is required for those patients
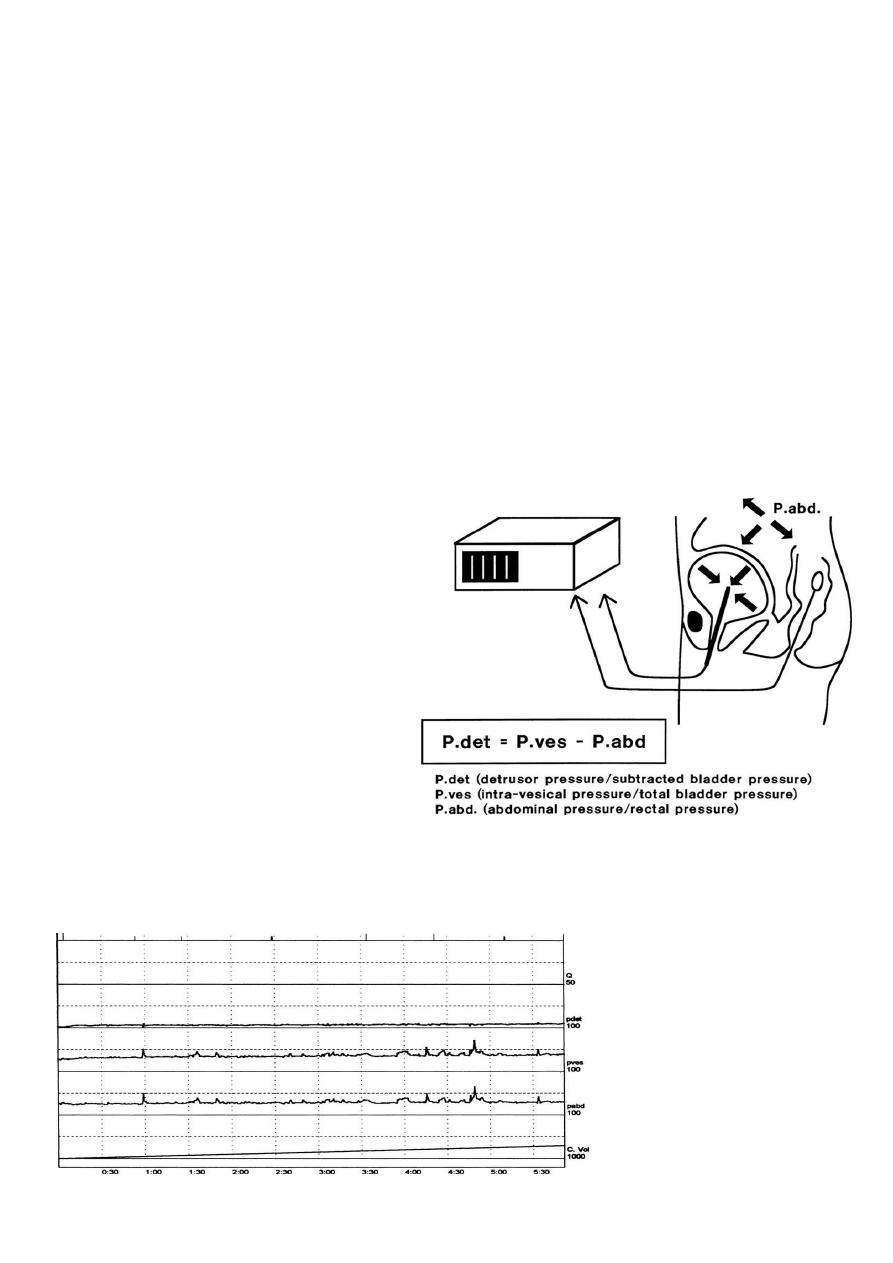
Investigations
1. Urinalysis
2. Renal function test
3. Imaging study
4. Instrumental exam. Cystoscopy
5. Urodynamic studies
"UDS"
3
Differential diagnosis
1. Cystitis
2. Chronic urethritis
3. Vesical irritation 2ry to psychic disturbance
4. Interstitial cystitis
5. Cystocele
6. Infravesical obstruction
Treatment
-The treatment is guided by the need to restore low pressure activity to the bladder in
order to preserve renal function, continence, & control infection
-Spinal shock ---> bladder drainage is required by intermittent catheterization , indwelling
catheter or suprapubic cystostomy
- Increase fluid intake to 2 – 3 l/day
- Spastic neuropathic bladder ---> many options:
1. Voiding by trigger tech.
2. Anticholinergic medications (parasympatholytic drugs) like oxybutynin(ditropan)
5mg 2-3 times /day
3. Indwelling catheter or CIC
4. Condom catheter & leg bag
5. Sphincterotomy
6. Sacral rhizotomy at S 3-4
7. Neurostimulation
8. Urinary diversion
-Flaccid neuropathic bladder ---->
1. Crede maneuver ( manual suprapubic pressure) accompanied by straining
2. Bladder training & care , voiding every 2hr
3. CSIC every 3-6 hr
4. TUR in hypertrophied bladder neck or BPH
5. parasympathmimetic drugs like bethanecol chloride( Urecholine) 5 – 50 mg every
6-8hr
4
complications
1. Infection : cystitis, periurethritis, prostatitis, epididymoorchitis, pyelonephritis
2. Hydronephrosis
3. Calculus
4. Renal imperment
5. Autonomic dysreflexia:
- dramatic elevation in systolic &/or diastolic pressure, increase pulse pressure,
bradycardia, headache, piloerection. brought by over distention of the bladder in
patients with cord lesion above T1
-Treatment of autonomic dysreflexia :
1) immediate catheterization
2) oral nifedipine (20mg) 30 min before cystoscopy as prophylaxis
3) alpha adrenergic blockers
prognosis
The greater threat to those patients is progressive renal damage caused by:
1) pyelonephritis
2) calculosis,
3) hydronephrosis
