1
fourth stage
Medicine
Lec-3
Dr.Jasim
2/11/2015
Arrhythmias
Arrhythmias is Disturbance of heart rhythm and/or conduction.
Sinus Rhythms
Premature Beats
Supraventricular Arrhythmias
Ventricular Arrhythmias
AV Junctional Blocks
1. Sinus Rhythms
Sinus Bradycardia
Sinus Tachycardia
Sinus Bradycardia
Deviation from NSR : A sinus rate of less than 60/min
Causes of Sinus Bradycardia
MI
Sinus node disease (sick sinus syndrome)
Hypothermia
Hypothyroidism
Cholestatic jaundice
Raised intracranial pressure
Drugs, e.g. β-blockers, digoxin, verap
2
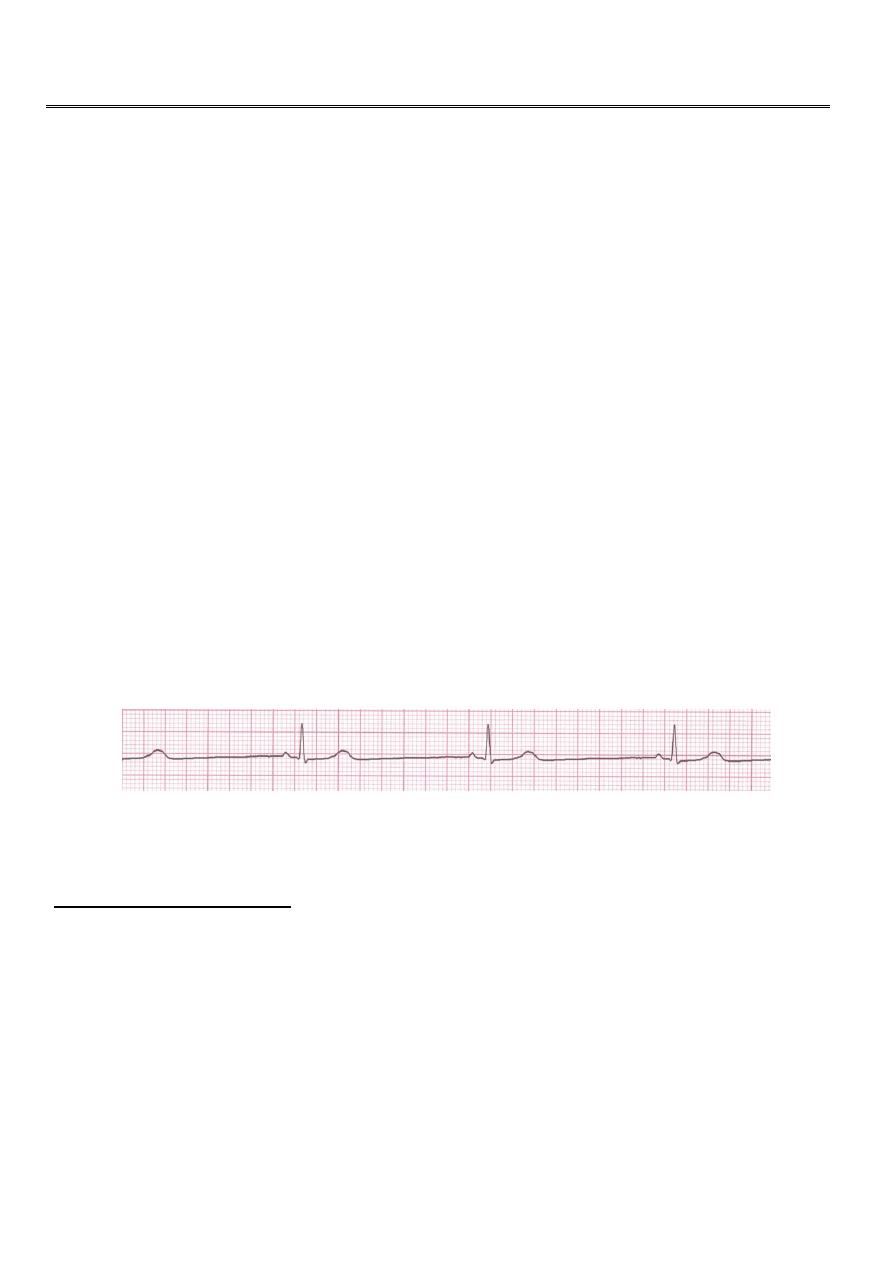
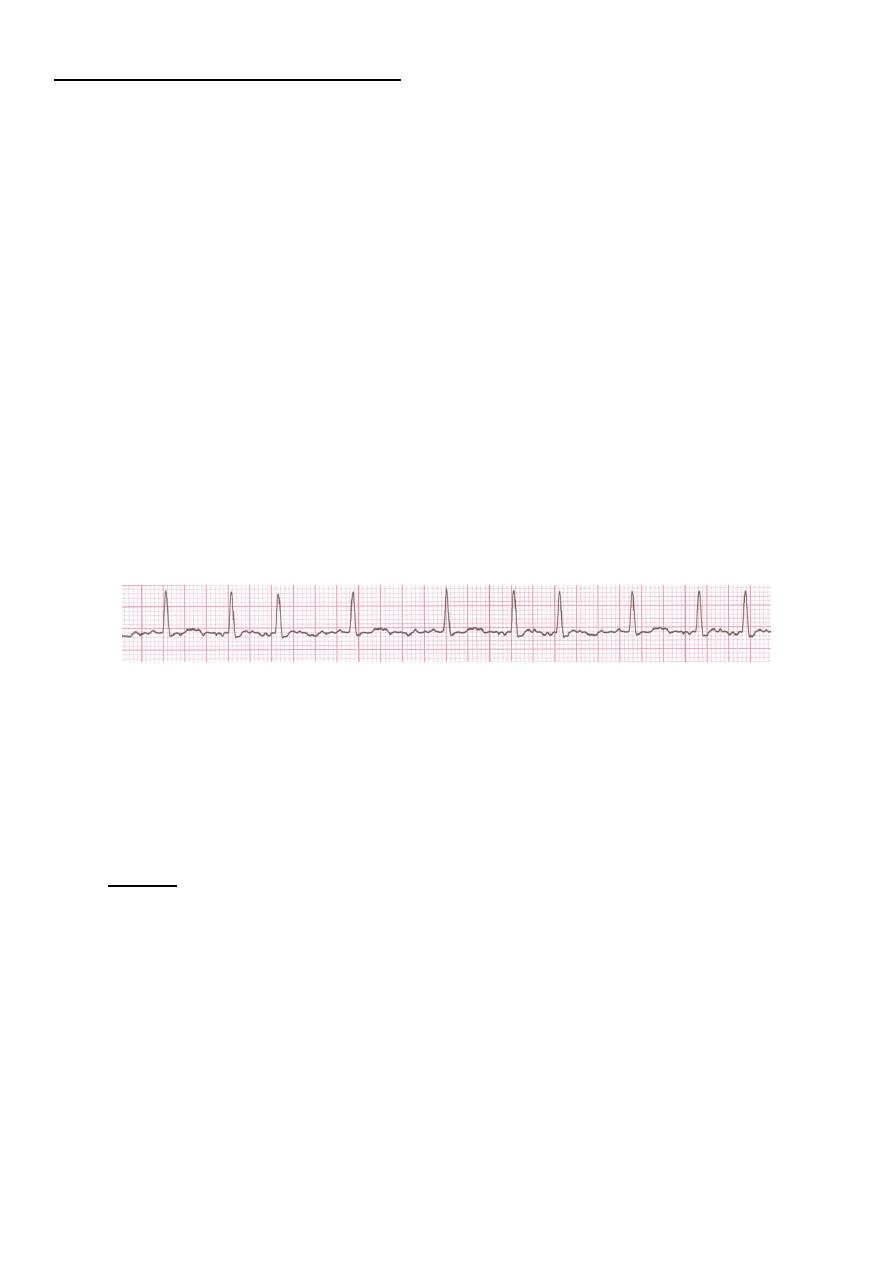
Rhythm
Rate ? 30 bpm
Regularity? regular
P waves? normal
PR interval? 0.12 s
QRS duration? 0.10 s
Interpretation? Sinus Bradycardia
Sinus Tachycardia
• Deviation from NSR
-a sinus rate of more than 100/min
Causes of Sinus Tachycardia
Anxiety
Fever
Anaemia
Heart failure
Thyrotoxicosis
Phaeochromocytoma
Drugs, e.g. β-agonists (bronchodilators)

3
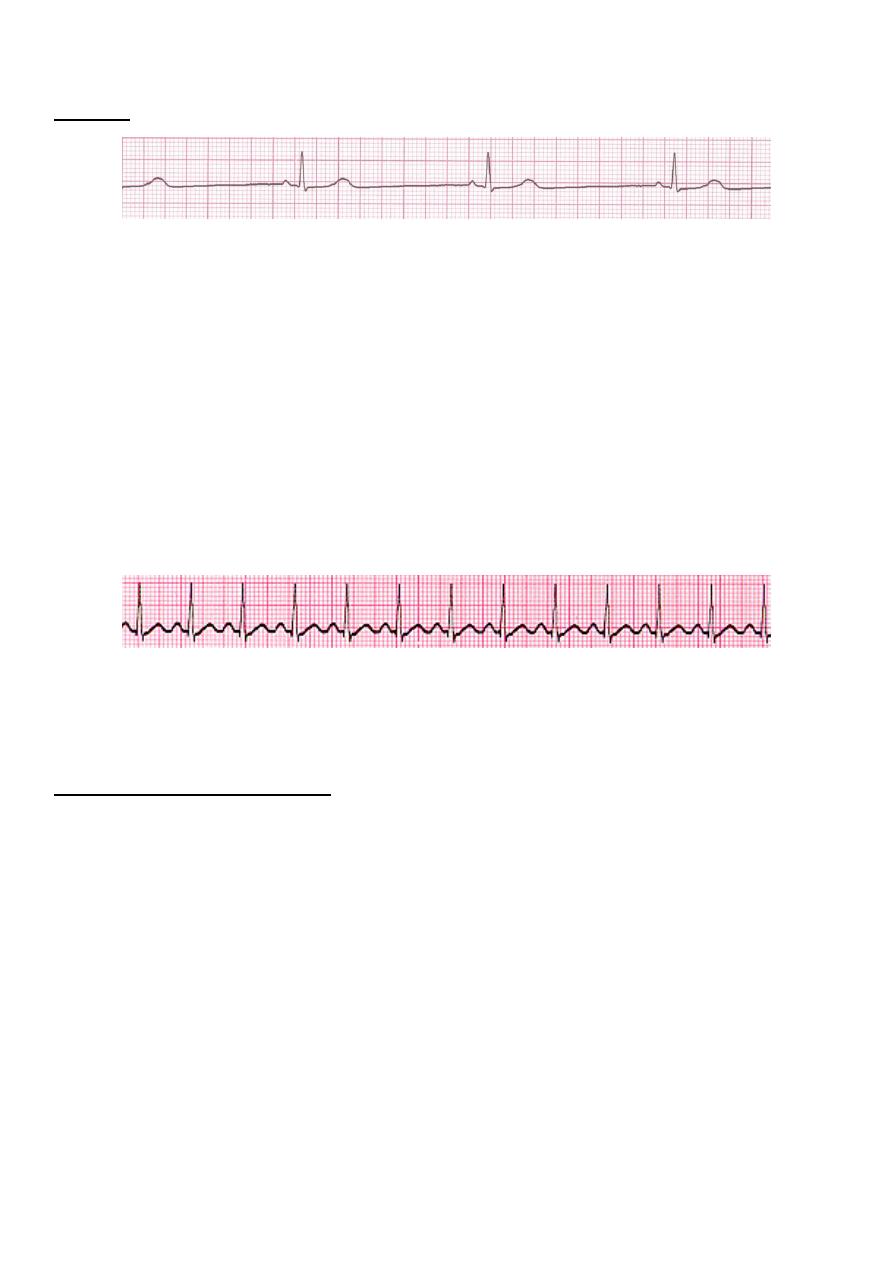
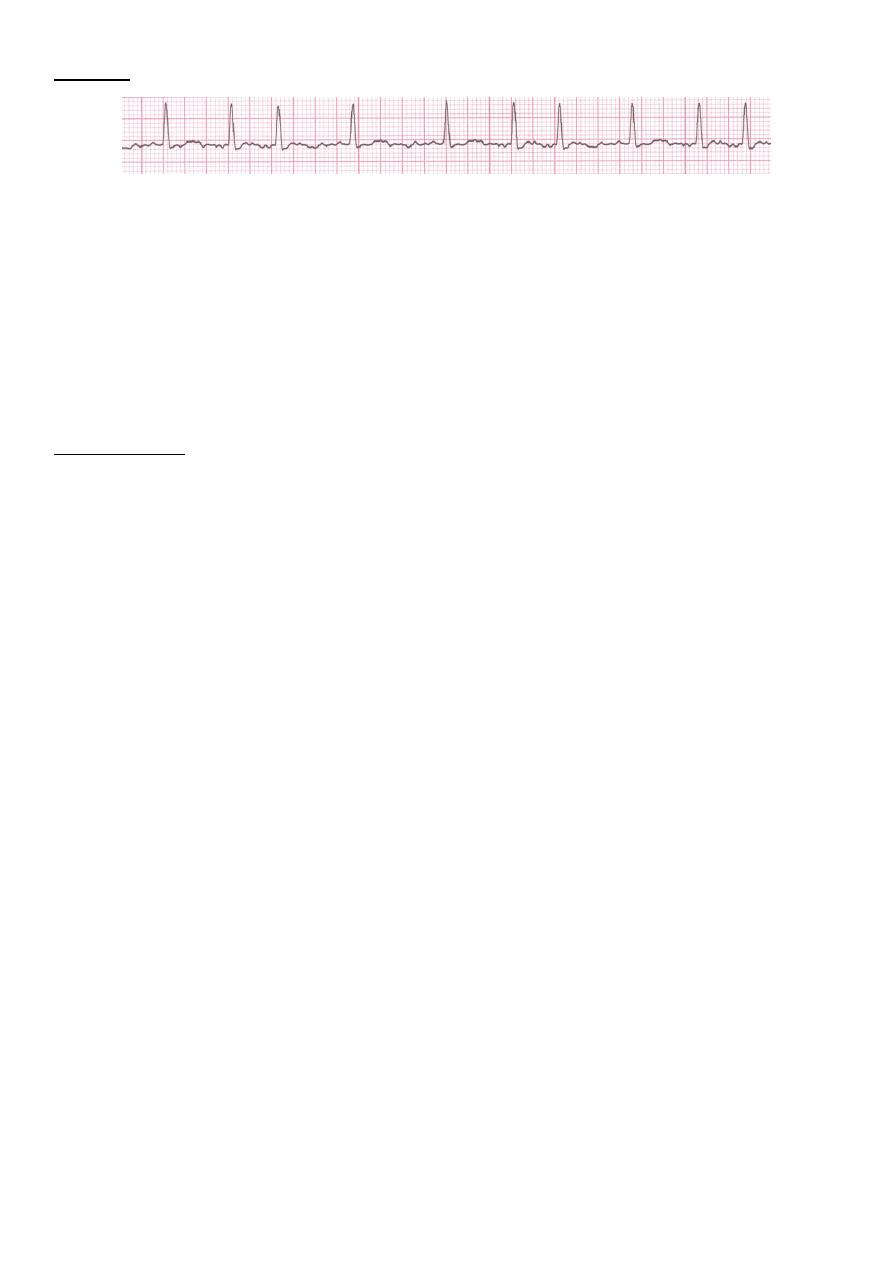
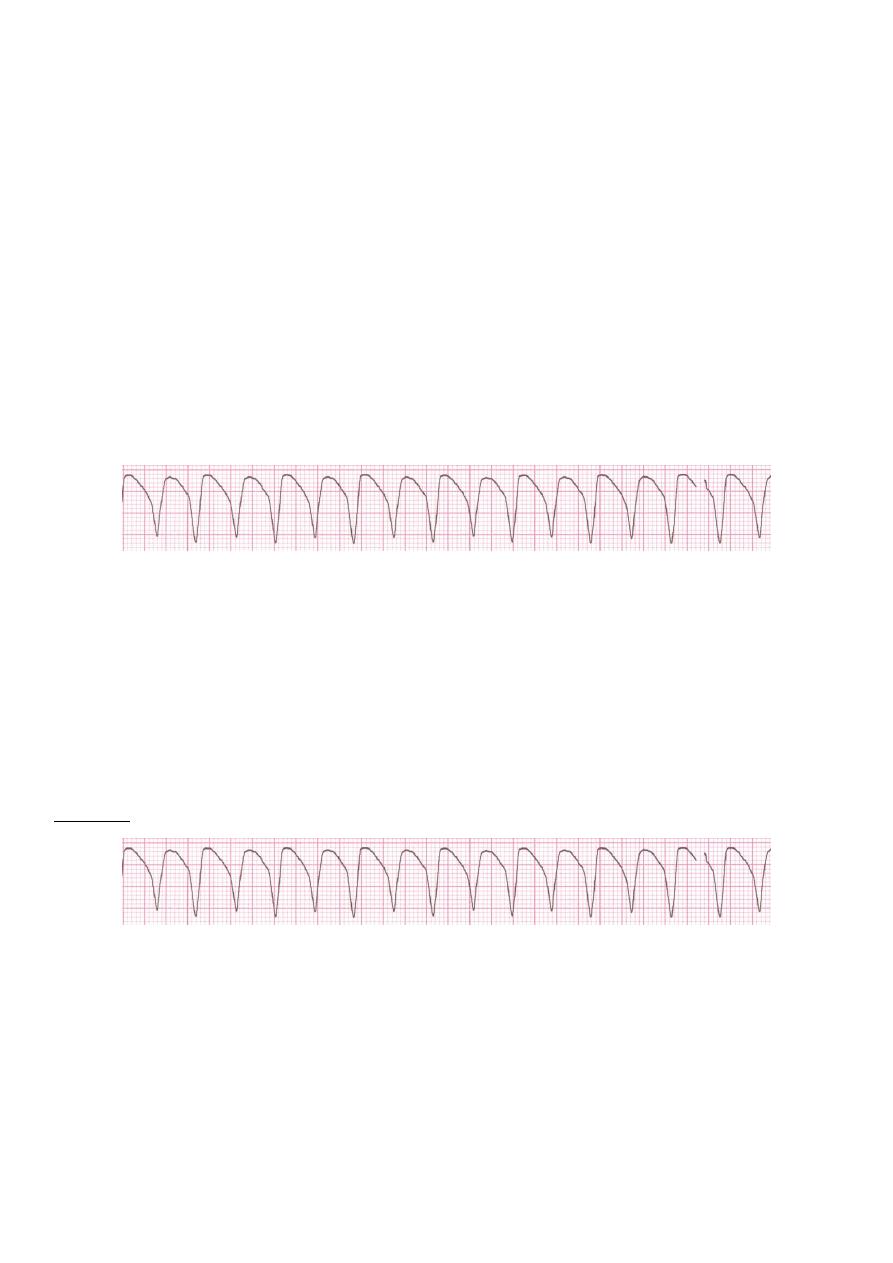
Rhythm
Rate? 130 bpm
Regularity? regular
P waves? normal
PR interval? 0.16 s
QRS duration? 0.08 s
Interpretation? Sinus Tachycardia
Sinus arrhythmia
• Phasic alteration of the heart rate during respiration (the sinus rate increases during
inspiration and slows during expiration
4
2. Premature Beats
Premature Atrial Contractions
(PACs)
Premature Ventricular Contractions (PVCs)
Premature Atrial Contractions
• Deviation from NSR
– These ectopic beats originate in the atria (but not in the SA node), therefore
the contour of the P wave, the PR interval, and the timing are different than a
normally generated pulse from the SA node.
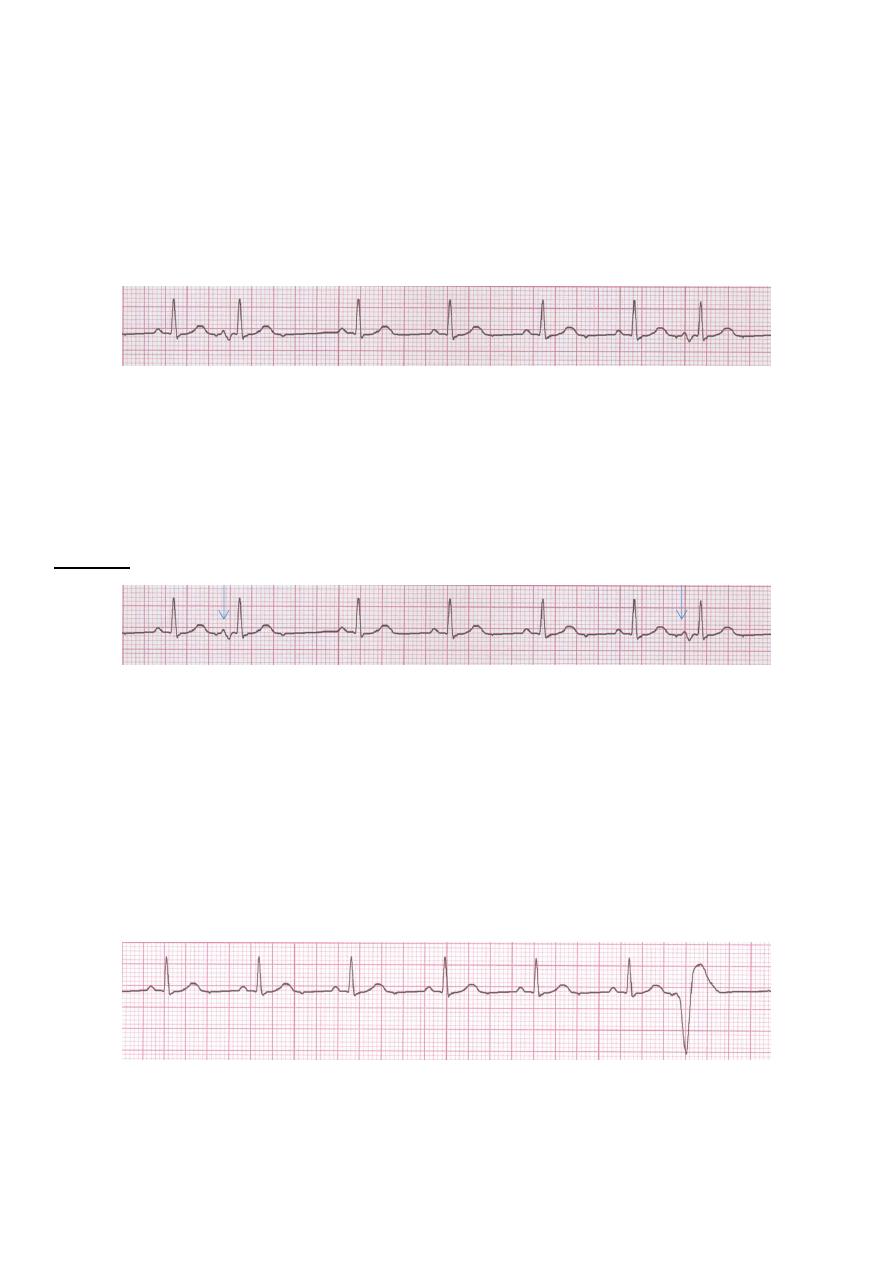
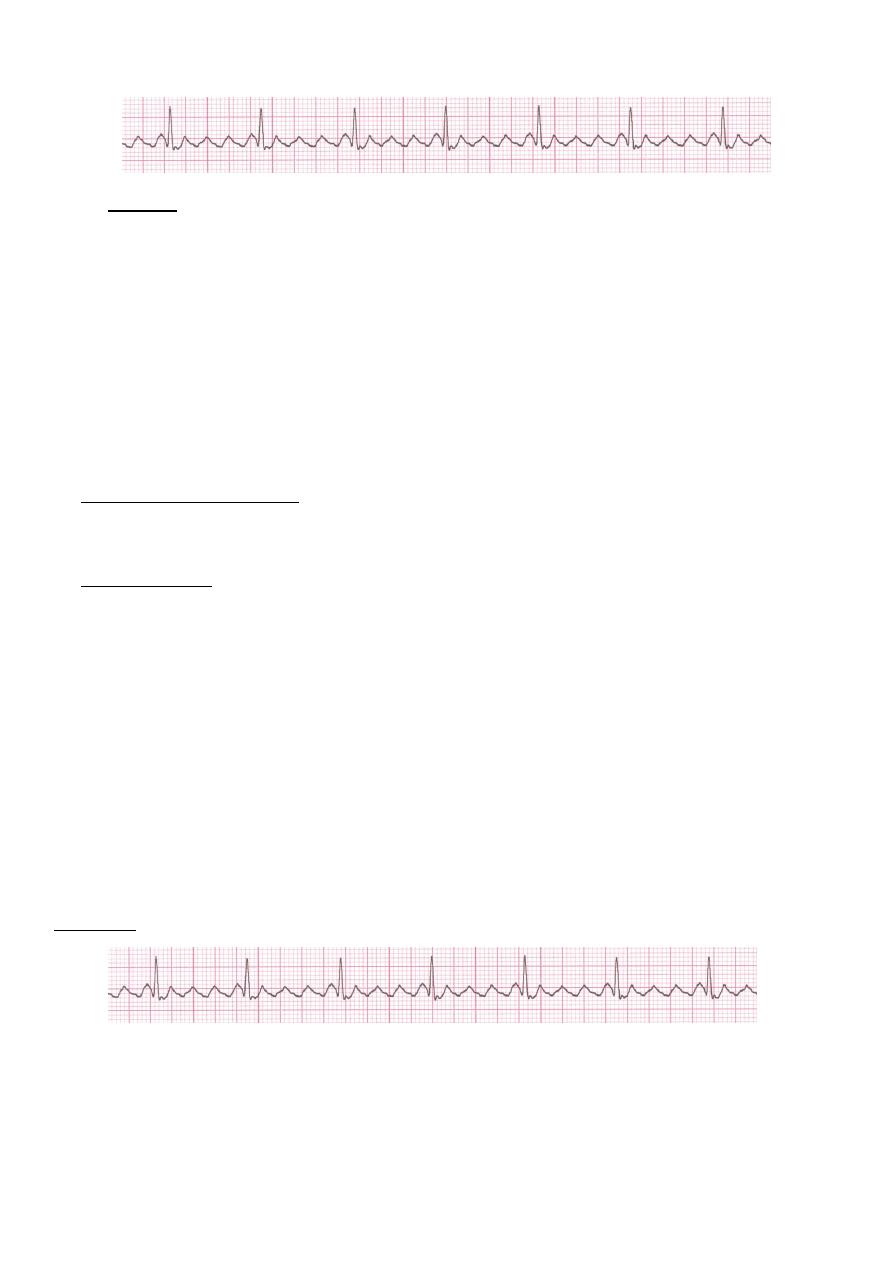
Rhythm
Rate? 70 bpm
Regularity? occasionally irreg
P waves? 2/7 different contour
PR interval? 0.14 s (except 2/7)
QRS duration? 0.08 s
Interpretation? NSR with Premature Atrial Contractions
Premature Ventricular Contractions PVCs
• Deviation from NSR
– Ectopic beats originate in the ventricles resulting in wide and bizarre QRS
complexes.
5
– When there are more than 1 premature beats and look alike, they are called
“uniform”. When they look different, they are called “multiform”
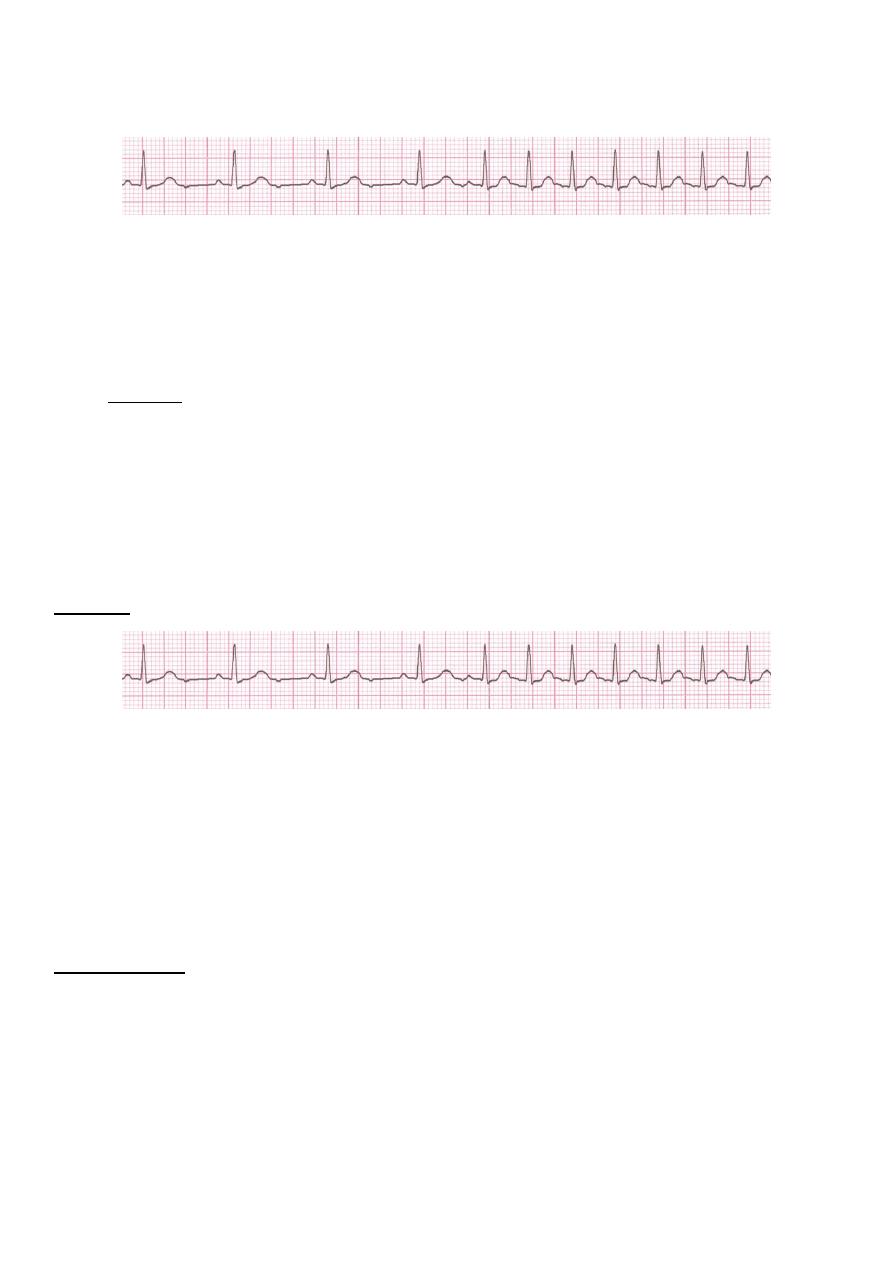
Rhythm
Rate? 60 bpm
Regularity? occasionally irreg
P waves? none for 7th QRS
PR interval? 0.14 s
QRS duration? 0.08 s (7th wide)
Interpretation? Sinus Rhythm with 1 PVC
3. Supraventricular Arrhythmias
Atrial Fibrillation
Atrial Flutter
Paroxysmal Supraventricular Tachycardia
Atrial Fibrillation
The most common sustained cardiac arrhythmia.
AF can cause palpitation, breathlessness and fatigue. In patients with poor
ventricular function or valve disease, it may precipitate or aggravate cardiac failure.
AF is associated with significant morbidity ( Thromboembolic )and a twofold increase
in mortality .
AF can be classified as paroxysmal (intermittent episodes which self-terminate within
7 days), persistent (prolonged episodes that can be terminated by electrical or
chemical cardioversion) or permanent.
6
Common causes of atrial fibrillation
Coronary artery disease (including acute MI)
Valvular heart disease, especially rheumatic mitral valve disease
Hypertension
Sinoatrial disease
Hyperthyroidism
Alcohol • Cardiomyopathy
Congenital heart disease
Chest infection
Pulmonary embolism
Pericardial disease
Idiopathic (lone atrial fibrillation)
• Deviation from NSR
– No organized atrial depolarization, so no normal P waves (impulses are not
originating from the sinus node).
– Atrial activity is chaotic (resulting in an irregularly irregular rate).
– Common, affects 2-4%, up to 5-10% if > 80 years old
• Etiology: Recent theories suggest that it is due to multiple re-entrant wavelets
conducted between the R & L atria. Either way, impulses are formed in a totally
unpredictable fashion. The AV node allows some of the impulses to pass through at
variable intervals (so rhythm is irregularly irregular).
7
Rhythm
Rate? 100 bpm
Regularity? irregularly irregular
P waves? none
PR interval? none
QRS duration? 0.06 s
Interpretation? Atrial Fibrillation
Management
Full history, physical examination, 12-lead ECG, echocardiogram and thyroid function
tests.
Restoration of sinus rhythm (Rhythm control),
Optimisation of the heart rate (Rate control)
Prevention of recurrent AF,
Reduction of the risk of thromboembolism,
Treatment of underlying cardiac disease
Rhythm control
Pharmacologic cardioversion Flecainide ,Propafenon,Amiodaron
Electrical cardioversion
• Less than 48 hours direct cardioversion.
• More than 48 hours +Anticoagulates for 4 weeks prior and 3 months
after.
Rate control
Using Digoxin, β-blockers and calcium antagonists, such as verapamil or
diltiazem
Catheter ablation in refractory case
Prevention of thromboembolism
Risk stratification is based on clinical factors using the CHA2DS2-VASc scoring
system.
Warfarin INR 2-3
Aspirin
8
Atrial Flutter
Etiology: a large (macro) re-entry circuit, usually within the right atrium encircling the
tricuspid annulus with every 2nd, 3rd or 4th impulse generating a QRS (others are
blocked in the AV node as the node repolarizes).
Deviation from NSR
No P waves. Instead flutter waves (note “sawtooth” pattern) are formed at a
rate of 250 - 350 bpm.
Only some impulses conduct through the AV node (usually every other
impulse)
Causes and Symptoms
Similar to atrial fibrillation
Management
Treat the cause
Rate control -Digoxine B blocker,verapamil.
Rhythm control –Amiodaron ,DC
Maintanance B- Blocker or amiodarone
Anticoagulant
Catheter ablation offers a 90% chance of complete cure and is the treatment of
choice for patients with persistent symptoms
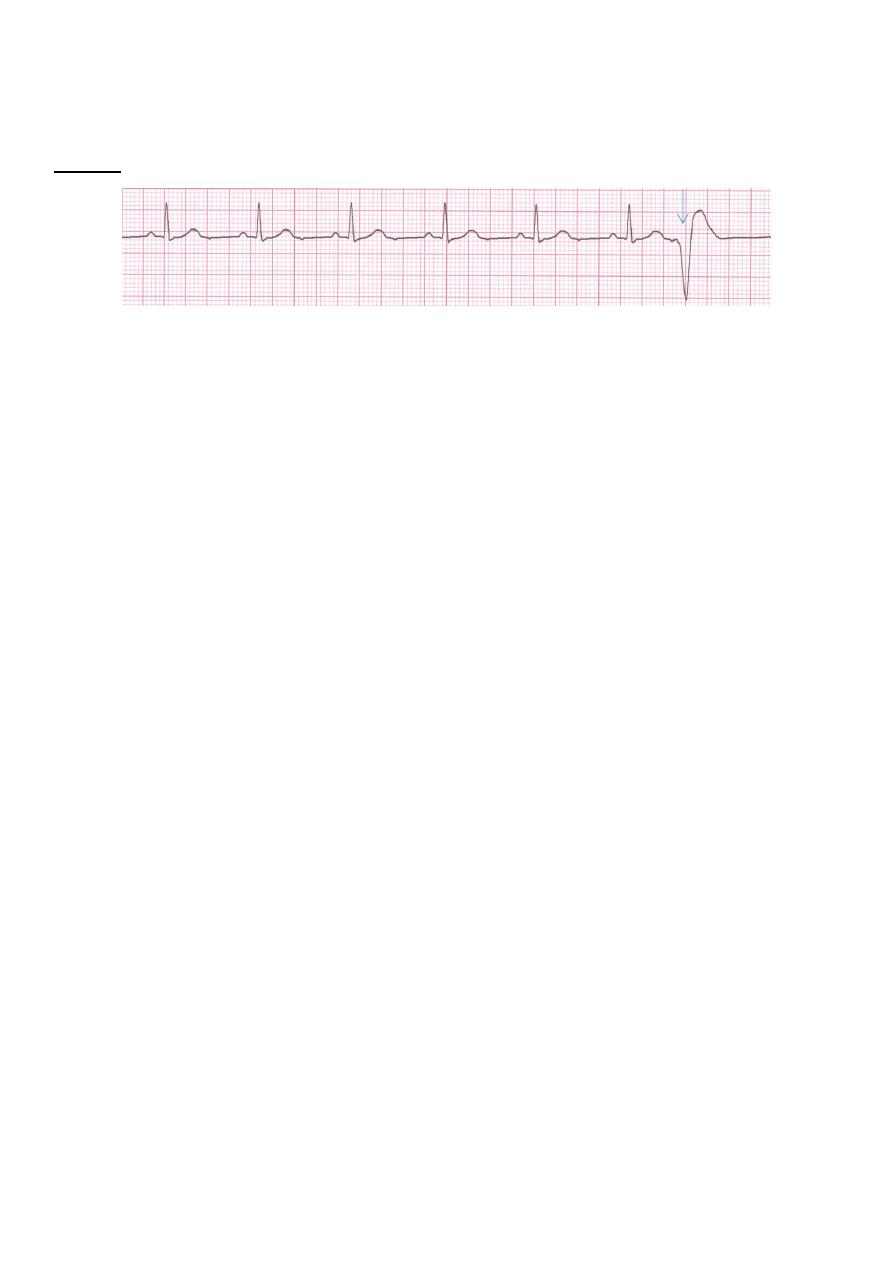
m
hyth
R
Rate? 70 bpm
Regularity? regular
P waves? flutter waves
PR interval? none
QRS duration? 0.06 s
Interpretation? Atrial Flutter
9
Paroxysmal Supraventricular Tachycardia (PSVTPSVT)
Deviation from NSR
The heart rate suddenly speeds up, often triggered by a PAC (not seen here)
and the P waves are lost.
Tends to occur in normal heart.
Etiology: There are several types of PSVT but all originate above the ventricles
(therefore the QRS is narrow).
Most common: abnormal conduction in the AV node (reentrant circuit looping in the
AV node).
Rate 150-250
Rhythm
Rate? 74 148 bpm
Regularity? Regular regular
P waves? Normal none
PR interval? 0.16 s none
QRS duration? 0.08 s
Interpretation? Paroxysmal Supraventricular
Management
Episode may be terminated by carotid sinus pressure or by the Valsalva manœuvre.
Adenosine (3–12 mg rapidly IV in incremental doses until tachycardia stops) or
verapamil (5 mg IV)
Recurrent SVT, catheter ablation is the most effective therapy and will permanently
prevent SVT in more than 90% of cases
10
4. Ventricular Arrhythmias
Ventricular Tachycardia
Ventricular Fibrillation
Ventricular Tachycardia
Dangerous.
Nearly in abnormal heart.
3 or more sucsussive PVC at rate of more than 120.
Can occur in normal heart.
Deviation from NSR
Impulse is originating in the ventricles (no P waves, wide QRS).
Etiology: There is a re-entrant pathway looping in a ventricle (most common cause).
Ventricular tachycardia (VT) occurs most commonly in the settings of acute MI,
chronic coronary artery disease, and cardiomyopathy.
Rhythm
Rate? 160 bpm
Regularity? regular
P waves? none
PR interval? none
QRS duration? wide (> 0.12 sec)
Interpretation? Ventricular Tachycardia
11
Management
Treat cause.
Hemodynamically unstable DC
Stable IV amiodarone or lidocaine.
With poor LV function indication for ICD
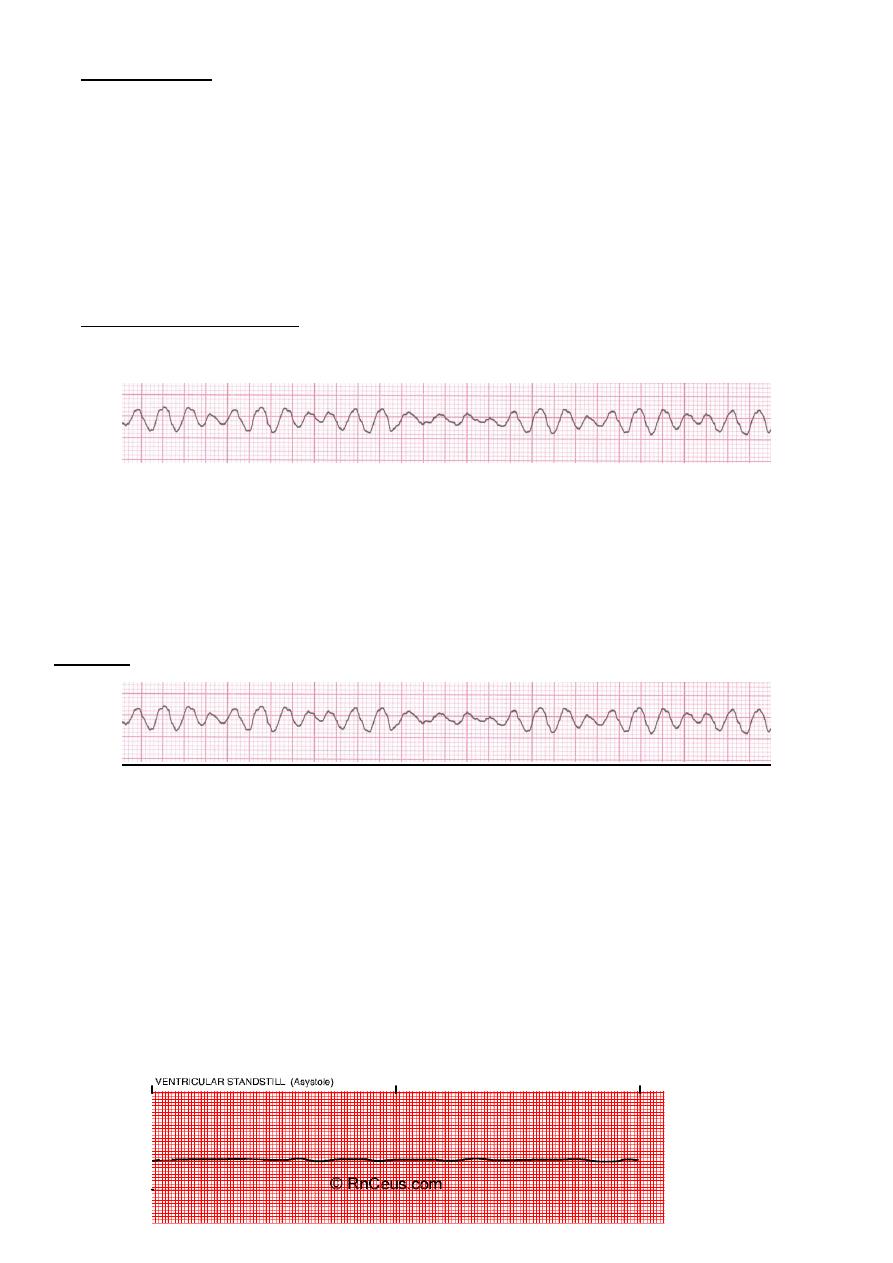
Ventricular Fibrillation
CARDIAC ARREST
Deviation from NSR : Completely abnormal
Etiology: The ventricular cells are excitable and depolarizing randomly.
Rapid drop in cardiac output and death occurs if not quickly reversed
Rhythm
Rate? none
Regularity? irregularly irreg.
P waves? none
PR interval? none
QRS duration
wide, if recognizable
Interpretation? Ventricular Fibrillation
Asystole
12
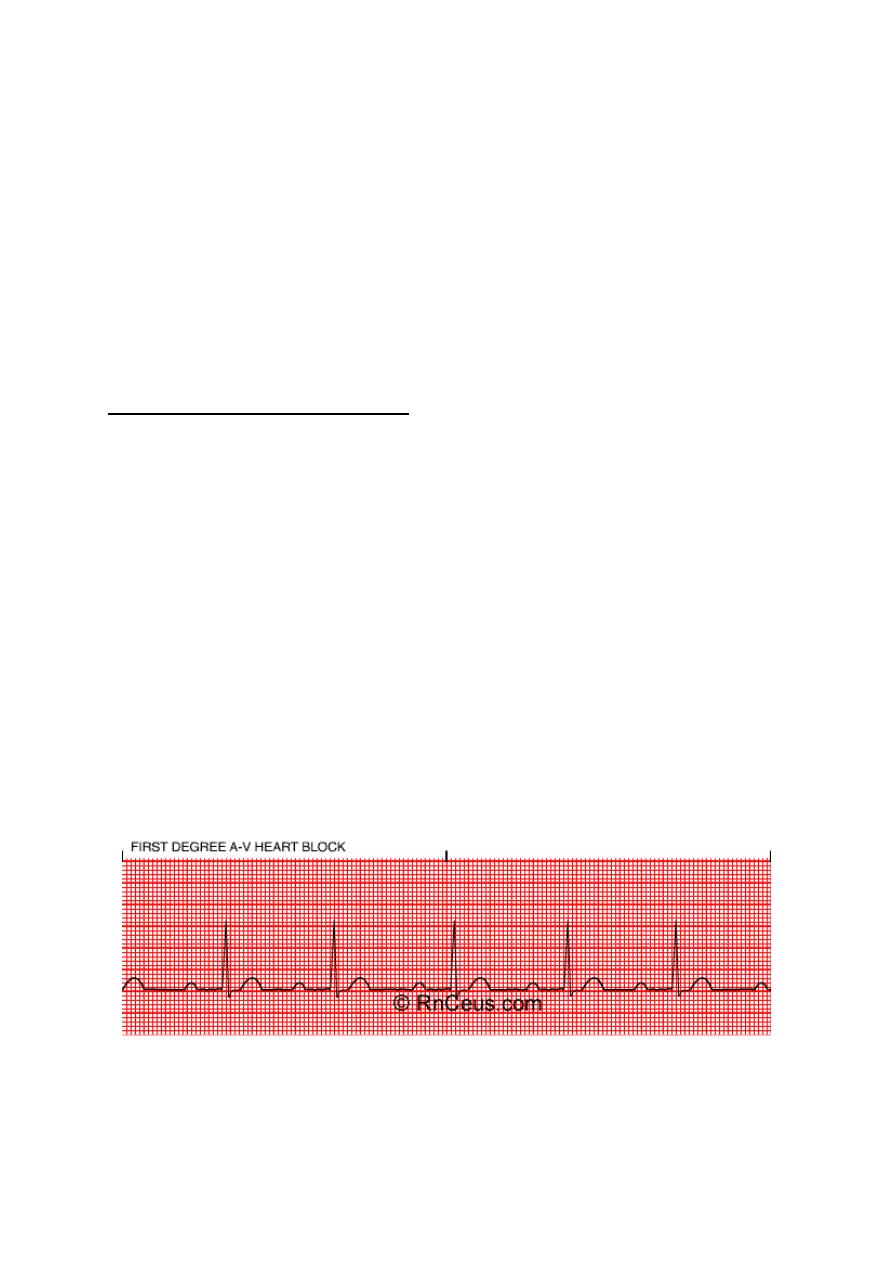
5. FIRST DEGREE A-V HEART BLOCK
• Rate: variable
• P wave: normal
• QRS: normal
• Conduction: impulse originates in the SA node but has prolonged conduction in the
AV junction; P-R interval is > 0.20 seconds.
• Rhythm: regular
• This is the most common conduction disturbance. It occurs in both healthy and
diseased hearts.
• First degree AV block can be due to:
inferior MI,
digitalis toxicity
hyperkalemia
increased vagal tone
acute rheumatic fever
myocarditis.
• Interventions include treating the underlying cause and observing for progression to
a more advanced AV block.
13
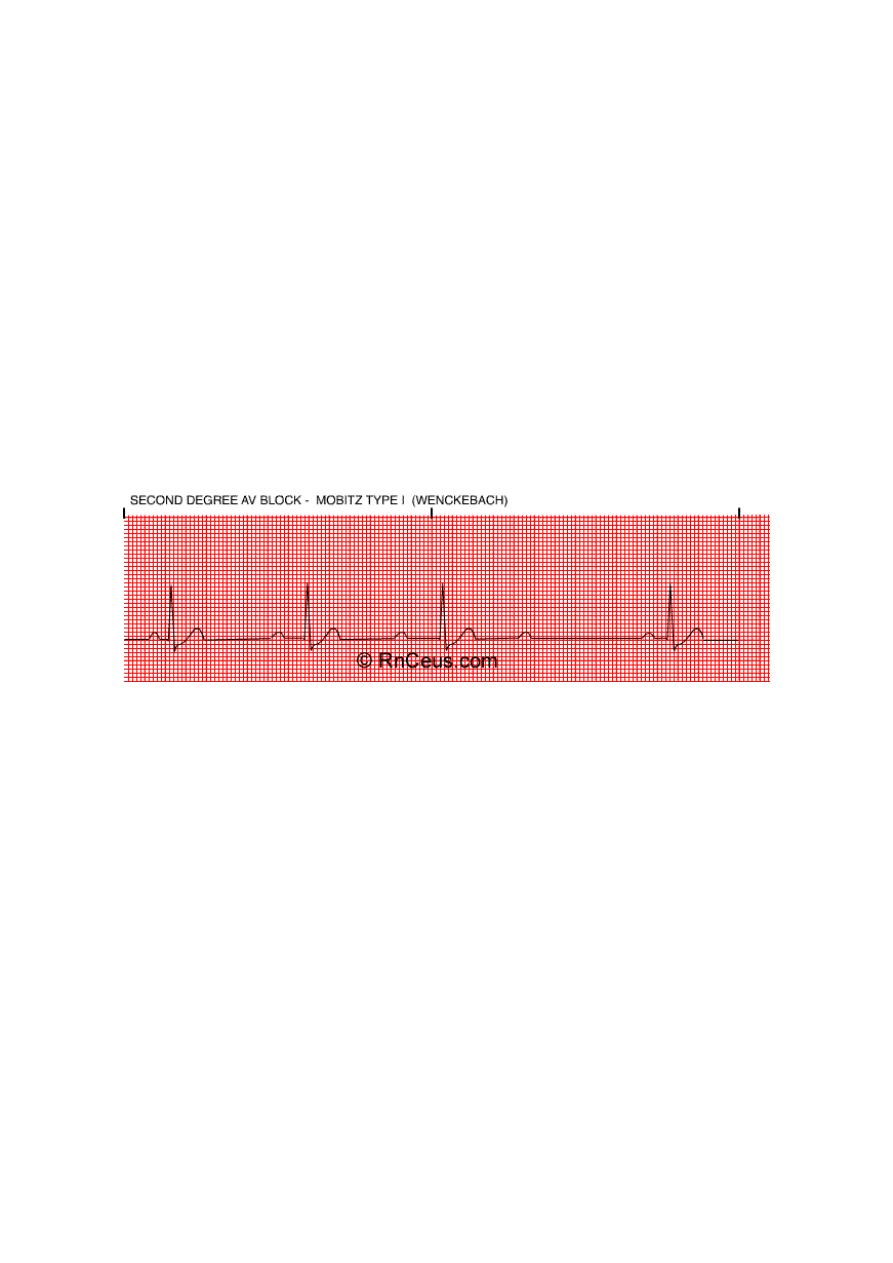
SECOND DEGREE A-V BLOCK MOBITZ TYPE I (WENCKEBACK)
Rate: variable
P wave: normal morphology with constant P-P interval
QRS: normal
Conduction: the P-R interval is progressively longer until one P wave is blocked; the
cycle begins again following the blocked P wave.
Rhythm: irregular
Second degree AV block type I occurs in the AV node above the Bundle of His.
It is often transient and may be due to acute inferior MI or digitalis toxicity.
Treatment is usually not indicated as this rhythm usually produces no symptoms.
SECOND DEGREE A-V BLOCK MOBITZ TYPE II
Rate: variable
P wave: normal with constant P-P intervals
QRS: usually widened because this is usually associated with a bundle branch block.
Conduction: P-R interval may be normal or prolonged, but it is constant until one P
wave is not conducted to the ventricles.
Rhythm: usually regular when AV conduction ratios are constant
This block usually occurs below the Bundle of His and may progress into a higher
degree block.
It can occur after an acute anterior MI due to damage in the bifurcation or the bundle
branches.
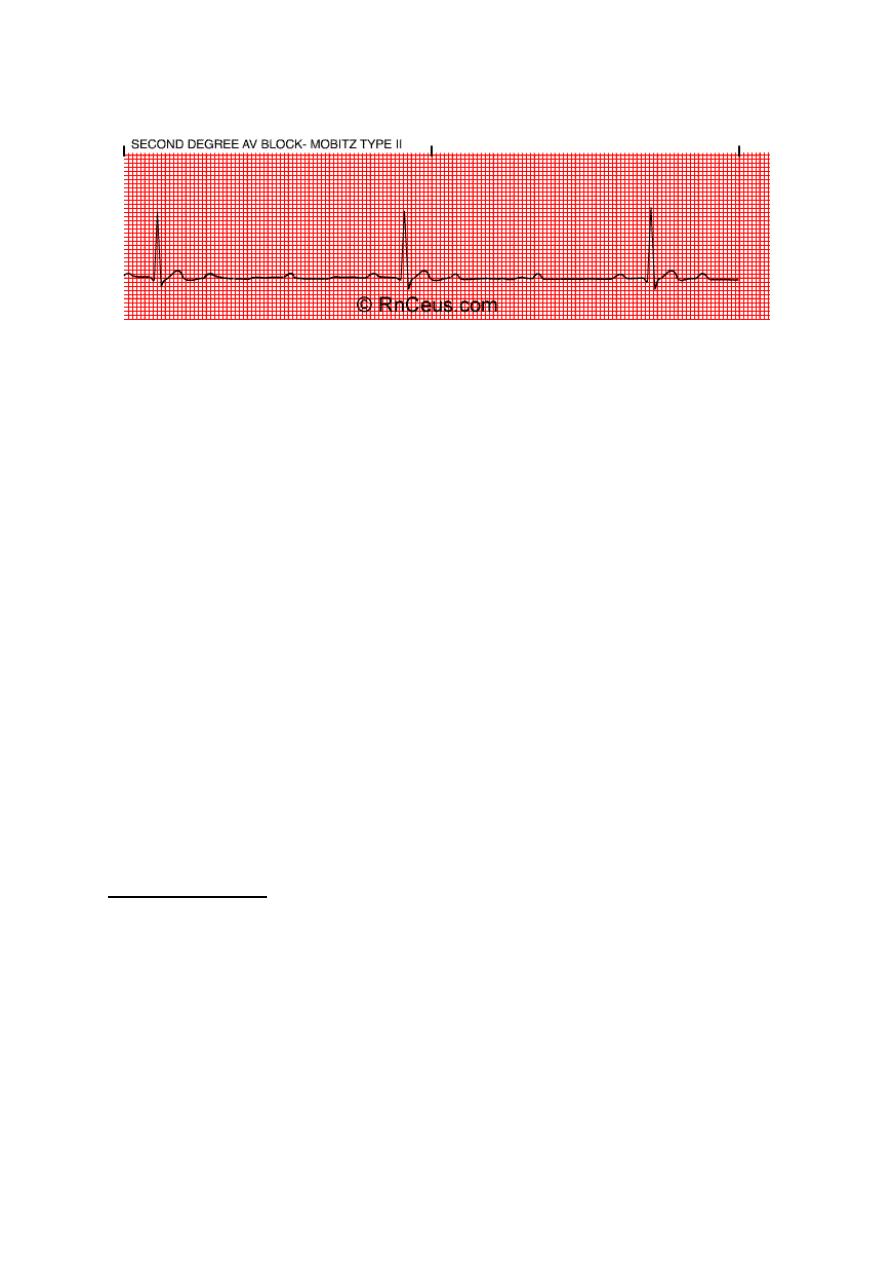
14
It is more serious than the type I block.
Treatment is usually artificial pacing.
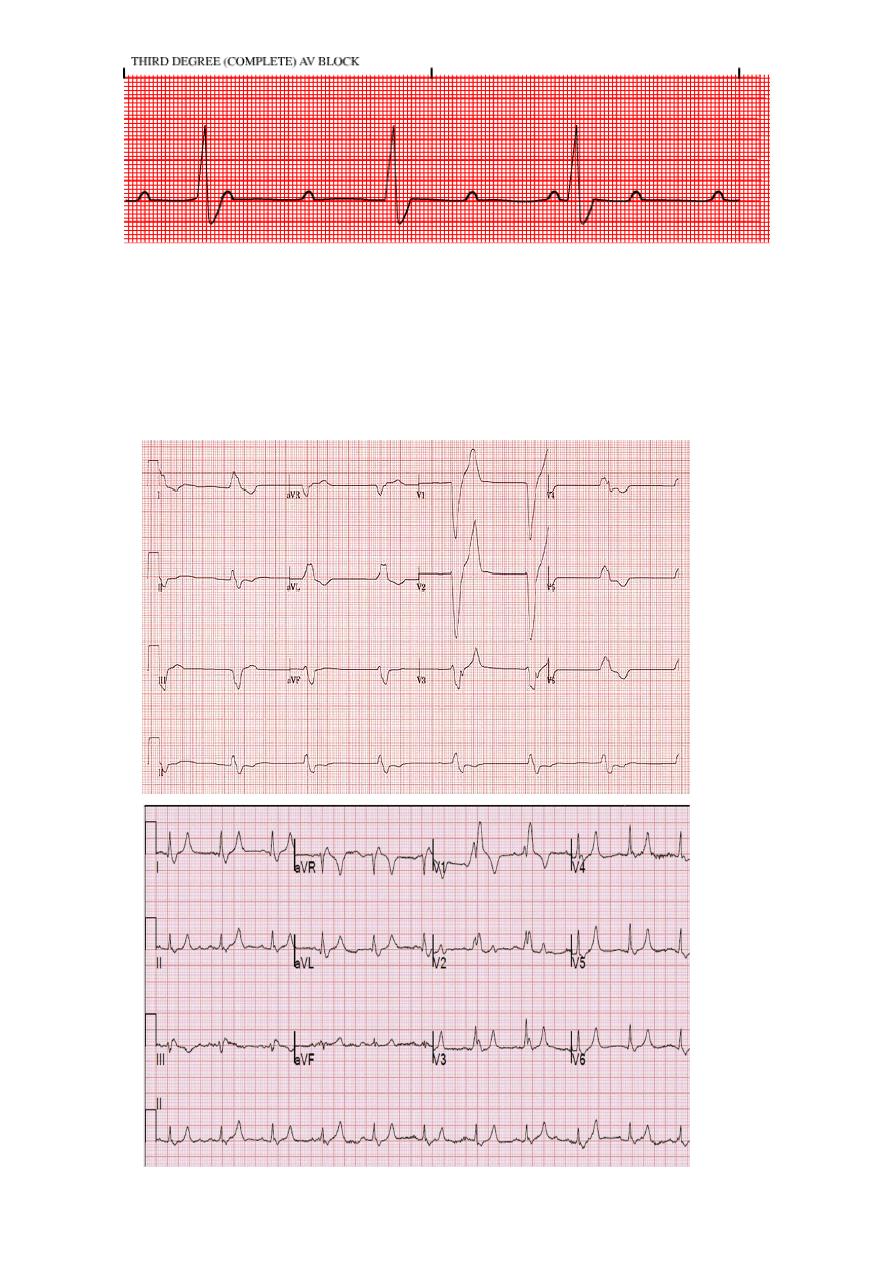
THIRD DEGREE (COMPLETE) A-V BLOCK
• Rate: atrial rate is usually normal; ventricular rate is usually less than 70/bpm. The
atrial rate is always faster than the ventricular rate.
• P wave: normal with constant P-P intervals, but not "married" to the QRS complexes.
• QRS: may be normal or widened depending on where the escape pacemaker is
located in the conduction system
• Conduction: atrial and ventricular activities are unrelated due to the complete
blocking of the atrial impulses to the ventricles.
• Rhythm: irregular
• Complete block of the atrial impulses occurs at the A-V junction, common bundle or
bilateral bundle branches.
• Another pacemaker distal to the block takes over in order to activate the ventricles
or ventricular standstill will occur.
• May be caused by:
digitalis toxicity
acute infection
MI and
degeneration of the conductive tissue.
• Treatment modalities include:
external pacing and atropine for acute, symptomatic episodes and
permanent pacing for chronic complete heart block.
15
Bundle branch block and hemiblock
• Left bundle branch block LBBB
• Right bundle branch block RBBB
