1
Forth stage
Medicine
(C.V.S)
Lec-6
د.جاسم محمد
2311/2015
Infective endocarditis
Definitions, general information:
Microbial infection of a heart valve (native or prosthetic ) or endothelial lining of the
heart or blood vessels or congenital defect. Commonly caused by bacteria, rarely by
other like fungi.
Most often involving aortic and mitral valves
3-10/100 000/year
Median age has increased from 30-40 to 47-69 yrs.
More common in women
The viridans group of streptococci is the most common pathogen in developing
countries
Staphylococcus aureus is the most common pathogen in developed countries.
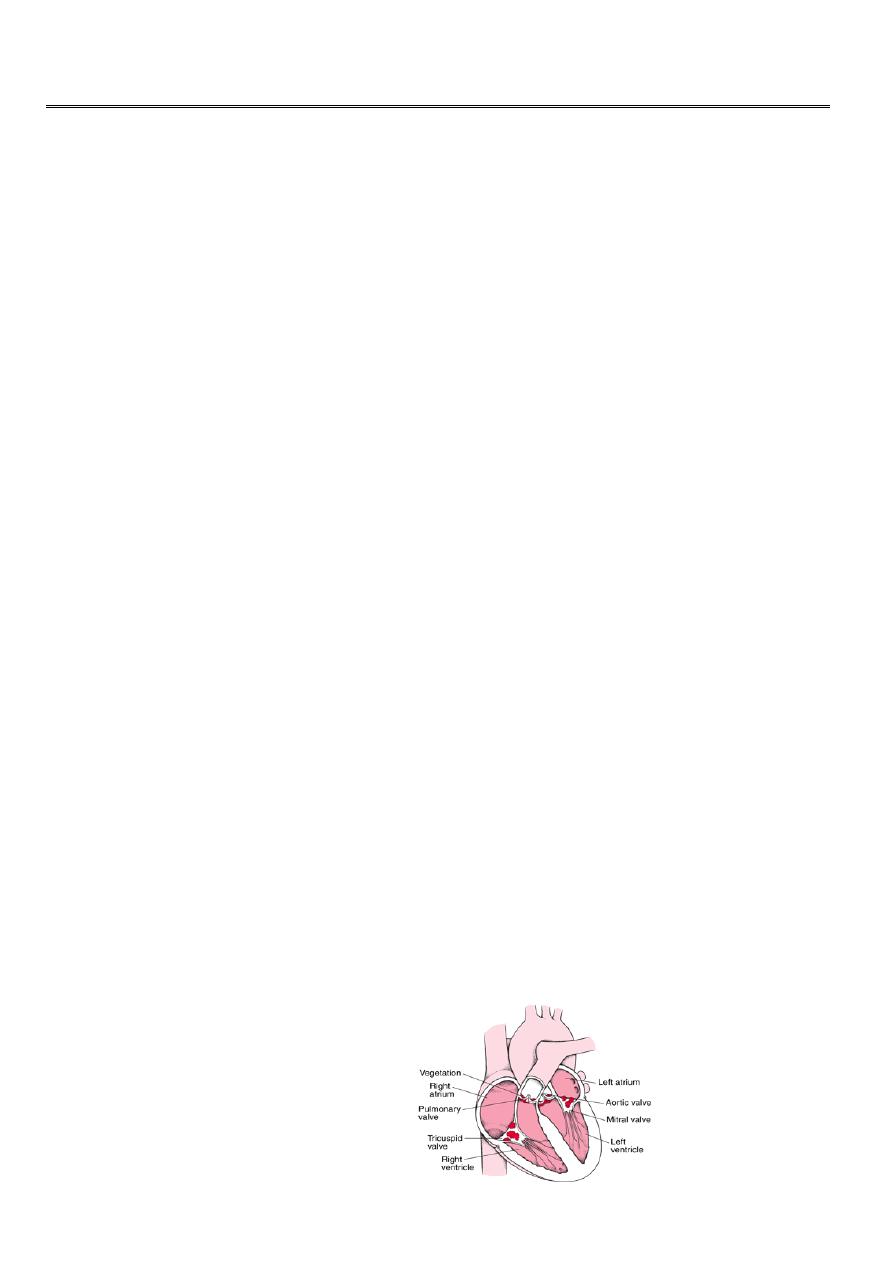
Pathophysiology:
Typically occur on preexisting endocardial damage(high jet pressure like VSD ,AR,MR)
That attract the fibrin and platlets accumulation which favour colonization of blood
borne bacteria – VEGITATIONS
As infection established Veg. enlarge or causing destruction or extension –Abscess
Extracardiac manifestations due to Emboli (Emboli can break off vegetations causing
abscesses at distant sites) or Immune complex depositions
More common lesions now:
Mitral valve prolapse
Degenerative calcific valvular stenosis
Bicuspid aortic valve
Prosthetic valves
Congenital defects
2
Microbiology
The viridans group of streptococci (Streptococcus mitis, Strep. sanguis) are commensals
in the upper respiratory tract that may enter the blood stream on chewing or teeth-
brushing, or at the time of dental treatment, Others including Enterococcus faecalis,.
And Strep. bovis, may enter the blood from the bowel or urinary tract. Staph. aureus has
now overtaken streptococci as the most common cause of acute endocarditis
Other like Coxiella burnetii, HACEK,Brucella ,fungi.
Clinical symptoms – when to suspect Subacute endocarditis
This should be suspected when a patient with congenital or valvular heart disease
develops a persistent fever.
Unusual tiredness, night sweats or weight loss, or develops new signs of valve
dysfunction or heart failure.
Less often, it presents as an embolic stroke or peripheral arterial embolism.
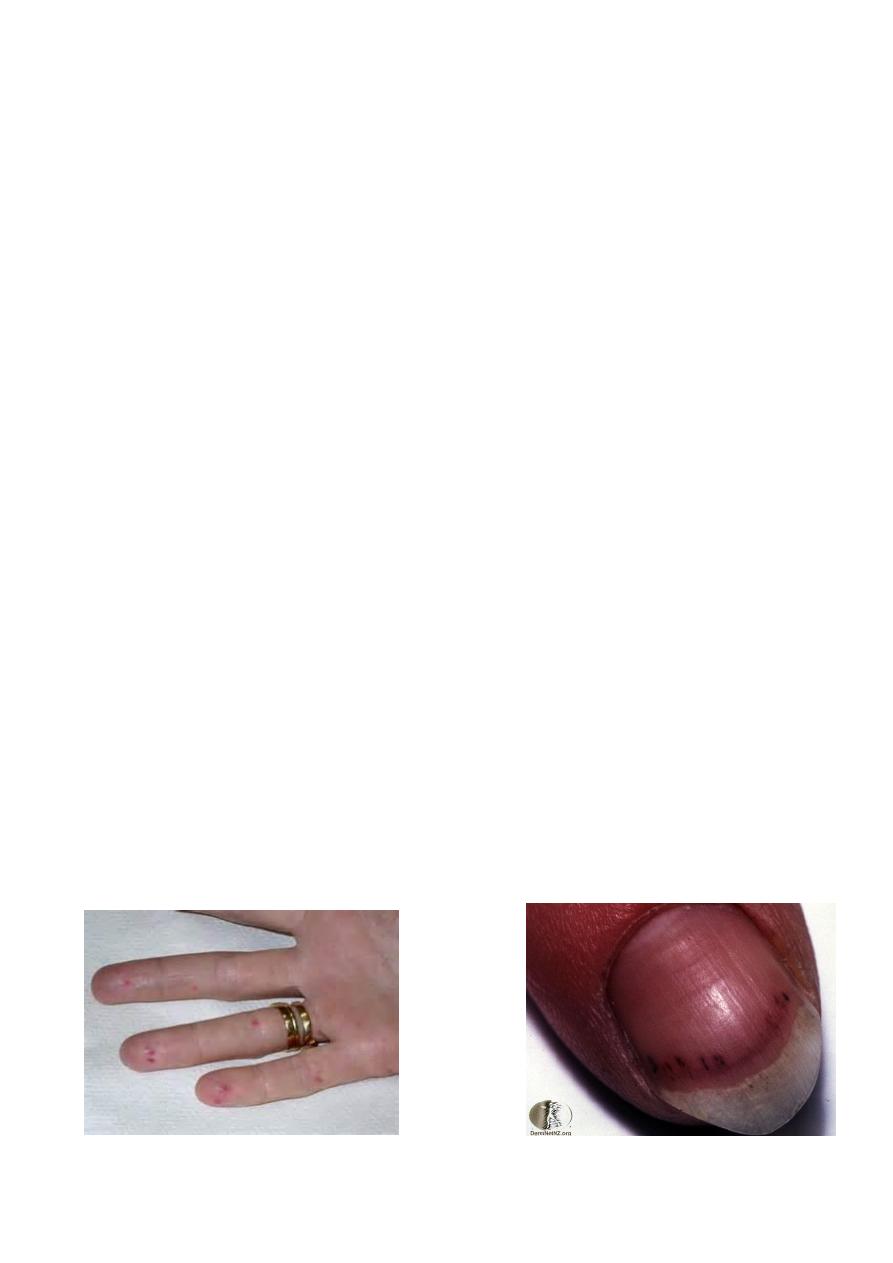
Other features include purpura and petechial haemorrhages in the skin and mucous
membranes, and splinter haemorrhages under the fingernails or toe nails. Osler’s nodes
are painful tender swellings at the fingertips that are probably the product of vasculitis;
they are rare. Digital clubbing is a late sign.
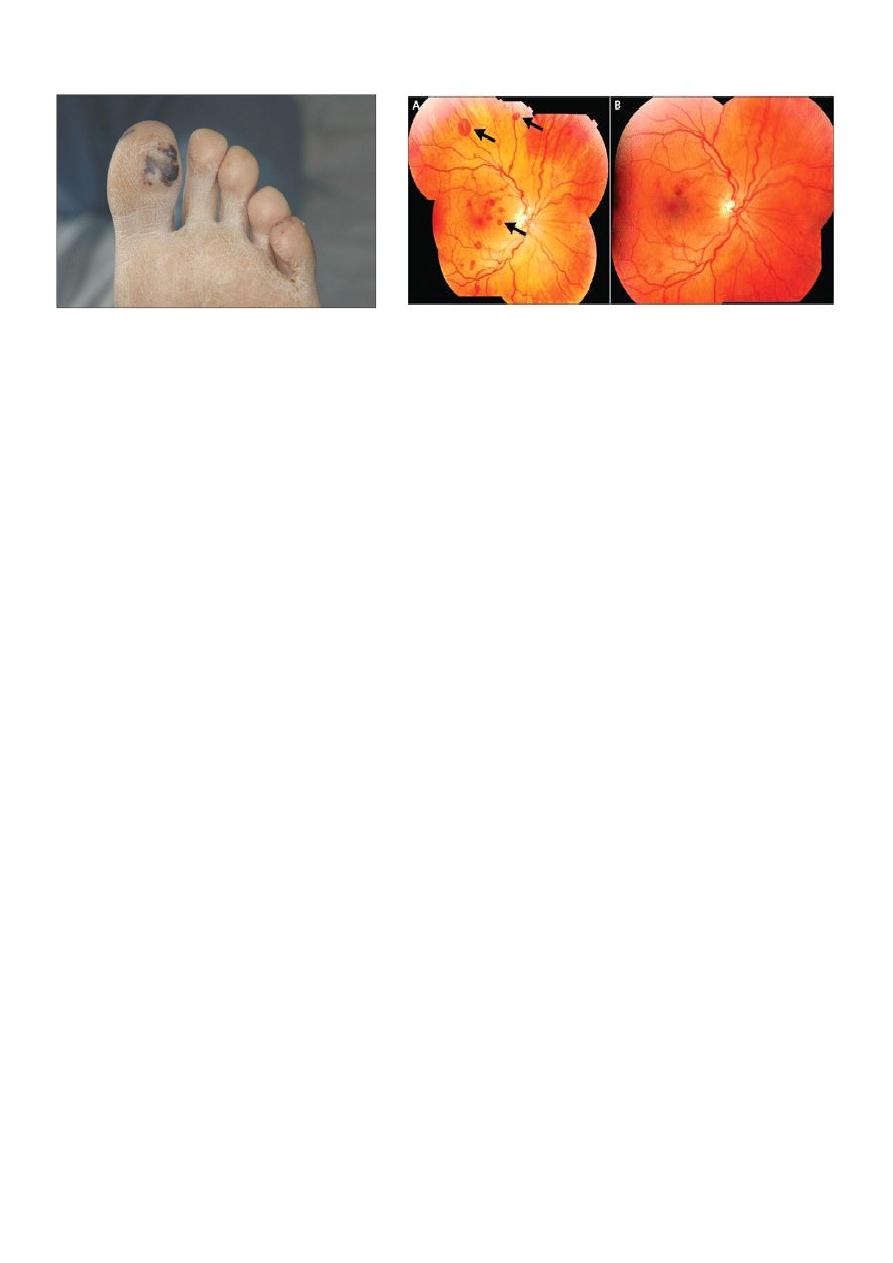
Roth spots, glomerulonephritis – up to 30% of patients
The spleen is frequently palpable
Osler Nodes Splinter Hemorrhage
3
Janeway Lesions Roth Spots
Acute endocarditis This presents as a severe febrile illness with prominent and changing
heart murmurs and petechiae
Embolic events are common, and cardiac or renal failure may develop rapidly.
Diagnosis
Duke criteria
Major criteria Minor criteria
1. Blood culture positive for typical
IE-causing microorganism
2. Evidence of endocardial involvement
Diagnosis
• 2 major criteria
or
• 1 major and 3 minor
or
• 5 minor criteria
Blood cultures
• Always before starting antibiotics.
• Always triple samples – aerobe, anaerobe and mycotic , 10 ml each.
• Three sets of samples required.
1. Predisposition heart condition or i.v. drug abuse
2. Fever – temp. >38 °C
3. Vascular phenomena – arterial emboli etc.
4. Immunologic phenomena – glomerulonephritis,
Osler’s nodes, Roth’s spots
5. Microbiological evidence – positive blood
cultures
but do not meet major criteria

4
Echocardiography
Transthoracic (TTE) and transoesophageal (TEE).
Echocardiography is key for detecting and following the progress of vegetations, for
assessing valve damage and for detecting abscess formation
.
Other investigations
Elevation of the ESR, a normocytic normochromic anemia, and leukocytosis are common
The ECG may show the development of AV block.
The chest X-ray may show evidence of cardiac failure and cardiomegaly
GUE Hematuria
Treatment basics
Success relies on eradication of pathogen
Bactericidal regiment should be used
Drug choice due to pathogen
Surgery is used mainly to cope with structural complications
A multidisciplinary approach, with cooperation between the physician, surgeon and
microbiologist.
Empirical treatment depends on the mode of presentation, the suspected organism, and
whether the patient has a prosthetic valve or penicillin allergy
If the presentation is acute, flucloxacillin and gentamicin are recommended, while for a
subacute or indolent presentation, benzyl penicillin and gentamicin are preferred
Those with penicillin allergy, a prosthetic valve or suspected meticillin-resistant Staph.
aureus (MRSA) infection, triple therapy with vancomycin, gentamicin and oral
rifampicin should be considered
SURGERY indicated :
Heart failure due to valve damage
Failure of antibiotic therapy (persistent/uncontrolled infection)
Large vegetations on left-sided heart valves with evidence or ‘high risk’ of systemic
emboli
Abscess formation

5
Complications
1. Congestive heart failure
• Most common complication
• Main indication to surgical treatment
• ~60% of IE patients
2. Uncontrolled infection
• Persisting infection
• Perivalvular extension in infective endocarditis
3. Systemic embolism
• Brain, spleen and lungs
• 30% of IE patients
• May be the first symptom
4. Neurologic events
5. Acute renal failure
6. Rheumatic problems
7. Myocarditis
Prophylaxis
• First and most important – proper oral hygiene
• Regular dental review
•
Antibiotics only in high-risk group patients
1. Prosthetic valve or foreign material used for heart repair.
2. History of IE
3. Congenital heart disease
• Cyanotic without correction or with residual lickeage
• CHD without lickage but up to 6 months after surgery
Use amoxycilin or
ampicylin
30-60 min prior to intervention
.
A.L.Y
