
1
Forth stage
Medicine (CVS)
Lec-9
Dr.Jasim
24/11/2015
Coronary Artery Disease
Atherosclerosis is the leading cause of death and disability in the developed and developing
world
Clinical manifestations depend on the particular vascular bed affected :
Coronary vasculature : angina, MI, sudden death
Cerebra l:TIA, stroke
Peripheral :claudication, gangrene
Renal : hypertension
Epidemiology
The three major clinical manifestations of atherosclerotic CVD are:
o CHD
o CVA
o PVD
Disease impact:
In 1997, more than 5mn Americans had CVD
Currently one in five American has some form of CVD
Each year 1mn deaths are due to CVD (42% of all deaths!)
One-sixth of CVD deaths are in persons <65 yrs of age
Annually
1.5mn Americans have MI
0.5mn die from CHD
0.5mn have stroke
0.15mn die from stroke
Death rates from CHD has decreased by 40% since 1968
CVD still remains the leading cause of death in developed nations
CHD & stroke are the 2nd and 3rd leading causes of mortality even in the developing
regions
2
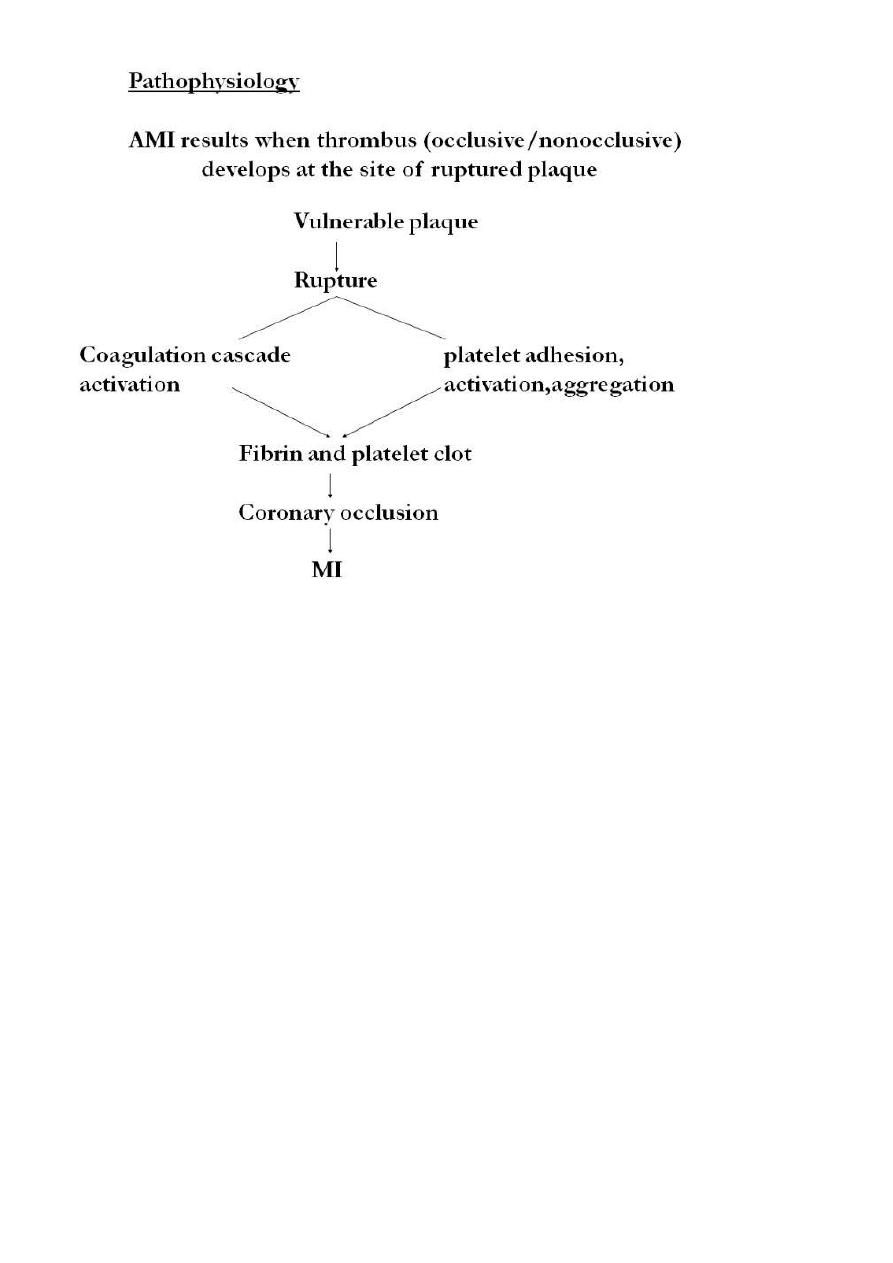
Pathophysiology
CADis almost always due Atherosclerosis
Occasionally, other such as aortitis, polyarteritis
Atherosclerosis is a progressive inflammatory disorder of the arterial wall that is
characterised by focal lipidrich deposits of atheroma.
Development of lesions, starting in childhood, progress through phases, caused by
injury to intima of artery
Phase I : fatty streaks – do not obstruct flow
Phase II: fibrous plaque- elevated lesion protruding into lumen obstructs flow to
varying degrees
Phase III: complicated lesions – partially or totally occlude lumen
Early atherosclerosis(Fatty streaks )tend to occur at sites of altered arterial shear
stress, such as bifurcations.They develop when inflammatory cells, predominantly
monocytes, bind to receptors expressed by endothelial cells, migrate into the intima,
take up oxidised low-density lipoprotein (LDL)particles and become lipid-laden
macrophages or foam cells. In response to cytokines and growth factors produced by
activated macrophages, smooth muscle cells migrate from the media of the arterial
wall into the intima, and change from a contractile to a repair phenotype in an attempt
to stabilise the atherosclerotic lesion.
Advanced lesion :
Vulnerable plaques Stable plaques
1-Thin fibrous cap 1-Thick cap
2-Large lipid core 2- Dense extracellular matrix
3-High macrophage content 3- Less lipid rich core
Concept of
“Risk factors”
for CAD evolved from prospective epidemiological studies in
US and Europe which demonstrated consistent association among characteristics observed at
one point of time in apparently healthy individuals and subsequent incidence of CAD in
these patients. But, presence of a risk factor does not necessarily imply a direct causal
relationship.
Risk factors
Non-modifiable risk factors
1. Age: death from CAD
with age
2. Sex
3. Family history
4. Race: afro-Americans have = 45% > hypertension than Caucasians

3
Modifiable Risk Factors
1. Cigarette smoking: 2X increased risk for CAD
2. HTN: damages blood vessels leading to plaque formation and atherosclerosis
3. Hyperlipidemia:
CAD and atherosclerosis by causing build up in artery walls
4. Physical Inactivity:
risk of CAD 2X
5. Diabetes:
risk 2X in men; 3X in women
6. Obesity
7. Stress : increased catecholamine release;
sympathetic response
Dyslipidemia
Better term than hyperlipidemia as it includes the risk of having low HDL.
Serum total cholesterol (TC) is a composite of:
LDL cholesterol- directly related to CVD
HDL cholesterol- inversely related to CVD
VLDL cholesterol- related to CVD in patients with DM and low HDL
Best single predictor for CVD risk is TC/HDL ratio.
Ideal ratio is <3, intermediate 3-5, high risk >5
This ratio is also the best predictor of treatment benefits
Hypertension
Potent risk factor for all CVD and dominant risk factor for stroke.
Graded relationship between level of BP and outcomes.
SBP rises with age, whereas DBP plateaus in the late middle life and decreases
somewhat then.
Trials for isolated systolic hypertension have shown benefits for both stroke and CHD
Systolic and diastolic hypertension increase the RR for CVD by 1.6 times
For combined Systolic and diastolic HTN the RR is 2.0
The risk for CVD is increased even in individuals with “high normal BP” (130-39/85-
89 mm Hg)
Smoking
This habit increases the risk of vascular outcomes by 2 fold.
Both, regular and filter cigarettes have same adverse effects.
Low tar/low nicotine products have not been shown to reduce the risk
Unlike other modifiable risk factors, cigarette smoking can be eliminated entirely
Benefits of quitting smoking are dramatic. Risk in ex-smokers falls to near non-
smoking levels in 2 yrs.
4
Obesity
It contributes independently to CVD risk and also aggravates known
CVD risk
factors.
Measures of obesity include:
1. BMI
2. Waist: hip ratio
Diabetes Mellitus
Patients with either type I or type II diabetes have increased risk for CVD
Risk of CHD is increased 2-fold in young men and 3-fold in young women with type 2
diabetes
Type II diabetics have one or more metabolic abnormalities (hypertriglyceridemia,
low HDL, hypertension)
They may also have normal LDL levels but LDL particles are dense and small thus
being more atherogenic
Spectrum of coronary artery disease
1. Silent ischemia
2. Chronic stable angina
3. Acute coronary syndromes
a) Unstable angina
b) NSTEMI
c) STEMI
4. Heart failure
5. Arrhythmia
6. Sudden death
Chronic stable angina
Angina pectoris is the clinical syndrome caused by transient myocardial ischaemia. It
may occur whenever there is an imbalance between myocardial oxygen supply and
demand. Coronary atheroma is by far the most common cause of angina.
Chest discomfort caused by transient myocardial ischemia without cell death
Usually brought on by
physical or emotional stress and promptly relieved by rest.
Precipitated by 4 “E’s”
1. Extreme emotion
2. Extreme temperature
3. Excessive eating
4. Exercise
Coronary atheroma is by far the most common cause of angina.
Physical examination is frequently unremarkable.
5
Investigations
Resting ECG often normal.
Exercise ECG.
Myocardial perfusion scanning.
Stress echocardiography.
Coronary arteriography
Management
i.
Risk factors modification such as smoking, hypertension and hyperlipidaemia.
ii.
Drugs
1. Antiplatelet therapy: Low-dose aspirin reduces the risk of adverse events such as MI
and should be prescribed for all patients with coronary artery disease indefinitely
.Clopidogrel (75 mg daily) is an equally effective.
2. Anti-anginal drug treatment:
Nitrates
Beta-blockers
3. Calcium channel antagonists
4. Potassium channel activators
iii.
Invasive treatment
a) Percutaneous coronary intervention PCI.
b) CABG
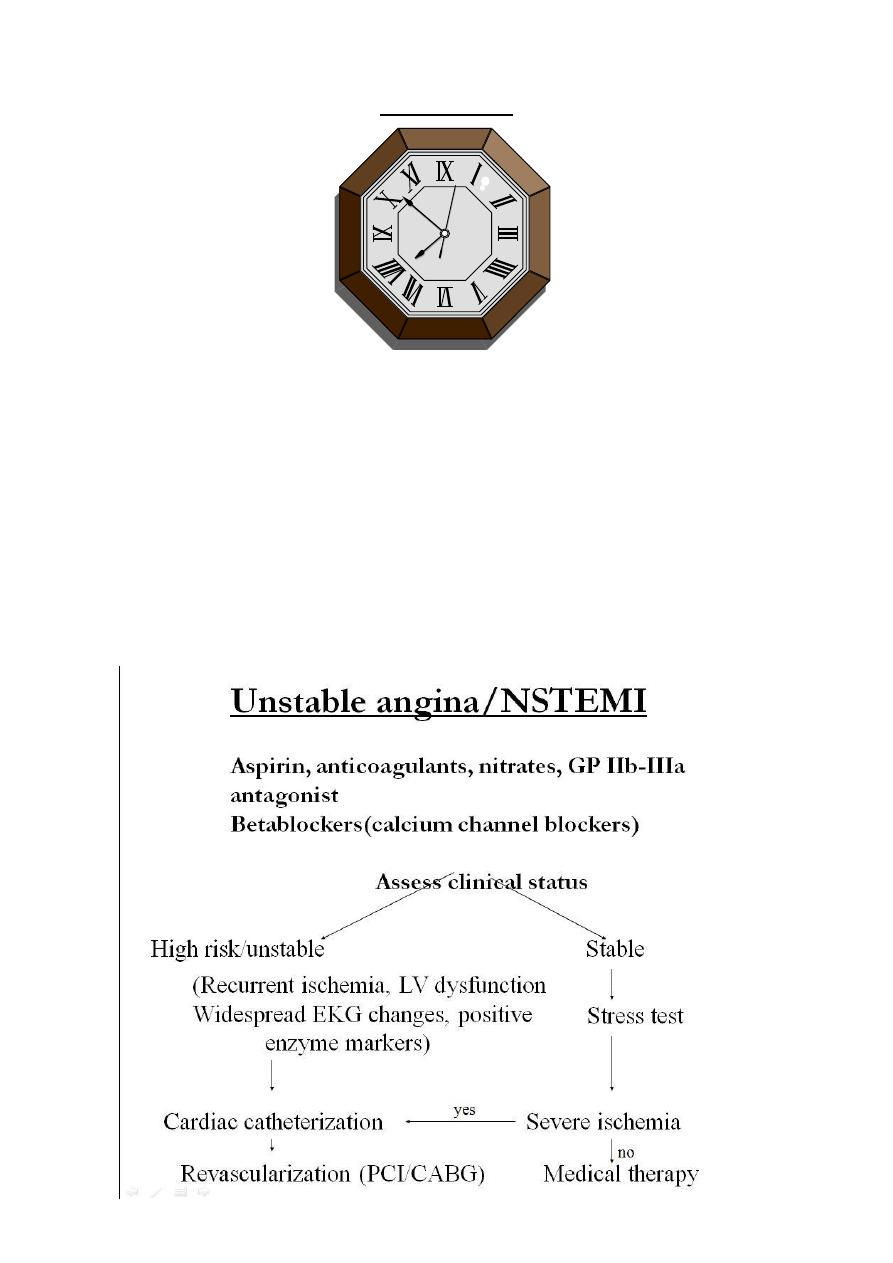
Acute coronary syndrome
Acute coronary syndrome is a term that encompasses both unstable angina and
myocardial infarction (MI). It is characterised by new-onset or rapidly worsening
angina (crescendo angina), angina on minimal exertion or angina at rest in the absence
of myocardial damage.
In contrast, MI occurs when symptoms occur at rest and there is evidence of
myocardial necrosis, as demonstratedby an elevation in cardiac troponin or
creatinekinase-MB isoenzym.
Acute myocardial infarction (AMI)
One of the most common diagnosis in hospitalized patients in industrialized nations
Mortality of acute MI is 30% and one-half of these deaths occur before hospitalization
Mortality after admission has decreased by 30% in last 2 decades
6
Presentation:
Chest pain- most common, similar to anginal pain but more severe and prolonged
described as severe, crushing/squeezing/pressure ....‘worst pain’ ever
Chest pain may be absent in pts with DM or in elderly
Atypical presentations: confusion, syncope, profound wkness, arrhythmia
Differential diagnosis:
1) Pericarditis
2) Pulmonary embolism
3) Pneumothorax
4) Aortic dissection
5) Esophageal spasm
Examination:
Anxiety, pallor, restlessness
Substernal chest pain with diaphoresis is strongly suggestiveof AMI
Those with anterior MI may have sympathetic overactivity whereas those with
inferior MI may have para-sympathetic overactivity
S3/S4
Transient systolic murmur due to dysfunction of mitral apparatus leading to mitral
regurgitation
7
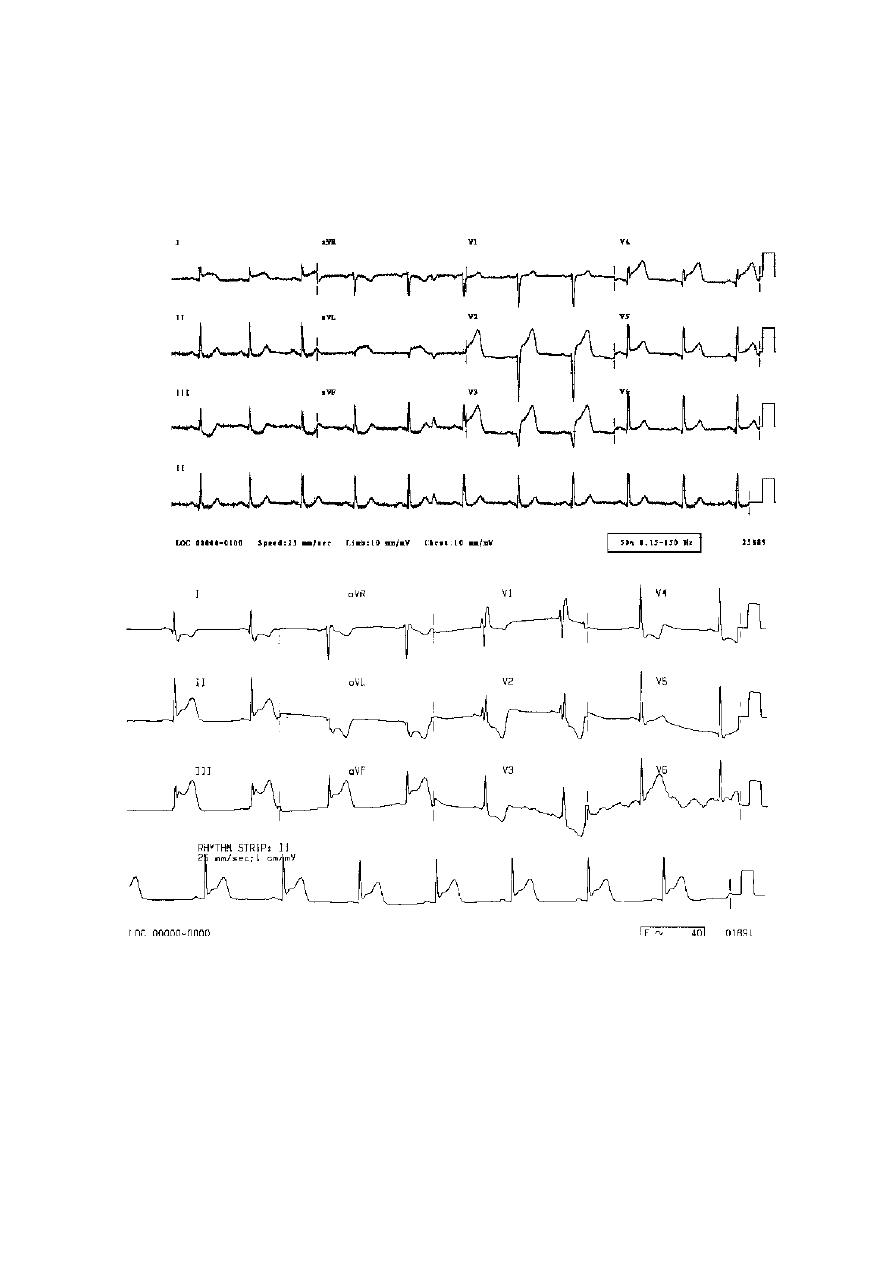
Laboratory findings:
EKG specific but insensitive tool for diagnosis of myocardial ischemia
Total occlusion of infarct related artery leads to ST elevation (STEMI) and subsequent
evolution of Q waves
Partial occlusion/early recanalization/rich collaterals leads to NSTEMI (non-ST
elevation MI)
8
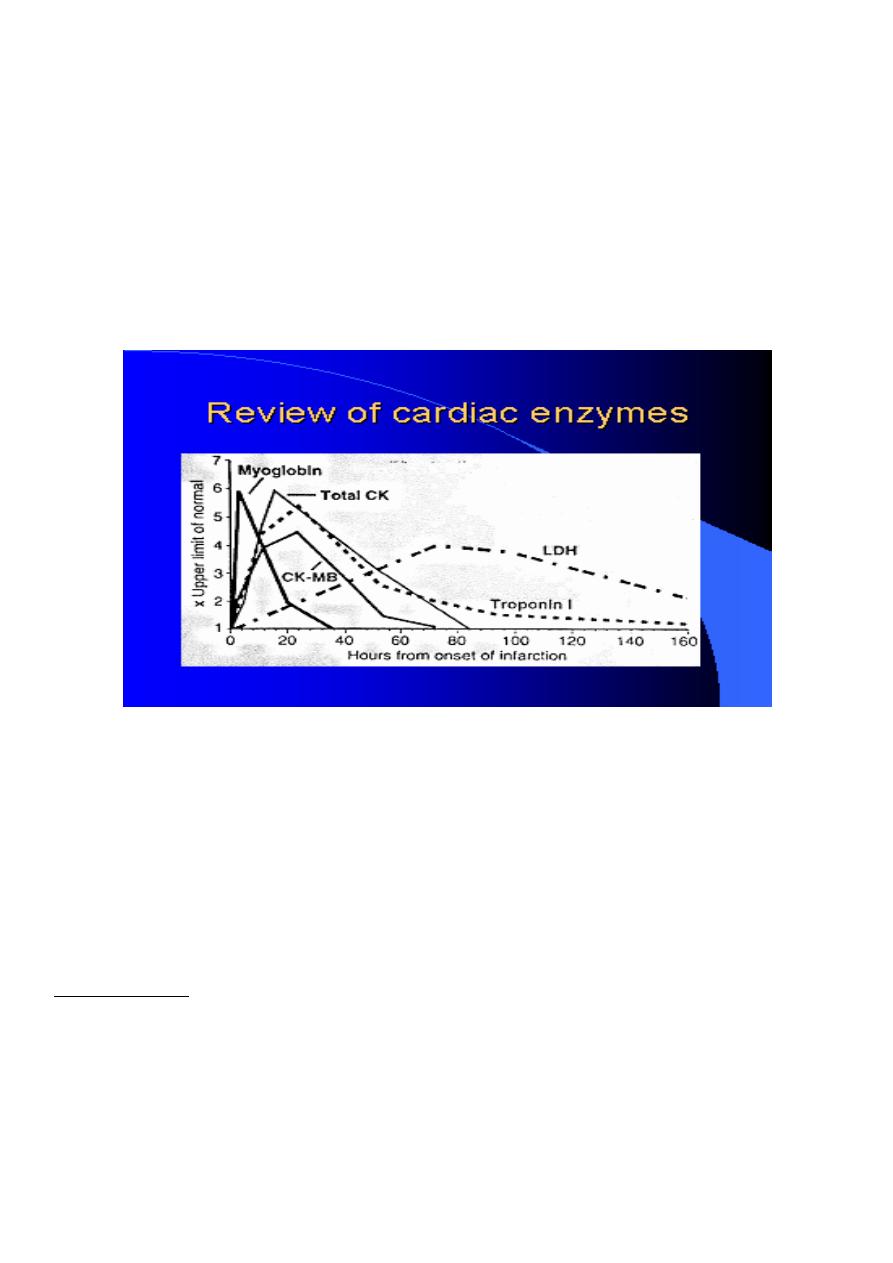
Serum cardiac markers:
Released into the circulation from necrotic heart muscle.
1-CK (creatine kinase) rises 4-8 hrs after onset of MI and normalize by 48-72 hrs,
it is not specific for myocardial necrosis , MB isoenzyme of CK is more specific
2-Cardiac specific troponins: more sensitive and specific than CK and CKMB for
identification of myocardial necrosis
3-Myoglobin- first serum marker to rise after MI, but lacks specificity.
Cardiac imaging
1-2D echocardiographyreveals regional wall motion abnormality also useful to identify
mechanical complications of MI
2-Radionuclide imaging used infrequently in the diagnosis of acute MI mainly used to risk
stratify patients with CHD
Management
Prehospital care:
Major elements include
Recognition of symptoms by the patient and prompt medical attention
Rapid deployment of EMS capable of resuscitation and defibrillation
Expeditious implementation of reperfusion
9
Goals of Initial management in ED
Control of cardiac pain
Rapid identification of patients suitable for reperfusion
Triage of low risk patients for subsequent care
Avoiding inappropriate discharge of patients with MI
Initial management
1) Focused history and Focused examiation
2) Reaassurance
3) Enssure IV acess + Basic investigaions
4) Aspirin: 160-325 mg chewable aspirin + Clopidogril
5) Oxygen by nasal cannula if hypoxemia is present
6) Sublingual nitroglycerine followed by IV infusion if needed
7) Intravenous betablockers (decrease myocardial oxygen demand, control chest pain and
reduce mortality)
8) Morphine for pain relief (given IV in small doses)+ Metelopromide
9) Monitor
10)
12 Leads ECG
11)
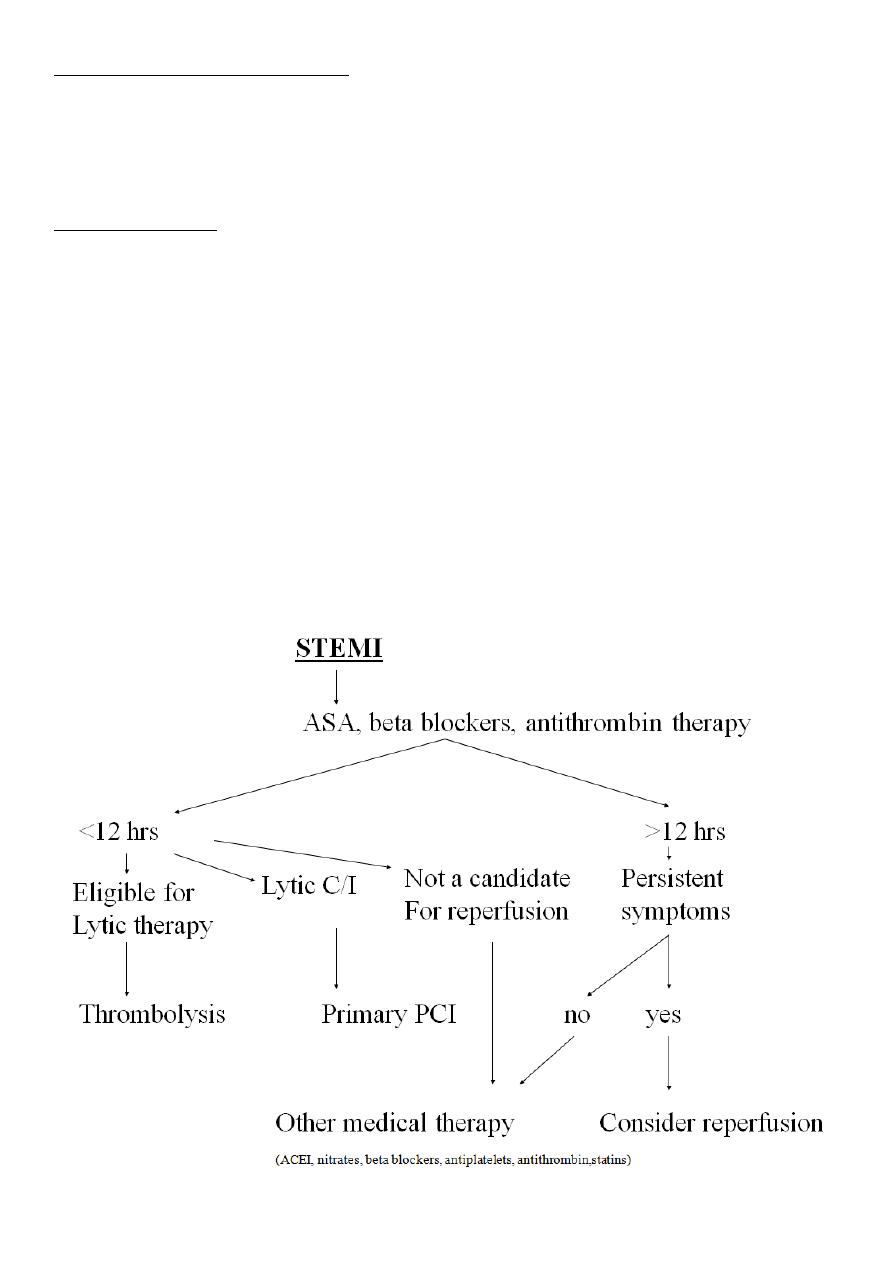
Consider Reperfusion therapy
a) Primary percutaneous coronary intervention (PCI).
b) Thrombolysis.
11
Time is muscle
Complications of acute coronary syndrome
1) Arrhythmias VF,AF, BRADYCARDIA
2) Ischaemia
3) Acute circulatory failure
4) Pericarditis
5) Mechanical complications
6) Embolism
7) Impaired ventricular function HF
8) Ventricular aneurysm

11
Maintanance Therapy
Life style changes
Aspirin
Clopidogril
B blocker
ACE inhibitors
Calcium channel blocker
Statins ( Antilipids)
