
1
Forth stage
Medicine
Lec-15
Dr.Jasim
1/3/2016
Congenital Heart Disease
Aetiology and incidence
• The incidence 0.8% of live births.
• Maternal infection or exposure to drugs or toxins may cause congenital
heart disease. Maternal rubella infection is associated with persistent
ductus arteriosus, pulmonary valvular stenosis, and atrial septal defect.
Maternal alcohol misuse is associated with septal defects, and maternal
lupus erythematosus with congenital complete heart block. Genetic or
chromosomal abnormalities such as Down’s syndrome may cause septal
defects.
• Divided into noncyanotic (L
R) and cyanotic (R
L) categories based
on direction of shunting
Incidence of congenital cardiac malformation
Ventricular septal defect 30
Atrial septal defect 10
Patent ductus arteriosus 10
Pulmonary stenosis 7
Coarctation of aorta 7
Aortic stenosis 6
Tetralogy of Fallot 6
Complete transposition of great arteries 4
Noncyanotic CHD (L
R)
1. Atrial septal defects (ASD)
2. Ventricular septal defects (VSD)
3. Patent ductus arteriosus (PDA)
4. Obstruction to blood flow
Pulmonic stenosis (PS)
Aortic stenosis (AS)
Aortic coarctation
2
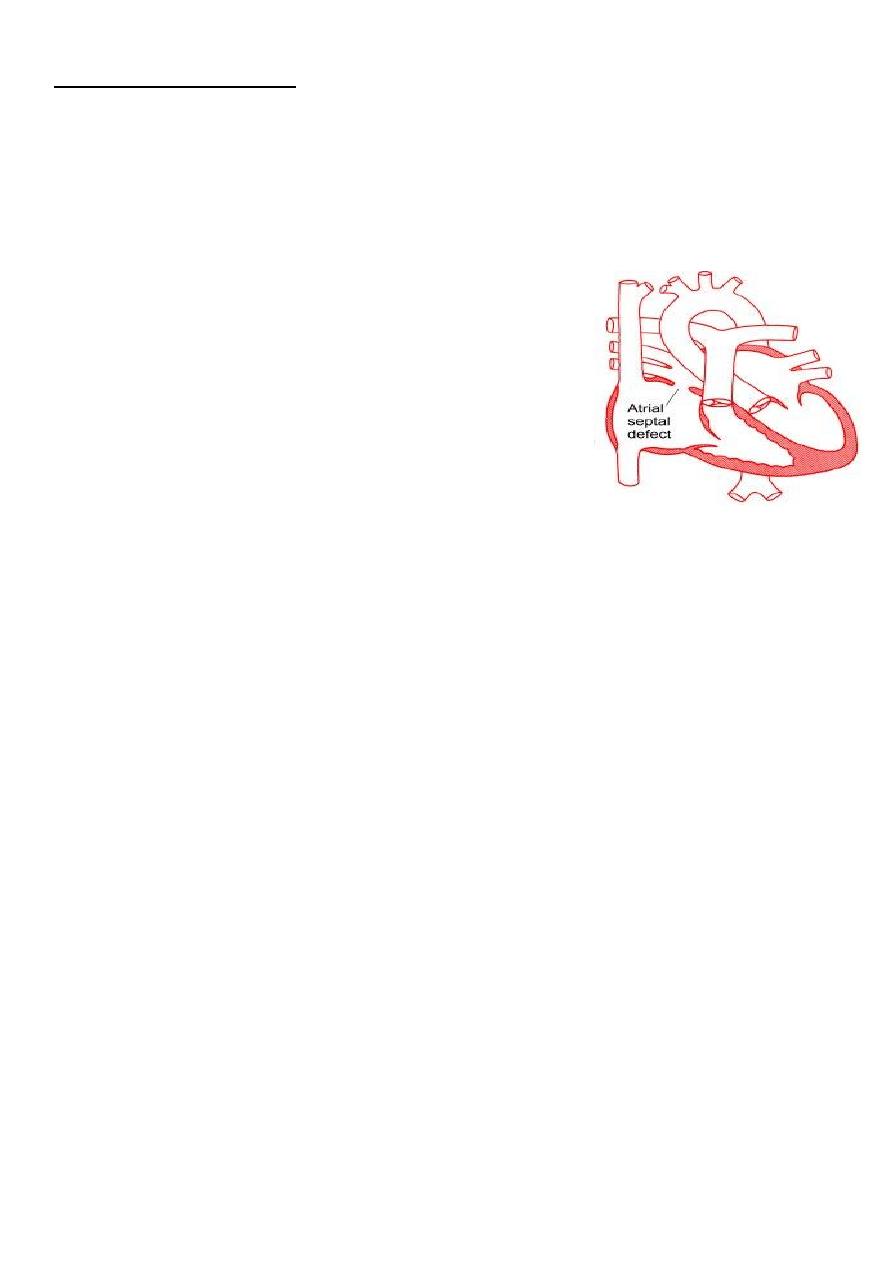
Atrial Septal Defect
Three major types:
1. Ostium secundum
most common
In the middle of the septum in the region of the foramen ovale
2. Ostium primum
Low position
Form of AV septal defect
3. Sinus venosus
Least common
Positioned high in the atrial septum
Clinical Features
Most children are asymptomatic for many years and the condition is often
detected at routine clinical examination
Qp/Qs > 1.5: symptoms (+) :-
1. Effort dyspnea (exercise intolerance)
2. Palpitation (Af/AF)
3. Paradoxical embolism
4. Pulmonary hypertension
5. Eisenmenger's syndrome ((If severe pulmonary hypertension develops,
a left-to-right shunt may reverse, resulting in right-to-left shunt and marked
cyanosis with clubbing))
6. signs:
a) Right ventricular heave
b) S2 widely split and usually fixed
c) Systolic murmur at left 2nd insterconstal space
d) mid-diastole rumble at LLSB (tricuspid flow)
Investigations
1. EKG: SR / Af / AF; RBBB
2. CXR: cardiomegaly, dilated PA
3. Echo: TTE, TEE
4. Cath: Qp / Qs, PA pressure
3
Treatment
Closure generally recommended when ratio of pulmonary to systemic blood flow
(qP/qS) is > 1.5:1
Closure can also be accomplished at cardiac catheterisation using implantable closure
devices.
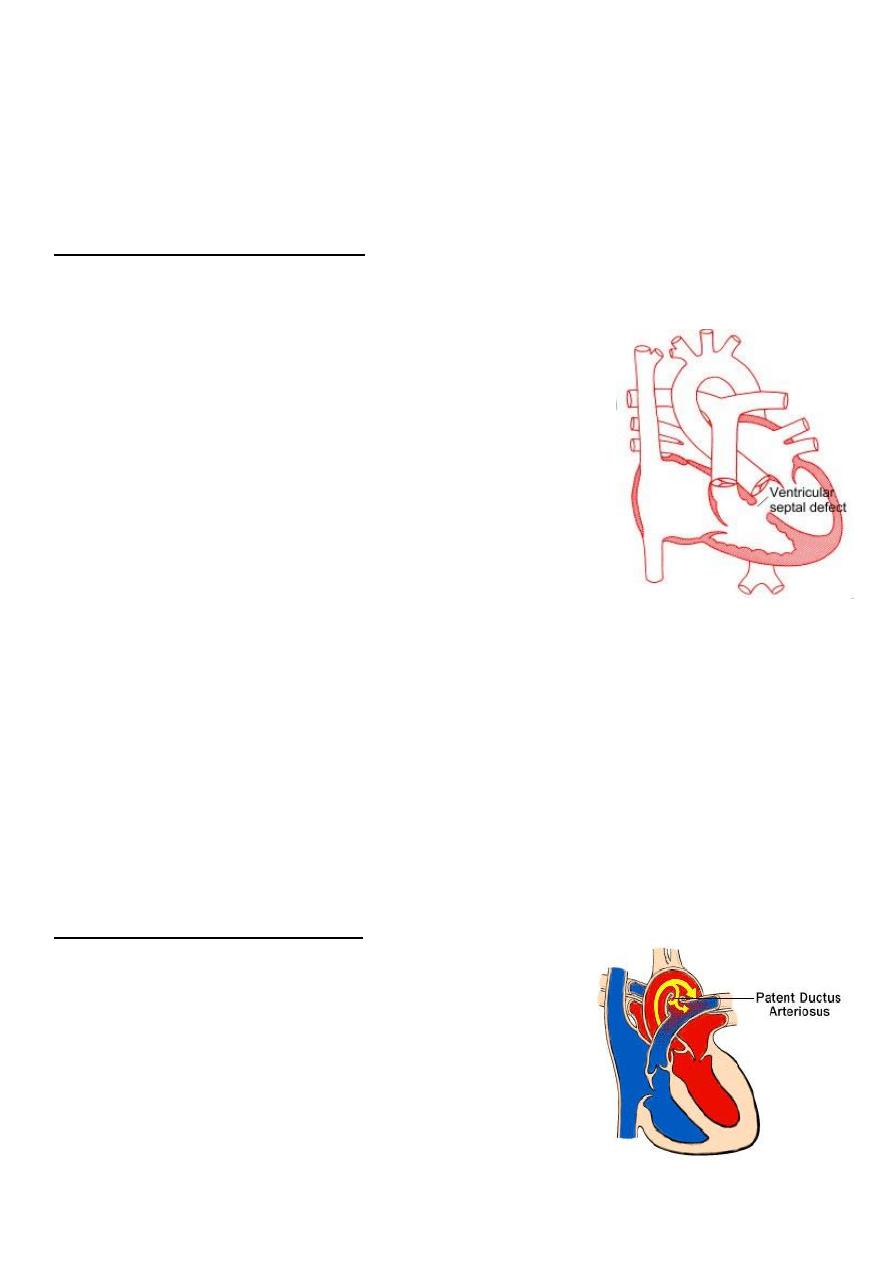
Ventricular Septal Defect
Single most common congenital heart malformation, accounting for almost 30% of all
CHD
Defects can occur in both the membranous portion of the
septum (most common) and the muscular portion
Two major types:
1. Small, All close spontanously (90% by 6 years)
2. Large VSDs with normal PVR (Usually requires surgery,
otherwise patient will develop CHF).
Clinical features
Asymptomatic
may present as cardiac failure in infants.
rarely as Eisenmenger’s syndrome
Systolic thrill and Harsh pansystolic murmur heard best at the left sternal border with
radiation over the entire precordium
Treatment
Small ventricular septal defects require no specific treatment. Cardiac failure in
infancy is initially treated medically with digoxin and diuretics.
Persisting failure is an indication for surgical repair of the defect. Percutaneous
closure devices are under development
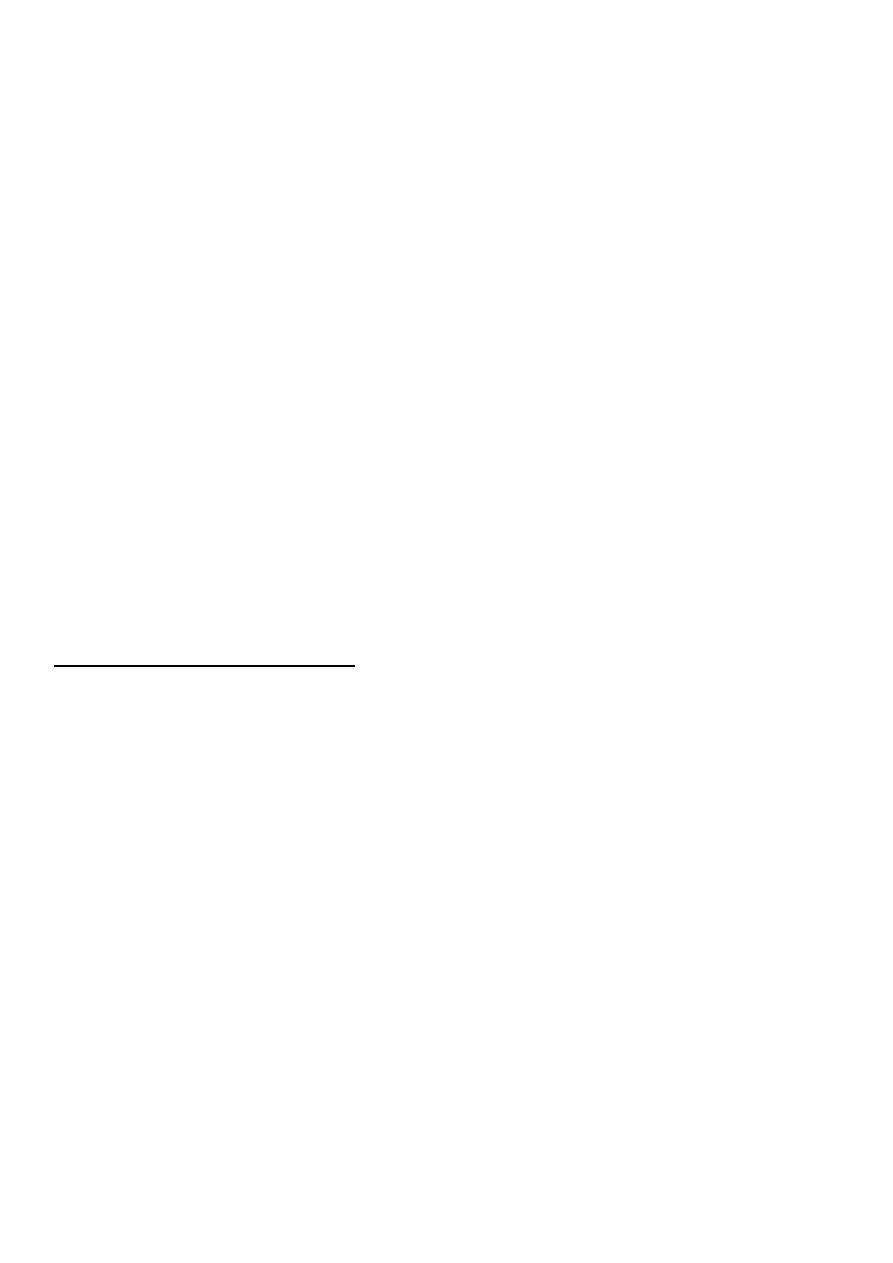
Patent Ductus Arteriosus
Persistence of normal fetal vessel joining the
pulmonary artery to the aorta.
Normally, the ductus closes soon after birth but
sometimes fails to do so.
Accounts for about 10% of all cases of CHD.
More common in females
4
Clinical Features
• Clinical findings and course depend on size of the shunt and the degree of associated
pulmonary hypertension.
• With small shunts there may be no symptoms for years, but when the ductus is large,
growth and development may be retarded.
• Usually there is no disability in infancy but cardiac failure may eventually ensue.
• Pulses are bounding and pulse pressure is widened
• A continuous ‘machinery’ murmur is heard with, maximal in the second left
intercostal space below the clavicle.
Treatment
• consists of surgical correction when the PDA is large.
• Transcatheter closure of small defects has become standard therapy
• In preterm infants indomethacin is used (80-90% success in infants > 1200 grams)
Coarctation of the aorta
• Narrowing of the aorta occurs in the region where the ductus arteriosus joins the
aorta, i.e. at the isthmus just below the origin of the left subclavian artery
• The condition is twice as common in males
Simple coarctation
Complex coarctation: combine other lesions (bicuspid aortic valve, intracranial
aneurysm)
Clinical Features
Epistaxis ,headache, leg weakness on exertion
Leg claudication is rare
Brachial pressure> popliteal pressure 10mmHg
The BP is raised in the upper body but normal or low in the legs. The femoral pulses
are weak, and delayed in comparison with the radial pulse
A systolic murmur is usually heard posteriorly, over the coarctation.
5
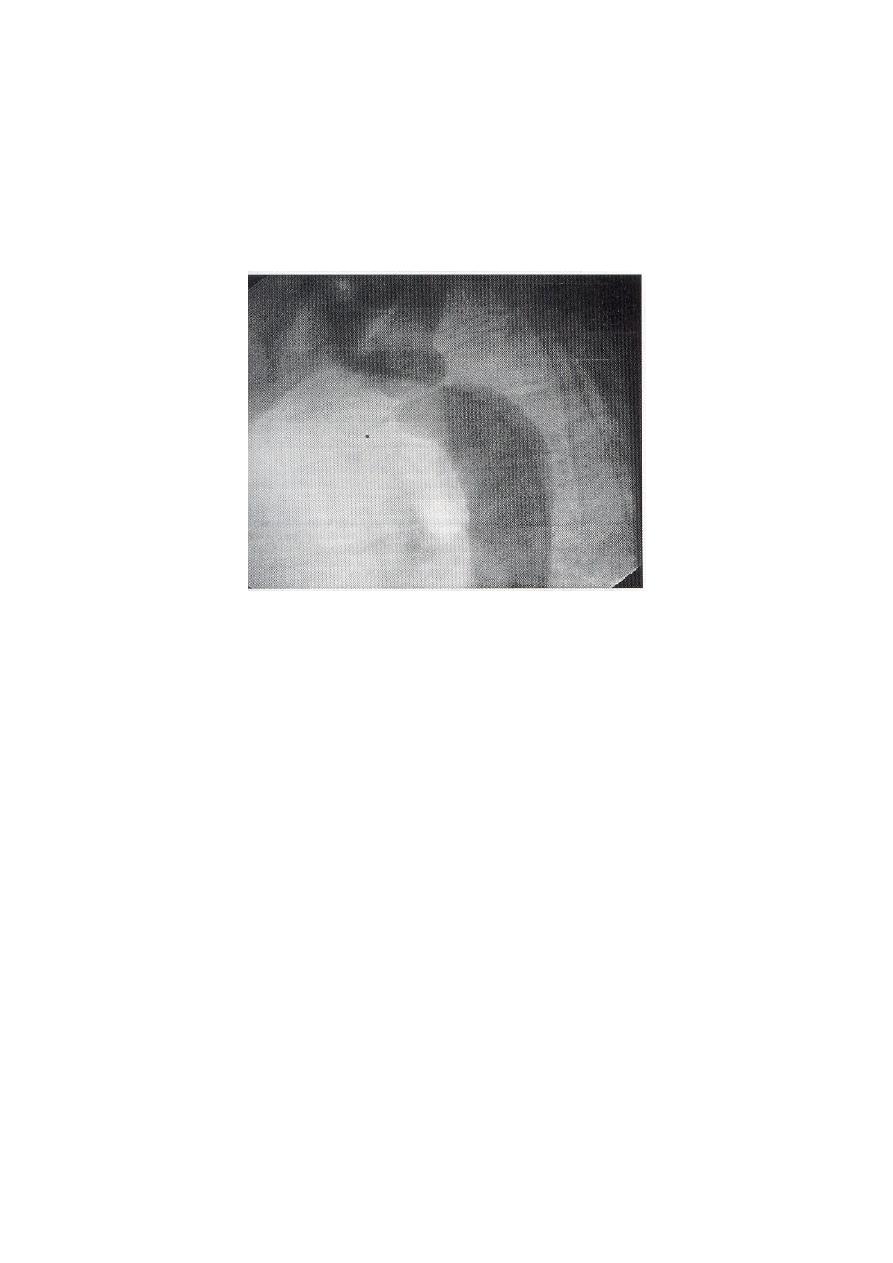
Investigations
1. Chest X-ray in early childhood is often normal but later may show changes in the
contour of the aorta (indentation of the descending aorta, ‘3 sign’) and notching of
the under-surfaces of the ribs from collaterals.
2. MRI is ideal for demonstrating the lesion .
3. The ECG may show left ventricular hypertrophy.
"pre-stenotic and post-stenotic dilatation to form “3” shape"
Treatment
Interventional indication:
1. Arm > leg systolic BP 10mmHg
2. Radial-femoral pulse delay
3. Peak trans-coarctation pressure gradient >20mmHg
Methods:
1. Surgery
2. Transcatheter

6
Cyanotic CHD (R
L)
1. Tetralogy of Fallot (TOF)
2. Tricuspid atresia (TA)
3. Total anomalous pulmonary venous return (TAPVR)
4. Truncus arteriosus
5. Transposition of the great vessels
Tetralogy of Fallot
1. VSD
2. Overriding aorta
3. RVOT obstruction(PS)
4. RVH
ASD (pentalogy)
• Most common cyanotic lesion
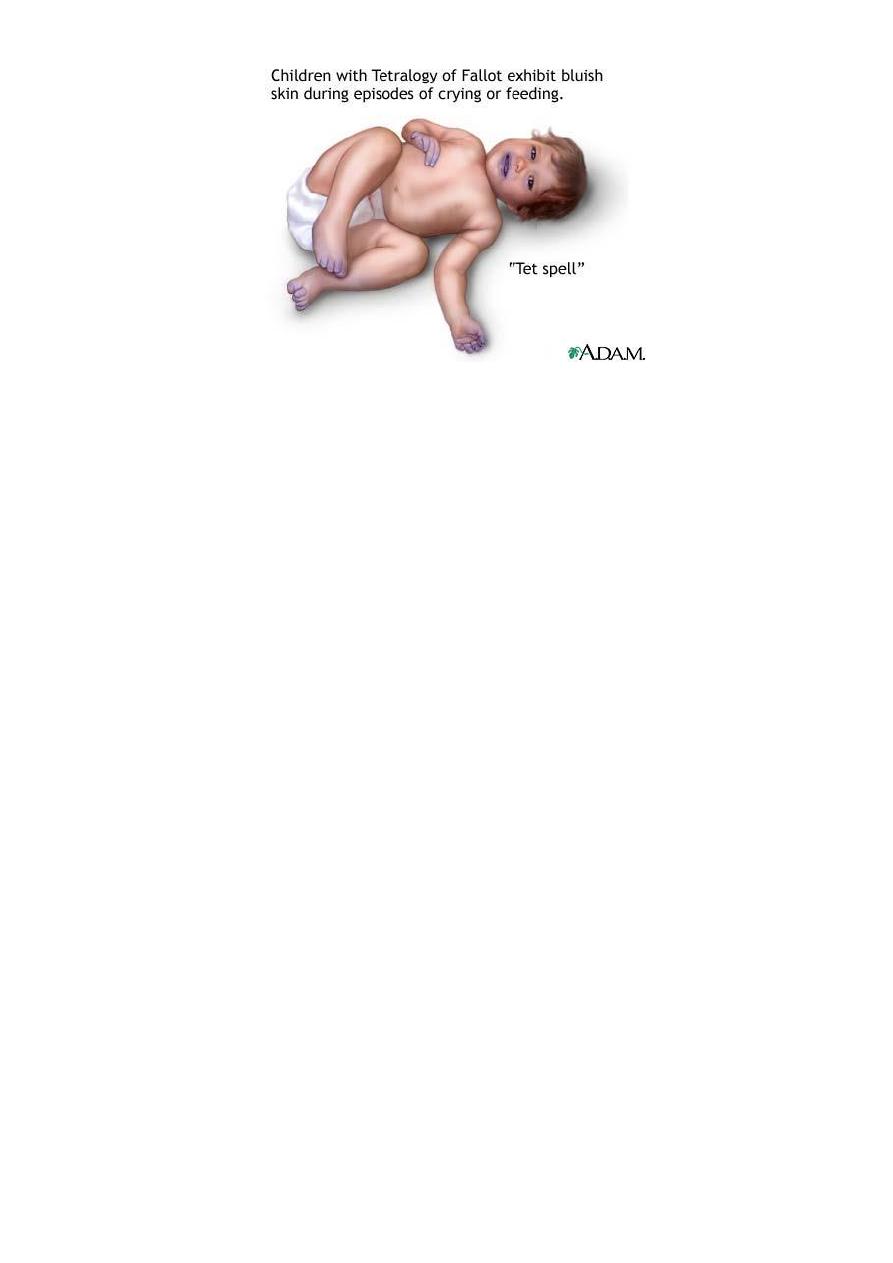
Clinical findings
vary depending on degree of RVOFT obstruction
Most patients are cyanotic by 4 months and it is usually progressive
Hypoxemic spells (“tet spells”) are one of the hallmarks of severe tetralogy
Clubbing
Systlic ejection murmur at the upper LSB
7
Tet spells most commonly start around 4 to 6 months of age and are charcterized by :
1. Sudden onset or deepening of cyanosis
2. Sudden onset of dyspnea
3. Alterations of consciousness
4. Decrease in intensity of systolic murmur
Investigations
1. ECG shows right ventricular hypertrophy
2. chest X-ray shows an abnormally small pulmonary artery and a ‘boot-shaped’ heart.
3. Echocardiography is diagnostic and demonstrates that the aorta is not continuous
with the anterior ventricular septum
Treatment
Surgical Repair may be staged (modified BT shunt) or complete.
