
1
Forth stage
Medicine
Lec-11
.د
رامي
1/1/2014
SEPSIS
Inflammation
• Natural response of tissues to injury or infection aiming for body defence and tissue
healing
• Acute inflammation is the response to acute injury, classically characterized by
hotness, redness, pain, and swelling.
• The inflammation starts local with sequestration and activation of leukocytes and
release of variety of inflammatory mediators from various cells.
• A delicate balance exists between pro- and anti-inflammatory mediators.
systemic inflammatory response syndrome (SIRS)
• Overwhelming infection (or injury) with excessive inflammatory response
• Local control of inflammation is lost
• Pro-inflammatory mediators are released to the circulation
Causes of SIRS
• Infection (sepsis)
• Trauma
• Acute pancreatitis
• Tissue necrosis
• Transfusion reaction
• Vasculitis
• Liver failure
• Disseminated malignancy
systemic inflammatory response syndrome (SIRS)
SIRS is defined by the presence of two or more of the followings:
• Temperature > 38.0
C or < 36.0
C
• Heart rate > 90/min
• Respiratory rate > 20/min
• PaCO2 <32 mmHg (or mechanically ventilated)
• White blood count > 12
10
9
/l or < 4
10
9
/l
If “SIRS” is caused by infection the condition is called “sepsis”
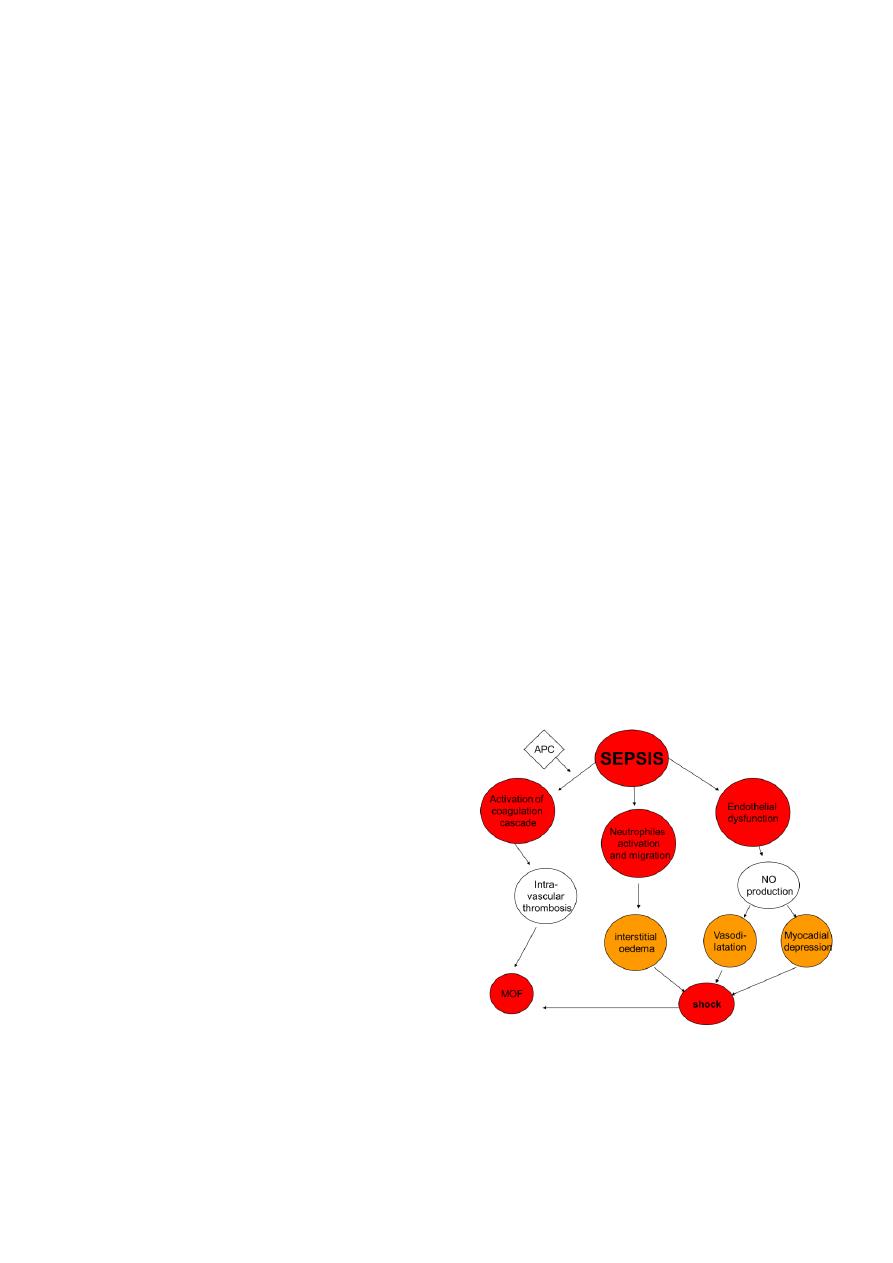
Pathogenesis of sepsis
Complex interaction between coagulation cascade, platelets, endothelial cells and white
blood cells including:
• Activation of coagulation cascade
2
• Endothelial dysfunction
• Activation of neutrophils
Activation of coagulation cascade
• Pro-inflammatory mediators activate the coagulation pathway
• This is inhibited by natural coagulation inhibitors (antithrombin
and activated
protein C (APC))
• When natural anticoagulants are depleted (together with endothelial dysfunction),
intravascular thrombosis and DIC develop
Activation of neutrophils
• Neutrophils adhere to the vascular endothelium
• Migrate through damaged endothelial cells to the interstitial space together with
fluids and proteins resulting in tissue oedema
• Excessive fluid leak reduces intravascular volume, causing hypovolaemia.
Endothelial dysfunction
• Predispose to microvascular thrombosis and DIC
• Produce nitric oxide (NO) which is a potent vasodilator and myocardial depressor
Reduced oxygen uptake
• A major component of the pathophysiology of sepsis is the inability to take up oxygen
at the mitochondrial level, even when the oxygen delivery is normal.
• The low oxygen extraction by the tissues raises plasma lactate and increases mixed
venous oxygen saturation.
Splanchnic hypoperfusion
• In patients with shock, splanchnic
hypoperfusion and ischaemia is
associated with:
increased gut mucosal permeability
translocation of microorganisms form the
gut lumen into the portal and lymphatic
circulation.
kupffer cells activation with the
production and release of inflammatory
mediators that further amplify the
inflammatory
Sepsis terminology
• Severe sepsis: sepsis with early organ dysfunction or hypotension
• Septic shock: sepsis associated with organ failure or severe hypotension
unresponsive to fluid resuscitation
• MOF: represent multiple organ dysfunction syndrome

3
Multiple organ dysfunction syndrome (MOF)
This can manifest in the
• lungs as acute respiratory distress syndrome (ARDS) or (ALI)
• kidneys as acute tubular necrosis (ATN)
• liver necrosis
• GIT ulceration and bleeding
• myocardial depression and heart failure
• disruption of coagulation (DIC)
Causative pathogenic microorganisms
• The vast majority of sepsis cases are caused by bacteria, both gram negative (most
common) and gram positive (which is increasing).
• Fungi (esp. candida) are also important particularly in neutropenic patients.
• Viruses and protozoa are also possible causes of sepsis.
• Microbial bloodstream invasion, with positive blood culture is not essential for the
development of sepsis as microbial products and toxins may illicit the same response.
Clinical features of sepsis
• Patients with sepsis may present with fever or hypothermia, tachycardia and warm
extremities (until late in the course of the disease), and tachypnoea.
• Many patients are hypotensive, and may be in shock state.
• Apart from these manifestations, patients usually present with clinical features of the
underlying infection, but many other patients do not show symptoms or signs that
refer to the site of the infection.
Original site of infection in sepsis
Common sites:
• The lungs (esp. nosocomial pneumonia, where gram negative bacilli are most
common).
• The urinary tract (acute pyelonephritis).
• The bloodstream (central venous line infection).
• The abdomen (intra-abdominal abscess or necrotic gut complicating abdominal
surgery).
Less common sites include:
• The heart valves (endocarditis)
• The meninges (meningitis)
• The bones and joints (acute osteomyelitis and septic arthritis)
• The female genital tract (septic abortion and puerperal sepsis)
• The GIT (Cl. Difficele infection)
• The sinuses (sinusitis)
Investigation in patients with sepsis
All patients require the following investigations:
• Culture of blood, sputum, urine, intravascular line, and wound discharge (blood
culture is positive in only 10% of cases partly because of prior use of antibiotics)
• CBP (including WBC differential count and platelets) and ESR
4
• General urine examination
• Chest X-ray
• Coagulation profile (prothrombin time, APTT, and fibrinogen)
Other investigations will depend on the clinical picture including:
• X-ray of the bones, abdomen, and sinuses
• Ultrasound examination of abdomen and pelvis
• CT scan of the abdomen, pelvis or other sites
• Echocardiography (transthoracic and transoesophageal)
• CSF examination
Management of sepsis
Antibiotic therapy
Prompt institution of appropriate antibiotic is essential. The antibiotic chosen should cover
all the likely causative microorganisms. This would depend on:
• The probable site of the infection
• The known resistant pattern in the hospital
• Previous antibiotic therapy
• Any available culture results
The antibiotics should be given intravenously, and in doses that ensure penetration to
infected tissues (esp. in meningitis and endocarditis).
• Early goal-directed therapy (EGDT) is an algorithmic approach to hemodynamic
optimization and resolution of global tissue hypoxia (aiming to normalize venous
oxygen tension or lactate level) within the first 6 hours of disease presentation.
• This approach is globally adopted and was shown to reduce in-hospital mortality
IV fluids and vasopressors
• Sufficient amounts of IV fluids should be given to replace the diminished
intravascular volume. Early effective fluid replacement in the first 6 hours was shown
to improve survival.
• Any crystalloid infusion is suitable, but normal saline is most commonly used. The
amount to be given varies but it is usually around 6 liters.
• If the patient is still hypotensive despite IV fluid replacement, a vasoactive agent
(vasopressors) has to be added. The choice is dopamine or noradrenalin given as IV
infusion at a dose sufficient to keep blood pressure normal usually with inotropic
drug (dobutamin)
Source control
Measures to eradicate the source of the infection are an integral component of therapy
This may include:
• Abscess drainage
• Debridement of devitalized infected tissue
• Removal of infected prosthesis.
other therapies
• The role of corticosteroid replacement therapy is controversial.
• Activated protein C is no more used in the treatment of sepsis
