1
Forth stage
Medicine
Lec-4
.د
رامي
1/1/2014
Pulmonary embolism
Venous thromboembolism:
pulmonary embolism (PE)
deep vein thrombosis (DVT)
1% of all patients admitted to hospital
5% of in-hospital mortality
A common mode of death in patients with cancer, stroke and pregnancy.
Pathophysiology of pulmonary embolism
Ventilation-perfusion mismatch and ischaemia to the peripheral pulmonary lung
tissues.
Acute increase in pulmonary vascular resistance which increase right ventricular load
and may reduce cardiac output.
Clinical features
The clinical presentation varies depending on the number and size of the embolus and
on the underlying cardiopulmonary reserve.
It is possible to recognize three major categories of cases:
Acute massive PE
Acute small and medium PE
Chronic thromboembolism

2
Acute massive PE
A big thrombus obstructing a major pulmonary artery causing low cardiac output and
acute right heart failure.
Sudden collapse (fainting), crushing central chest pain and severe dyspnoea.
Examination would reveal tachypnoea, tachycardia, hypotension (or cardiogenic
shock), raised JVP and cyanosis.
CXR is commonly normal (or show subtle oligaemia).
ECG: tachycardia and may show S
1
Q
3
T
3
, anterior T-wave inversion or RBBB
Arterial BGA: hypoxaemia and hypocapnea
Differential diagnosis: acute myocardial infarction (MI), pericardial tamponade and
aortic dissection.
Acute small or medium PE
Occlusion of segmental pulmonary artery leading to pulmonary infarction with or
without pleural effusion.
Dyspnoea, pleuritic chest pain and haemoptysis.
Tachycardia, low grade fever, but normal BP. Pleural rub or crackles can be heard.
Dullness and diminished breathing at the lung base may indicate pleural effusion or
elevated dome of the diaphragm.
CXR may show opacities (of any size or shape); more specifically it may show
horizontal linear opacities or wedge shaped pleural based opacities. Pleural effusion
or raised hemidiaphragm may be noticed.
ECG: sinus tachycardia
Arterial BGA: normal or show mild hypoxaemia and hypocapnea
Differential diagnosis: pneumonia
Chronic thromboembolism
Chronic occlusion of pulmonary microvasculature caused by multiple small emboli or
a sequel to previous organized thrombus, resulting in chronic pulmonary
hypertension.
The patient presents with exertional dyspnoea and features of right heart failure.
ECG: right ventricular hypertrophy and strain.
Arterial BGA: exertional hypoxaemia
3
Consider the diagnosis of VTE in any patient presenting with:
New or worsening dyspnoea
Chest pain
Sustained hypotension
without alternative obvious cause
particularly in patients who have risk factors
Diagnosis
Three questions should be in mind on facing a patient with suspected VTE:
Is the clinical presentation consistent with PTE?
Does the patient have risk factors?
Any alternative diagnosis that can explain the presentation?
The ECG may show tachycardia only, the CXR is commonly normal. Both investigations are
more useful in excluding other diagnosis like MI (ECG), pneumonia and pneumothorax
(CXR)
D-dimer
D-dimer is a specific degradation product of cross linked fibrin. Apart from PE, it also
rises in MI, pneumonia and sepsis.
Low D-dimer has a high negative predicted value and other investigations are
unnecessary if the clinical probability is low.
D-dimer is not useful in intermediate and high risk patients because a further
investigation is mandatory even if it is normal
Imaging
CT pulmonary angiography (CTPA)
Ventilation-perfusion scan (V/Q scan)
Colour Doppler ultrasound of the leg
4
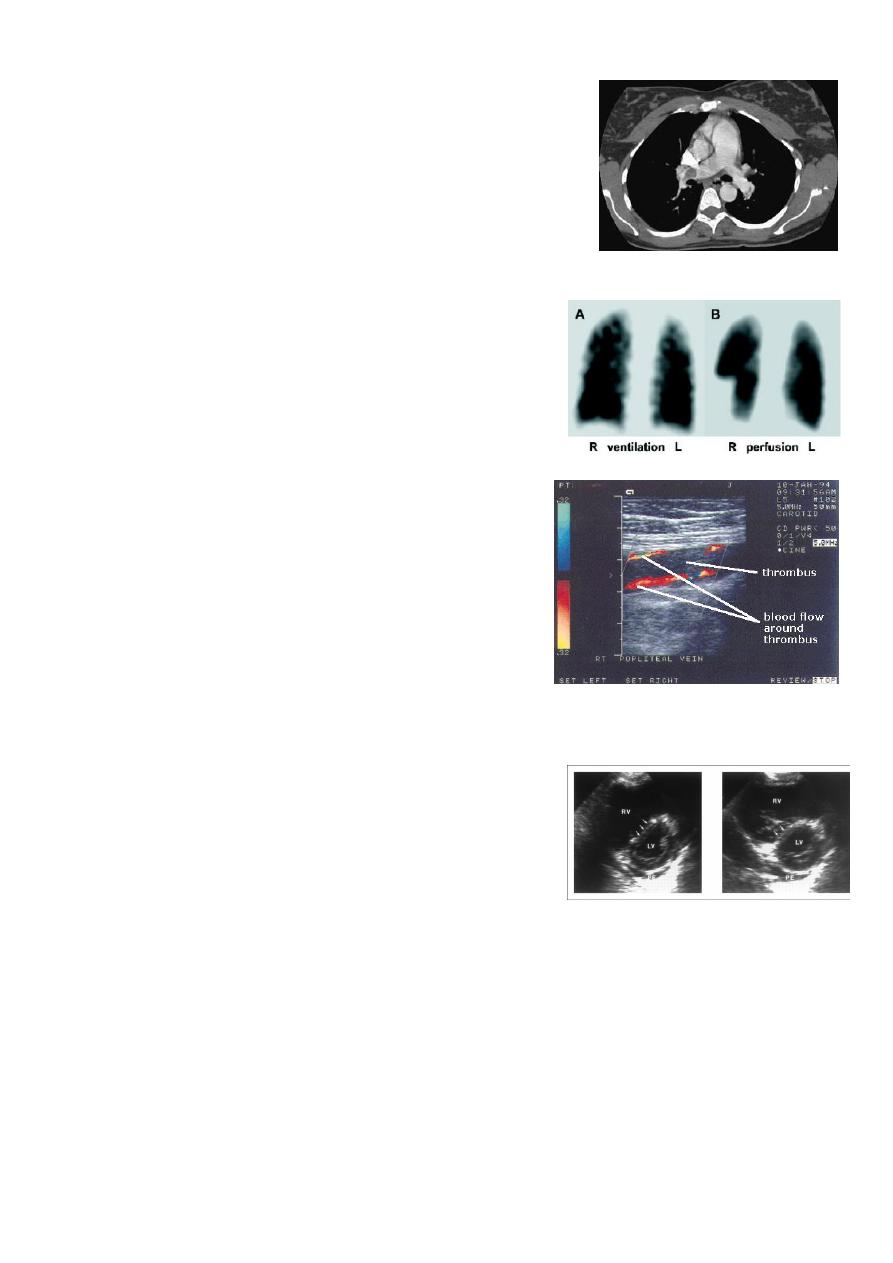
CT pulmonary angiography (CTPA)
It visualizes the distribution and extent of emboli in
positive cases.
It may also prove alternative diagnosis
Simultaneous visualization of femoral and popliteal
veins for DVT improves sensitivity.
Can be performed safely in pregnant women (with
foetal shielding).
Ventilation-perfusion scan (V/Q scan)
Less commonly used.
It is more useful in patients without pre-existing
cardiopulmonary disease and normal CXR;
otherwise the interpretation of the results can be
difficult.
Colour Doppler ultrasound of the leg
The investigation of choice in the assessment of
suspected DVT.
It can be performed in patients with suspected
pulmonary embolism to prove the presence of
thrombus in the leg veins.
Echocardiography
It is helpful in the evaluation of patients with acute
circulatory collapse.
Acute right ventricular dilatation is usually present
in massive PE
A thrombus may be visible.
Alternative diagnosis, like heart failure and
pericardial tamponade can be excluded
Management
General measures
Oxygen therapy for hypoxaemic patients
Circulatory shock should be treated with intravenous fluids. Enotropic agents are of
limited value
Opiates may be necessary to relieve pain and distress
Resuscitation by external cardiac massage in moribund patient may be successful
Diuretics and vasodilators should be avoided

5
Anticoagulation
Subcutaneous low molecular weight heparin (LMWH) is preferred
Fondaparinux is a pentasaccharide that is also approved for treatment of VTE.
Unfractionated heparin can also be used, but it should be administered as continuous
intravenous infusion (through infusion pump) and requires adjustment of APTT
The duration of heparin (or fondaparinux) treatment should be at least 5 days, during
which oral warfarin is commenced
Patients with a persistent risk factor or a history of previous thrombosis should
receive warfarin for life.
Those with identifiable and reversible risk factor require 3 months therapy.
If the condition is idiopathic or the risk factor is weak, anticoagulation for 6 months is
recommended.
Warfarin is teratogenic, so VTE should be treated with LMWH during pregnancy
(giving prophylactic dose after the initial therapeutic dosing).
Thrombolytic therapy
Thrombolysis is indicated in any patient presenting with acute massive PE
accompanied by cardiogenic shock.
Less certain indications include right ventricular dilatation and hypokinesia on
echocardiography , severe hypoxaemia or high troponin level
Patients with haemorrhagic risks should be excluded, as there is a risk of intracranial
haemorrhge.
Caval filters
Inferior vena caval filter is indicted in the following situations:
When anticoagulation is contraindicated
Massive haemorrhage on anticoagulation
Recurrent PE despite anticoagulation
