1
4th stage
باطنية
Lec-9
د.ظاهر
6/12/2015
Pneumothorax
Pneumothorax
It is a significant global health problem, with a reported incidence
of 18–28/100 000 cases per annum for men and 1.2–6/100 000
for women.
The term „pneumothorax‟ was first coined by Itard and then
Laennec in 1803 and 1819 respectively, and refers to air in the
pleural cavity (ie, interspersed between the lung and the chest
wall).
At that time, most cases of pneumothorax were secondary to
tuberculosis, although some were recognised as occurring in
otherwise healthy patients („pneumothorax simple‟).
Pneumothorax
Secondary spontaneouse (SSP) is associated with underlying lung
disease, in distinction to primary spontaneous pneumothorax, PSP.
Although tuberculosis is no longer the commonest underlying lung
disease in the developed world,the consequences of a pneumothorax in
patients with pre-existing lung disease are significantly greater, and the
management is potentially more difficult.
Pneumothorax
Traumatic pneumothorax results from penetrating or blunt
trauma.
Iatrogenic pneumothorax may follow procedures such as
thoracentesis, pleural biopsy, subclavian or internal jugular vein
catheter placement, percutaneous lung biopsy, bronchoscopy
with transbronchial biopsy, and positive-pressure mechanical
ventilation.

2
Pneumothorax
Primary pneumothorax affects mainly tall, thin boys and men
between the ages of 10 and 30 years. It is thought to occur from
rupture of subpleural apical blebs in response to high negative
intrapleural pressures.
Family history and cigarette smoking may also be important
factors.
Secondary pneumothorax occurs as a complication of COPD,
asthma, cystic fibrosis, tuberculosis, Pneumocystis pneumonia,
menstruation (catamenial pneumothorax), and a wide variety of
interstitial lung diseases.
Clinical Findings of Pneumothorax
• Chest pain ranging from minimal to severe on the affected side
and dyspnea occur in nearly all patients. Symptoms usually begin
during rest and usually resolve within 24 hours even if the
pneumothorax persists.
• Alternatively, pneumothorax may present with life-threatening
respiratory failure if underlying COPD or asthma is present.
• If pneumothorax is small (less than 15% of a hemithorax), physical
findings, other than mild tachycardia, are unimpressive.
Clinical Findings of Pneumothorax
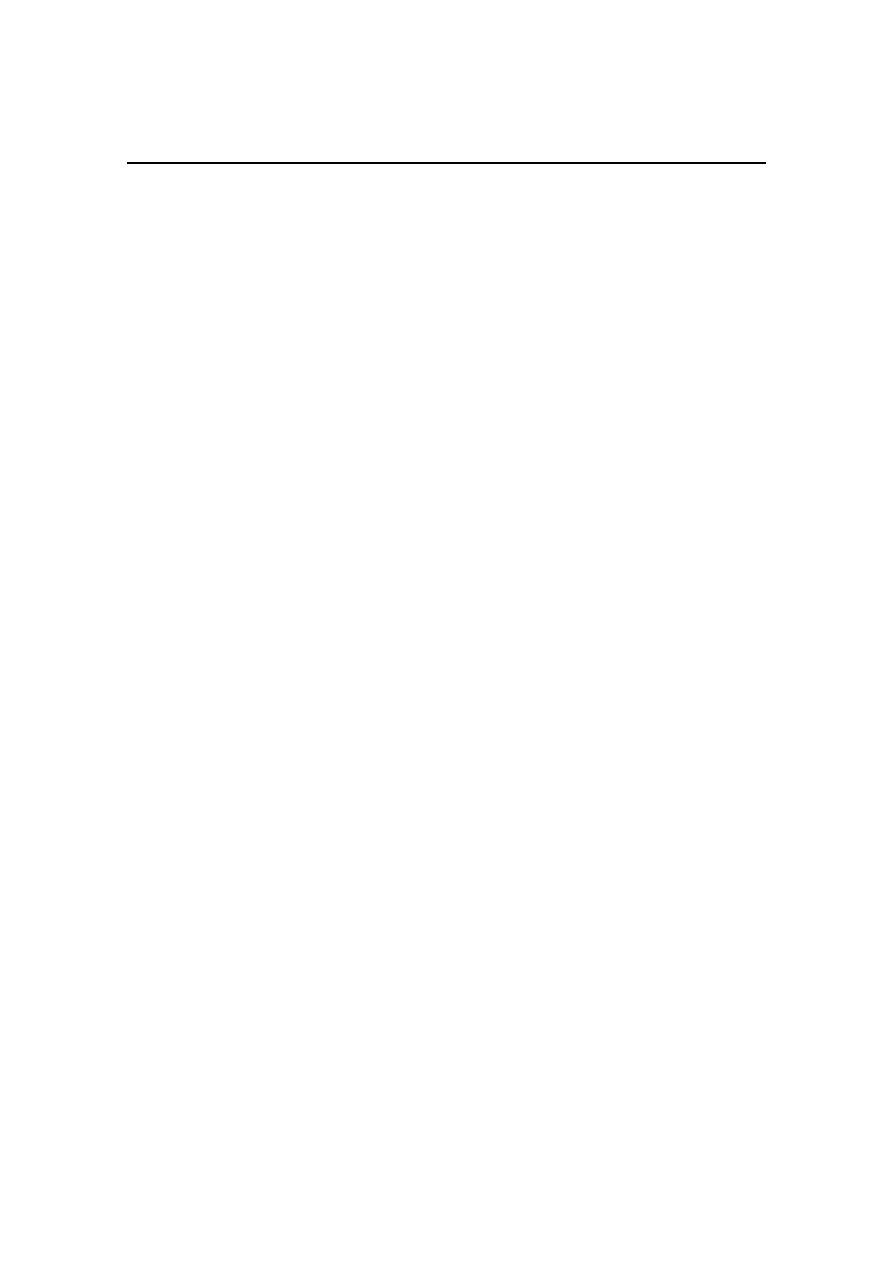
• If pneumothorax is large, diminished breath sounds, decreased
tactile fremitus, and decreased movement of the chest are often
noted.
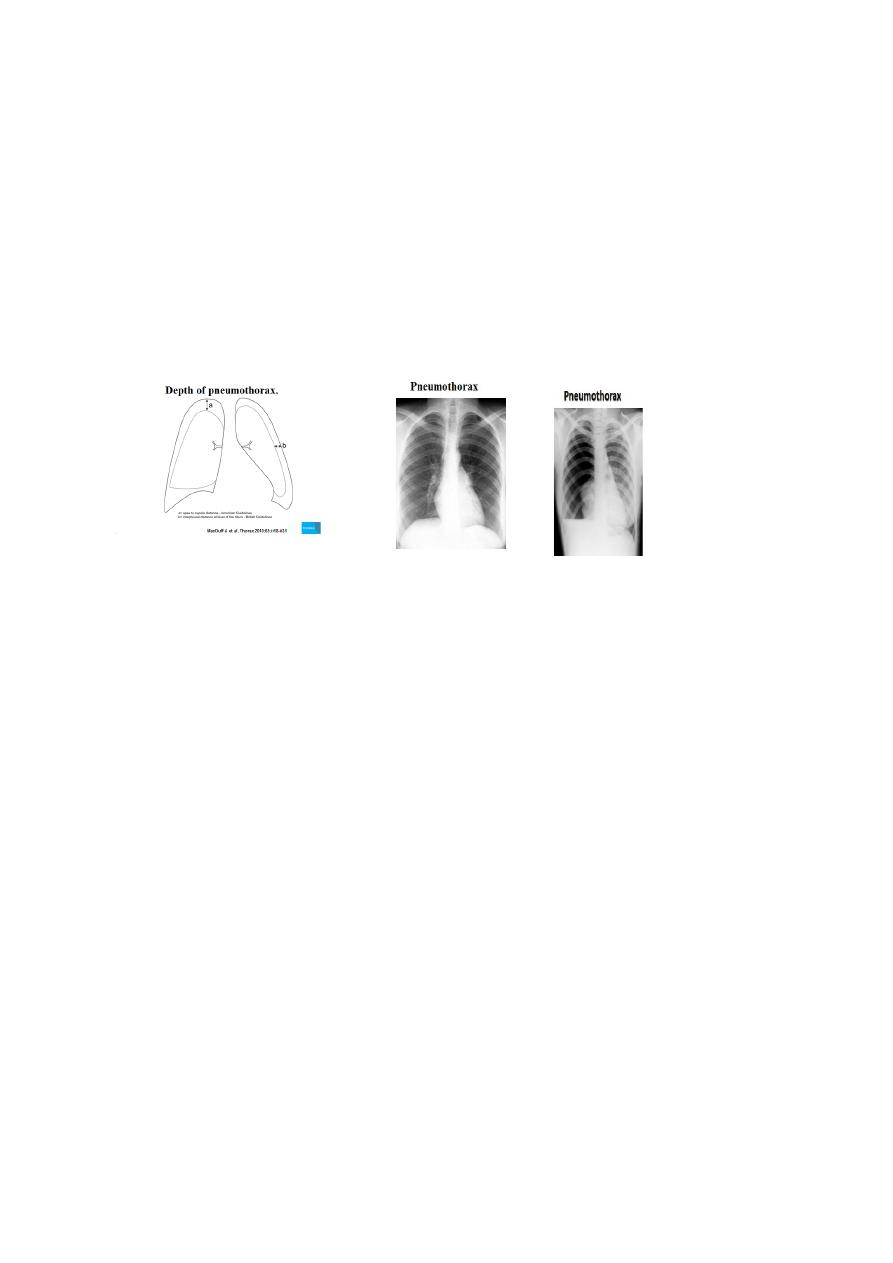
• Tension pneumothorax should be suspected in the presence of
marked tachycardia, hypotension, and mediastinal or tracheal
shift.
3
How to investigate patient with suspected Pneumothorax
A-LABORATORY FINDINGS:
Arterial blood gas analysis is often unnecessary but reveals hypoxemia
and acute respiratory alkalosis in most patients.
Left-sided primary pneumothorax may produce QRS axis and precordial
T wave changes on the ECG that may be misinterpreted as acute
myocardial infarction.
How to investigate patient with suspected Pneumothorax
B-IMAGING
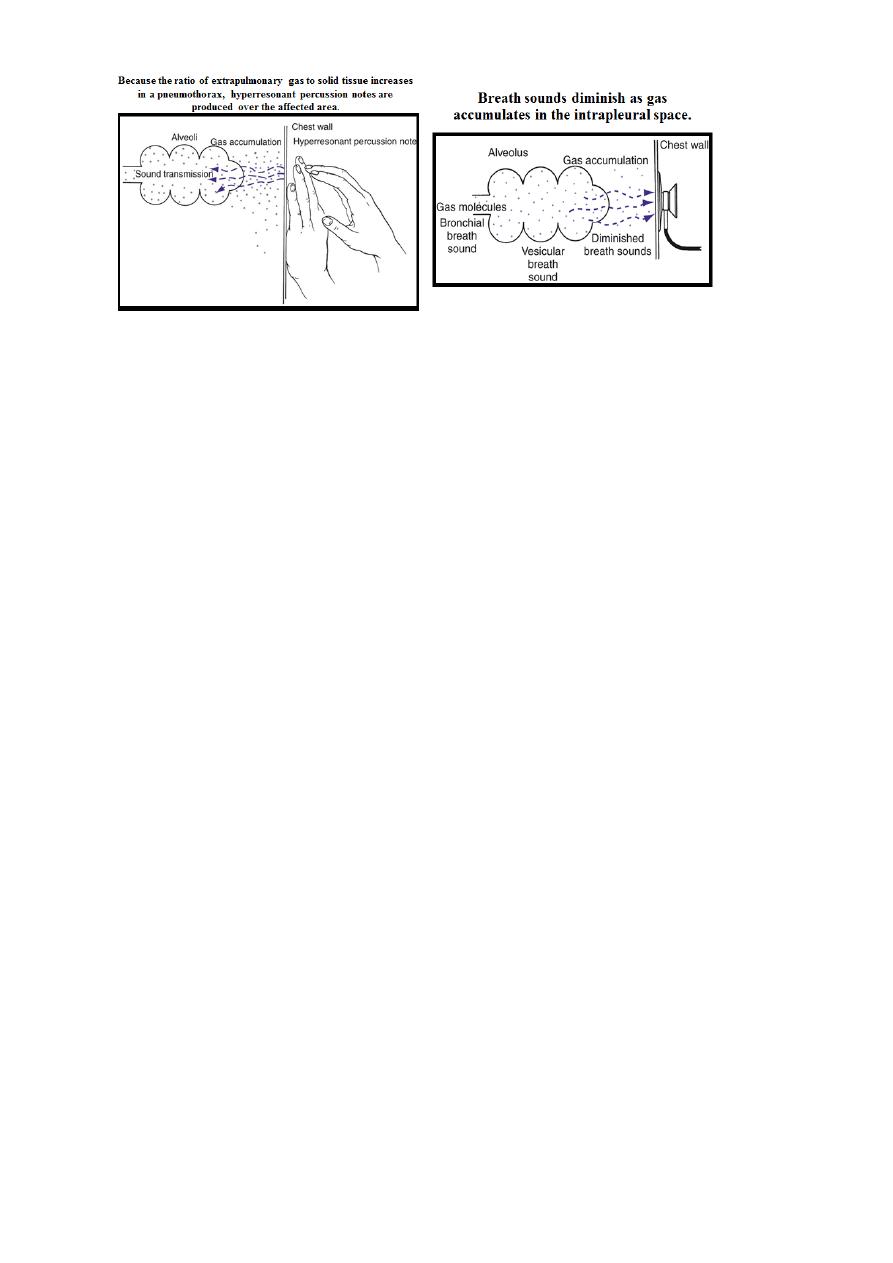
Demonstration of a visceral pleural line on chest radiograph is diagnostic
and may only be seen on an expiratory film.
A few patients have secondary pleural effusion that demonstrates a
characteristic air-fluid level on chest radiography. In supine patients,
pneumothorax on a conventional chest radiograph may appear as an
abnormally radiolucent costophrenic sulcus (the “deep sulcus” sign).
4
Imaging for Pneumothorax
Standard erect PA chest x-ray.
Lateral x-rays.
Expiratory films.
Supine and lateral decubitus x-rays.
Ultrasound scanning.
Digital imaging.
CT scanning.
How to investigate patient with suspected Pneumothorax
• B-IMAGING……
In patients with tension pneumothorax, chest radiographs show a large
amount of air in the affected hemithorax and contralateral shift of the
mediastinum.
5
Differential Diagnosis of Pneumothorax
• If the patient is a young, tall, thin, cigarette-smoking man, the
diagnosis of primary spontaneous pneumothorax is usually
obvious and can be confirmed by chest radiograph.
• In secondary pneumothorax, it is sometimes difficult to
distinguish loculated pneumothorax from an emphysematous
bleb. Occasionally, pneumothorax may mimic myocardial
infarction, pulmonary embolization, or pneumonia
Treatment of Pneumothorax
Treatment depends on the severity of pneumothorax and the nature of
the underlying disease.
In a reliable patient with a small (< 15% of a hemithorax), stable
spontaneous primary pneumothorax, observation alone may be
appropriate.
Many small pneumothoraces resolve spontaneously as air is absorbed
from the pleural space; supplemental oxygen therapy may increase the
rate of reabsorption.

6
Treatment of Pneumothorax
• Simple aspiration drainage of pleural air with a small-bore
catheter (eg, 16 gauge angiocatheter or larger drainage catheter)
can be performed for spontaneous primary pneumothoraces that
are large or progressive.
• Placement of a small-bore chest tube (7F to 14F) attached to a
one-way Heimlich valve provides protection against development
of tension pneumothorax and may permit observation from
home.
• The patient should be treated symptomatically for cough and
chest pain, and followed with serial chest radiographs every 24
hours.

7
Treatment of Pneumothorax
• Patients with secondary pneumothorax, large pneumothorax,
tension pneumothorax, or severe symptoms or those who have a
pneumothorax on mechanical ventilation should undergo chest
tube placement (tube thoracostomy).
• The chest tube is placed under water-seal drainage, and suction is
applied until the lung expands.
• The chest tube can be removed after the air leak subsides.
Treatment of Pneumothorax
• All patients who smoke should be advised to discontinue smoking
and warned that the risk of recurrence is 50%. Future exposure to
high altitudes, flying in unpressurized aircraft, and scuba diving
should be avoided.
• Indications for thoracoscopy or open thoracotomy include
recurrences of spontaneous pneumothorax, any occurrence of
bilateral pneumothorax, and failure of tube thoracostomy for the
first episode (failure of lung to reexpand or persistent air leak).
Surgery permits resection of blebs responsible for the
pneumothorax and pleurodesis by mechanical abrasion and
insufflation of talc.
Treatment of Pneumothorax
• Management of pneumothorax in patients with Pneumocystis
pneumonia is challenging because of a tendency toward
recurrence, and there is no consensus on the best approach.
• Use of a small chest tube attached to a Heimlich valve has been
proposed to allow the patient to leave the hospital.
