
1
4th stage
Medicine
Lec-11
د. ظاهر1/1/2016
APPROACH TO PATIENT WITH RESPIRATORY DISEASE AND
PHYSICAL EXAMINATION
Examination of the patient with suspected pulmonary disease includes inspection,
palpation, percussion, and auscultation of the chest.
An efficient approach begins with observing the pattern of breathing, auscultation of the
chest, and inspection for extrapulmonary signs of pulmonary disease. More detailed
examination follows from initial findings
Extrapulmonary signs of intrinsic pulmonary disease
Include digital clubbing, cyanosis, elevation of central venous pressures, and lower
extremity edema.
Digital clubbing refers to structural changes at the base of the nails that include
softening of the nail bed and loss of the normal 150-degree angle between the nail
and the cuticle.
The distal phalanx is convex and enlarged: its thickness is equal to or greater than the
thickness of the distal interphalangeal joint.
Hypertrophic pulmonary osteoarthropathy is a syndrome of digital clubbing, chronic
proliferative periostitis of the long bones, and synovitis.
It is seen in the same conditions as digital clubbing but is particularly common in
bronchogenic carcinoma.
The cause of clubbing and hypertrophic osteoarthropathy may reflect platelet
clumping and local release of platelet-derived growth factor at the nail bed.
Cyanosis is a blue or bluish-gray discoloration of the skin and mucous membranes
caused by increased amounts (> 5 g/dL) of unsaturated hemoglobin in capillary blood.
Cyanosis is therefore not a reliable indicator of hypoxemia but should prompt direct
measurement of arterial PO2 or of hemoglobin saturation
Estimation of central venous pressure (CVP) and assessment of lower extremity
edema are indirect measures of pulmonary hypertension, the major cardiovascular
complication of chronic lung disease.
Elevated CVP is a pathologic finding associated with impaired ventricular function,
pericardial effusion or restriction, valvular heart disease, and chronic obstructive or
restrictive lung disease.
Peripheral edema is a nonspecific finding that, in the setting of chronic lung disease,
suggests right ventricular failure
Look for any obvious chest or spine deformities.

2
These may arise as a result of chronic lung disease (e.g. emphysema), occur
congenitally, or be otherwise acquired.
Pectus excavatum: Congenital posterior displacement of lower aspect of sternum.
This gives the chest a somewhat "hollowed-out" appearance. The x-ray shows a
subtle concave appearance of the lower sternum.
The pattern of breathing refers to the respiratory rate and rhythm, the depth of
breathing or tidal volume, and the relative amount of time spent in inspiration and
expiration.
Normal values are a rate of 12–14 breaths per minute, tidal volumes of 5 mL/kg, and
a ratio of inspiratory to expiratory time of 2:3.
Tachypnea is an increased rate of breathing and is commonly associated with a
decrease in tidal volume.
Respiratory rhythm is normally regular, with a sigh (1.5–2 times normal tidal volume)
every 90 breaths or so to prevent collapse of alveoli and atelectasis.
Alterations in the rhythm of breathing include rapid, shallow breathing, seen in
restrictive lung disease and as a precursor to respiratory failure
Kussmaul :breathing, rapid large volume breathing indicating intense stimulation of
the respiratory center, seen in metabolic acidosis.
Cheyne-Stokes respiration, a rhythmic waxing and waning of both rate and tidal
volumes that includes regular periods of apnea. This last pattern is seen in patients
with end-stage left ventricular failure or neurologic disease and in many normal
persons at high altitude, especially during sleep.
During normal quiet breathing, the primary muscle of respiration is the diaphragm.
Movement of the chest wall is minimal.
The use of accessory muscles of respiration, the intercostal and sternocleidomastoid
muscles, indicates high work of breathing.
At rest, the use of accessory muscles is a sign of significant pulmonary impairment.
As the diaphragm contracts, it pushes the abdominal contents down.
Hence, the chest and abdominal wall normally expand simultaneously.
Expansion of the chest but collapse of the abdomen on inspiration indicates
weakness of the diaphragm.
Chest examination
o The chest normally expands symmetrically. Asymmetric expansion suggests unilateral
volume loss, as in atelectasis or pleural effusion, unilateral airway obstruction,
asymmetric pulmonary or pleural fibrosis, or splinting from chest pain.
o The palpation as follows:
o The trachea at the suprasternal notch, to detect shifts in the mediastinum; on the
posterior chest wall, to gauge fremitus and the transmission through the lungs of
vibrations of spoken words; and on the anterior chest wall to assess the cardiac
impulse.
3
o All these maneuvers are characterized by low interobserver agreement
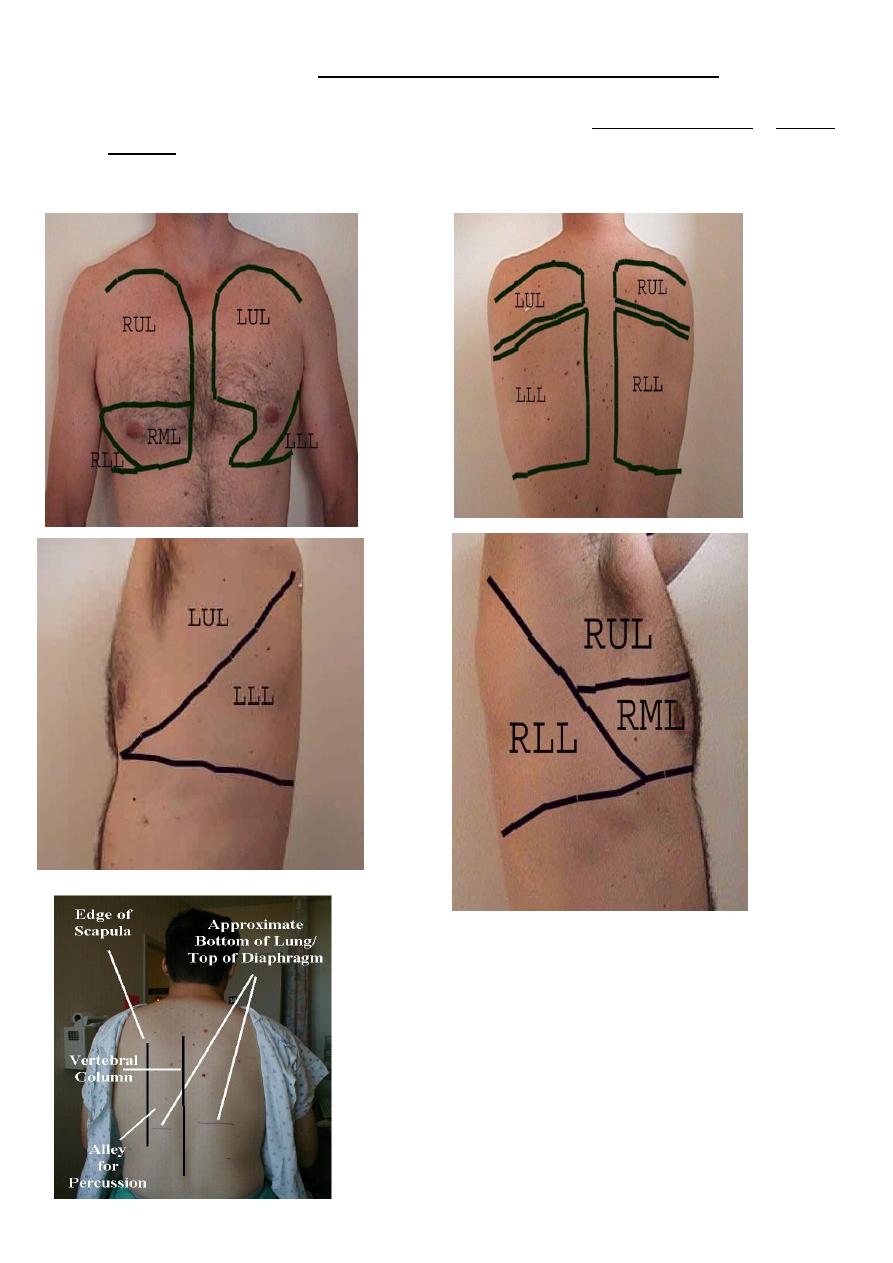
o Chest percussion identifies dull areas that correspond to lung consolidation or pleural
effusion .
o Hyperresonant areas suggesting emphysema or pneumothorax.

4
Auscultation of the chest
Normal lung sounds heard over the periphery of the lung are called vesicular.
They have a gentle, rustling quality heard throughout inspiration that fades during
expiration.
Normal sounds heard over the suprasternal notch are called tracheal or bronchial lung
sounds. They are louder, higher-pitched, and have a hollow quality that tends to be louder
on expiration.
Bronchial lung sounds heard over the periphery of the lung are abnormal and imply
consolidation.
Globally diminished lung sounds are an important finding predictive of significant airflow
obstruction.
Abnormal lung sounds (“adventitious” breath sounds) may be continuous (> 80 ms in
duration) or discontinuous (< 20 ms).
Continuous lung sounds are divided into (a)wheezes, which are high-pitched, musical, and
have a distinct whistling quality.
Wheezes occur in the setting of bronchospasm, mucosal edema, or excessive secretions.
(b) Rhonchi, which are lower-pitched, sonorous, and may have a gurgling quality. Rhonchi
originate in the larger airways when excessive secretions and abnormal airway collapsibility
cause repetitive rupture of fluid films.
Rhonchi frequently clear after cough.
In each case(wheezes or Rhonchi),the airway is narrowed to the point where adjacent
airway walls flutter as airflow is limited.
Discontinuous lung sounds are called crackles— brief, discrete, nonmusical sounds with a
popping quality.
Fine crackles are soft, high-pitched, and crisp (< 10 ms in duration).
They are formed by the explosive opening of small airways previously held closed by
surface forces and are heard in interstitial diseases or early pulmonary edema.
Coarse crackles are louder, lower-pitched, and slightly longer in duration (< 20 ms) and
probably result from gas bubbling through fluid.
Coarse crackles are heard in pneumonia, obstructive lung disease, and late pulmonary
edema.
The timing and character of crackles can reliably distinguish different pulmonary disorders.
Fine, late inspiratory crackles suggest pulmonary fibrosis, while early coarse crackles suggest
pneumonia or heart failure.
