1
Forth stage
Medicine
Lec-2
د.فاخر
1/1/2102
Pituitary gland
The pituitary is located at the base of the brain, in
a small depression of the sphenoid bone (sella
turcica).
Purpose: control the activity of many other
endocrine glands “ Master gland”
Has two lobes, the anterior & posterior lobes.
Boundaries :-
1- Superiorly : optic chiasma
2- Inferiorly : sphenoidal sinuses
3- Lateral : cavernous sinuses ( contain 3
rd
, 4
th
and 6
th
cr. Nerves + internal carotid artery )
Structure :-
Composed of anterior and posterior lobes , connected to pituitary by infundibular
stalk , portal vessels carry blood from hypothalamus to anterior lobe of pituitary
nerve fibers to posterior lobes .
Physiology :-
• Hormones secreted from anterior pituitary(controlled by substances
produced in hypothalamus and released into portal blood flow down pit
stalk)
1. LH,FSH
2. TSH
3. Prolactin
4. GH
5. ACTH
• Hormones secreted from post pituitary (synthesized in hypothalamus and
transported through nerve axon down to be released from pos pit gland
1. ADH (anti diuretic hormone ) 2. Oxytosin

2
Anatomy :-
• Anterior lobe: glandular tissue, accounts for 75%
of total weight. Hormones in this lobe are
controlled by regulating hormones from the
hypothalmus (stimulate or inhibit)
• Posterior: nerve tissue & contains axons that
originate in the hypothalmus. Therefore this lobe
does not produce hormones but stores those
produced by the neurosecretory cells in the
hypothalmus. Release of hormones is triggered by
receptors in the hypothalmus.
Anterior Pituitary Secretes :
• GH:stimulates growth of bone and muscle , promotes protein synthesis and
fat metabolism.
• ACTH(Adrenocorticotropin ): stimulates adrenal gland cortex secretion of
mineralcorticoids (aldosterone) & glucocorticoids (cortisol).
• TSH: stimulates thyroid to increase secretion of thyroxine, its control is
from regulating hormones in the hypothalmus
• Prolactin:stimulates milk production from the breasts after childbirth to
enable nursing. Oxytoxin from posterior lobe controls milk ejection.
• FSH: promotes sperm production in men and stimulates the ovaries to
enable ovulation in women. LH and FSH work together to cause normal
function of the ovaries and testes.
• LH: regulates testosterone in men and estrogen, progesterone in women.
Posterior Pituitary secrets :
• Antidiuretic hormone or ADH - also called vasopressin, vasoconstricts
arterioles to increase arterial pressure; increases water reabsorption in distal
tubules.
• Oxytocin: stimulates uterus to contract at childbirth; stimulates mammary
ducts to contract (milk ejection in lactation).
3
Presenting problems in hypothalamic and pituitary diseses
A-Hypopituitarism
1-anterior pituitary hormone deficiency
• Combined deficiency of any of the ant pituitary hormones.
• Clinical presentation vary.
• Most common cause is pituitary macroadenoma
Causes of ant pituitary hormone deficiency :
1.Structuralprimary pit tumor
Adenoma, carcinoma, Craniopharyngioma, Meningioma, Heamorrhage
(apoplexy), Langerhans cell histocytosis, Arachnoid cyst, Secondary tumour
(leukemia, lymphoma), Chordoma
2.Inflammatory / infiltrative
sarcoidosis, haemochromatosis, infections (pit abscess, TB,
syphlis,encephalitis).
3.Congenital deficiencies
GnRh (kallmann’s syndrome), TRH, GHRH, CRH
4
4. Functional
chronic systemic illness, excessive excersise, anorexia nervosa
5.Other
head injury, parasellar radiotherapy and surgery, post partum necrosis
(Sheehan's syndrome)
Clinical assessment
1-Progressive loss of pit. functions in following consequences
- GH :
-
Lethargy, muscle weakness, increased fat mass
-Gonadotrophines (LH,FSH) :
Loss of libido,
in male
gynecomastie, decrease shaving
oligomenorrhea or amenorrhea
in female
absent pubic hair in both sexes with
fine & wrinkled skin
chronic anemia
- ACTH (loss of cortisol, with maintenance of aldosteron )
hyponatremia and postural hypotension with normal K+
pallor due to lack of melanocyte stimulation by B-Lipotrophic hormone
-TSH (Secondary hypothyroidism)
apathy and cold intolerance
2. Acute presentation
* acute glucocorticoid deficiency ppt by infection or injury
* in secondary apoplexy.

5
Investigations :
1- ACTH deficiency
Short ACTH stimulation test Insulin tolerance test only if uncertainty in
interpretation of short ACTH stimulation test (e.g. acute presentation)
2- LH/FSH deficiency
In the male, measure random serum testosterone, LH and FSH
In the pre-menopausal female, ask if menses are regular
In the post-menopausal female, measure random serum LH and FSH (which
would normally be > 30 mU/L)
3- TSH deficiency
Measure random serum T4
Note that TSH is often detectable in secondary hypothyroidism, due to inactive
TSH isoforms in the blood
4- Growth hormone deficiency
Only investigate if growth hormone replacement therapy is being contemplated
Measure immediately after exercise
Consider other stimulatory tests
2-posterior pituitary hormone deficiency :
- Cranial diabetes insipidus
Only investigate if patient complains of polyuria/polydipsia, which may be
masked by ACTH or TSH deficiency
- Exclude other causes of polyuria with blood glucose, potassium and
calcium measurements
- Water deprivation test or 5% saline infusion test
6
Management :
A-Chronic hormone replacement therapy:
1. Cortisol replacement (hydrocortisone )
2. Thyroid hormone replacement (thyroxin 100-150 microgram)
3. Sex hormone replacement (restore normal sexual function and prevent
osteoporosis)
4. GH Replacment
- daily subcutaneous self injection of GH to children and adolescents before
epiphysis fusion
- can be given in some adults
-monitoring by measurement of serum insulin like growth factor (IGF-1)
-Side effects Na retention with peripheral edema ad carpal- tunnul syndome
B- Identify hormone excess :
Hyperprolactinemia ,
Acromegaly ,
Cushing’s syndrome
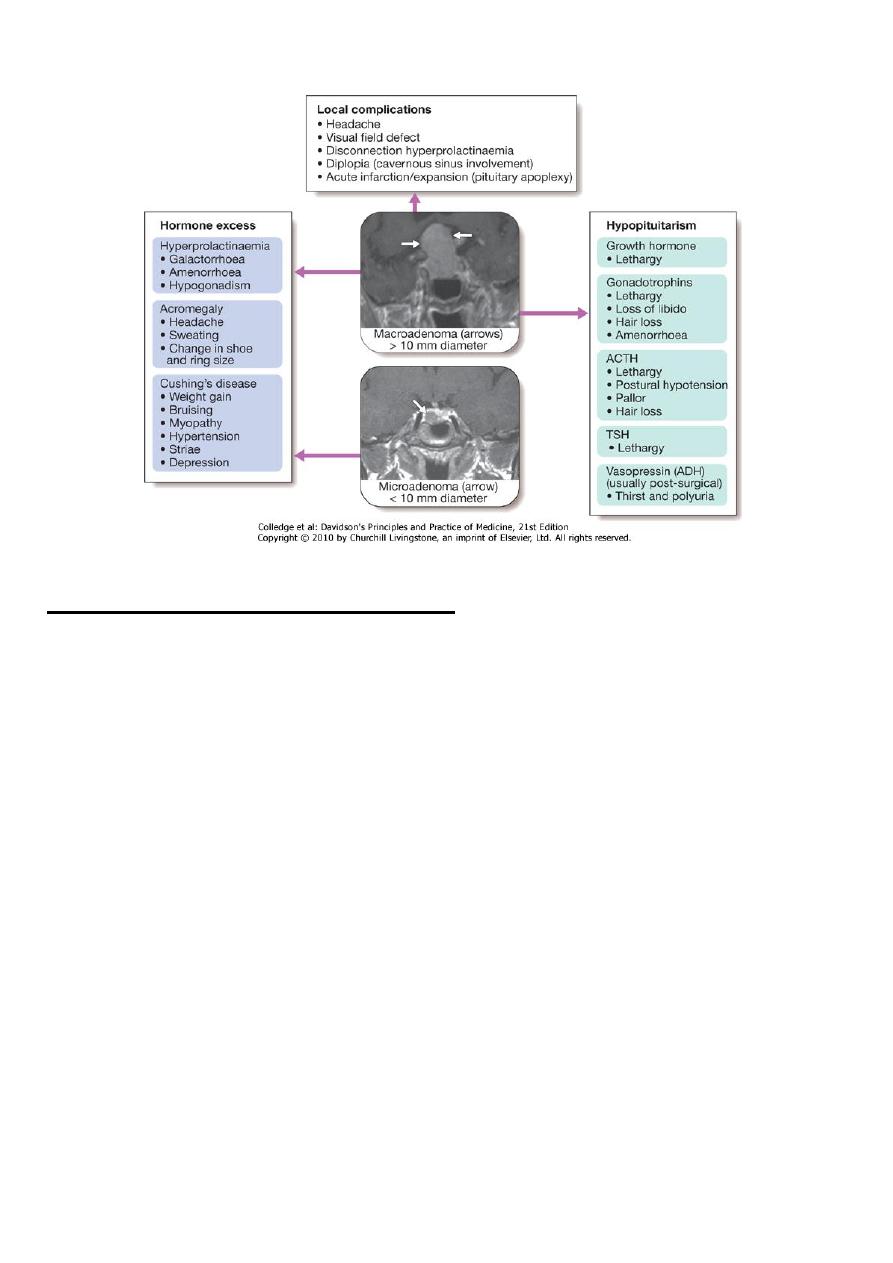
PITUITARY TUMOUR :
Way of presentation:
• Mass effect depending on size and location
- most intraseller tmors are macroadenoma
- majority of extrasellar tumors are craniophryngiomas
- most paraseller masses are meningiomas
• Incidentally by CT or MRI
Clinical presentation :
1-Headache
2-Visual field defect

7
*bitemporal hemianopia, or upper quadrianopia (optic chiasma compression)
* unilateral loss of acuity or scotoma (optic n compression due to supraseller
extension of tumour)
*homonymous hemianopia (optic tract compresion)
3- Optic atrophy by fundoscopy
4- Diplopia and strabismus
(compression on 3rd, 4th, and 6th cranial n due to lat extension to cavernous
sinus)
5-Acute onset hypopituitarism due to apoplexy
(bleeding into cystic lesion, or tumour infarct)
6-Non hemorrhagic infarction in a normal pit
)Obstetric hmg (Sheehan's syndrome
DM
Inc intracranial pressure
Investigations :
• MRI or CT scan for suspected patients
• Biopsy for definite diagnosis (at time of operation)
Management :
1- Treatment of associated hypopituitarism
2- Urgent management for visual pathway pressure (within 4 months)
*measure prolactin first if >5000 mU/L with suspicion of macroprolactinoma
then trial of dopamine agonist surgery
3- Surgical approach
* Trans-sphenoidal approach via nostrils in most cases
* Trans-frontal via craniotomy for suprasellar t
* Repeat pit function tests 4-6 wk following surgery
* Repeat imaging after few months
8
4- External radiotherapy
*for radiosensitive tumours,
*avoid in emergency condition
*risk of hypopit in 50-70%
*impair cognitive functions, cause vascular changes, induce primary brain
tumours
5- For nonfunctioning tumours
*repeated imaging
SH.J
