
1
Forth stage
Medicine
Lec-5
د.فاخر
1/1/6102
Adrenal disorders
-Cortisol is a normal hormone produced in the outer portion, or cortex, of the adrenal
glands, located above each kidney. The normal function of cortisol is to help the body
respond to stress and change. It mobilizes nutrients, modifies the body’s response to
inflammation, stimulates the liver to raise the blood sugar, and it helps control the amount
of water in the body. Another adrenal cortex hormone, aldosterone, regulates salt and
water levels which affects blood volume and blood pressure. Small amounts of androgens
(male hormones) are also normally produced in the adrenal cortex. Cortisol production is
regulated by adrenocorticotrophic hormone (ACTH), made in the pituitary gland, which is
located just below the brain.
-Catechalomines: Activity
Stimulates the “fight or fight” reaction
Increased plasma glucose levels
Increased cardiovascular function
Decreased gastrointestinal and genitourinary function
- The adrenal gland is divided into two parts, adrenal cortex and medulla.
The adrenal cortex secretes androgen, mineralocorticoids (eg, aldosteron) and
glucocorticoids (eg, cortisol).
The adrenal medulla secretes catecholamines (eg, epinephrine, norepinephrine,
dopamine).
MEDULLA -----> sympathetic system
CORTEX--->
Zona Glomerulosa-Renin-Angiotensin-Aldosterone Axis
Zonae Fasciculata/Reticularis-Hypothalamic –pituitary-Adrenal Axis
-Steroid actions
Amino acid catabolism (muscle wasting)… gluconeogenesis in the liver..
Hyperglycemia… increased insulin output… eventual beta cell failure… fat
deposition… diabetes
Ca resorption, impairment of Ca absorbtion, increased renal Ca excretion….
osteoporosis
Increased gastric acidity… ulcer formation or aggravation
K loss and Na retention… edema and hypertension
2
Initially increased antibody release.. Eventually decreased antibody production,
lymphocytopenia, eosinopenia, neutrophelia, polycythemia… susceptibility to
infections
Maintenance of arteriolar tone and blood pressure
-Mineralocorticoids
Aldosteron is primarily involved with fluid and electrolyte balance
The principle stimulus for aldosterone is angiotensin ll.
Aldosteron secretion causes sodium reabsorption in the distal renal tubule in
exchange for potassium and hydrogen ions.
The net effects are, fluid retention, decrease in plasma potassium and metabolic
alkalosis.
Cushing’s Syndrome
-Excessive stimulation of glucocorticoid receptors
-Most common --> iatrogenic (predinisolone)
- rare ---> Non-iatrogenic
Aetiology
ACTH –dependent
Pit. Adenoma secreting ACTH(Cushing disease)
Ectopic ACTH(bronchial carcinoid, small -cell lung Ca)
Iatrogenic (ACTH therapy)
Non-ACTH –dependent
Iatrogenic (Chronic steroid therapy)
Adrenal adenoma
Adrenal carcinoma
Pseudo-cushings syndrome(cortisol excess as part of another
illness)
Alcohol excess
Major depressive illness
Primary obesity
3
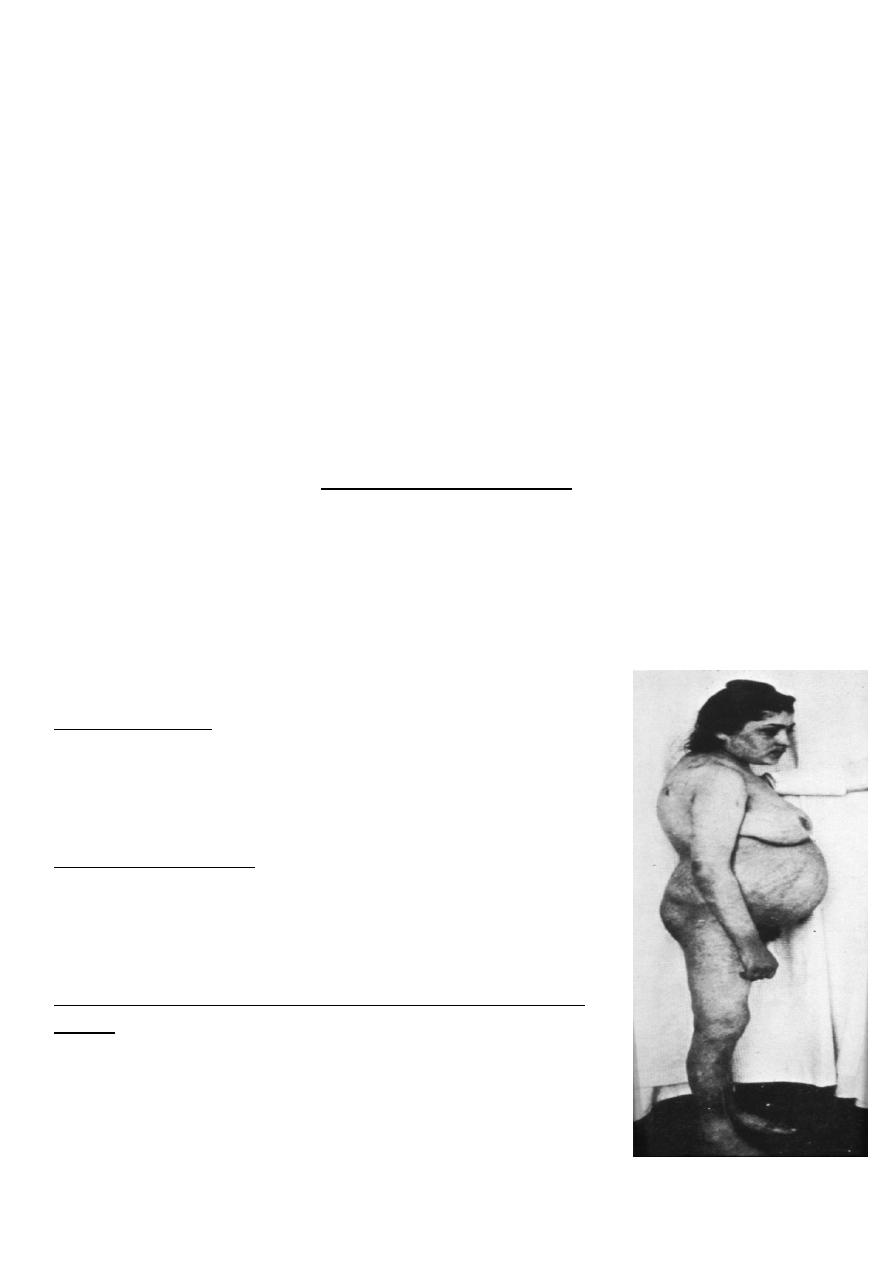
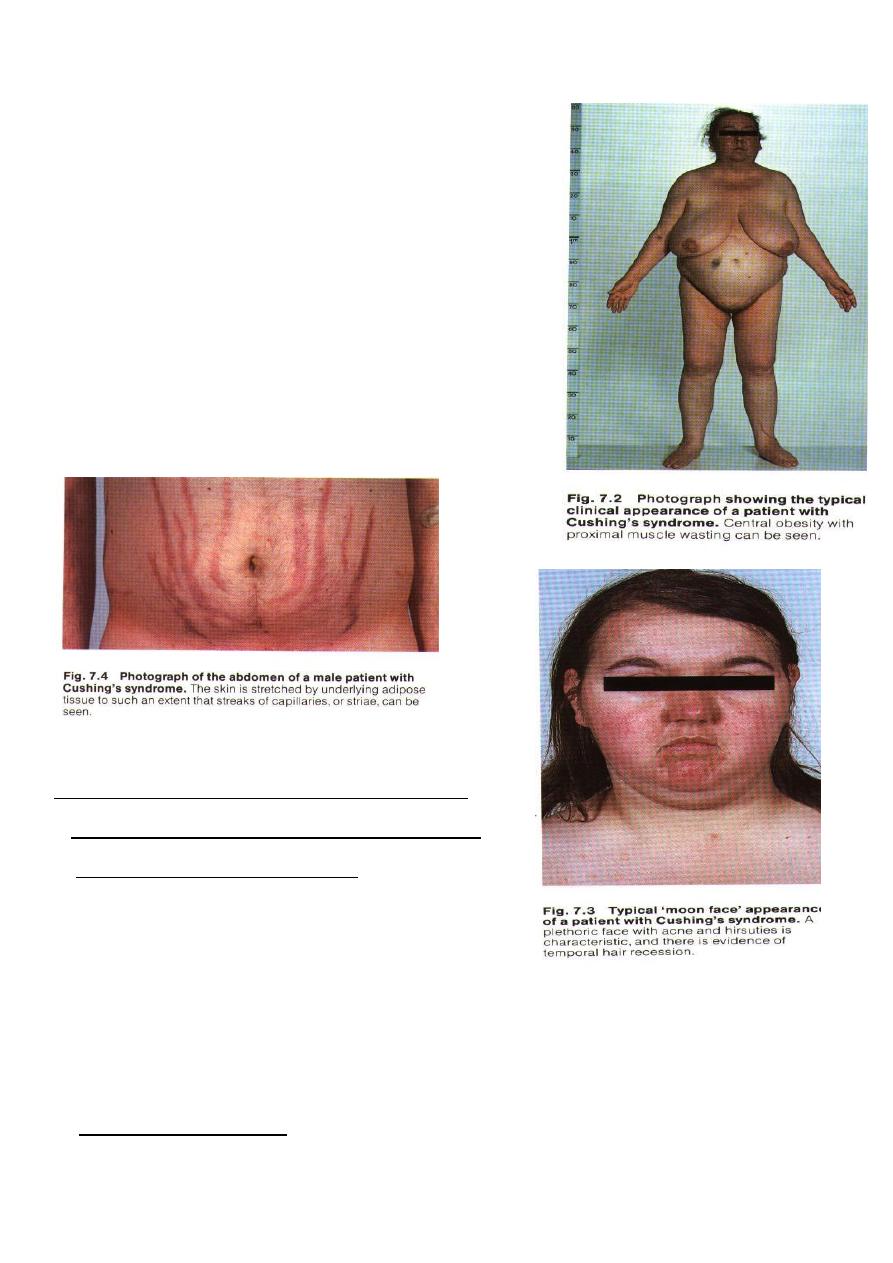
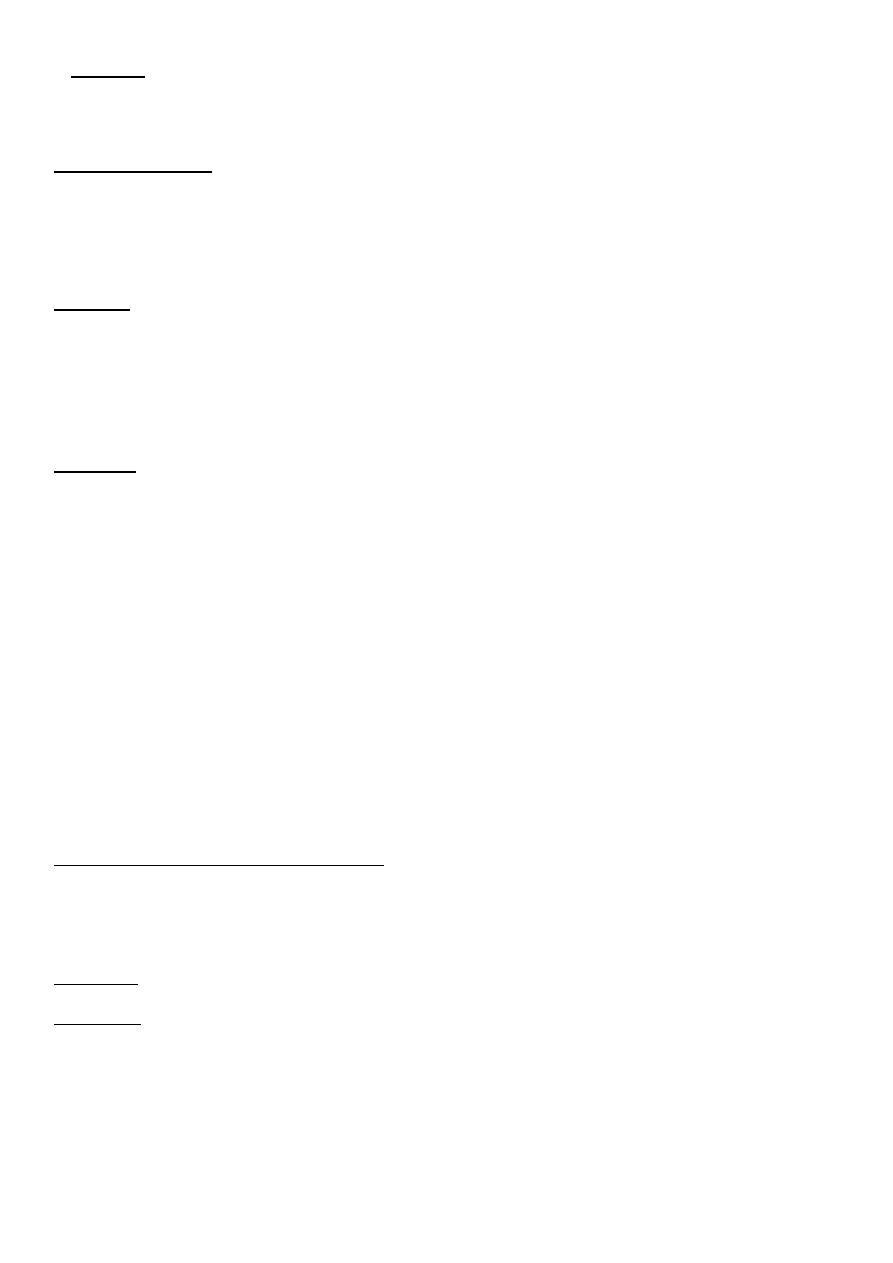
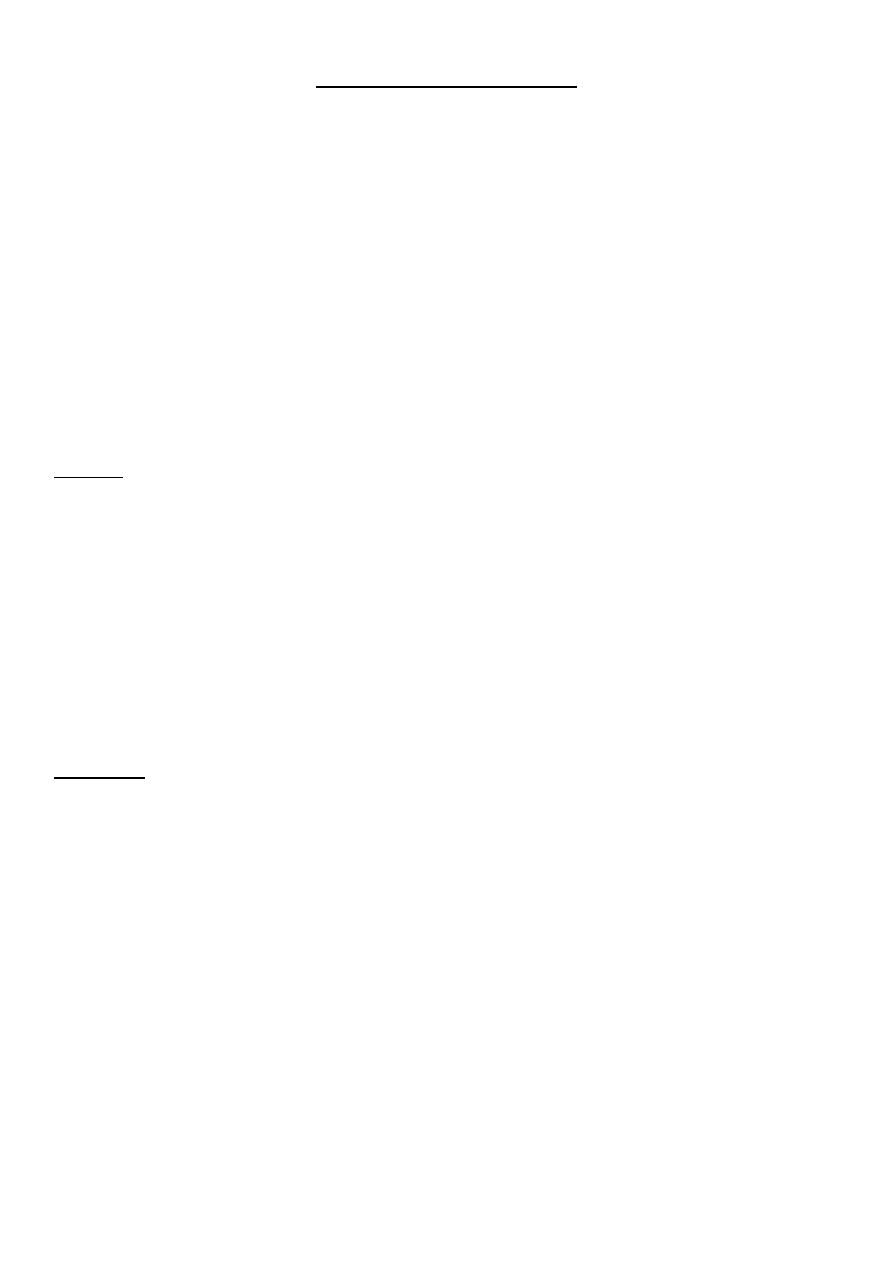
Major Clinical Features in Cushing’s Syndrome
1. Weight gain, Central obesity
2. Moon face and plethora
3. Muscular weakness, especially proximal
4. Depression and psychosis
5. Oligomenorrhoea or amenorrhoea in females
6. Hirsuties
7. Striae, acne, skin-thinning, bruising
8. Polyuria, nocturia
9. decreased libido and impotence in males
10. Hypertension
11. diabetes or impaired glucose tolerance
12. Loss of height and osteoporosis
investigations
1-Biochemical evaluation of Cushing syndrome:
a-Urinary free cortisol excretion over 150 ug\ day.
b- dexamethasone suppression test
glucocorticoids inhibit secretion of hypothalamic CRH
and pituitary ACTH but do not directly affect adrenal
cortisol production. The overnight 1-mg
dexamethasone suppression test requires administration of 1 mg of dexamethasone at
11 PM with subsequent measurement of cortisol level at 8 am.4 In healthy individuals, the
serum cortisol level should be less than 2.2 ug/dL (exclude cushing).
c- loss of circadian rhythm of cortisol secretion
Normal values, 10-25 ug\ml in the morning, 2-10 ug\ml in the evening, elevated serum
cortisol at 11 PM can be an early finding.
4
d-Recently, measuring salivary cortisol level has gained interest, as it is a simple and
convenient way of obtaining a nighttime sample. levels less than 1.3-1.5 ng/mL exclude
Cushing syndrome.
2-Imaging studies
CT or MRI brain and abdomen
Chest X ray
Chest CT
3-Others
Tumour markers
Treatment
SURGERY
*Transsphenoidal removal of pituitary tumors, or Bi-adrenalectomy ..
*Pituitary irradiation is employed when transsphenoidal surgery is not successful or
not possible
Adrenal tumour Lap.removal
Patients with endogenous Cushing syndrome who undergo resection of pituitary,
adrenal, or ectopic tumors should receive stress doses of glucocorticoid in the
intraoperative and immediate postoperative period
*lifelong glucocorticoid and mineralocorticoid replacement is necessary in those
patients who undergo bilateral adrenalectomy.
MEDICAL(Metyrapone, Ketoconazole)
Few weeks prior to surgery
Non-resectable tumour
Radiation
Cytotoxic
5
Adrenal Insufficiency
Pathophysiology
-Addison disease is adrenocortical insufficiency due to the destruction or dysfunction of the
entire adrenal cortex. It affects glucocorticoid and mineralocorticoid function. The onset of
disease usually occurs when 90% or more of both adrenal cortices are dysfunctional or
destroyed.
-Frequency : The prevalence of Addison disease is 40-60 cases per 1 million population.
-Age :The most common age at presentation in adults is 30-50 years.
-Sex :Idiopathic autoimmune Addison disease tends to be more common in females and
children.
Causes of Adrenal Insufficiency
Primary
1. Idiopathic (Addison disease)
2. Tuberculosis
3. Fungal infections
4. Adrenal hemorrhage
5. Congenital adrenal hyperplasia
6. Sarcoidosis
7. Amyloidosis
8. Metastatic neoplasia
9. Others
Secondary
1. After exogenous glucocorticoids
2. After the cure of Cushing syndrome (removing endogenous glucocorticoids)
3. Hypothalamic and pituitary lesions
Major Clinical Features in Adrenal Insufficiency
1. Weakness
2. Skin : Mucous membrane and skin pigmentation, darkening of hair freckling, vitiligo,
pigment accentuation at nipples, and friction areas, pigment concentration in skin
creases and in scars
3. Loss of weight, emaciation, anorexia, vomiting, diarrhea
4. Hypotension
5. Salt craving
6. Hypoglycemic episodes
6
7. Acute Adrenal crises
a) Acute circulatory shock
b) Sever hypotension ,hyponatremia ,Hyperkalemia and in some cases hypoglycemia
,hypercalcemia.
c) cramps, vomiting, diarrhea ,unexplained fever may be present.
d) Often pp by infection or surgery
Investigations
1-Random plasma cortisol
2-Short ACTH stimulation test; In patients with Addison disease, both cortisol and
aldosterone show minimal or no change in response to ACTH.
3-ACTH assay
4-Plasma renin activity and aldosterone
5-Lab tests
hyponatremia
Hyperkalemia
metabolic acidosis
6-elevated (BUN) and creatinine due to the hypovolemia with decreased glomerular
filtration rate.
7-Hypoglycemia
8-adrenal autoantibodies may be present
9-Imaging study
Chest x-ray-- TB
CT abdomen
Treatment
-The goals of pharmacotherapy are to reduce morbidity and to prevent complications e.g
adrenal crisis;
1- corticosteroid replacement (Cortisol 15mg am 5mg pm )
2- mineralocorticoid ( Fludrocortisone 0.05-0.1 mg PO qd; some patients may only require
alternate-day dosing).
3-In acute adrenal crises ---> medical emergency !!
IV hydroctisone and IV fluids (NS and 10% dextrose +treat pp factor )
