
1
4th stage
Obstetrics
Lec
Dr.Ahmad
3/16/2016
Induction
OF labour
Labour induction:
is the process of artificially initiating uterine contraction prior to their spontaneous
onset , leading to cervical dilatation, effacement and delivery of the baby.
The term generally referred to pregnancy after 24 weeks of gestation.
Augmentation of labour (acceleration):
the attempt to assists or accelerate labour that have been already begun normally.
Labour is the onset of regular , painful uterine contractions associated with dilatation
of the cervix and descent of the presenting part.
Indication of induction :
The purpose of an induction is to achieve benefit to the health of mother and / or
baby, which must be exceed that to be gained by continuing pregnancy (excluding
planned caesarean delivery).
It should only performed if there is a reasonable chance of success and if risks of
process to the mother and / or fetus are acceptable. If either of these is not the case,
a planned caesarean section should be performed instead.
Induction is indicated when the continuance of pregnancy may no longer be advisable
in the following clinical circumstances:
1. prolonged pregnancy.
2. Intrauterine fetal death .
3. intra uterine growth restriction (IUGR).
4. oligohydramnios due to placental insuffiency.
5. hypertensive disorder with pregnancy (pre-eclampsia, eclampsia).
6. Deteriorating maternal illness.

2
7. Prolonged PROM
8. Unexplained antepartum haemorhage.
9. Diabetes mellitus.
10. Gestational hypertension.
11. Rh isoimmunization.
12. Chorioamnionitis .
13. Logistic factors (e.g., history of rapid labour, distance from hospital) .
Contraindications
1. Malpresentations (e.g., transverse or oblique lie, footling breech).
2. Absolute cephalo-pelvic disproportion .
3. Placenta previa .
4. Previous major uterine surgery or classical Caesarean section.
5. Invasive carcinoma of the cervix.
6. Prolapsed cord.
7. Active genital herpes.
8. Gynecological, obstetrical, or medical conditions that preclude vaginal delivery
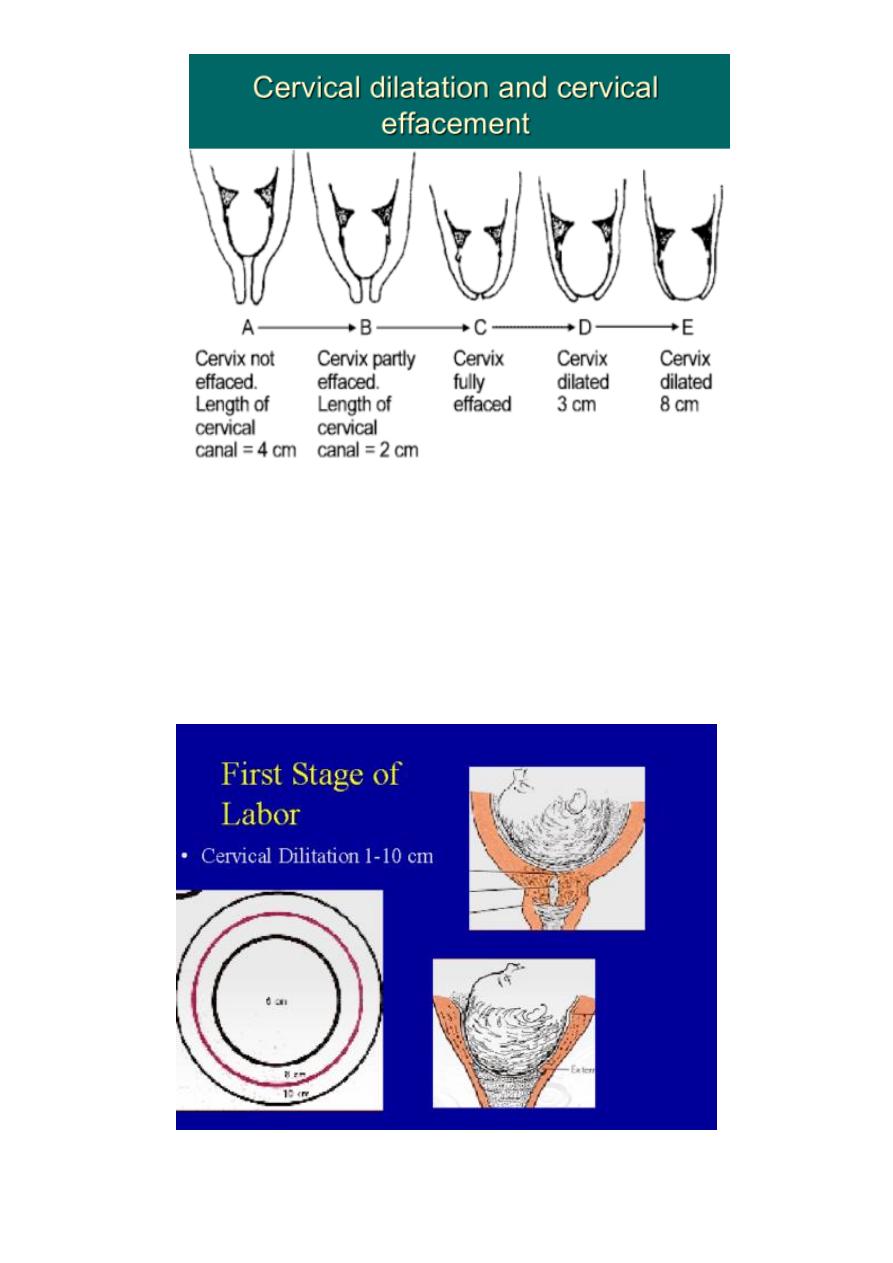
Cervical changes during pregnancy :
During pregnancy the cervix remains firm and closed to ensure the integrity of the
pregnancy , in the last few weeks of pregnancy the cervix become softer, shorter
moves forward and starts to dilate as natural preparation for labour.
The effect of the upper segment muscle is to stretch and thin the lower segment and
cause effacement and dilatation of cervix.
3
Cervical effacement:
process of inclusion of the length of the cervix into the lower uterine segment of the
uterus, which is normal process in the last few weeks of pregnancy and is necessary
preparation for the onset of spontaneous labour.
This process greatly facilitate labour and augment the chance of the vaginal delivery .
4
Cervical ripening assessment :
induction of labour is a common obstetric procedure where the state of the cervix is clearly
related to the success of labour induction , duration of labour and likelihood of vaginal
delivery
.
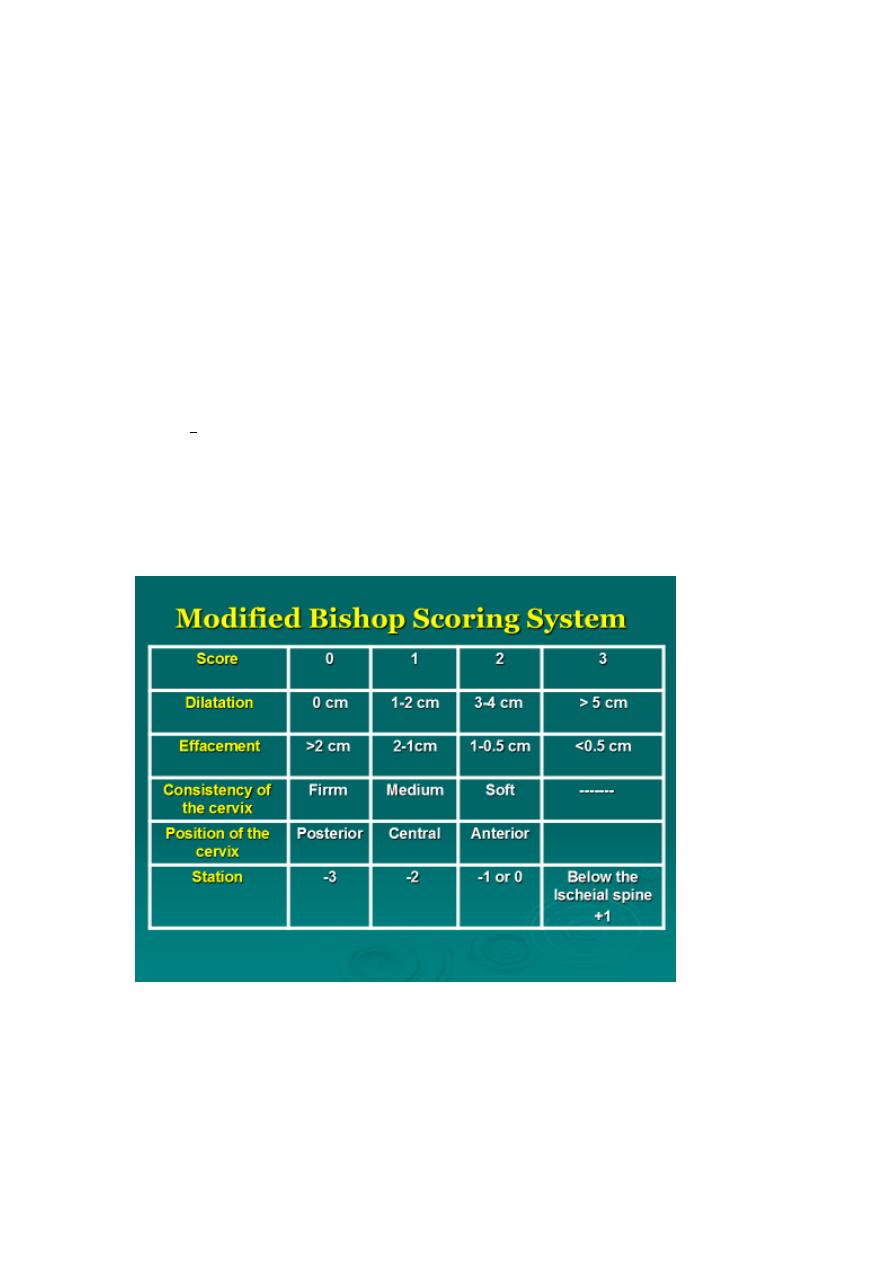
1. Modified Bishop Score :
This score is predicting for the succession of induction of labour.
The total score is in the range of 0-13, a score of 9 or more is favourable for successful
induction.
High scores (9 to 13) (favourable cervix) are associated with an easier, shorter
induction that is less likely to fail.
Low scores (less than 5) (unfavourable cervix) point to longer induction that is more
likely to fail.
2. transvaginal sonography:
the presence of cervical wedging and decrease cervical
length before induction was associated with shorter latent phase and shorter labour.
5
3. fibronectin level:
fetal fibronectin might be a marker of the cervical changes and
readiness for labour .
BUT the Bishop score still the most widely used method for cervical assessment before
induction as it is inexpensive, readily available and correlates well with induction success.
General principles related to the practice of induction of labour :
Induction of labour should be performed only when there is a clear medical indication
for it and the expected benefits outweigh its potential harms.
consideration must be given to the actual condition, wishes of woman, with emphasis
being placed on cervical status, the specific method of induction of labour and
associated conditions such as parity and rupture of membranes.
Induction of labour should be performed with caution since the procedure carries the
risk of uterine hyperstimulation and rupture and fetal distress.
Wherever induction of labour is carried out, facilities should be available for assessing
maternal and fetal well-being.
Failed induction of labour does not necessarily indicate caesarean section.
Wherever possible, induction of labour should be carried out in facilities where
caesarean section can be performed.
Where induction is essential for severe fetal or maternal problems, it should be
attempted regardless of the ripeness of the cervix after attempts to soften it with local
prostaglandins. in this situation if the induction fails, Casearean section is reasonable
whereas if an induction is successful, Caesarean section has been satisfactorily avoided.
6
Management of induced labour:
Assessments before induction of labour:
Assessment of gestational age and consideration of potential risks to the mother or
fetus.
Assess indication of induction.
Fetal lie and presentation by abdominal examination and assess the well-being of fetus.
Pelvic assessment.
Assess condition of cervix (Bishop's score).
Blood type and screen for antibodies and cross match.
Methods of induction of labour:
The more remote from term, the more difficult induction of labour will be frequently
requiring more than one technique over a period of a few days.
Those employed by women that do not require medical prescription: caster oil,
acupuncture, breast nipple stimulation, sexual intercourse.
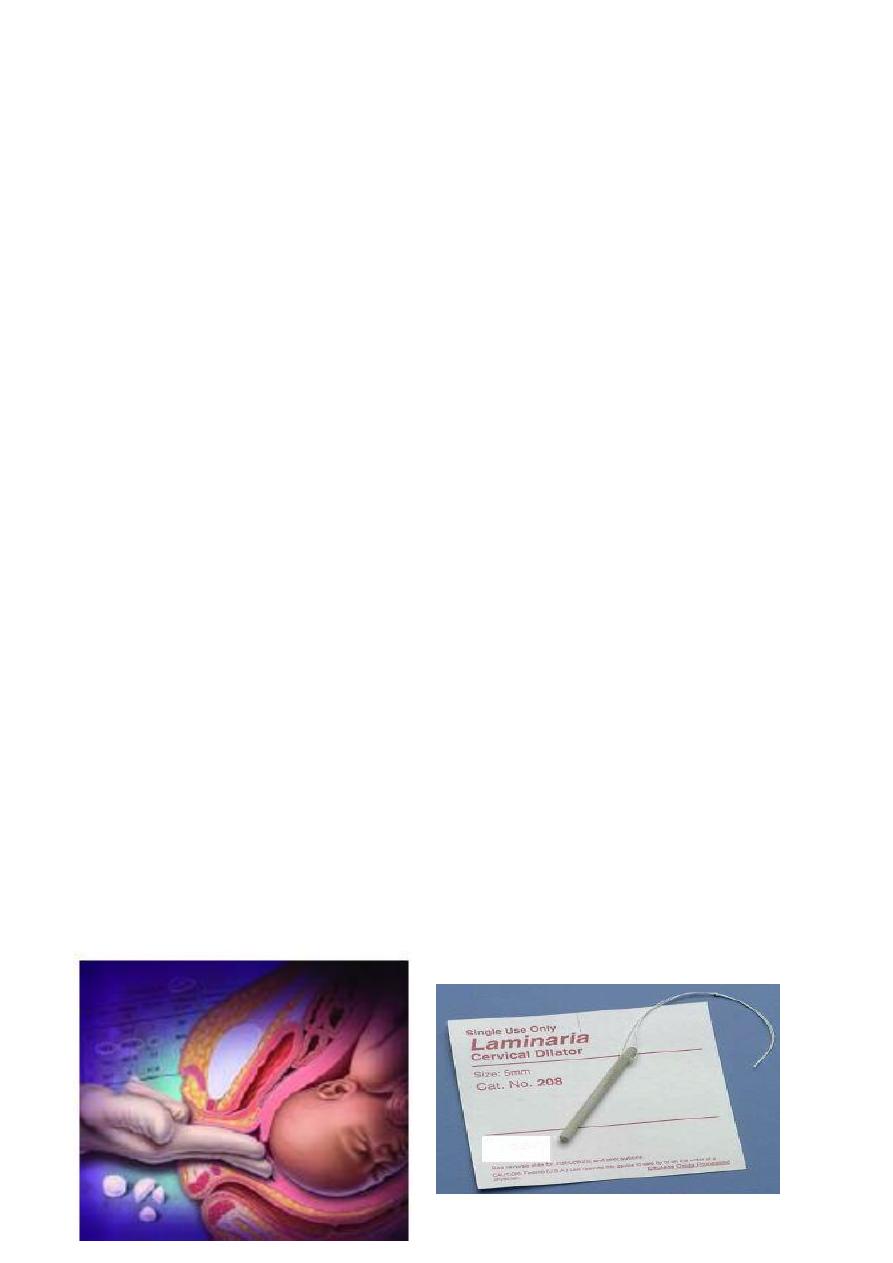
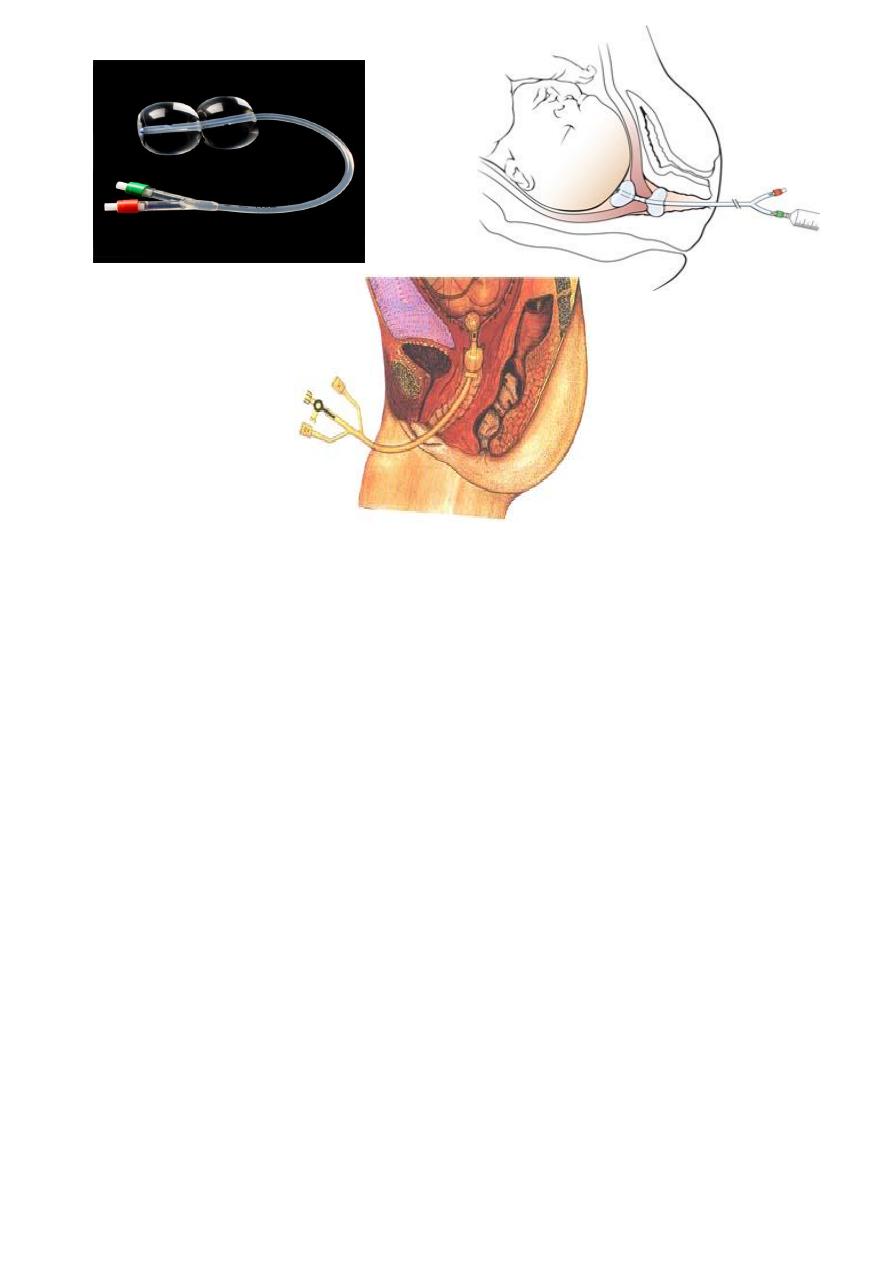
Mechanical force to promote cervical effacement and dilatation and initiation of
uterine contractionsmembrane sweeping, hygroscopic (synthetic osmotic dilators
(e.g., Lamicel)) and mechanical dilators (Balloon devices), extra-amniotic infusion of
saline, Amniotomy.
All have a similar mechanism of action as it exert local pressure that stimulates the
release of prostaglandins.
7
The risks associated with these methods include:
1. infection (endometritis and neonatal sepsis).
2. Bleeding
3. membrane rupture
4. placental disruption.
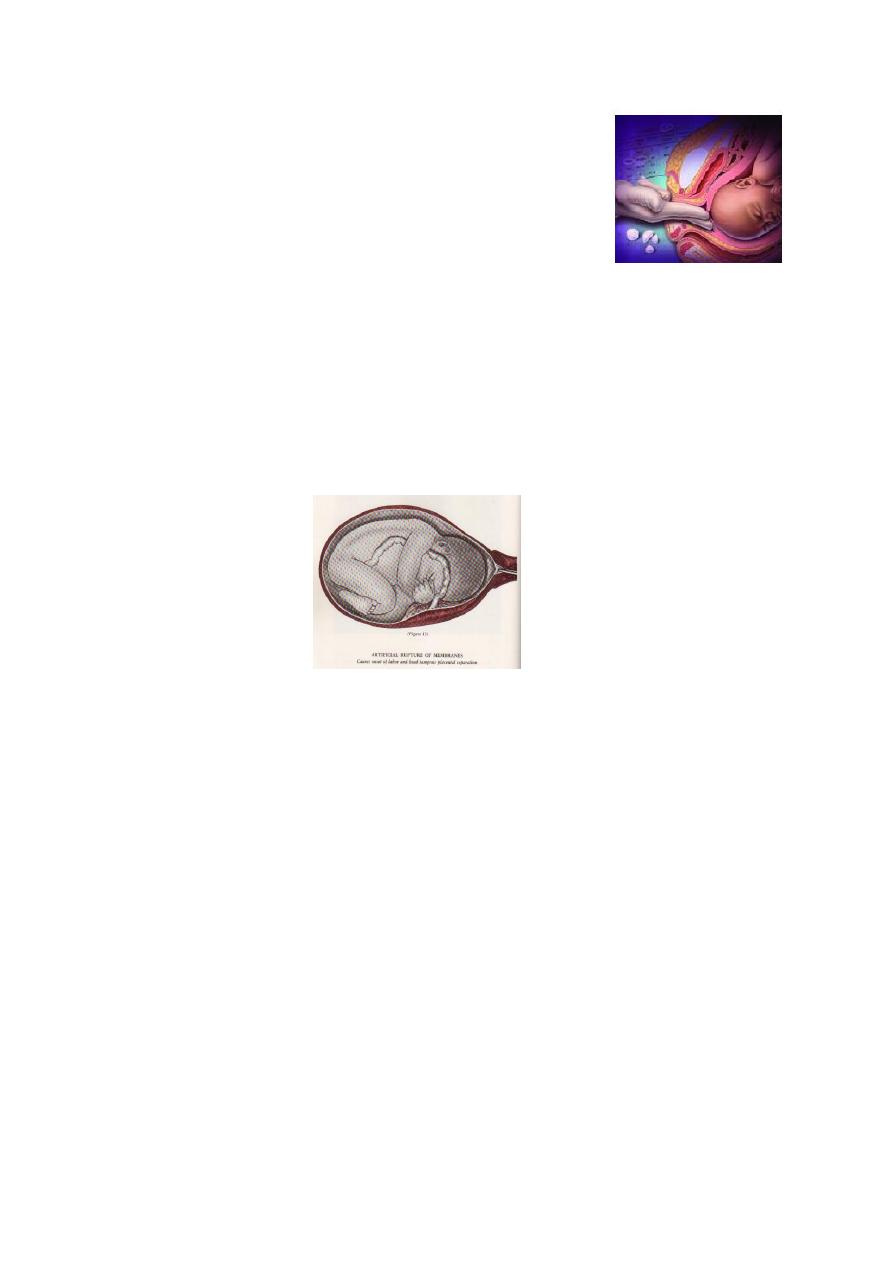
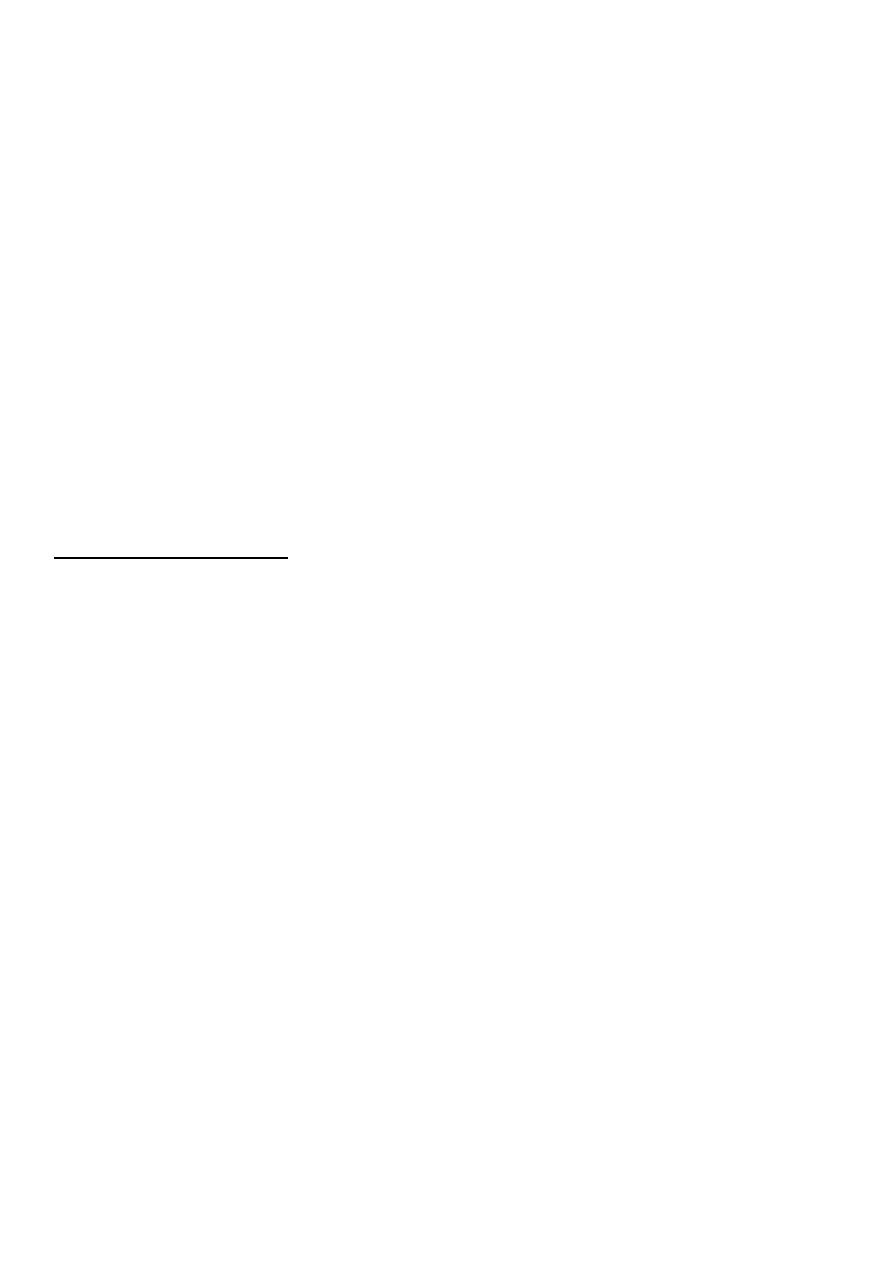
Amniotomy
:
Manipulation of the membranes cause prostaglandin release,uterine contractions,and
cervical rippining
Before rupturing the membrane it is necessary to :
patient should empty her bladder
mild degree of left lateral tilt to reduce the chance of supine hypotention .
Cervical condition (ripe or not ).
Reactive fetal heart rate
Presenting part (head )is well applied to cervix. excluding any evidence of low lying
placenta or umbilical cord the membrane over the presenting part
8
Membrane sweeping:
The membranes are stripped by inserting the
examining finger through the internal cervical os and
moving it in a circular direction to detach the inferior
pole of the membranes from the lower uterine
segment.
Amniotomy :
The fetal heart rate is recorded before and after the procedure.
The nature of the amniotic fluid is recorded (clear, bloody, thick or thin, meconium).
Risks associated with this procedure include:
1. umbilical cord prolapse or compression.
2. maternal or neonatal infection.
3. fetal heart deceleration.
4. bleeding from placenta previa or low-lying placenta.
5. possible fetal injury.
Pharmacological agents
to alter the cervical state, initiate uterine contraction or act
by combination of methods: Prostaglandins, oxytocin.
9
Oxytocin:
Oxytocin is the preferred pharmacologic agent for inducing labor when the cervix is
favorable or ripe.
It stimulates uterine activity with frequency and force of contractions being proportional
to oxytocin concentration in plasma.
It should be given as intravenous (IV) infusion to discontinue it's used quickly once any
complication develops .half life is 5-12 minutes and its physiologic effect will diminish
within 15-30 minutes after discontuation.
Start with 1-2 mU/ minute and increase variably according to contractions every 30
minutes up to a maximum of 32 mU/ minute. The aim is to attain contractions at a
frequency of 3-4 per 10 minutes.
Use balanced solution (such as normal saline or Ringer’s lactate).
Oxytocin should not be prescribed within 6 hours following administration of vaginal
prostaglandins.
Prior and During labour induction with oxytocin fetal heart rate and uterine activity
should be assessed and documented with each increasing dose.
If excessive uterine activity (greater than five contractions in 10 minutes or contractions
lasting longer than 120 seconds) occurs with:
A. normal fetal heart rate pattern:
decrease the oxytocin infusion rate and then reassess uterine activity to determine if any
further interventions are required.
B. a non-reassuring fetal heart rate pattern:
intravenous oxytocin infusion should be discontinued to correct the abnormal pattern.
repositioning of the woman in the lateral position.
assessing blood pressure.
increasing intravenous hydration if not contraindicated by the maternal condition.
pelvic examination to assess cervical dilation and rule out cord prolapse.
oxygen by face mask.
If the hyperstimulation does occur, it can be counteracted by tocolytic administration (
for example B2 agonist as Salbutamol ) , IV infusion.
10
Complication of oxytocin :
1. Hyperstimulation.
2. water intoxication with convulsion and coma.
o occurred if prolonged administration of high dose of oxytocin in large
o volume of electrolyte-free fluid because Antidiuretic effect.
3. post partum haemorrhage: mainly due to uterine atony.
4. poor uterine action.
5. Neonatal hyperbilirubinemia.
associated with maternal oxytocin infusion of more than 20 units due to vasopressine –like
activity of oxytocine that cause osmotic swelling of erythrocytes, leading to decreased
deformabilty and more rap destruction with resultant hyperbilrubinaemia in the neonate.
Prostaglandins : (PG)
Prostaglandins act on the cervix to enable ripening by a number of different mechanisms.
Risks associated with the use of prostaglandins include:
1. uterine hyperstimulation
2. maternal side effects such as nausea, vomiting, diarrhea, and fever.
Prostaglandins of the E2 and F2α class have been used to initiate labour. Prostaglandin
E1 analogues as misoprostol (Cytotec) can be used as it is safe and inexpensive agent for
cervical ripening it should not be used to women who have a uterine scar.
Prostaglandins may be given via oral, intravaginal, intracervical or intravenous routes.
Intracervical gel and intravaginal preparations have fewer systemic side effects than
others.
When prostaglandins are used, close monitoring of the woman and fetus should begin
immediately after administration of the drug.
There are other Agents currently being researched

11
Complication of induction of labour
There are a number of potential hazards for both mother and fetus from induction of
labour either as a result of initialing labour before spontaneous onset , or as a consequence
of the method of induction used . These are:
1. Failed induction.
2. Uterine hyperstimulation.
3. fetal distress.
4. Cord prolapse.
5. Abruptio placentae.
6. uterine rupture.
7. Inadvertent preterm delivery.
8. Hyponatremia
9. Neonatal hyperbilibubinemia :
10. Hypotonic uterine postpartum hemorrhage :
Intrapartum management of induced labour:
Record finding consecutively on a partogram.
Continuous fetal heart rate monitoring and uterine contraction.
