Thyroid gland 2
Professor Nashwan Q MahgoobDepartment of Surgery
Medical College/University of Mosul
Hypothyroidism
Failure of thyroid gland to produce adequate level of H. It is either:1- Congenital: due to ageneses of the gland.
2-Acquired: due to:
A- Thyroid ablation by drug, RAI, surgery
B-Post thyroiditis (hashimotos)
C-Autoimmune (spontaneous)
D- Secondary to pituitary failure.
• Congenital Hypothyroidism: both sex can involved,
• the patient fail to thrive with mental retardation, poor growth, large tongue, umbilical hernia, poor feeding and constipation.• Investigation: high level of TSH, low T3, T4.
• Treatment : Early replacement therapy to prevent permanent and irreversible mental retardation.
• The dose should be regulated periodically for long life.
Acquired Hypothyroidism (spontaneous type)
Effect female above 50 years, its autoimmune process, it is slowly and progressive disease with or with out goiter.Clinical picture:
CVS: bradycardea, cardiomegaly, pericardial effusion,
heart failure.
GIT: anorexia, increase WT, and constipation.
CNS: poor performance, somnolence, apathy and dementia.
Dermis: dry thick yellow skin, molar flash, loss of hair, intolerance to cold.
Genital: decrease libido, impotence, menstrual irregulation,
• Investigation:
• 1- Low T3,T4. high TSH• 2- ECG show low voltage,
• bradycardea, flat T wave.
• 3- High serum cholesterol.
• Treatment :Full replacement
• therapy of thyroxin.
Thyrotoxicosis
State of hyper functioning thyroid gland due to increase T4 and or T3 production. Affects 2% of women and 0.2% of men, It is 8 times more common in female.
The commonest causes are:
1-primary hyperthyroidism (Graves disease)
2-Toxic multinodular goiter (secondary)
4-Toxic solitary nodule (Plummer's disease)
5-Other rare causes:
A-Thyroiditis
B-Post partum
C-Judbassedow syndrome (excessive iodine intake)
D-Thyrotoxicosis factitia (excessive thyroxin intake)
E-Ectopic thyroid H secretion (teratoma (stroma ovari), chorio carcinoma, hydetedform mole)
F-Thyroid carcinoma.
G- Drug induced like lethium and imudarone.
Thyrotoxicosis -Types-
1-Graves disease (primary thyrotoxicosis)
its autoimmune disease. An antibody to TSH receptor is formed which act like TSH (LATS, TSI) with long period of action.
It represent 60 to 80% of cases.
May be hereditary, with strong familial predisposition.
The whole gland is hyperactive, its more common in young age female, the condition appear suddenly, there is sever eye manifestation (50% of patients), pretebial myxodema and dermopathy.
50% of patients may have other autoimmune conditions such as type I diabetes mellitus, Addison's disease, pernicious anemia, and myasthenia gravis.
2-Toxic multinoduler goitre (secondary thyrotoxicosis) Due to long standing goiter, the internduler tissue become hyperactive independent on TSH. Its more in female above 50 years, the condition is gradual in onset, there is less eye manifestation but more cardiac problem, its less sever than primary type, not associated with autoimmune diseases.
3-Toxic nodule usually in female 30 to 40 years, a localized mass in the thyroid become hyperactive independent on TSH, other thyroid tissue is suppressed.
Clinical features of Thyrotoxicosis - systemic pictures-
CNS : Tremor, hyperkinetic movements, nervousnessIrritability, emotional disturbance, insomnia, behavioral abnormalities, psychoses.
CVS: Palpitation, tachycardia, cardiac arrhythmias, cardiac failure .
Locomotor: Myopathy, wasting, tiredness and lethargy.
GIT: increase appetite with loss of WT and diarrhea.
Dermis: warm moist skin, intolerance to heat, facial flushing, loss of hair, fragile and soft nails.
Genital: increase libido, but decrease fertility, miscarriage, amenorrhea , gynecomastea, impotence
Clinical features of thyrotoxicosis-local pictures-
In case of graves disease the gland is universally enlarged ,smooth firm or soft, it may show bruit and thrill at its upper pole.
In toxic nodule a single mass at thyroid gland is found.
In toxic multinoduler goitre, multiple masses of deferent size and consistency may be found.
Pressure pictures inform dyspnoea due to pressure on the trachea or dysphagea due to pressure on the esophagus, or occlusion of SVC in case of mediastinal extension may be present.
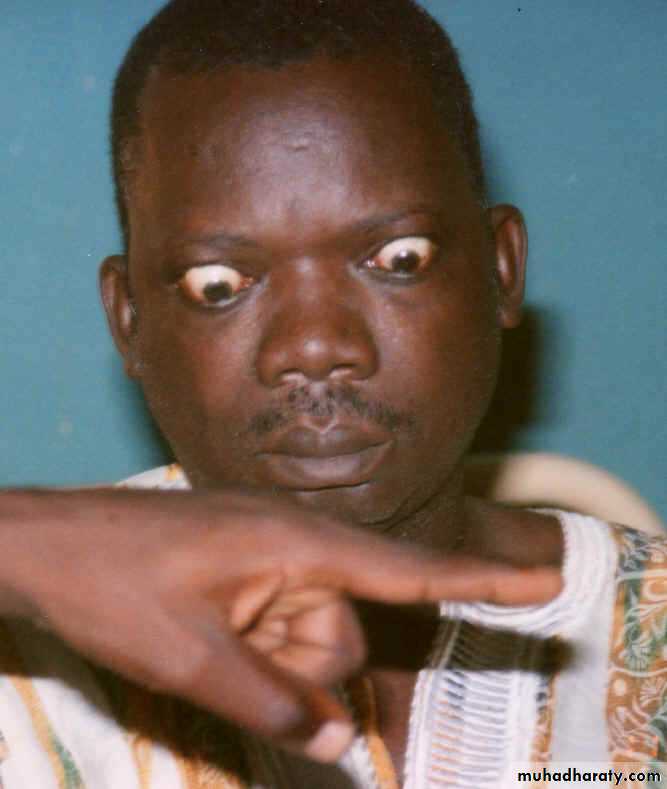
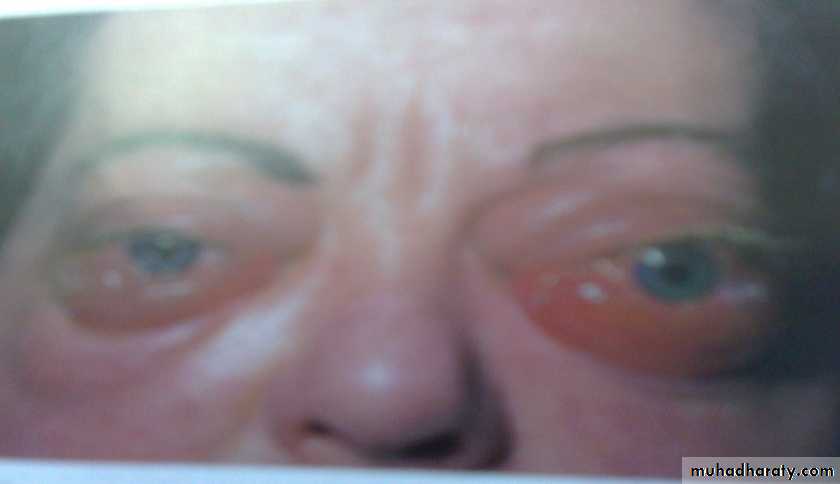
Clinical features of thyrotoxicosis -Ophthalmic pictures-
1- mild exophthalmoses:
A- bulging of the eye ball due to deposition of fluid in the retrobalber space. (exophthalmoses)B- lid retraction: widening of palpabral fissure due to retraction of upper eyelid (stellwag sign).
C- lid lag: lagging of the upper eyelid in following finger during looking downward (vonegrefe sign).
Both B and C are due to continuous contraction of levator plapabri superiors
Clinical features of thyrotoxicosis -Ophthalmic pictures-
2- Moderate exophthalmoses:Excessive bulging of the eye ball because of deposition of fat.
Absence of wrinkling at forehead on looking upward (joffroy sign).
3-Severe exophthalmoses:
Increase of intraocular pressure result
in double vision.
Difficulty in convergence (mobius sign)
Pretibial myxoedemaOccurs in 1-2% patients with Graves' disease as painless thickening of the skin, nodules or plaques due to deposition of glycos-amino-glycans substance Usually occurs on shins or dorsumof foot Strongly associated with ophthalmopathy, there is high level of antibody.Respond to local steroid and disappear after treatment of thyroid toxicity
4- progressive exophthalmoses: appear after surgical treatment of thyrotoxicosis, result in chemosis, corneal ulceration and intraocular muscle paralyses.
• Type of inv.
• graves• Multinoduler
• toxic goitre
• Toxic nodule
• RAIU
• Antibody
• positive
• negative
• negative
• F T3,T4 level
• TSH level
• Thyroid scan
• Whole gland is hyperactive
• Internoduler tissue is hyper active
• the nodule is hyper active
Thyrotoxicosis -investigation-
Treatment of thyrotoxicosis
Anti-thyroid drugs
Inhibit synthesis of thyroxin by interfering with trapping, oxidation and coupling of iodide.
Most commonly used drugs are: carbimazole,methmazol and propylthiouracil, it can be used as:
1- short-term (3-4 months) prior to definitive treatment by radioiodine or surgery.
2-long-term (12-24 months) to induce remission in Grave's disease.
3-Block and replacement therapy: large dose of carbimazol (40mg) with thyroxin (100 micro-gm) for 1-2 years to decrease size of the gland, prevent hypothyroidizm, and decrease relapse.
Advantage - no surgery or radioactive material
Disadvantages1-Treatment is prolonged.
2-Failure rate after 2 years treatment is 50% specially in large goiter with high level of antibody.
3-Impossible to predict which patients will remain in remission.
4-Of no use in multinoduler or in toxic nodule.
5- Side effect like Agranulocytosis or aplastic anaemia (Patients advice to seek medical attention if they develop sore throat), hepatitis, peripheral neuritis and polyarteritis,.
6- Goitergenic
7-Crosses the placenta and appear in the milk.
Radioactive iodine
I131 is commonest isotope used, the aim is to destroythe thyroid tissue.
Dose 200–600 MBq, 20% need 2 doses.
Advantage - no surgery or prolonged drug therapy.
Disadvantages
1-Isotope facilities must be available.
2-80% of patients become hypothyroid after10 years.
3-Indefinite follow up required.
4-Need 3 to 4 months to exert its action.
5- May cause genetic abnormalities.
6-Contraindicated in children, pregnancy, breast feeding and below 25 years and those with ophthalmopathy.
7- Pregnancy to be avoided 4 months after treatment.
8- Increase overall cardiovascular mortality rates.
9- progression of Graves' ophthalmopathy
Indications of RAI: old patients with small or moderate-sized goiters, those who have relapsed after medical or surgical therapy, and those in whom antithyroid drugs or surgery are contraindicated.
Surgery
The aim is to remove the thyroid tissue to decrease hormone production.
Indications of surgery:
1-Relapse after adequate course of anti-thyroid drugs, or its side effect in Grave's disease or presence of pressure manifestation.
2-In toxic multinoduler and toxic nodule
Advantages: Goiter is removed, high and rapid cure rate.
Disadvantages
5% develop recurrent thyrotoxicosis
20 to 80% develop postoperative hypothyroidism
0.5% develop parathyroid insufficiency
Side effect of surgery.
Guide in thyrotoxicosis treatment
The choice of therapy depends on:1-Age of the patient
2-Size of the thyroid
3-Type of thyroxicosis
4-The patient intelligence,
personality and wishes.
5-The ability of follow up
6- The availability of medication
7- The cost effectiveness
Preoperative preparation
A-The patient should be euthyroid at time of operation, this can be achieved by:1- Propranalol 40mg tds to decrease sympathetic over activity, and prevent change of T4 to T3 at cellular level, its given for 2 weeks preoperatively and continuo for 10 days post operatively to compete the T4 which has half life of 10 days.
2- Carbimazol 10 to 40mg till the patient become euthyroid (4 to 6 weeks) then 5 to 10mg till the day of operation.
3-Logul iodine drops- 3 drops 3 times a day for 10 days to render thyroid less vascular and firm.
Preoperative preparation
B-Investigation1- Indirect laryngoscopy to asses the vocal cord since 3% of patients may have symptom less cord paralyses.
2- Thyroid antibody in case of graves disease.
3- TSH level , which should be normal.
3- Serum calcium.
4- Cervical x ray to asses thyroid extension and cervical spine for any OA changes.
5- ECG, Hb, serum urea, FBS, blood group.