1
Forth stage
Obstetric
Lec-7
د. أحمد جاسم
1/1/2016
MULTIPLE PREGNANCY
Definitions:
In general terms, multiple pregnancy is a pregnancy with two or more fetuses.
Twins make up the vast majority (97 – 98%) of multiple gestations.
Pregnancies with three or more fetuses are referred to as ‘higher multiples’
Prevalence:
In the UK, twins currently account for approximately 1.5% of all pregnancies. Higher
multiples occur in 1 in 2500 pregnancies.
Traditionally the expected incidence has been calculated using Hellin’s rule. Using this rule,
twins were expected in 1 in 80 pregnancies, triplets in 1 in 80
2
and so on.
Risk factors:
For dizygotic twinning include:
Previous multiple pregnancy
Family history (maternal side)
Increasing maternal age
Racial origin (more common in women of West African ancestry, less common in
those of Japanese ancestry)
Assisted conception
Classification:
The classification of multiple pregnancy is based on:
number of fetuses: twins, triplets, quadruplets, etc.,
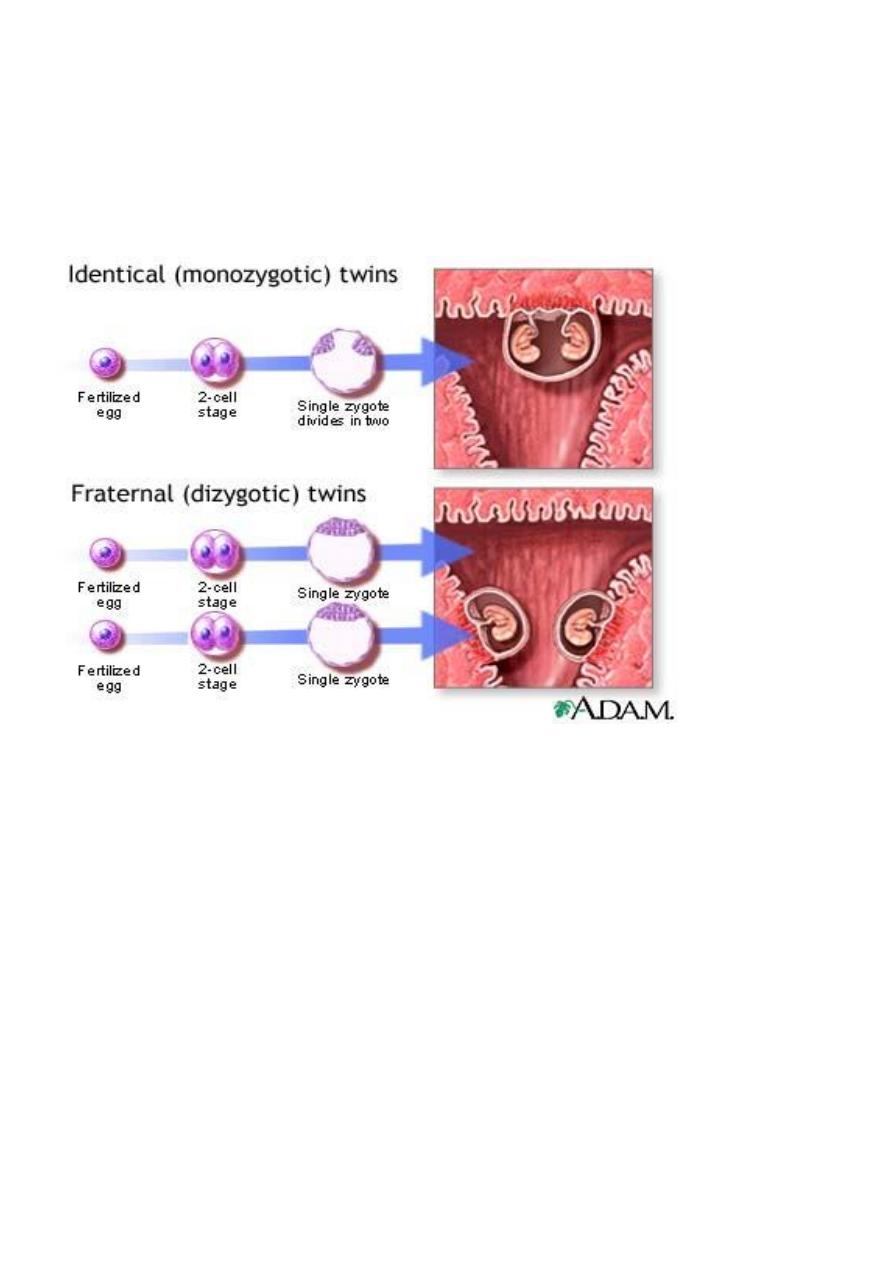
number of fertilized eggs: zygosity (dizygotic & monozygotic),
number of placentas: chorionicity (dichorionic & monochorionic),
number of amniotic cavities: amnionicity (diamniotic & monoamniotic)
2
Aetiology:
Dizygotic twins arise from the release of two eggs at ovulation.
Monozygotic
twins arise from a single fertilized ovum that split into two identical
structures
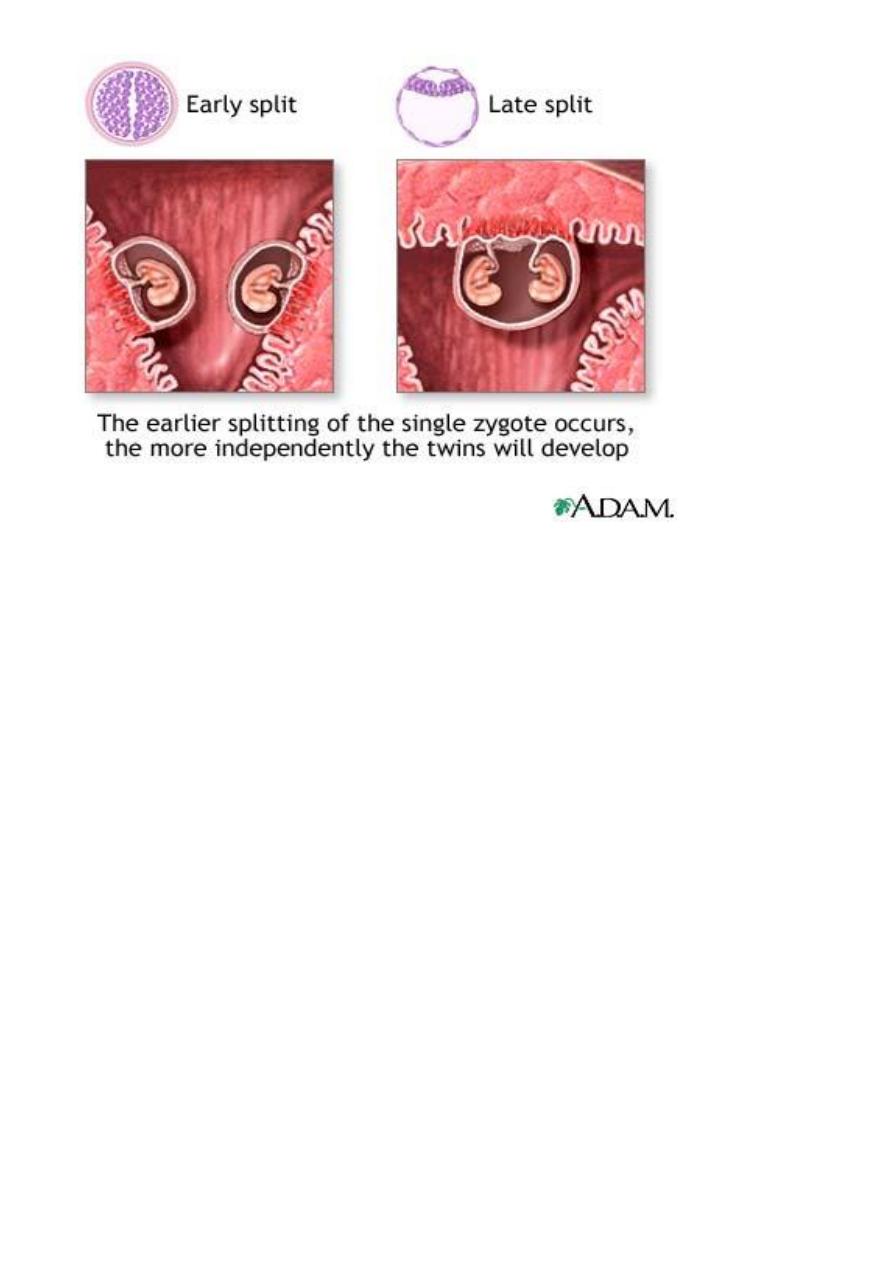
The type of monozygotic twin depends on how long after conception the split
occurs:
embryo splits at 3 days ---» two chorions, two amnions (DCDA).
embryo splits at 4-7 days ---» single placenta, one chorion, two amnions
(MCDA).
embryo splits at 8-12 days ---» single placenta, one chorion and one amnion
(MCMA) (rare).
embryo splits at 13 days ---» conjoined or Siamese twins (very rare)
3
Physiological changes:
o All the physiological changes of pregnancy (increased cardiac output, volume
expansion, relative haemodilution, diaphragmatic splinting, weight gain, lordosis, etc
are exaggerated in multiple gestations.
o The ‘minor’ symptoms of pregnancy may be exaggerated.
o For women with pre-existing health problems, such as cardiac disease, a multiple
pregnancy may substantially increase their risk of morbidity.
Presentation:
Nearly all multiple pregnancies are now diagnosed in the first trimester by
ultrasound. However, some twins die and are absorbed in the first half of pregnancy
('the disappearing twin' syndrome) and early scanning increases awareness of this
phenomenon.
Early symptoms may include hyperemesis and other exaggerated pregnancy-related
symptoms. The uterus may be palpated abdominally earlier than 12 weeks
gestation.
In the second half of pregnancy, may present with large-for-dates uterine size,
higher than expected weight gain, > 2 fetal poles on palpation and two or more fetal
heart rates heard on auscultation.

4
Management:
Prenatal diagnosis:
Fetal abnormality is more common in multiple pregnancies - both the maternal age specific
chromosomal disorders (as increasing maternal age is a risk factor for multiple birth) and
fetal anatomical disorders.
However there are important difference in both risk and management, based upon
chorionicity:
Each fetuses of a dichorionic twin pregnancy has a risk of structural anomalies, such as
spina bifida, that is similar to that of singleton. Therefore the chance of finding an anomaly
within a dichorionic twin pregnancy is twice that of a singleton.
In contrast, each fetus in a monochorionic twin pregnancy carries a risk for abnormalities
that is four times that of a singleton.
This is presumably due to a higher risk of vascular events during embryonic development.
Regarding chromosomal abnormalities, in dizygotic twins, the maternal age – related risk
for chromosomal abnormalities for each individual twin remains the same as for a singleton
pregnancy.
Therefore, at a given maternal age, the chance that at least one of the twin pair is affected
by a chromosomal defect is twice as high as for a singleton pregnancy.
In monozygotic twin pregnancies, chromosomal abnormalities affect neither fetus or both.
The risk is based upon maternal age
Nuchal translucency assessment (ultrasound measurement of the translucency of the
nuchal fold in the fetal neck between 10 and 14 weeks) identifies individual fetuses at high
risk of trisomy.
Serum screening is unreliable.
Invasive prenatal diagnosis (amniocentesis and chorionic villous sampling) is challenging as
there are at least 2 fetuses to sample correctly and should be undertaken in a tertiary
referral centre.
If one fetus is detected as abnormal, selective termination (if desired) must be accurately
targeted. Selective termination in monochorionic pregnancies risks co-twin sequelae and
require different technique.
Antenatal:
Twin pregnancies should be referred to obstetricians for shared care due to the
higher risk they present.
5
Women should be booked to deliver in a hospital with a SCBU.
Early determination of chorionicity should be routine and this is done most reliably
by ultrasound in the late first trimester. In dichorionic twins, there is a V-shaped
extension of placental tissue into the base of the inter-twin membrane, referred to
as the ‘lambda’ or ‘twin-peak’ sign.
o In monochorionic twins, this sign is absent and the inter-twin membrane joins
the uterine wall in a T-shape.
Assessment of chorionicity later in pregnancy is less reliable and relies upon
assessment of fetal gender, number of placentas and the characteristic of the
membrane between the two amniotic sacs. The ‘lambda’ sign becomes less accurate,
and membrane thickness must be utilized. Those twins found to be monochorionic
should be scanned frequently to detect twin-twin transfusion or intra-uterine growth
retardation at an early stage. If suspected, these pregnancies should be referred to
tertiary fetal medicine centres for further management.
All twin pregnancies (regardless of chorionicity) are regularly scanned after about 30
weeks to monitor growth and fetal well-being with early delivery induced in cases of
growth cessation and/or poor Doppler blood flow indices.
Anaemia should be looked for and treated vigorously (many would recommend
routine (as opposed to selective) supplementation of folic acid and iron in multiple
pregnancy).
Hospital bed rest in uncomplicated cases is not recommended.
Maternal complications such as pre-eclampsia are also more common in multiple
pregnancies so antenatal carers should be vigilant for early signs.
Intrapartum:
On admission in labour, obtain IV access, blood grouped and saved, monitor fetal heart
rates separately and check position of lead fetus:
In 60% case both fetuses present as cephalic
In 20% cases 1st twin cephalic, 2nd breech
In 10% cases breech/cephalic
In 10% cases breech/ breech
Vaginal delivery of twins
With no complicating factors, the mother can go into spontaneous labour provided the first
twin has a cephalic presentation. When the first twin presents transversely, Caesarean
section is indicated. When the first twin presents as a breech, clinician usually recommend
6
delivery by elective Ceasarean section. this is largely because of the increased risk
associated with singleton breech vaginal delivery. Other factors include dwindling
experience of breech delivery and the rarely seen phenomenon of ‘looked twins’ (the chin
of the first (breech) baby looked against the chin of the second (cephalic) baby).
The ideal criteria for a twin labour are:
Spontaneous onset,
Cephalic presentation of twin 1,
Twin 1 larger than twin 2,
Dichorionic pregnancy.
With rupture of membranes, check for prolapse of umbilical cord.
Immediately after the first baby, abdominal palpatrion should be done to determine
the lie of the second fetus:
If longitudinal, rupture the second amniotic sac (once presenting part is
engaged, usually after a couple of contractions) and proceed to delivery.
If transverse, external cephalic or internal podalic version may be attempted to
bring into longitudinal lie. If successful, as confirmed by vaginal examination,
then rupture the second amniotic sac once the fetal head is engaged. If
unsuccessful, deliver by Caesarean section.

7
Contractions can reduce after the birth of the first fetus and if they do not quickly
return (within 15 minutes), set up an IV oxytocin infusion following which birth of
second fetus should be straightforward. The second twin should deliver within 20-45
minutes of the first twin.
Where there are difficulties with the delivery of the second twin or if it develops a
bradycardia, a vacuum extraction (in cephalic position) or breech extraction can be
performed without necessarily resorting to Caesarean delivery.
Third stage should be actively managed by IM injection of Syntometrine® or
Syntocinon® as the fetal head is being born to avoid postpartum haemorrhage.
Twin deliveries should be attended by 2 paediatricians, 2 obstetricians and an
anaesthetist.
Complications:
Although a naturally occurring phenomena, multiple pregnancies are considered high-risk
because:
Smaller babies - fetuses tend to be individually smaller than those in a singleton
pregnancy because of greater demand for nutrients and slower in utero growth i.e.
light-for-dates. Monozygotic twins tend to be smaller than dizygotic twins.
Increased risk of prematurity - the mean gestation for twins is 37 weeks and for
triplets 31 weeks.
Higher risk of congenital abnormality associated with multiple pregnancies (x2-4 rate
in singleton pregnancies).
Higher rates of cerebral palsy found in twins (1-1.5%) and triplets (7-8%).
Perinatal mortality rate for twins is significantly higher than singletons (x5) and even
higher for triplets (x6). Rates are higher for monochorionic twins than dichorionic
twins (49 versus 11.5/1000).
Higher rate of maternal pregnancy-related complications such as hyperemesis
gravidarum, polyhydramnios, pre-eclampsia, anaemia, antepartum haemorrhage.
Higher rate of complications in labour - malpresentation, cord prolapse, premature
separation of placenta, cord entanglement, postpartum haemorrhage.
Also the non-medical financial, social and emotional consequences of caring for twins
or higher order multiples need to be kept in mind.

8
Complication unique to monochorionic twinning: twin-to-twin
transfusion syndrome (TTTS)
In all monochorionic twin pregnancies there are placental vascular anastamoses
present which allow communication between the two fetoplacental circulations.
In some monochorionic twin pregnancies, imbalance in the flow of blood across
these arteriovenous communication result in twin-to-twin transfusion syndrome.
The donor twin may become growth restricted and oliguric with oligohydromnios.
The recipient fetus become hypervolaemic, leading to polyuria and polyhydramnios.
There is a risk of myocardial damage and a high output cardiac failure. It occurs in
about 15 percent of twins with a shared placenta.
Complication unique to monoamniotic twinning:
monoamniotic twin share a single amniotic cavity, with no dividing membrane between the
two fetuses.
they are at increased risk of cord accident (cord entanglement)
