
1
Forth stage
Obstetric
Lec-12
د . احمد جاسم
1/1/2014
Medical disorder with pregnancy
THYROTOXICOSIS IN PREGNANCY
It Hazards is Abortion and preterm labour.
During pregnancy, there is increased estrogen level which causes:
enlargement of thyroid gland.
Increase production of thyroid –binding globulin by liver.
Increase in total amount of T4 and T3 mostly in form of protein-bound thyroxin and
therefore there are no changes in the amount of free circulating active fraction of T4
and T3.
There is iodine deficiency in pregnancy due to:
increases Renal clearance of iodine in pregnancy.
fetal thyroid activity.
It occur in 1in 500 pregnancies. it is mostly due to Graves disease. (autoimmune
thyrotoxicosis)
Clinical Picture
Weight loss in spite of good appetite.
Intolerance to heat.
Tremors.
Resting pulse over 100 beats/min.
Exophthalmos.
Investigations
Free T4 (raised) T3 resin uptake (raised)
Elevated Serum free T4 and suppressed TSH level establish the diagnosis of
hyperthyroidism.
Avoid radioactive-iodine testing because of fetal thyroid pickup and retention.

2
Effect of hyperthyroidism on pregnancy
uncontrolled disease is associated with maternal and fetal complications including:
Thyroid storm (thyrotoxic crisis)
Heart failure.
miscarriage
gestational hypertension.
Pre-eclampsia.
Premature labour.
IUGR
stillbirth
Treatment
Propylthiouracil: 100-200 mg t.d.s. or
Carbimazole: 10-15 mg t.d.s.
Thyroxine is combined with antithyroid drugs in the last trimester to protect the
neonate from hypothyroidism. Breast feeding is contraindicated because the drugs are
excreted in milk.
Surgical management :
may be considered (thyroidectomy) if:
medical treatment fails
there is clinical suspicions of cancer
compressive symptoms due to goiter.
It is advisable to delay surgery until the second trimester because the rate of
spontaneous abortion is highest during the first trimester.
operation is safe if mother properly prepared.
Hyporthyroidism
Avoid radioactive-iodine testing because of fetal thyroid pickup and retention.
It occurs in nearly 1%of pregnant women and is usually due to autoimmune Hashimotos
thyroiditis or idiopatheic myxoedema or following treatment of hyperthyroidism.
Rarely get pregnant if not treated
3
Effects of hypothyroidism on pregnancy
Pregnant women on appropriate treatment can expect a normal pregnancy outcome,
but untreated maternal hypothyroidism has been associated with an increased risk
of:
Spontaneous abortion.
Gestational hypertension and preclampsia.
Abruption placentae.
Premature delivery.
Low birth weight.
Stillbirth.
Lower intelligence levels in offspring and Reduced intelligence quotient(IQ).the insult
is likely to occur in the first trimester and therefore pre-conceptional optimization of
T4 therapy is important.
Investigation:
Elevated TSH level.
Low levels of serum T3 and T4
Treatment :
Thyroxin is titrated against biochemical result and is safe in pregnancy and lactation.
thyroid function test every 2-3 months. more frequent measurements are made if the
clinical or biochemical condition is deranged.
EPILEPSY IN PREGNANCY :
It is relatively common disorder occurring in 1% of women of child-bearing age.
Effects of pregnancy on seizure
Pregnancy has no consistent effect on epilepsy. seizure frequency during pregnancy may
increase , decrease ,or remain the same.
Anticonvulsant drug dose may still same as non pregnant level or need increase and
patient must be monitored during pregnancy to ensure that dose adjustments are made
as appropriate.

4
Effects of epilepsy on pregnancy :
There are pregnancy complication associated with epilepsy:
1. Increase congenital abnormality.(neural tube defect, cardiovascular malformations
and cleft lip and palate).It may be due to:
anticonvulsant medication
hypoxia resulting from seizure.
2. Increase perinatal mortality
3. Ante-partum haemorrhage.
4.Post-partum haemorrhage.
5. Pre-eclampsia.
6. Hyperemesis gravidarum.
7. Premature labour.
8. Prolonged labour.
9. Low birth weight
10. Increase intrauterine fetal death.
Neonatal complications :
Increase risk of epilepsy in child. (4fold increase)
Increase risk of haemorrhagic disease of newborn.
Drug withdrawal symptoms.
Neonatal morbidity and mortality
Effects of anti-epilieptic drugs on fetus and newborn :
1. Major and minor congenital abnormalities.
2. Neonatal withdrawal effects.
3. Vitamin K deficiency with haemorrhagic disease in newborn.
4. Developmental delay or behavioural difficulties.
5. Increase in childhood malignancies.
Management :
Preconceptional care:

5
Delay conception until epilepsy is well controlled.
Monotherapy is recommended with the lowest dose of drug.
Folic acid 5mg/day.
Discuss risk of fetal malformation and the role of prenatal diagnosis.
Discuss the risk of epilepsy in offspring
Antenatal care :
Women with epilepsy who become pregnant constitute a high-risk group and need
Multidisciplinary care team with regular antenatal visits.
*Proper seizure control is the aim to minimize maternal morbidity (fits can be fatal) as
well as uncontrolled seizure are more harmful to fetus than the potential risks of drug
therapy so patients should receive anticonvulsant drug and must be monitored free drug
levels monthly.
Advise good diet, sleep and avoidance of precipitating factors.
*Offer prenatal diagnosis. All patients should receive anomaly ultrasound assessment to
exclude specific abnormalities associated with their medication and fetal
echocardigraphy at about 18 weeks.
*Vitamin K supplementation given from 36 weeks onward to prevent neonatal bleeding
disorder.
The management of labour and delivery :
The management of labour and delivery follows obstetric indications and spontaneous
vaginal delivery should be the aim if no contraindication.
*Epileptic seizures may occur during labour and as such may confuse the diagnostic
situation that includes eclampsia. Epileptic seizures should be treated and may be
reduced with the use of epidural anaesthesia.
Postnatal care (postpartum) :
Vitamin K to neonate.
*Check for fetal abnormality.
Monitor for neonatal withdrawal.
*
Breast feeding is safe.
*
*Post-partum drug doses may need to be adjusted if doses have been increased
during pregnancy.
6
*Advise about avoidance of seizure related accident and specific advice must be
given about childcare..
Contraceptive advice:
Mirena (medicated intra uterine contraceptive device)can be used as it is not
affected.
Depo-provera injection(progesterone) every 10 weeks.
50 µg estrogen combined oral contraceptive pills if decide to use combined oral
contraceptive pills.
EPILEPSY IN PREGNANCY :
Grand mal epilepsy is the commonest type.
Treatment: phenobarbitone or phenytoin. Folic acid should be given with phenytoin as it
is antifolic .
There is risk of foetal malformations.
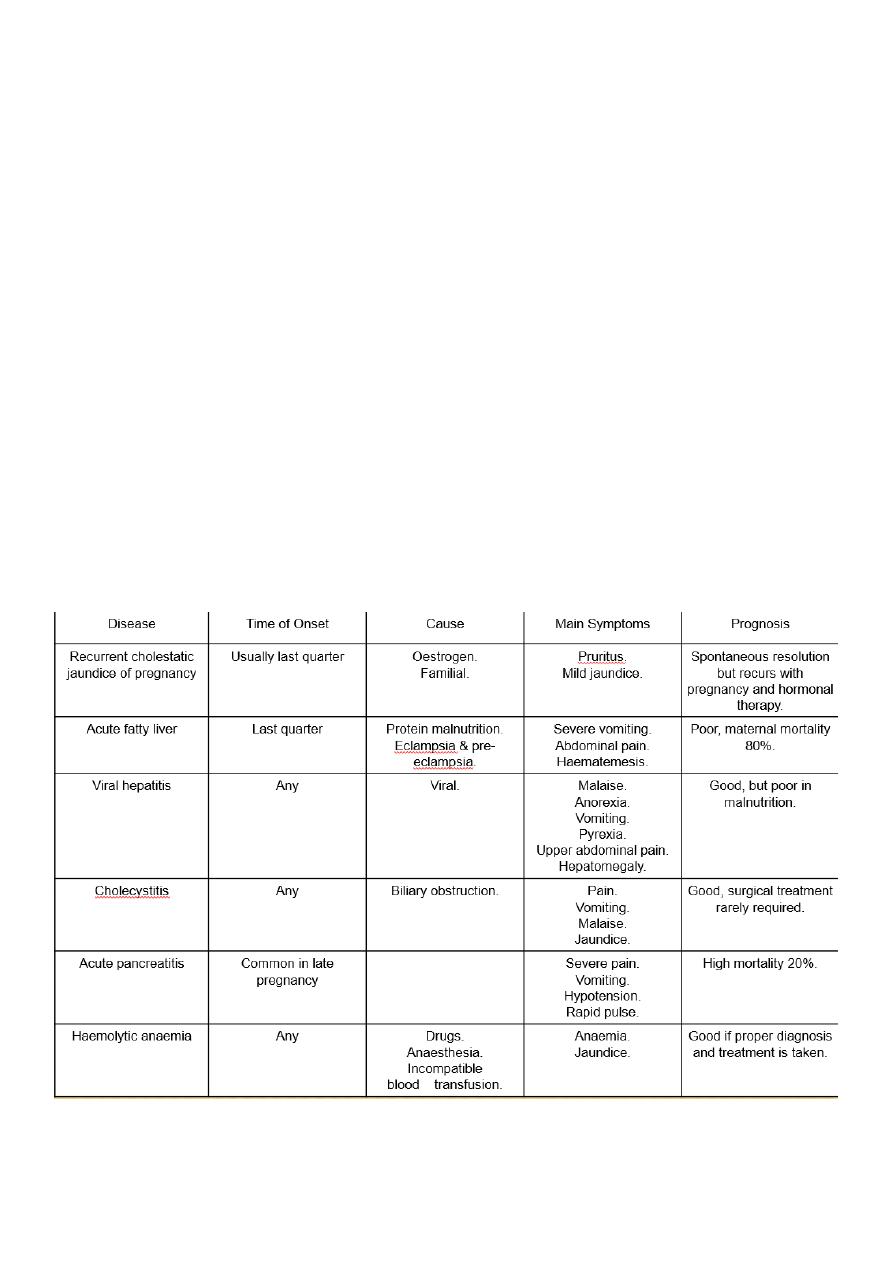
Jaundice in Pregnancy :
Jaundice in pregnancy can be caused by
1. 1. Obstetric cholestasis Intrahepatic cholestasis (recurrent)

7
2. 2. Complication of severe pre-eclampsia, eclampsia.
3. 3.Persistant severe hyperemesis gravidarum refractory to all treatment.
4. 4. Acute hepatic failure.
5. 5. Haemolytic jaundice.
6. 6. Congenital hyperbilirubinaemias
7. 7. Viral hepatitis.
8. 8.Side effect of drug (chlorpromazine).
Bronchial asthma :
Asthma is the most common respiratory disorder affecting 3% of women of childbearing
age.
Effect of pregnancy on bronchial asthma :
Pregnancy has variable effect on asthma but for the vast majority of women there is no
impact whatsoever. Pregnancy itself does not seem to increase the frequency or severity
of asthma.
About 1in 10 asthmatics will suffer an acute attack in labour.
Risk of postpartum deterioration should be discussed with women.
Effect of bronchial asthma on pregnancy :
A. in well controlled asthma No increase in obstetrical problem.
B. Severe and poorly controlled asthma does have a detrimental effect on pregnancy
and is associated with an increased incidence of:
Abortion.
Intrauterine fetal death (IUFD).
intrauterine growth restriction (IUGR).
hypertensive disorders.
preterm rupture of membranes.
preterm labour.
Managing pregnancy in asthmatic patients :
Preconceptional care:

8
It is important that women receive good advice pre-pregnancy about the potential
impact of their medical condition and enter pregnancy with appropriate confidence
about medication.
Base line investigation: peak flow measurement.
Antenatal care:
Pregnant asthmatics should be followed closely during pregnancy to ensure adequate
maternal and fetal assessment.
Standard antenatal care is advised in pregnant women with well controlled mild and
moderate asthma, while multidisciplinary unit for Poorly controlled and severe asthma
cases.
prevention is the key, and known triggers of exacerbations should be eliminated or
avoided in home and at work.
The management of asthma in pregnancy is essentially the same as in non-pregnant
patients and continuo treatment which given before pregnancy. Short-acting and long-
acting beta 2 agonist, inhaled steroids and theophylline can all be used with confidence
in pregnancy.
Any patient whose asthma seems to be deteriorating, particularly in the third trimester,
should be seen by an obstetric physician for review.
It is obviously desirable that control of asthma should be at its optimum prior to the
onset of labour.
Care should be at optimizing medical treatment to asthmatic attacks and the use of
aggressive treatment should these attacks occur.
Asthmatic pregnant women should have:
1. peak flow measurement.
2. Glucose tolerance test to those receiving steroids.
3. Ultrasound examination for fetal growth and well-being.
Timing of delivery:
Depend on maternal and fetal status.
If pregnancy is progressing well, there is no need for early intervention and it is
advisable to await spontaneous onset of labour.
Early delivery can be considered for fetal growth restriction or maternal deterioration.

9
Management of labour and delivery :
Vaginal delivery is the aim and caesarean section is performed only for obstetric
reasons.
If patient on steroids, hydrocortisone required to cover labour.
No form of analgesia is contraindicated. Epidural is the preferred analgesia and
anaesthesia. General anaesthesia should be avoided if possible as it increase risk of
broncho-spasm and chest infection.
Drugs used in obstetrics which should not be used in asthmatic women as it cause
brochospasm
are
Ergometrin.
Non-steroidal anti-inflammatory drugs.
ProstglandinsF2α.
Aspirin.
