
1
Forth stage
Obstetric
Lec-11
.د
ا
سماء
1/1/2016
Obstetric procedures
CAESAREAN SECTION:
Is an operation used to deliver a potentially viablefetus through an incision in the anterior
abdominal wall and the uterus .(operation for delivery of non viable fetus ~ hysterotomy ).
Types of C.S :
Classified according to the site of uterine incisions:
1- Lower segment C.S. : Transverse incision in the lower uterine segment .
Advantage :
reduced chance of rupture .
reduced risk of bleeding ,peritonitis ,
paralytic ileus and bowel adhesion.
2- Upper segment C.S : Vertical incision in the upper uterine segment , This incision may
be made in the lower segment (low vertical incision) but It’ll invariably extendinto the
upper segment .
Indication of C.S.
Dystocia (maternal/fetal )
- CPD.
- Failed induction of labour.
- Abnormal uterine action.
Maternal
- Disease : PE , Eclampsia/DM/cardiac dis./ cervical CA .
- Previous uterine surgery : Classical C.S. /Previous 2 C.S./Previous myomectomy (Full
thickness ) .
- Obstruction to birth canal : fibroid / ovarian tumour.
Fetal :
- Fetal distress .
- Cord prolapse.
- Fetal malpresentation.

2
Placental :
- placenta previa .
- abruptio placentae.
Indications for classical C.S.:
1. PTD of breech presentation with poorly formed
lower uterine segment ,when transverse incision may be
too narrow to allow a traumatic delivery .
2. Transverse lie (back inferior) with ruptured membrane.
3. Lower segment restricted because of fibroid ,
or dense adhesions .
4. Caesarean hysterectomy .
5. Post mortem C.S. to rescue the fetus from dead mother.
6. Invasive cervical cancer.
Technique of C.S. now favors :
-Prophylactic antibiotics .
-Cohen’s incision .
-Delivery of the placenta by controlled cord traction .
-Leaving the uterus in during repair .
-Not reperitonealizing .
Preparation for C.S. :
- Left lat. Position .
- Empty the stomach and antacid .
- Thrombo prophylaxis .
- Prophylactic antibiotics .
- Catheterization .
- Skin preparation : shaving . iodine , chrorhexidine
Skin incision :
-Low transverse suprapubic incision : more cosmotic , less dehiscence and hernia .
-Cohen’s incision : less post operative febrile morbidity , shorter operative time .
3
-Midline or paramedian incision : better exposure .
*The skin wound is about 15 cm in length ,excise the scar of previous C.S. operation .
Uterine incision :
-Low transverse LSCS : less dissection of the bladder ,blood loss is less ,lower incidence
of uterine rupture
-Low vertical incision
-Classical or upper segment incision
Risk of C. S. :
Maternal risk
Mortality after C.S. is 5-10X after normal vaginal delivery
Risk is more after emergency than elective C.S..
:
Immediate complications
-Anasthesia , aspiation (Mendelson’s syndrome)
-Haemorrhage (blood transfusion and shock)
-Injury to adjacent organs .
-Infection .
-Post operative ileus .
-Pulmonary embolism .
Rupture in pregnancy &labour , Placenta previa,
Remote :
Intestinal obstruction and hernia, Risk of repeated C.S.
Fetal risk :
1.Risk of anasthesia .
2.Respiratory problems (transient tachypnea)
3.Intracranial haemorrhage (difficult delivery)
4.Prematurity ( inaccurate date ).
Delivery after previous C.S.
-There is a tendency against repetition of C.S. in patient with previous scar in order not to
compromisethe obstetric future of the patient.
4
for non
.,
one lower segment C.S
previous
Vaginal delivery is allowed in patients with
-
.
with normal obstetric situation
,
recurrent indication
-Factors increase scar rupture are: type of C.S. (Risk of rupture of scar is more in
patient with classical C.S. (2.2%~ 0.5%) with higher maternal and fetal mortality),
sepsis after the previous C.S., implantation of the placenta over the scar in the next
pregnancy.
Timing of elective C.S :
-When C.S. indicated for maternal indication there is little choice in timing delivery. If
indication is for fetal interest :fetal maturity and fetal condition determine the timing of
C.S..
-Maturity determined by proper pregnancy dating ,proved with ultrasound ,and better in
case of doubt is by amniocentesis and L/S ratio.
Assisted Vaginal Delivery:
-
Vaccum (ventose)
-
Forceps
assisted vaginal delivery offers the option of operative procedure to achieve delivery with
the potential safety & quickly removing the infant, mother & obstetrician from a difficult
or hazardous situation when spontaneous vaginal delivery does not occur within a
reasonable time.
Indication for assisted delivery:
Maternal Indication :
stage .
nd
1. Maternal distress during 2
stage .
nd
2. Prolonged 2
stage of labour .
nd
reduce the stress of the 2
ulmonary or vascular disease to
3. Cardiop
4. Vaginal birth after previous lower segment C.S. to reduce the stress on the scar .
5. Significant vaginal bleeding .
Fetal Indications :
1. Malposition of the fetal head (OP, OT)
2. Fetal distress ( bradycardia or deceleration ) and cord prolapse .
3. Preterm baby (1500 – 2500 Kg )
5
4. Vaginal delivery of breech : forceps for after coming head to avoid traction on the
trunk and the cervical spine and produce controlled flexion of the head .
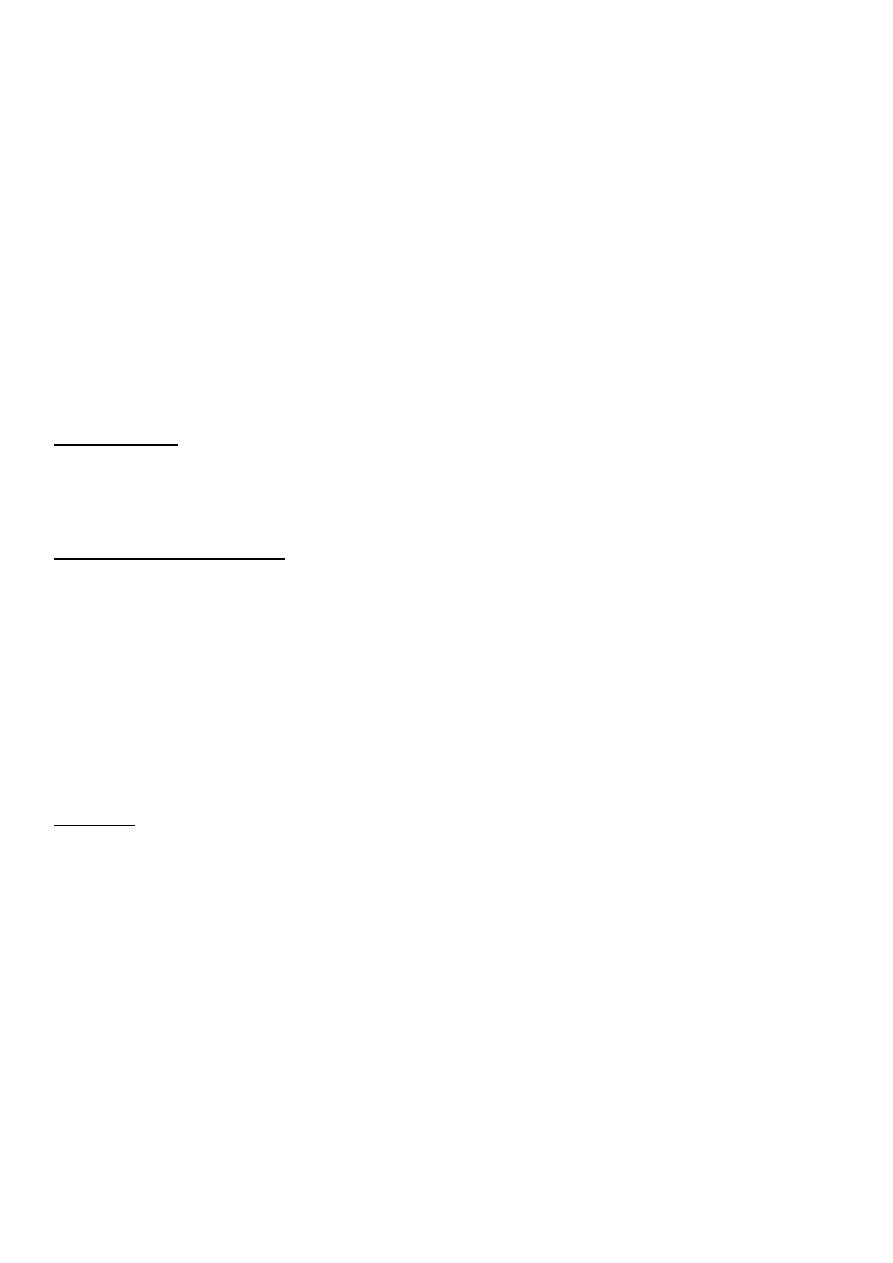
Forceps
has two blades.
Each blade has two curves , a shank
and a handle
There is a lock.
Types of obstetric forceps :
1-Short curved forceps Used for Outlet forceps operation or for delivery of the head
during C.S. ,it has short shank
(2.5 cm),light in weight.
6
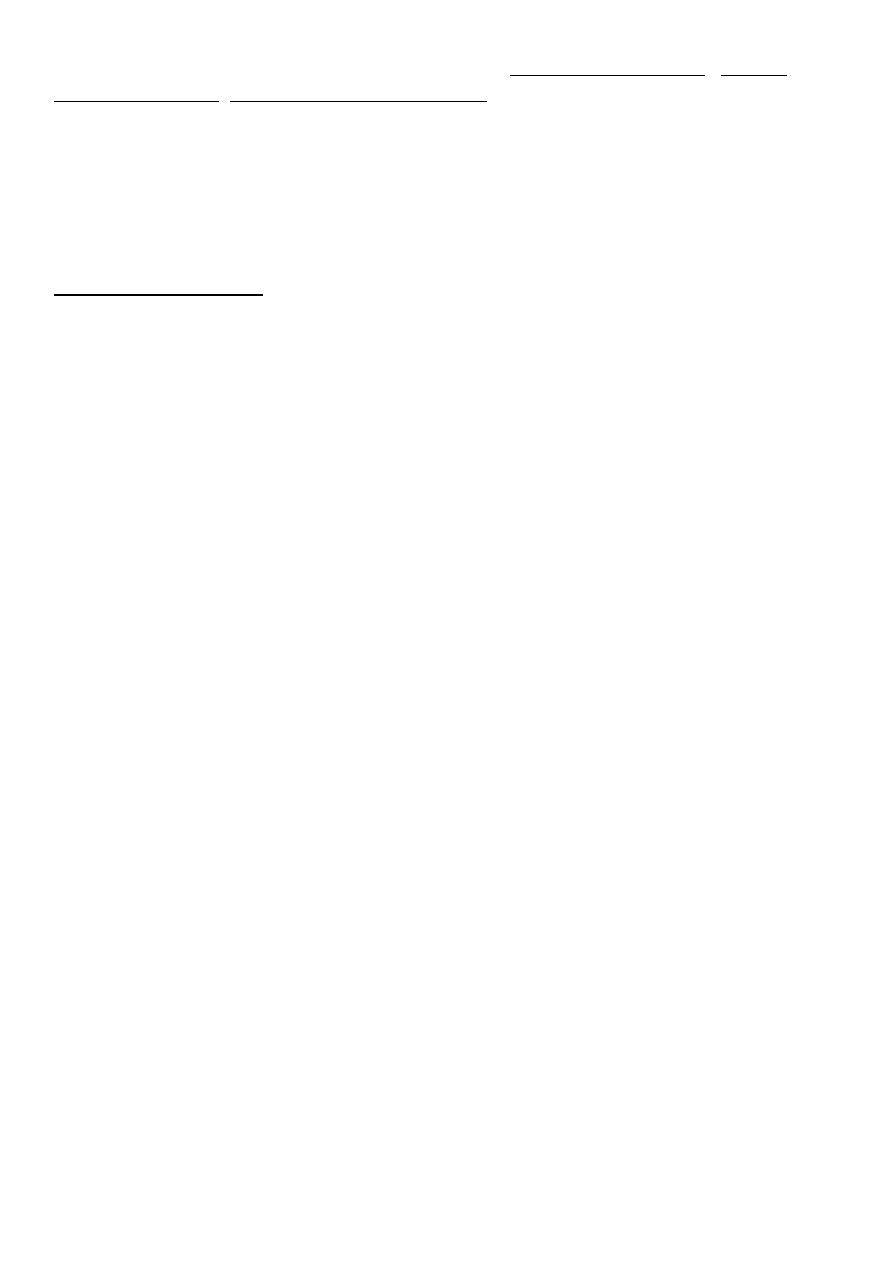
2-Long curved forceps Used for delivery of the
head from the midcavity,long
shank (6.5 cm),heavy weight .
3-Kielland’s forceps : It has a
sliding lock allows Sliding of one blade on
theother so it allows accurate placement at any
position or station of the head.
-the pelvic curve is initially backward then sweeps
forward but never reach the plane of the shank and
handle make a safe rotation in labour
:
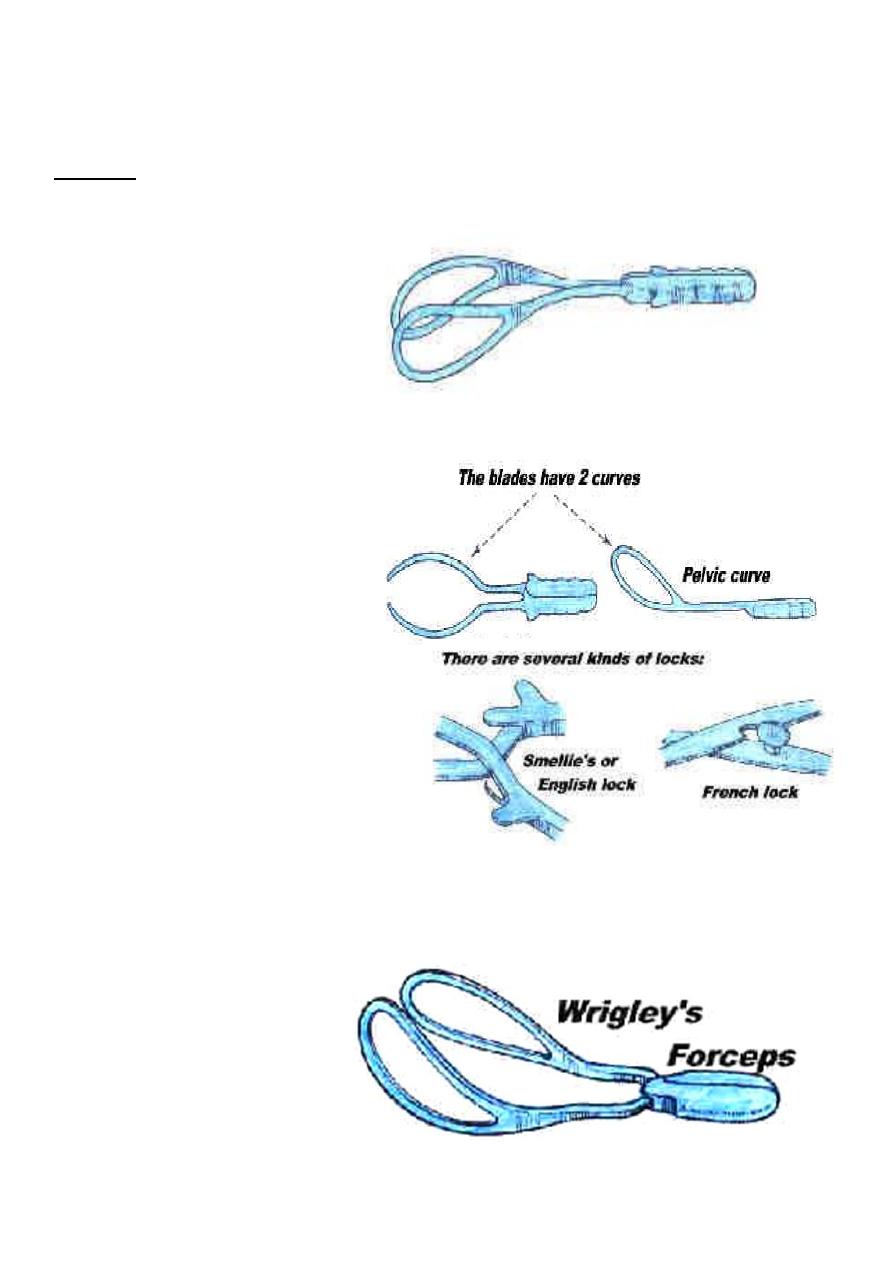
Types of vacuum
1.Rigid vaccum:
* O’neil * Bird * Malmstorm
2.Soft vacuum:cause less fetal injury ,higher failure rate
Funnel mashroom ring

7
Contraindication
Absolute :
1. lack of engagement .
2. Condition that contraindicate vaginal delivery.(pelvic abnormality , fetopelvic
disproportion)
3. Fetal malposition (face ,brow).
4. Dead fetus with postmortem changes .
5. Inability to diagnose the position of the fetal head .
Relative :
1. Fetal macrosomia .
2. Lack of experience .
3. Repeated fetal scalp blood sampling or trauma .
4. Fetal bleeding or suspected coagulation defect .
5. Premature < 34 weeks or less than 1500 gm .
Prerequisites for delivery with forceps and vacuum:
Assisted delivery should be carried as a trial with cautious attempt at delivery and is
appropriately carried out in the operative theater with immediate recourse to C.S. when
unusual difficulty is encountered at delivery.
:
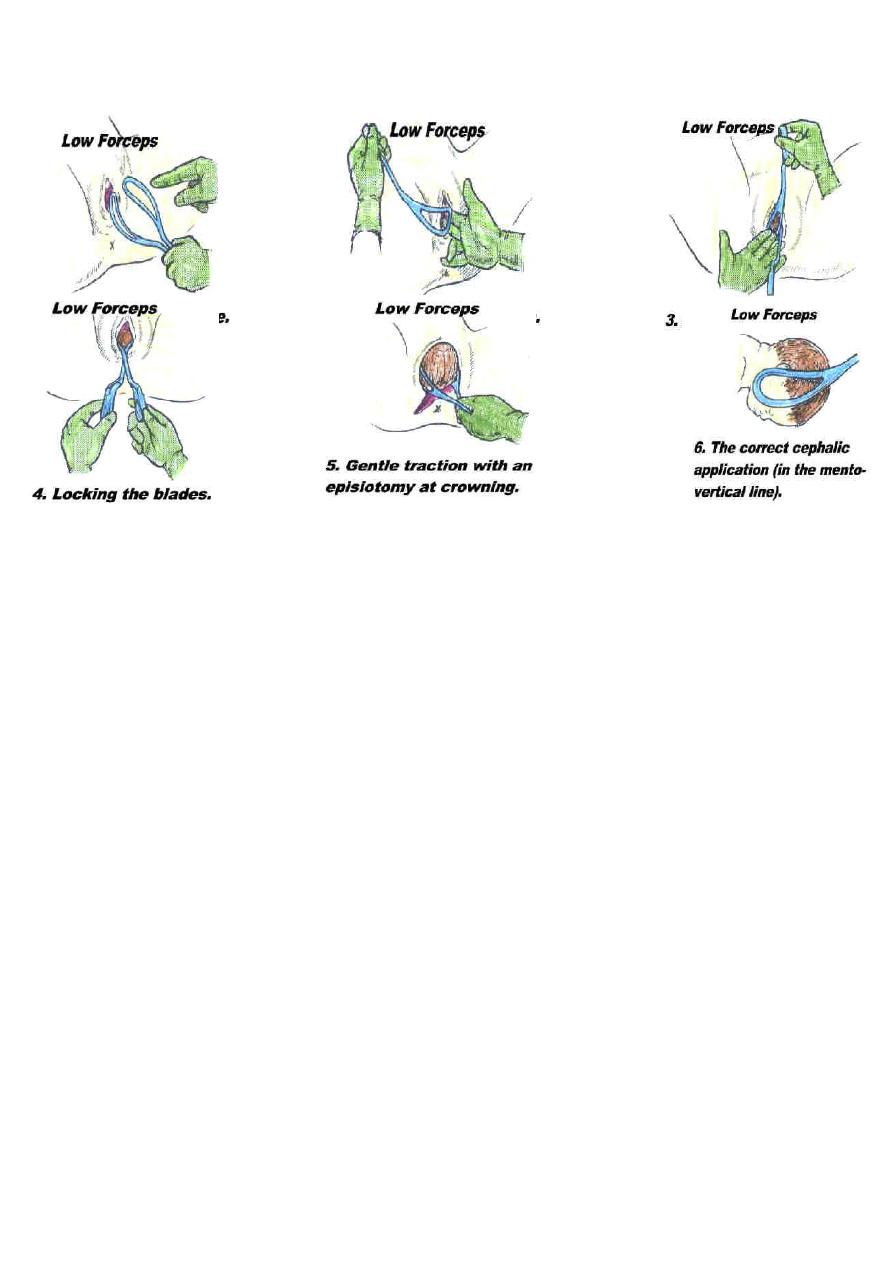
The following steps should be certain before application of forceps
1. Engaged head .
2. Position and attitude of the head .
3. Clinically adequate pelvis (mid ,outlet )
4. Empty bladder .
5. Ruptured membrane .
6. Cervix is fully dilated .
7. Appropriate anaesthesia (vacuum without )
8. Experience of the doctor .
9. Well informed patient .
10. working equipment .
8
Forceps application:
Technique of vacuum
- A betadine or antiseptic soap solution is applied to the rim of the cup the cup slipped
carefully in the vagina
.
-the cup is positioned over flexing point of fetal head
-the negative pressure of this system is increased to 0.2kg/cm2
-and perimeter of the cup is checked for intrapped cervical or vaginal tissue
-negative pressure is increased by 0.2kg/cm2 every 2 minute to a maximum pressure of
0.8kg/cm2 in order to build a chignon
.
-then at this point the traction in the axis of birth canal can be applied during uterine
contraction
-by placing hand in the vagina with the thumb in the cup an index finger on the fetal scalp .
traction force can be monitored in the following manner
-gradual increase in the traction force until the cup began to slip away from the fetal scalp ,
diminished fetal traction are then hold for the remainder of uterine contraction
-Release traction between uterine contractions
-the expectation is that the presenting part should descend with each push-pull event and the
head will be delivered within approximately 5 pulls
.
-the fetal heart is monitored through out the procedure with an external fetal heart monitor
once the head is delivered .the suction is disconnected and the cup removed
9
Complication of assisted delivery :
than vacuum .
is more common with forceps
Maternal complication :
Soft tissue injuries includes :
1-Genital : uterine ,cervical ,vaginal ,perineal lacerations .
Entrapment of the cervix is specific to the vacuum
2-Bladder and urethral injury : retention ,fistula .
3-Rectal injuries : laceration ,fistula ,defecation problem
Fetal complication :
: 1. Transient facial marks.
With forceps
2. Facial palsy .
3. Fracture of skull or facial bones .
4. Sever cervical cord damage .
:
With vacuum
1. Scalp injury . 6. Fracture of skull .
2. Cephalhaematoma . 7. Neonatal jaundice
3. Subgleal haematoma . 8. Retinal haemorrhage
4. Intracranial haemorrhage .. 9. Brachial plexus injury .
5. Tentorial tears . 10. cerebral palsy .
Episiotomy :
Episiotomy :Is a surgical incision of the perinium to increase the diameter of the vulval
outlet during childbirth
Indication
:
Absolute
1. previous pelvic reconstruction
pelvic floor surgery
.
2
:
Relative
1. short rigid perinium
.
shoulder dystocia
.
2
11
.
fetal distress
.
3
.
4.instrumental or breech delivery
Types of episiotomy:
1-Midline episiotomy :vertical incision towards the anus , less blood loss ,easier repair
,quicker healing , less pain in the postpartum period ,less dysparunia
.
risk of extension to the anus
2-Medio-lateral episiotomy : start at midline then laterally to avoid the anal sphinctor
3-Lateral episiotomy
Technique of episiotomy :
-Consent
-Anaesthesia as local infiltration
-Performed at crowning of the head to reduce the bleeding
-Sharp scissors used to make single incision about 3-6 cm length involving skin
,subcutaneous ,and superficial perineal muscules(2nd degree tear
.)
-Immediate suturing after delivery to reduce blood loss ,using interrupted or continuous
suturing of the muscules and subcutaneous tissues and subcuticular or interrupted suturing is
used for the skin
Complication:
1.Difficult repair.
2.heavy bleeding.
3.extention to the anus.
4.infection.
5.pain and dyspareunia.
6.weak point in the perinium-tear.
7.Dryness from injury to bartholine gland.
After care:
1.analgesia,oral or suppositories.
2.prophylactic antibiotics.
3.washing with water and soap.
4.hot sitz bath.
5.removal of stitches at 5 days.
