
1
Forth stage
Obstetric
Lec-3
.د
امنة
1/1/2016
Polyhydromnios & Oligohydromnios
Amniotic fluid
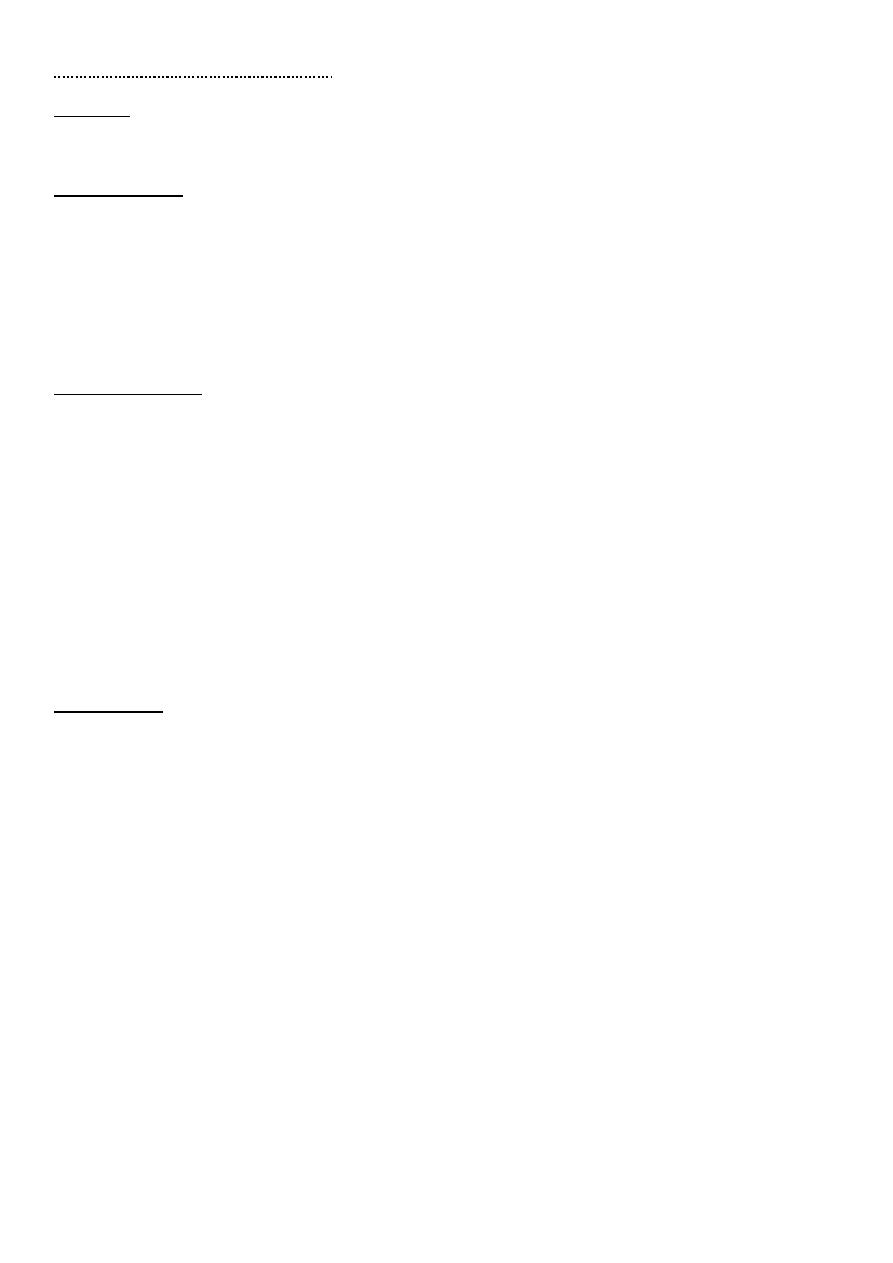
During the first trimester, amniotic fluid passes from maternal circulation into the amniotic
sac. Early in the second trimester, the baby starts to swallow the fluid, pass it through his
kidneys & excrete it as urine which he then swallows again, recycling the full volume of
amniotic fluid every few hours.
So the baby plays an important role in keeping just the right amount of fluid in amniotic sac.
It serve a vital function in protecting the developing baby from pressure or trauma, allowing
limb movement, hence normal posture development & permitting the fetal lungs to expand
& develop through breathing.
The amount of fluid gradually increases until reach its maximum volume of about 800 ml at
28 wks. This volume maintained until close to term when it begins to fall to about 500 ml at
week 40.The baby regularly swallow the amniotic fluid & its passed out as urine so the baby
controls the volume of amniotic fluid around him.
Sometimes, this system breaks down resulting in either too much or too little fluid , both of
which can present problems.
Clinical assessment of amniotic fluid volume
unreliable & objective definitions of
abnormalities in amniotic fluid volume depends
essentially on non-invasive method such as
ultrasound. These include;
1-the deepest vertical pool (DVP)
2-amniotic fluid index (AFI)
See fig.1
Fig.1 scoring the AFI or DVP

2
Deepest vertical pocket (DVP): it's performed by assessing a pocket of maximal depth of
amniotic fluid on ultrasound which is free of umbilical cord & fetal parts.
DVP between 2-8 cm considered normal.
< 2 cm considered as oligohydromnios.
> 8 cm considered as polyhydromnios.
Amniotic fluid index (AFI): is a score (expressed in cm) given the amount of amniotic fluid
seen in ultrasound of a pregnant uterus. It's an index for fetal well-being & it's a part of
biophysical profile. To determine AFI, we use 4 quadrant technique, when the deepest
vertical length of each pocket of fluid is measured in each quadrant & summing them.
An AFI between 8-18 is considered normal
< 5 considered as oligohydromnios
> 20-24 considered as polyhydromnios
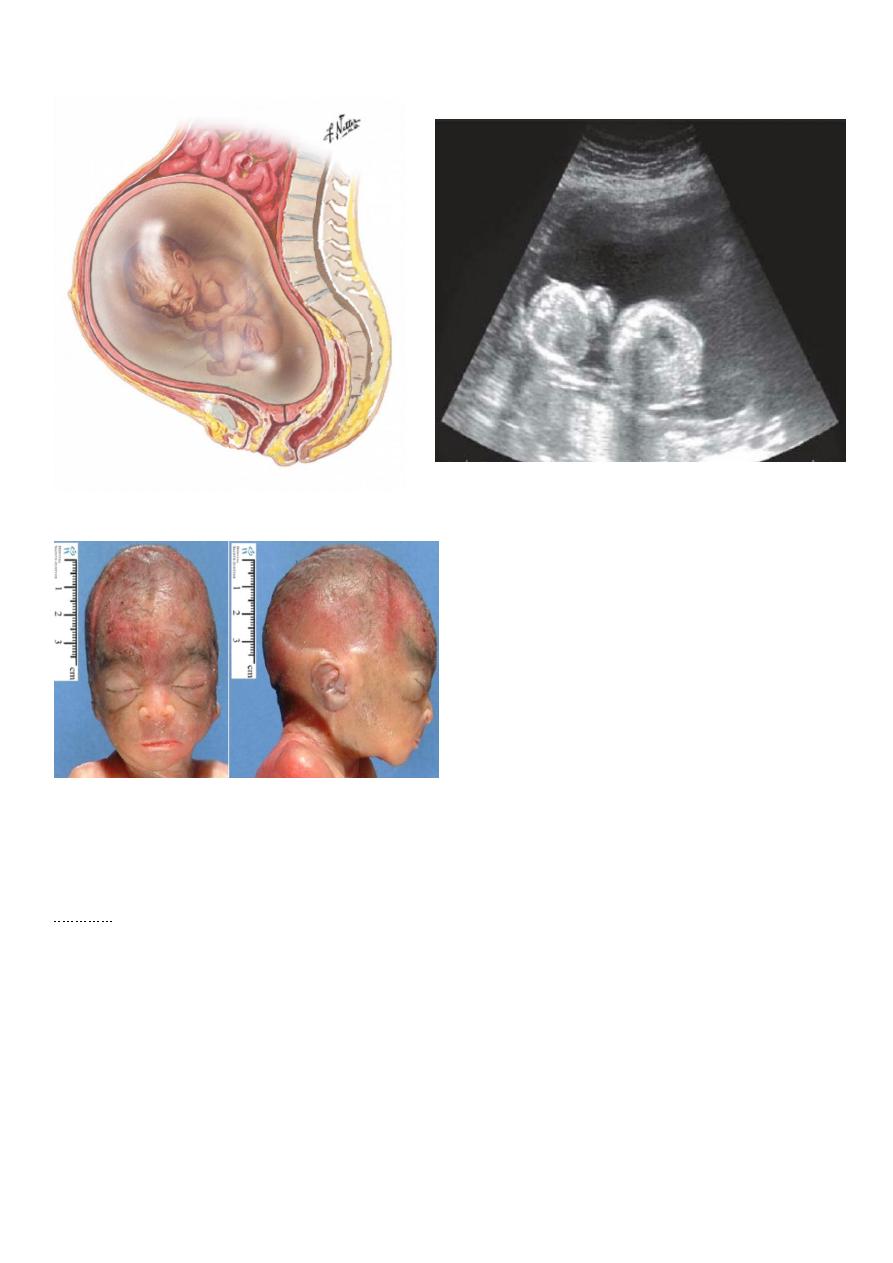
Oligohydromnios
Oligohydromnios is a condition in pregnancy characterized by a deficiency of amniotic
fluid, it is defined as AFV < 5th percentile for gestation, AFI < 5 or DVP < 2cm.
It complicates approximately 3.9% of pregnancies. Fig.2
Anhydromnios means no amniotic fluid.
Causes
1-preterm premature rupture of membrane (PPROM) (50%).
2-placental insufficiency commonly associated with IUGR.
3-congenital fetal anomalies.
....a-renal agenesis.
....b-renal dysplasia.
....c-urethral obstruction (atresia or posterior valve).
4-prolonged pregnancy or post-term.
5-maternal drugs as NSAID.
6-maternal complications as hypertension, dehydration, preeclampsia.
3
Assessment of oligohydromnios Fig.2 oligohydromnios
HISTORY
...History of PPROM, post maturity, drugs intake, less fetal movement.
EXAMINATION
...Clinical examination may reveal the presence of chronic hypertension or pre-eclampsia.
...Fetal pools may be very obviously felt, the uterus "full of fetus" because of scanty liquid.
...Fetal malpresentation
...Symphysiofundal height is small for gestation (small for date uterus).
INVESTIGATIONS
1-Ultrasound examination
...May reveal IUGR or presence of structural anomalies in kidney
...Biophysical profile
...Exclusion of congenital anomalies.
...Degree of oligohydromnios.
2-Color doppler ultrasound of both uterine & umbilical circulation.
3-Fetal specimen for karyotyping & viral infection.
TREATMENT
Depend on;
-Aetiology, Gestational age, Fetal status & Severity.
-bed rest
-maternal hydration to increase amniotic fluid volume either oral or IV hypotonic fluid
(2L/d).
-amnioinfusion during labour to prevent umbilical cord compression in severe cases of
oligohydromnios with serial USG to monitor growth, AFI, BPP.
-fetal surgery seems to improve survival in case of congenital lower urinary tract
obstruction.
-labour usually induced in the case of pregnancy at term or postdate or in case of ROM.

4
Complications of oligohydromnios
Fetal risk
1-perinatal mortality..due to congenital anomalies or prematurity or a sequelae of PPROM
including chorioamnionitis.
2-pulmonary hypoplasia, is a disorder of impaired lung growth, it's characterized by
diminished size.
3-skeletal deformities. Potter syndrome is the association of flattened facies, postural
deformities & pulmonary hypoplasia as sequelae of oligohydromnios, first reported in
association with bilateral renal agenesis.
4-prematurity.
5-fetal distress.
Maternal risk
1-increase the risk of CS due to fetal distress secondary to either IUGR, malformation or
cord compression.
2-high rate of physician intervention.
Fetal prognosis
The aetiology of oligohydromnios has an effect on perinatal mortality as pulmonary
hypoplasia & limb deformities are common.
Renal agenesis carry bad prognosis after birth.
Sever oligohydromnios prior to 24 wks carries a poor prognosis.
Polyhydromnios
Polyhydromnios is an excess amount of amniotic fluid it's defined as AFV above 95th
centile for gestational age, AFI> 20-24 or DVP of >8 cm. It complicates 2-3% of
pregnancies. It's more common in multipara than in primi. See fig.4
Classification of severity
Mild....DVP=8-12 cm
Moderate.....DVP=12-15 cm
Severe......DVP=>15 cm.
5
Fig.4 polyhydromnios
Fig.3 Potter syndrome
Causes
1-Maternal
...DM
2-Fetal
...intestinal obstruction (duodenal, esophageal atresia).
...esophageal compression secondary to thoracic or mediastinal mass as diaphragmatic
hernia.
...impairment of swallowing due to CNS lesion as anencephaly.
6
...chromosomal abnormalities as trisomy 18
...fetal polyuria
...multiple gestation (twin-twin transfusion syndrome) causing acute polyhydromnios.
...cardiac failure due to fetal anemia.
...congenital infection
...fetal hydrops secondary to high output cardiac failure. Fig.3 Potter syndrome
3-Placental
...chorioangioma of placenta
4-idiopathic.
Assessment of polyhydromnios
HISTORY
...A careful history, with attention to maternal symptoms, dis.such as DM or recent viral
infection is important.
...The woman may notice that her abdomen is enlarged quickly & the fetus unusually
mobile.
...If the uterus is very much enlarged she may have dyspnoea & indigestion.
...In rare cases of acute poly hydromnios, there is abdominal pain & vomiting.
...It may present as severe abdominal swelling & discomfort.
EXAMINATION
...the abdomen will appear distended.
...the uterus is larger than expected for the duration of pregnancy (large for date uterus).
...abdomen may be tense, tender & fetal pools will be hard to palpate.
...oedema of abdominal wall & vulva is some time seen.
...the presentation is unstable.
...it may be difficult to hear fetal heart beat.
7
INVESTIGATION
1-Ultrasound scanning to assess;
...degree of polyhydromnios
...identify multiple pregnancy & fetal anomaly
2-Karyotype if there is structural abnormalities.
3-investigation to mother for DM.
4-screening for viral infection.
TREATMENT
1-Polyhydromnios without symptoms & without any evidence of fetal abnormallties
requires NO treatment.
2-treatment indicated when there is severe polyhydromnios, aim of treatment is to reduce
maternal discomfort & prolong pregnacy.
A-when pregnancy remote from term & woman is in discomfort & there are no fetal
abnormalities, options of treatment are;
1- medical treatment
...prostaglandin synthetase inhibitors (indomethacin)...decrease fetal urine output then
decrease polyhydromnios but the side effect of it that it causes premature closure of ductus
arteriosus.
2-amniocentesis
...aseptic slow aspiration of amount of liquor from amniotic sac under ultrasound guide.
Serial amniocentesis carries a risk of precipitating preterm labour & leads to rapid re-
accumulation of liquor.
3-correction of underlying pathology as correction of blood sugar in diabetic mother
B-in case near term in which the woman is in serious discomfort, labour should be induced.
Intrapartum management
1-allow labour to progress & monitor progress of labour by partogram.
2-during labour, rupture of membrane done with slow release of liquor by controlled ARM
to decrease risk of abruptio placenta.
3-check for cord prolapses when membrane ruptured.
4-active management of 3rd stage of labour as PPH can occur due to uterine atony due to
uterine over distension.

8
Complications of polyhydromnios
Fetal risks
1-perinatal mortality ranging from 10-30% which is secondary to the presence of congenital
abnormalities & preterm delivery.
2-hypoxia secondary to cord prolapse & abruption placenta.
Maternal risks
Maternal complications mostly attributed to uterine distension & include;
1-abdominal discomfort
2-spontaneous preterm labour
3-spontaneous rupture of membrane with risk of
...umbilical cord prolapse
...abruption placenta due to sudden decompression of uterus.
4-malpresentation & unstable lie.
5-post-partum hemorrhage due to post-partum uterine atony.
6-increase incidence of CS due to unstable lie & placenta abruption.
7-higher incidence of pre-eclampsia that may be a manifestation of mirror syndrome in
association with fetal hydrops.
