1
Forth stage
Obstetric
Lec-7
.د
امنة
1/1/2016
Obstetrics injuries
These include;
1~Rupture of uterus
2~Cervical tears
3~Vaginal tears
4~Haematoma of vulva
5~Perineal tears
6~Trauma to the pelvic joints and nerves
Rupture of uterus
It's define as disruption of the continuity of the pregnant uterus. It's an obstetrics emergency.
Incidence ; about 1:4000, 95% of cases occur in multipara particularly grand multipara.
Rupture occurs at junction of upper & lower segment or at site near the point of uterine vesseles .
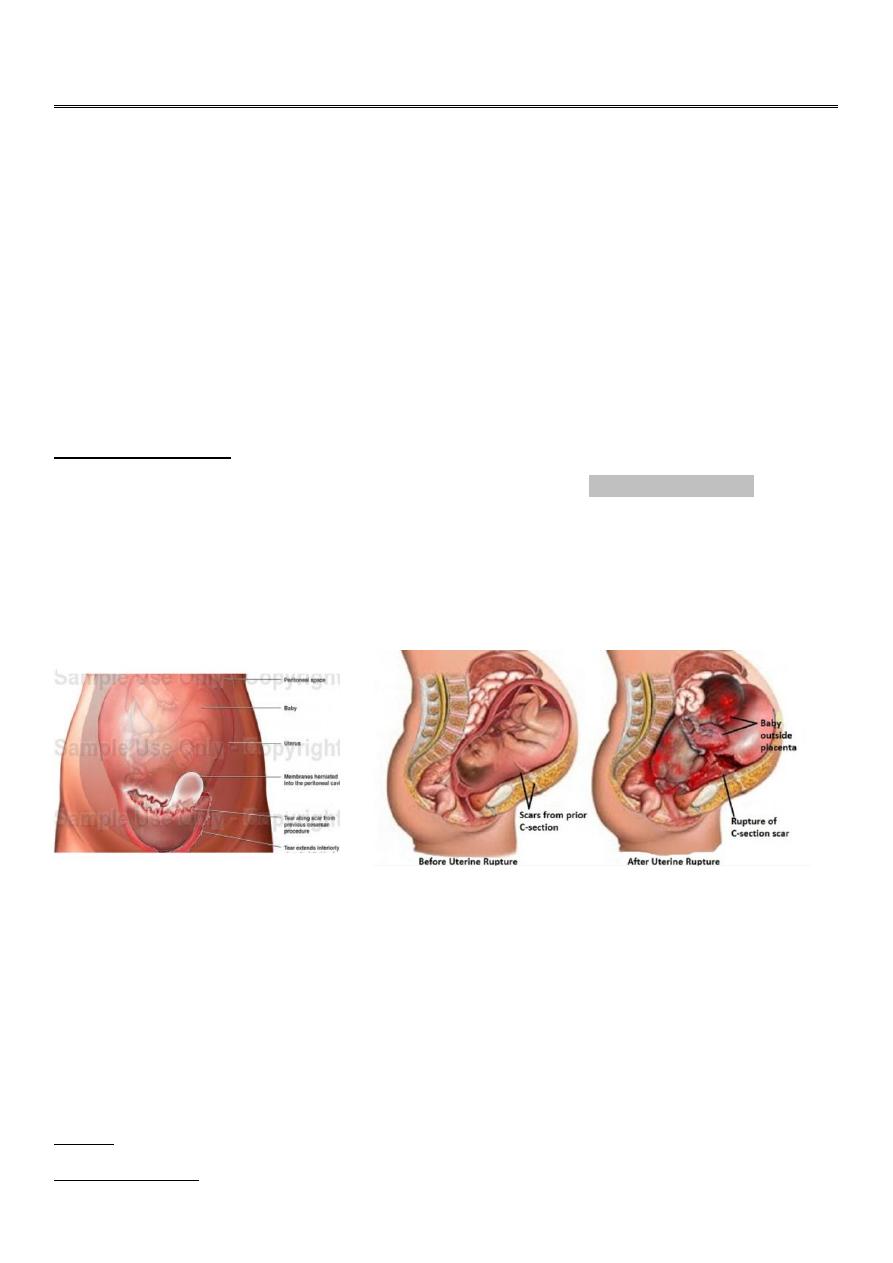
Bleeding may occur into peritoneal cavity or may track down between bladder& upper vagina.Fig.1
Fig.1 rupture uterus
Types
1~complete involving the whole uterine wall including the peritoneum .
2~incomplete, not involving the peritoneal coat .
Causes
1-during pregnancy
2
A-spontaneous
-rupture of a uterine scar eg. previous CS mainly upper segment CS, myomectomy, hysterotomy.
-abruptio placenta with severe concealed haemorrhage.
-rupture of a rudimentary horn at the 4th-5th month.
B -traumatic
-perforation during vaginal evacuation.
-external trauma.
2-during labour
A-spontaneous
-obstructed labour
-rupture of uterine scar
-grand multipara due to degeneration and overthining of the uterine muscle .
B-traumatic
-internal version
-manual removal of placenta
-instrumental delivery eg.forceps or ventous applications before full cervical dilatation.
C-improper use of oxytocin
Clinical pictures
A~impending rupture
Before actual rupture, the following manifestations may be detected
~lower abdominal pain
~tender uterine scar
~vaginal spotting (minimal bleeding).
B~actual rupture
Symptoms
~sudden severe abdominal pain (it's differentiated from labour pain being continuous).
~if the patient was in labour, there is cessation of uterine contractions.
~shoulder pain on lying down due to irritation of the phrenic nerve by accumulating blood under
diaphragm.
~silent rupture, minimal symptoms may occur in rupture lower segment scar due to presence of fibrosis.
3
Signs
General examination ...patient may be in shock state. This may appears post partum in case of traumatic
rupture uterus.
Abdominal examination
...examine the scar of previous operation .
...fetal parts are prominent and felt easy abdominally
...the presenting part recedes upwards
...abnormal fetal attitude and lie.
...FH sound usually undetected.
...in incomplete rupture, the fetous still inside the uterus with suprapubic painful tender swelling which is
an accumulated blood in the vesico-uterine pouch .
Vaginal examination
...the presenting part recedes upwards.
...vaginal bleeding may be present.
...contracted pelvis may be detected.
Differential diagnosis
...abruptio placenta
...disturbed advanced extrauterine pregnancy
...other causes of acute abdomen
Treatment
1-shout for help
2-blood transfusion and anti-shock measures (wide bore canula, iv crystalloid solution, oxygen )
3-immediate laparotomy.
4-deliver the fetous and placenta.
5-explore the rupture site.
...if it's amenable for repair & the patient didn't complete her family....repair is done.
...if it's not amenable for repair...hysterectomy is done.
6-exploration of the other viscera mainly the bladder .
7-internal iliac artery ligation may be needed in case of broad ligament hematoma.
8-vaginal repair if there is slight extension of a cervical tear.
4
9-monitor pulse & blood pressure
10-insert foley catheter & monitor urine output
11-post operative care ;
-antibiotics & analgesia.
-family planning & take a period of time before next pregnancy with good antenatal care, if she becomes
pregnant she should deliver by CS .
prventive measures
##During pregnancy ;
1-good antenatal care for assessment of pelvis, fetal size, presentation& position.
2-planning for hospital delivery for a patient who has previous CS
3-training to midwifes to recognize high risk pregnancy & time of referal to hospital .
##During labour ;
1-monitor the labour using partogram
2-proper use of oxytocin
3-hard pressure on abdomen should be avoided to force delivery
4-early diagnosis of complications
5-exploration of the genital tract after difficult labour or instrumental delivery
Complications
(
risks
)
A~maternal
...shock
...haemorrhage
...paralytic ileus
...bladder, ureter or visceral injuries
...infection
...maternal death
B~fetous
...death due to asphyxia from detachment of placenta .
5
Cervical lacerations (tear ).
more common on left side.
Aetiology
1- ventous or breech extraction before full cervical dilation
2-manual dilatation of cervix
3-improper use of oxytocin
4-precipitate labour
Predisposing factors
...cervical rigidity
...scarring of the cervix
...edema as in prolonged labour
...placenta previa due to increased vascularity
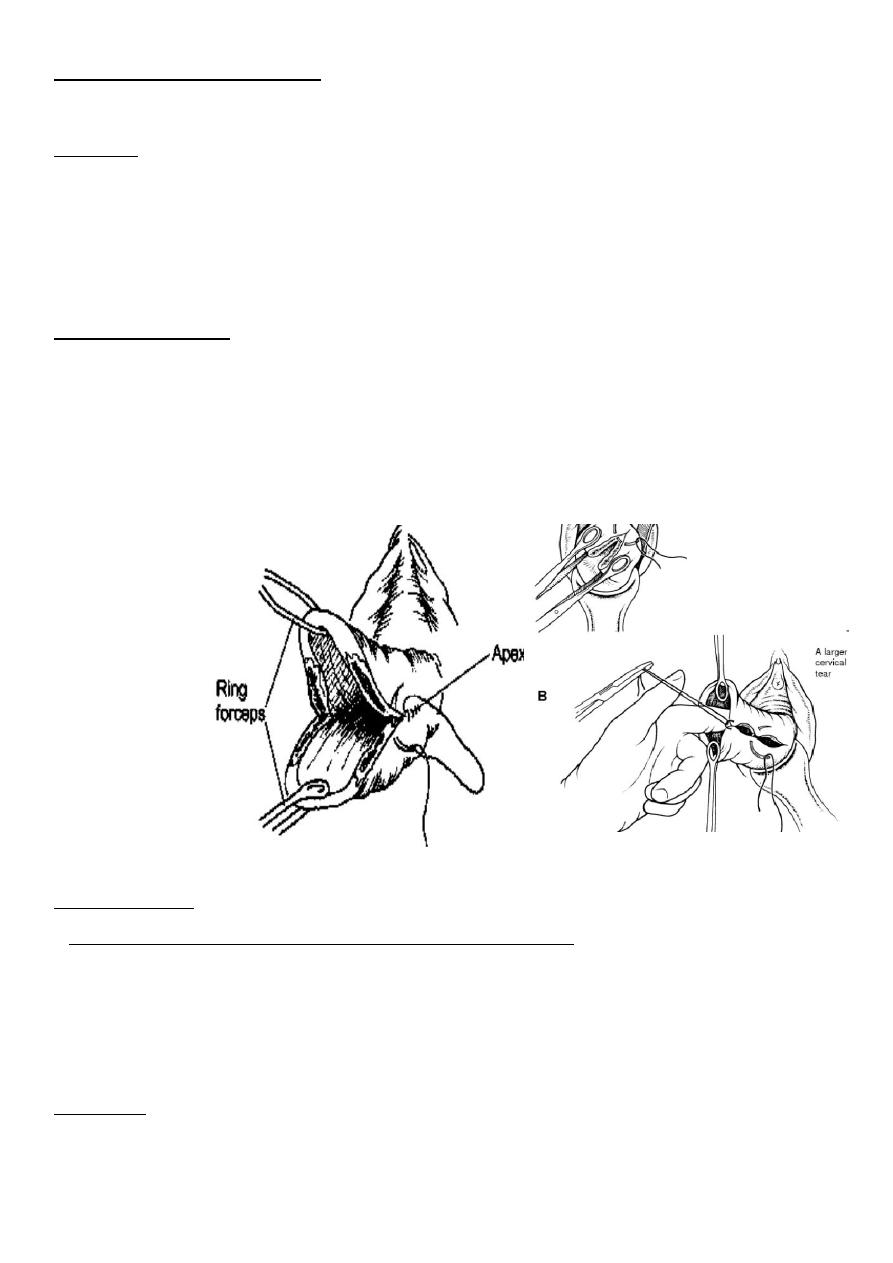
Fig.2 cervical tear .
Fig.3 repair of
cervical tear
Clinical features
1-sever vaginal bleeding after delivery inspite of well contracted uterus .
2-vaginal examination ;the tear can be felt
3-speculum exam; using a posterior wall self retaining speculm or vaginal retractor & 2ring forceps to grasp
anterior & posterior lips of cervix . so the tear can be visualized .Fig.2
Treatment
Immediate repair: is carried out under general anaesthesia with good light exposure.
6
Interrupted cut gut dexon or vicryl sutures are taken starting from above the apex of the tear to control
bleeding from the retracted blood vessels. Fig.3
If the apex is not easily seen a traction on a stitch taken as high as possible in the tear will show the apex.
Complications
1-PPH
2-rupture uterus due to upward extension
3-infection; cervicitis & parametritis
4-cervical incompetence leading to future recurrent abortion or pre-term labour
5-ureteric injury from extension of tear or during its repair .
Vaginal lacerations
Causes
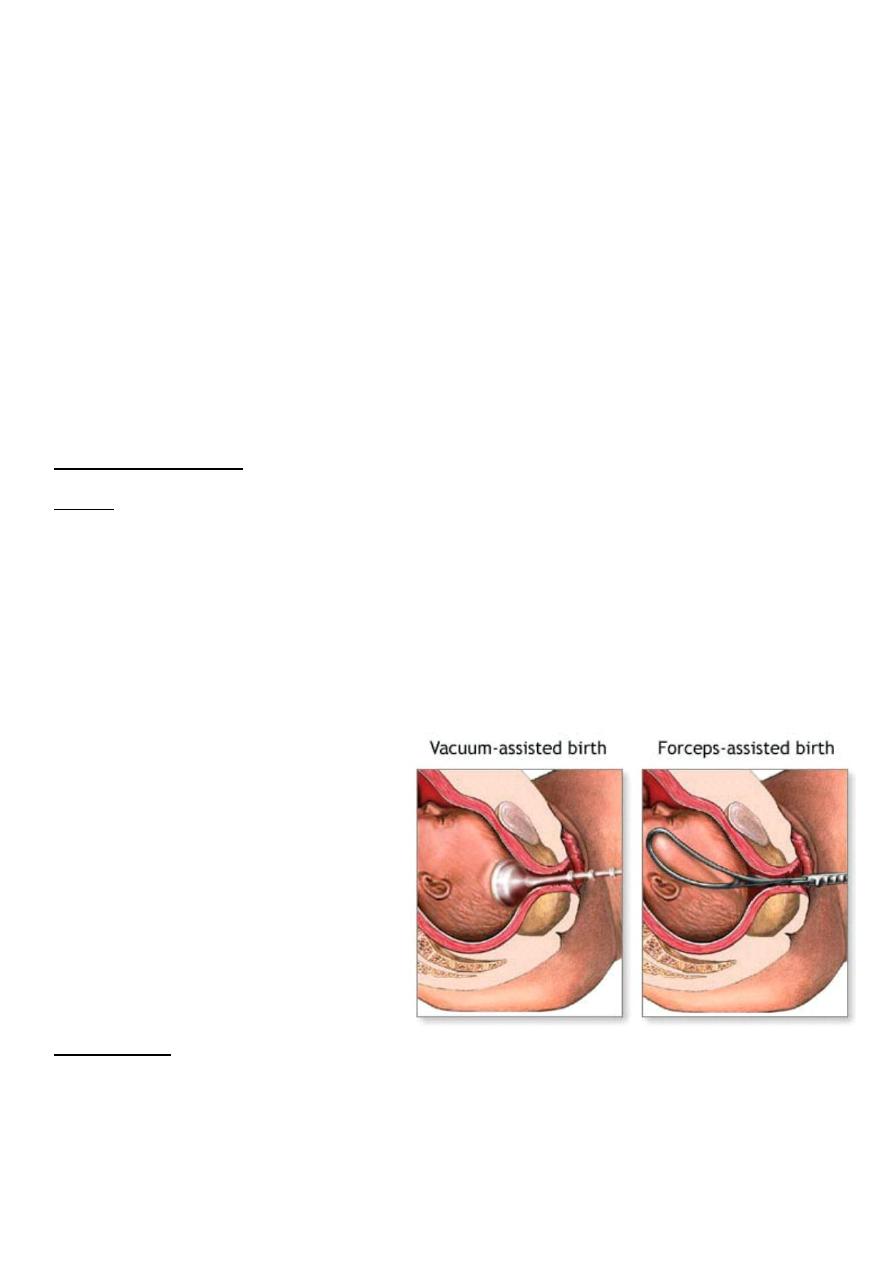
Primary lacerations less common and caused by: Fig.4
...Forceps application.
...Destructive operations.
...Vacuum extraction if the cup sucks a part from the vaginal wall.
Secondary lacerations: more common and are due to extension from perineal or cervical tears
Fig.4 instrumental delivery
Management
Immediate repair: Continuous locked cat gut sutures are taken starting from above the apex to control
bleeding from the retracted blood vessels.
Tight pack: may be needed to control bleeding from a raw surface area. Foley's catheter should be inserted
before packing and both are removed after 12-24 hours.
7
Hematoma of genital tract
A.Vulval (Infra-Levator) Haematoma
Causes
:
*Traumatic due to:
...incomplete haemostasis during repair of episiotomy or tear.
...Direct trauma as kick or falling down.
*Spontaneous: due to rupture of a varicose vein.
Clinical picture
The haematoma usually appears 12-48 hours after delivery.
The collection of blood is limited by the levator ani above but laterally it may extend to fill the ischiorectal
fossa reaching a volume of 500 ml or more.
There is a progressive enlarged, painful, tender, tense, bluish swelling at the vulva.
Manifestations of hypovolaemia (e.g. hypotension and rapid pulse) and anaemia may be present.
B.Vaginal (Supra-Levator) Haematoma
Causes
:
Deep vaginal lacerations (see before).
Clinical picture:
The blood is collected paravaginally above the levator ani muscle.
It may not be visible externally.
It may not be painful until reaching a large size.
Manifestations of hypovolaemia and anaemia may be present
Management
:
**Small not-increasing haematoma (less than 5cm);is managed conservatively as it usually resolves
spontaneously. Prophylactic antibiotic may be given to guard against secondary infection with analgesia
with blood transfusion if patient anaemic .
**Large increasing haematoma:
...It is incised longitudinally,
...evacuation of the clotted blood,
...bleeding points are ligated,
...the gap is closed in layers.
8
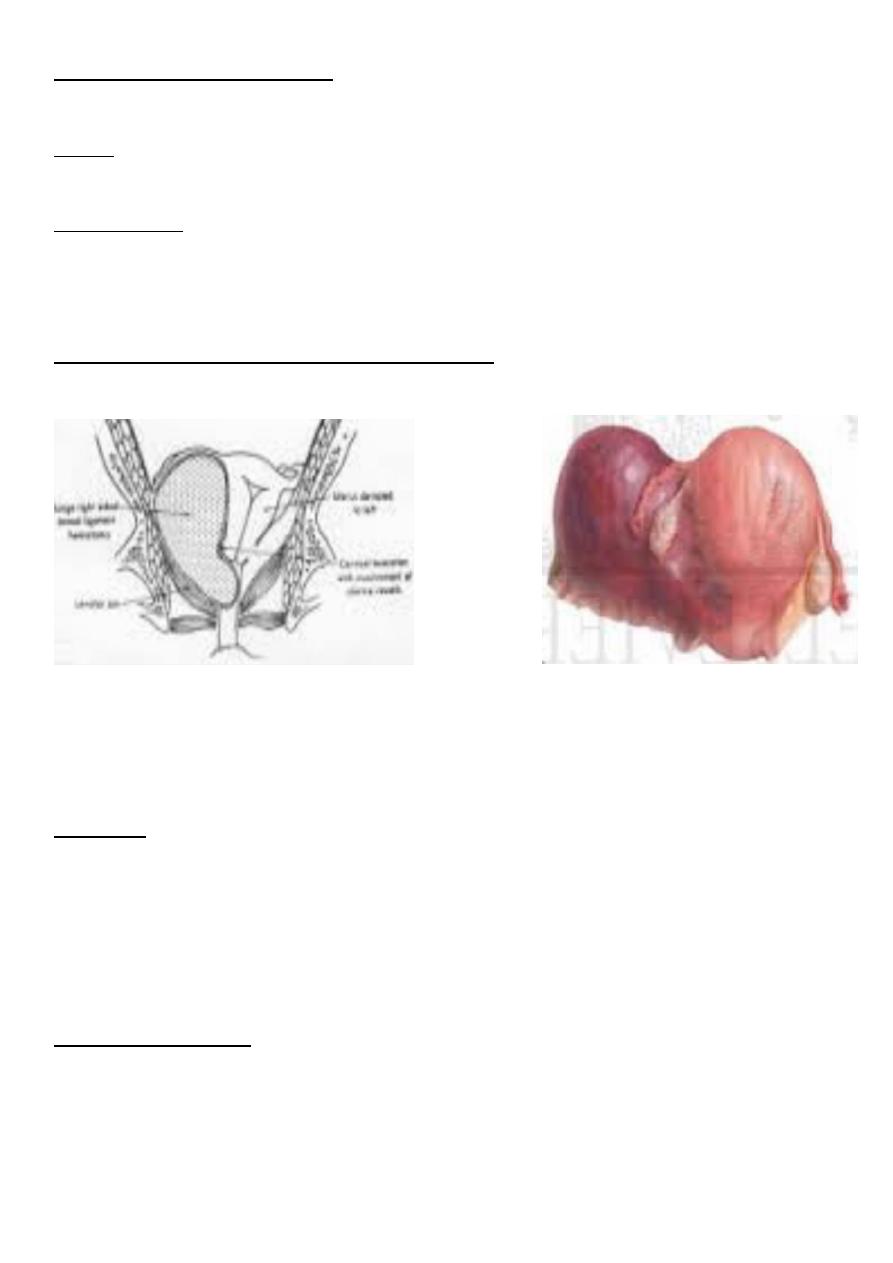
Broad ligament haematoma
Form in broad ligament, it may follow spontaneous vaginal delivery or CS.
Causes
Upper vaginal,cervical or uterine tears which usually involve the vaginal or uterine artery.
Clinical picture
Hypovolaemia, anaemia or shock: is usually present due to large amount of internal haemorrhage.
Swelling on one side of the uterus which increasing over a period of hours or days and may reach up to the
lower pole of the kidney or even the diaphragm.
The uterus is felt separate and deviated to the opposite side. Fig.5
Fever, ileus and unilateral leg oedema: may develop later.
Fig.5 broad ligament haematoma
Treatment
*Small not-increasing haematoma: is managed conservatively as vulval haematoma.
Antibiotics, blood transfusion may be required.
*Large increasing haematoma: Laparotomy,Evacuation of the blood clots,Securing haemostasis, bilateral
internal artery ligation or hysterectomy may be indicated(rare).
Perineal lacerations
Anatomy
The perineal body is a pyramidal mass of tissues about 4´ 4 cm between the lower vagina anteriorly, the
anal canal and lower rectum posteriorly.
It is composed of the following layers respectively:
9
Skin.
Superficial fascia.
Perineal muscles;
external anal sphincter,
superficial and deep perinei muscles,
bulbocavernosus, and
ischiocavernosus.
※They contract during intercourse and defecation.
※During delivery, they may be markedly stretched and teared.
Aetiology
Lack of perineal elasticity:
Elderly primigravida.
Excessive scarring from a previous operation as posterior colpoperineorrhaphy.
Friability due to perineal oedema.
Marked perineal stretch allowing head extension before crowning.
Macrosomic baby.
Face to pubis delivery.
Forceps delivery.
Narrow subpubic angle pushing the head backward.
Rapid perineal stretch
Precipitate labour.
Rapid delivery of the after-coming head in breech presentation.
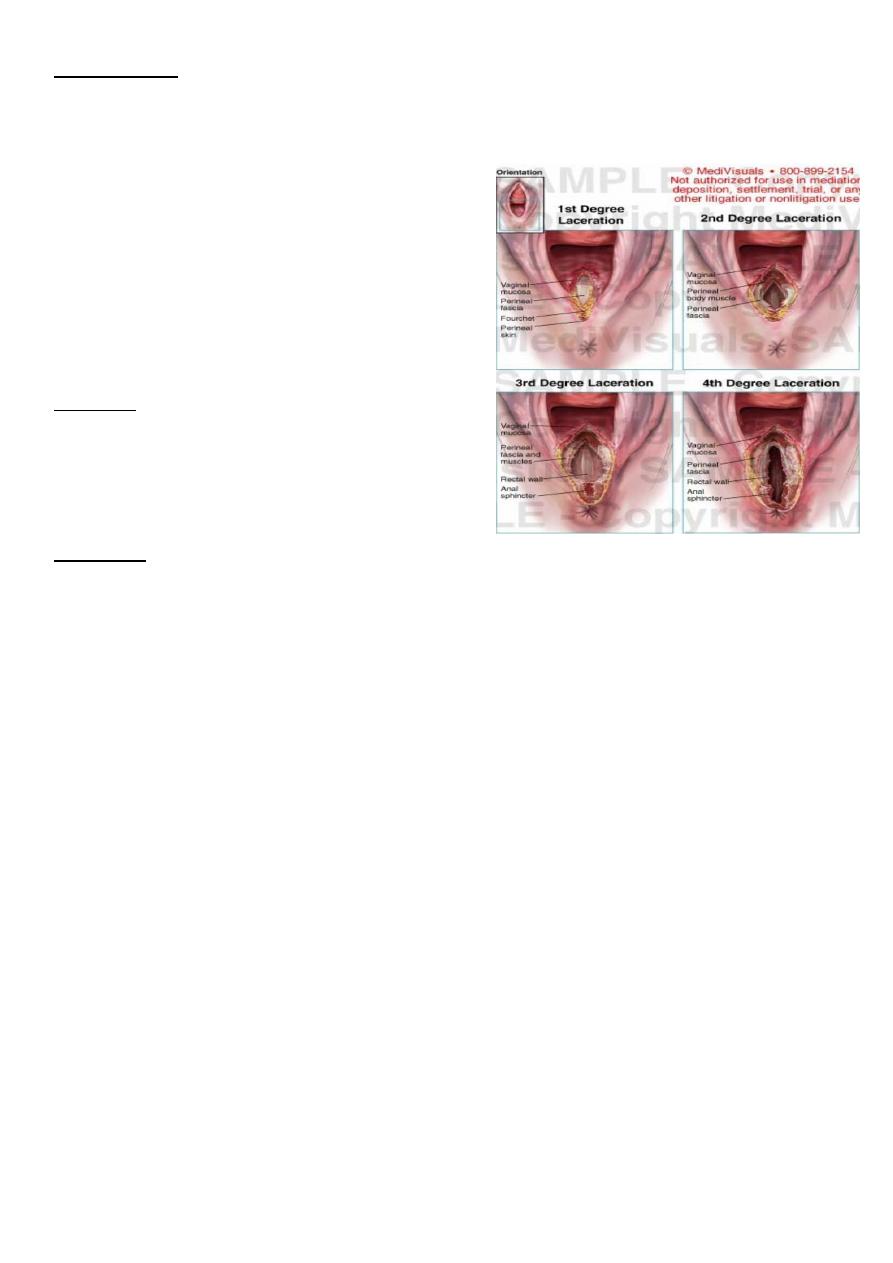
Degree
First degree: involves the perineal skin, and the posterior vaginal wall.
Second degree: involves the previous structures + the muscles of the perineal body but not the external
anal sphincter.
Third degree: involves the previous structures + the external anal sphincter.
Fourth degree: involves the previous structures + the anterior wall of the anal canal or rectum.
Incomplete perineal tear = 1st or 2nd degrees.
Complete perineal tear = 3rd or 4th degrees. See fig.6
Hidden perineal tear: The levator ani muscle is teared without apparent perineal tear predisposing to
future prolapse.
11
Complications
1-Postpartum haemorrhage.
2-Puerperal infection.
3-Incontinence of stool and flatus in unrepaired or
imperfectly repaired 3rd or 4th degree tear.
4-Residual recto-vaginal fistula in imperfectly repaired 4th
degree tear.
5-Future genital prolapse.
6-Dyspareunia due to tender vaginal scar.
Prevention
*Proper management of second stage of labour.
*Episiotomy in the proper time.
Treatment
.
Fig.6 perineal tear
Any perineal tear should be repaired within 24 hours.
Can be repaired under local infiltration anaesthesia.
1-First degree tear:
The vaginal wall is repaired with continuous locked or interrupted sutures and the skin with interrupted
sutures.
2-Second degree tear:
The perineal muscles are approximated by interrupted chromic cut gut sutures.
The vagina is sutured as in the 1st degree tear.
The superficial perineal muscles are sutured by interrupted chromic cutgut.
The skin is sutured as in the 1st degree tear.
3-Third degree tear:
The torn ends of the external anal sphincter is identified and sutured together by interrupted cutgut.
The levator ani muscles are approximated in front of the rectum.
The vagina, superficial muscles and skin are sutured as before.
4_Fourth degree tear:
The rectal wall is sutured by 2 layers of inverted interrupted cutgut not including the mucosa.
The external sphincter, levator ani, superficial muscles and skin are sutured as before.

11
Post operative care
*The perineal wound is kept clean and sterile by using antiseptic solution after each micturition or
defecation.
In the complete perineal tear:
*Intravenous fluid for 48 hours,
*soft, low residue diet for an additional 48 hours,
*regular diet after that, laxatives are not used in the first 4-5 days, but stool softeners are allowed.
*Prophylactic antibiotic is given.
Maternal n. injuries during labour
*foot drop (pressure on popliteal nerve near neck of fibula by leg support .
*injury of 4th & 5th lumber n roots .
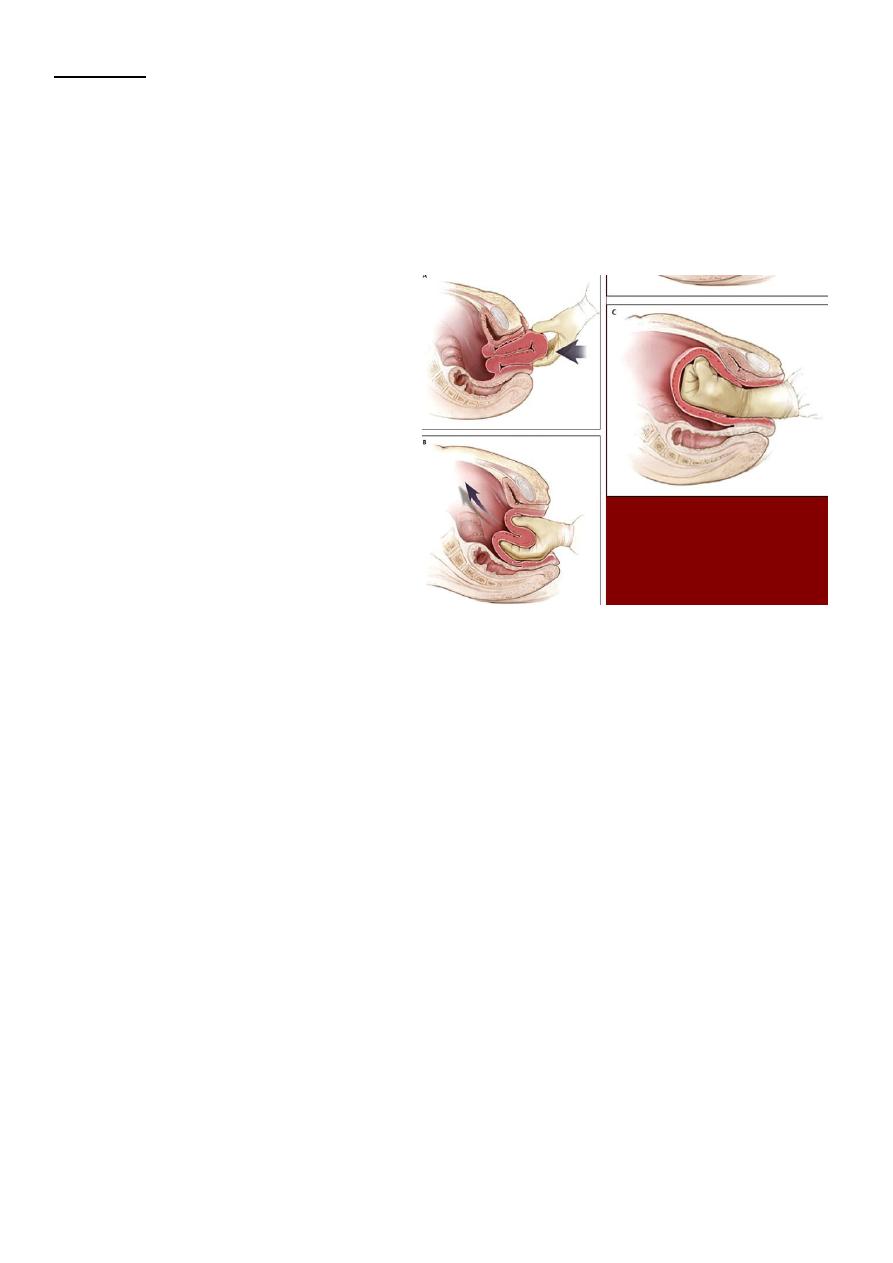
Uterine inversion
The body of the uterus becomes partially or completely turned out (inside out) after delivery of fetus .it
can be fatal if untreated.There is descent of uterine fundus into cavity through cervix or even through
vulva. It's very rare. Fig.7
Causes
Improper management of third stage of labour by pulling the umbilical cord or pressing on fundus while
the uterus is not contracting & placenta has not yet separated.
Symptoms & signs
*Pain
*Shock out of all proportion to visible blood loss.inversion exerts traction on peritoneal structures which
can elect a profound vasovagal response. There is a risk of profuse bleeding due to uterine atony causing
hypovolemic shock as well.
*appearance of uterine fundus at vulva sometimes .
Note ; unexplained shock during third stage of labour should always suggest possibility of uterine
rupture or uterine inversion & vaginal examination should be done .
12
Treatment
1-immediate intravascular volume expansion with IV crystalloids.
2-immediate replace the uterus through cervix by manual compression by hand to avoid oedema of uterus
which making replacement more difficult. If this fails, hydrostatic pressure works well .
3-give oxytocin to encourage uterine contraction after replacement.
4-surgical replacement rarely required.
Fig.8 manual replacement of uterus
