1
Forth stage
Obstetric
Lec-4
.د
امنة
1/1/2016
PRE-LABOUR RUPTURE OF MEMBRANES ( PROM )
Pre-labour rupture of membrane (PROM) refers to spontaneous rupture of membrane with
leakage of amniotic fluid in the absence of uterine activity at any gestational age. It's a
common clinical problem seen in every day practice in obstetrics.
According to gestational age it is either;
*Term premature rupture of membrane (TPROM) refers to a patient who is beyond 37 wks
gestation & has present with rupture of membrane prior to the onset of labour. It's occurs
in 8% of term pregnancies.
*Preterm premature rupture of membrane (PPROM) is rupture of membrane prior to
37wks gestation. It's occurring in 2-3% of preterm pregnancies.
When PROM occurs, the fetus loses the relative isolation & protection afforded within the
amniotic cavity. The interval between rupture membrane & the
onset of contractions is referred to as the latency period.
Anytime ROM lasts > 18hr before delivery is considered as
prolonged ROM.
Most patients (90%) enter spontaneous labour within 24 hr
when they experience ROM at term. The latency period tend to
be longer with decreasing gestational age as at 32 wk, only 50%
will labour within 24-48 hr.s
Aetiology
Term PROM
Rupture of membrane at term usually reflects physiological
processes. Programmed cell death & activation of catabolic
enzymes & mechanical forces result in ruptured membrane.
Preterm PROM
It usually has pathological origins
1-ascending infection appears one of the major causes. Most of infection appears
subclinical & give few signs or symptoms.
2-antepartum hemorrhage (APH).
3-cervical weakness (incompetence), failure of cervix to be a barrier to ascending infection
& by allowing membrane to prolapse.
2
4-maternal smoking.
Risk factors
Most risk factors for preterm labour can be applied to PPROM Fig.1 ROM
1-low socioeconomic status
2-low body mass index.
3-smoking
4-history of previous preterm labour.
5-UTI
6-vaginal bleeding at any time in pregnancy
7-amniocentesis.
Complications (risks) of PROM.
A-Maternal risks
1-intrauterine infection
2-abruption placenta
3-PPH
4-retained placenta
5-puerperal sepsis & septic shock leading to maternal death.
B-Fetal risks
1-infection
2-prematurity & its complications
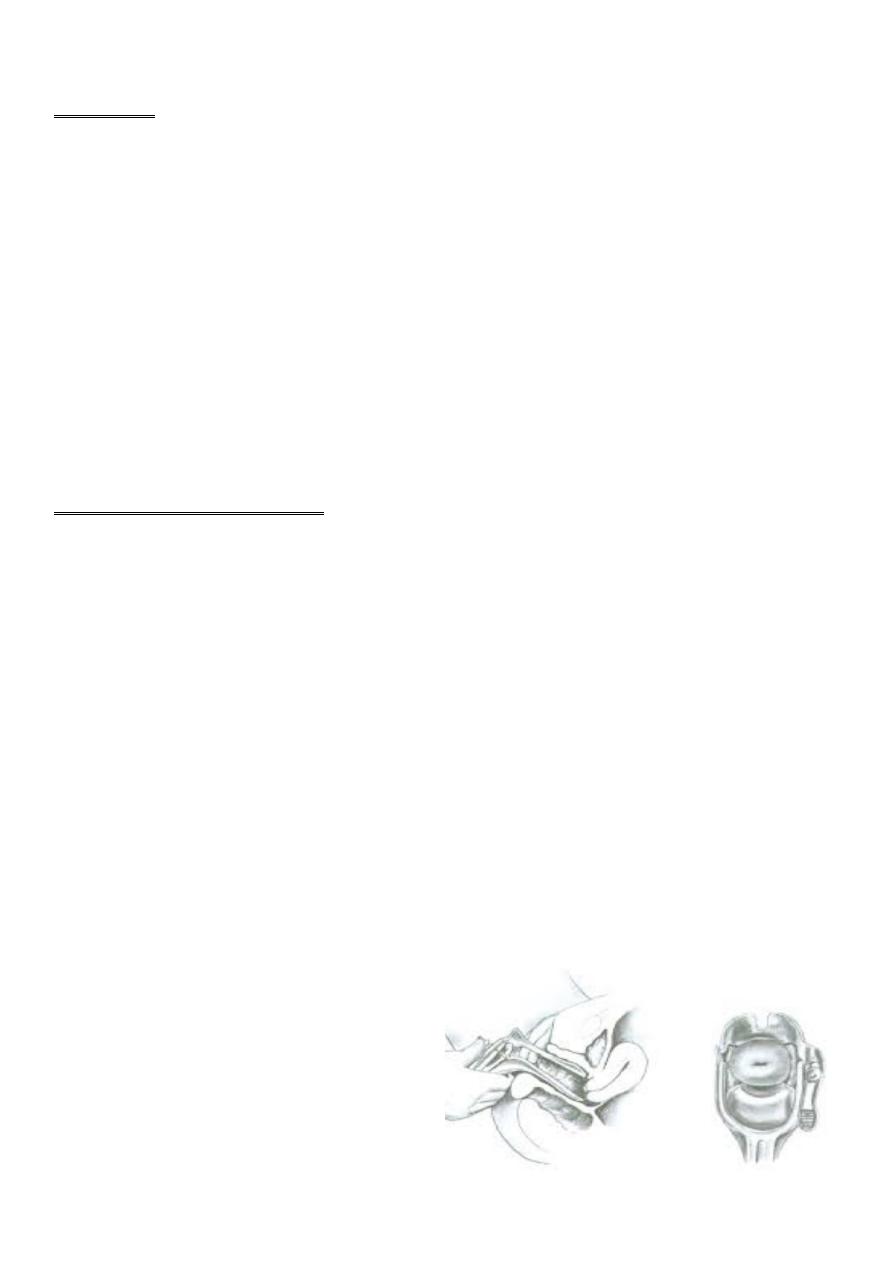
3-increase the risk of cord prolapse Fig.2 Speculum Examination
4-pulmonary hypoplasia
5-fetal or neonatal death.

3
Diagnosis
HISTORY
...calculate gestational age.
...past obstetric history (parity, previous history of PROM).
...gush of fluid vaginally with continued leakage from vagina sometimes or leaking in
dribbles, ask about duration, odor & color.
...ask about vaginal bleeding.
...ask about fever
...ask about fetal movement as it may be reduced.
Note. The watery vaginal discharge due to rupture of membrane must be distinguished
from;
*episodic urinary incontinence (so ask about frequency, urgency, incontinence & dysuria) as
UTI may present in a similar way with slight urine leakage).
*leucorrhoea (increase amount of normal vaginal discharge) is common in pregnancy, so
ask about previous vaginal discharge.
EXAMINATION
General...the woman may be flushed & her temperature & pulse rate increased if there is
infection.
Abdominal...presence of tenderness over uterus suggesting intrauterine infection.
...fundal height may be less than period of amenorrhea.
...examine for lie & presentation.
...fetal heart may showed fetal tachycardia which suggest intrauterine infection.
Vaginal (sterile speculum examination). Fig.2
...leakage of fluid from the cervix either spontaneously or after slight fundal pressure or
after cough is diagnostic
...visual inspection of cervix to estimate any cervical dilatation.
Note; it's important to avoid a digital examination unless the patient is thought to be in
established labour, because PV increases the incidence of chorioamnionitis, post-partum
endometritis, neonatal infection.

4
INVESTIGATIONS
1-haemoglobin
2-leukocytes count.
3-C-reactive protein.
4-general urine exam.
5-pelvic USG to assess gestational age, amount of liquor, fetal lie & presentation, fetal wt.,
any fetal anomalies & placental site. The presence of an average amount of amniotic fluid
by ultrasound doesn't exclude PROM.
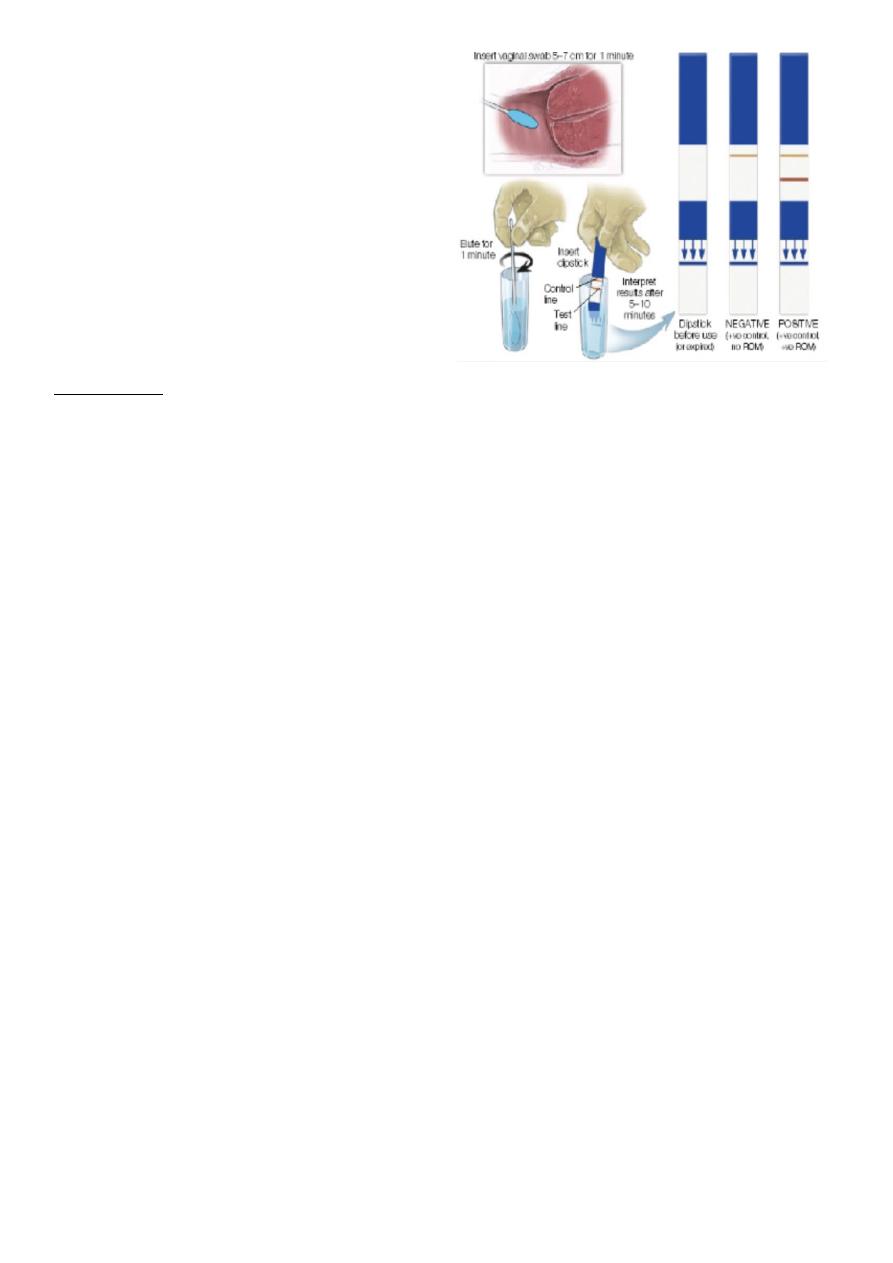
6-Nitrazine test
The normal vaginal PH is between 3.5-4.5. Amniotic fluid is more alkaline, with a PH of 7.1-
7.3. Nitrazine paper will turn blue when PH above 6, however, the presence of
contaminating substances eg. blood, semen, urine or bacterial vaginosis can give a false-
positive result.
7-Fern test
Estrogens in the amniotic fluid cause crystallization of the salts in the amnio.fluid when it
dried. Under microscope, the crystals resemble the blades of a fern.
8-amnio dye test or tampon test.
9-Amnisure test, this test uses rapid molecular testing to identify placental a-microglobulin-
1 via immunoassay, which appears to have a higher sensitivity & specificity.
10-cervical culture including Chlamydia & Neisseria. Such infections more likely to present
with PROM.
(a) (b)
5
Fig.3 Investigations for ROM (c)
(a) Nitrazine test
(b) Fern test
(c) Amnisure test
TREATMENT
The treatment varies depending on the gestational age of the fetus.
All patients with ROM should be asked to come to hospital & the treatment options are;
1-Delivery (active management)
2-Conservative (expectant management).
1-Delivery
Induction of labour by oxytocin if there is no contraindication for vaginal delivery. The
delivery indicated if patient in active labour, or with chorioamnionitis, fetal distress &
placental abruption.
2-Consevative (expectant management) includes;
A-hospitalization.
B-discussion of the risk & benefits of this management with patient & her family.
C-bed rest
D-no pelvic examination unless indicated & using sterile gloves.
E-abdominal examination to detect any abnormal lie or presentation.
F-evaluation of maternal & fetal status daily.
G-continued clinical observation of mother for signs of chorioamnionitis 12 hourly apart
including; pulse, temperature, tender uterus, changes in color or odor of liquor.
H-continued clinical observation of fetus by using CTG for fetal tachycardia & fetal
movement.
6
I-serial investigations (WBC count, C-reactive protein, vaginal cultures & HSG).
J-prophylactic antibiotics. Erythromycin (250mg orally 6 hr.ly) for 10 days.
K-corticosteroids to enhance lung maturation.
L-tocolysis in case of PPROM is not recommended.
M- If the conditions remain stable, the immature fetus has a benefit of expectant
management even if for a short time to allow administration of steroid & antibiotics. We
should stop expectant & shift to delivery if there is evidence of chorioamnionitis, maturity,
and spontaneous onset of labour.
N-neonatologist should be informed.
Treatment according to gestational age
A-Term PROM
The risk of infection increases with the duration of ROM.
Induction of labour with oxytocin is usually recommended as it decrease risk of infection &
shorten hospital stay.
If expectant management was chosen as they are waiting for spontaneous labour to begin,
it should not last more than 24hr, if labour not begins, induction of labour should be done.
B-Preterm PROM (PPROM)
The management is a balance between the risks of prematurity if delivery occurs vs. the risk
of maternal & fetal infection; before 34 wk....conservative management if there is no
indication to immediate delivery.
PPROM between 34-37wk....induction of labour is of benefit than conservative
management.
Prognosis
Prognosis depends on gestational age at delivery. The prognosis is good after 32 wk
gestation.
Chorioamnionitis
Is an inflammation of the fetal membranes (amnion & chorion ) due to bacterial infection.
It can be diagnosed by one or more of the following;

7
1-maternal pyrexia > 38C°
2-maternal tachycardia >100 beats/min.
3-uterine tenderness
4-offensive vaginal discharge.
5-fetal tachycardia >160 beats/min.
6-raise C-reactive protein.
7-raise in maternal WBC count.
When chorioamnionitis clinically suspected, delivery is recommended as antibiotic is not
curative.
Delivery by induction of labour, avoid CS as much as you can because of risk of maternal
infection, with IV broad spectrum antibiotic.
Complications of Chorioamnionitis
A-maternal
1-septicemia
2-infection in the pelvic region & abdomen.
3-endometritis (an infection of the endometrium).
B-newborn infant
1-sepsis
2-meningitis
3-respiratory problems.
