Cesarean Section
Dr. Bara'a Lukman MohammedDefinition
Cesarean Section is the delivery of a fetus from the uterus by abdominal and uterine incisions, after 28 weeks of pregnancy.It is called hysterotomy, if it is done
before 28 weeks of pregnancy.
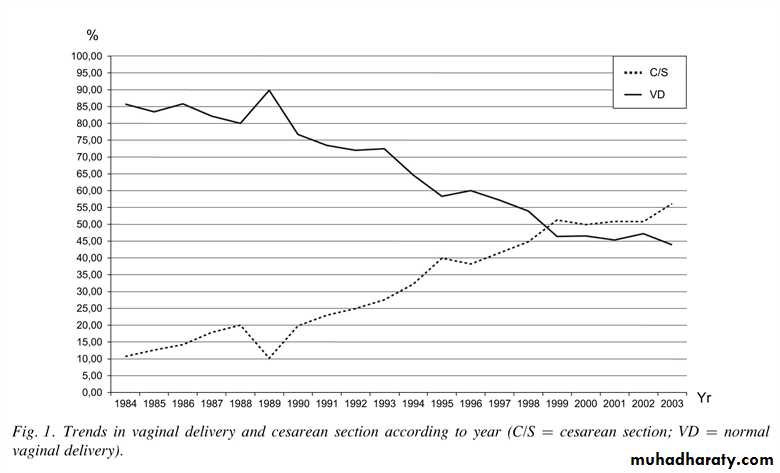
The cesarean rates during the past decade, both in the United States and worldwide, have increased dramatically.
The percentage of women in the United States delivering by cesarean increased from <5.0% in 1965 to 30.2% in 2005 and has increased 40% since 1996.
Although perinatal outcome in the United States improved during the time when the cesarean rate increased, it also improved in other countries where cesarean rates remained low. Notably, the incidence of cerebral palsy has not declined during the past 20 years, primarily because perinatal morbidity and mortality more often are a function of antepartum events, abnormal fetal growth, congenital anomalies, and premature birth.
Significance:
• Cesarean section is safe, but it’s not as safe as a planned vaginal delivery.
• In the U.S. there is a fourfold risk of death compared to vaginal birth.
• In England, emergency cesarean birth has a ninefold risk of death when compared to vaginal and elective cesareans have a threefold risk.
• Women are twice as likely to be rehospitalized within 60 days of birth when compared with women who have a vaginal birth.
Avoiding First C-Section Should Be Priority
Avoiding primary cesarean sections unless there is a medical necessityDoctors, midwives, and childbirth educators must give full and honest advice based on the available information; they may persuade but never coerce. Active participation by patients should be encouraged to arrive at a safe and logical informed decision about method of delivery, with carers recommending what they perceive to be the best course of action in keeping with the available evidence
Complications
Cesarean delivery is not an innocuous procedure. A variety of postpartum complications, including unexplained fever, endometritis, wound infection, hemorrhage, aspiration, atelectasis, urinary tract infection, thrombophlebitis, and pulmonary embolism, can occur in up to 25% of patients.The frequency of maternal death related to cesarean delivery varies with the institution and with the condition necessitating the procedure. Maternal mortality rates are now <1 in 1,000 operations, and many deaths are related to the underlying maternal illness or anesthetic complications.
Late maternal complications of cesarean delivery include:
intestinal obstruction from adhesionsdehiscence of the uterine incision in subsequent pregnancies. Both of these complications are more common with the classic incision than with a lower uterine segment incision.
The incidence of placenta previa and abnormal myometrial invasion by the placenta (accreta/increta/percreta) also is increased with each successive cesarean and can cause severe and intractable hemorrhage.
Impact on Neonates
Breastfeeding, bonding & attachment issues
Respiratory effects
Fetal injuriesTiming Of CS
Cesarean section may be performed as an elective procedure (planned in advance) or as a non-elective one (the urgency of the procedure being performed determined by the nature of the indication).Elective cesarean delivery
elective caesarean section may be justified, but decisions must take into account the risk to the infant associated with delivery before 39 weeks' gestation.
It is now clear that respiratory distress syndrome is indeed seen in "term" infants and is a considerable source of morbidity and mortality in this group.
Indication:
Cesarean delivery is necessary when labor is unsafe for either the mother or fetus.The four primary indications for cesarean delivery include:
dystocia,
elective repeat cesarean delivery,
fetal distress,
and abnormal fetal presentation.
INDICATIONS FOR ELECTIVE CS
Known CPD
Malpresentation (Breech, Transverse lie)
Multiple pregnancy (when first fetus is not in cephalic presentation)
Fetal macrosomia (over 5000g, GDM – 4500g)
Placenta previa
Repeat CS
Uterine surgery eg. Hysterotomy, myomectomy
Ca of the Cervix/ tumour obstructing the birth canalvesicovaginal fistula repair
HIV
Active herpes
INDICATIONS FOR EMERGRENCY CS
Severe PET/ eclampsia (especially with unfavourable cervix)Abruptio placntae
Fetal distress
Compromised fetus 2ry to DM, HT, isoimmunization
Cord prolapse
Failed induction
Failure to progress in labour
Obstructed labour
Malpresentation in labour brow, mentopost. shoulder presentations, breech
APH
Preoperative testing and preparation for CS
Pregnant women should be offered a haemoglobin assessment before CS to identify those who have anaemia. Although blood loss of more than 1000ml is infrequent after CS (it occurs in 4 to 8% of CS), it is a potentially serious complication.
Prescribe antibiotics (one dose of first-generation cephalosporin or ampicillin)
Preoperative testing and preparation for CS
Assess risk for thromboembolic disease (offer graduated stockings, hydration, early mobilisation and low molecular weight heparin)To reduce the risk of aspiration pneumonitis: Empty stomach, Pre-medication with an antacid (sodium citrate 0.3% 30 mL or magnesium trisilicate 300 mg) + Cimetidine IV 1 hr before CS
Women having CS with regional anesthesia require an indwelling urinary catheter to prevent over-distension of the bladder, because the anaesthetic block interferes with normal bladder function
Maternal Position During CS
All obstetric patients undergoing CS should be positioned with left lateral tilt to avoid aorto-caval compressionBy tilting the operating table to the left
or place a pillow or folded linen under her right lower back
Anaesthesia
1 General anaesthetic.2 Regional anaesthesia ( Epidural block. - Spinal block ).
Regional anaesthesia is regarded as considerably safer than general anaesthesia with respect to maternal mortality
Procedure overview:
The pelvis and uterus are entered.
The head of the infant is delivered & the infant’s airway is cleared.
The infant’s body is delivered.
The placenta is removed.
The uterus is closed.
The abdominal wall layers are closed.
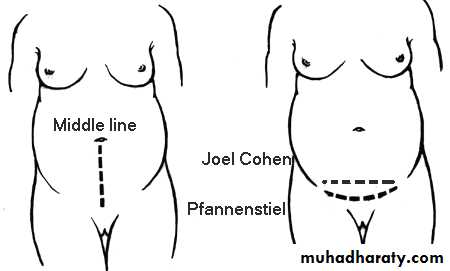
Types of abdominal wall incision:Midline vertical Suprapubic transverse
Transverse incision:Advantage:
Stronger with less likelihood of dehiscence or hernia.
Cosmetic advantage is apparent.
Disadvatage
Exposure in some women is not as optimal
TYPES OF CS:Classified according to the site of uterine incisions:
Lower segment CS Classical CSLower segment C.S.
Transverse incision in the lower uterine segment .
Advantage : reduced chance of rupture .
reduced risk of bleeding, peritonitis , paralytic ileus and bowel adhesion.
.
Upper segment (Classical C.S) :
Vertical incision in the upper uterine segment .
This incision may be made in the lower segment (low vertical incision) but It’ll invariably extend into the upper segment .
Indications for classical incision:
Transverse lie with SROMStructural abnormality that makes lower segment approach difficult
Constriction ring with neglected labour
Fibroids in the lower segment
Ant. PP & abnormally vascular lower segment
Mother dead & rapid delivery is required
Very preterm fetus in breech presentation
Uterine Incisions
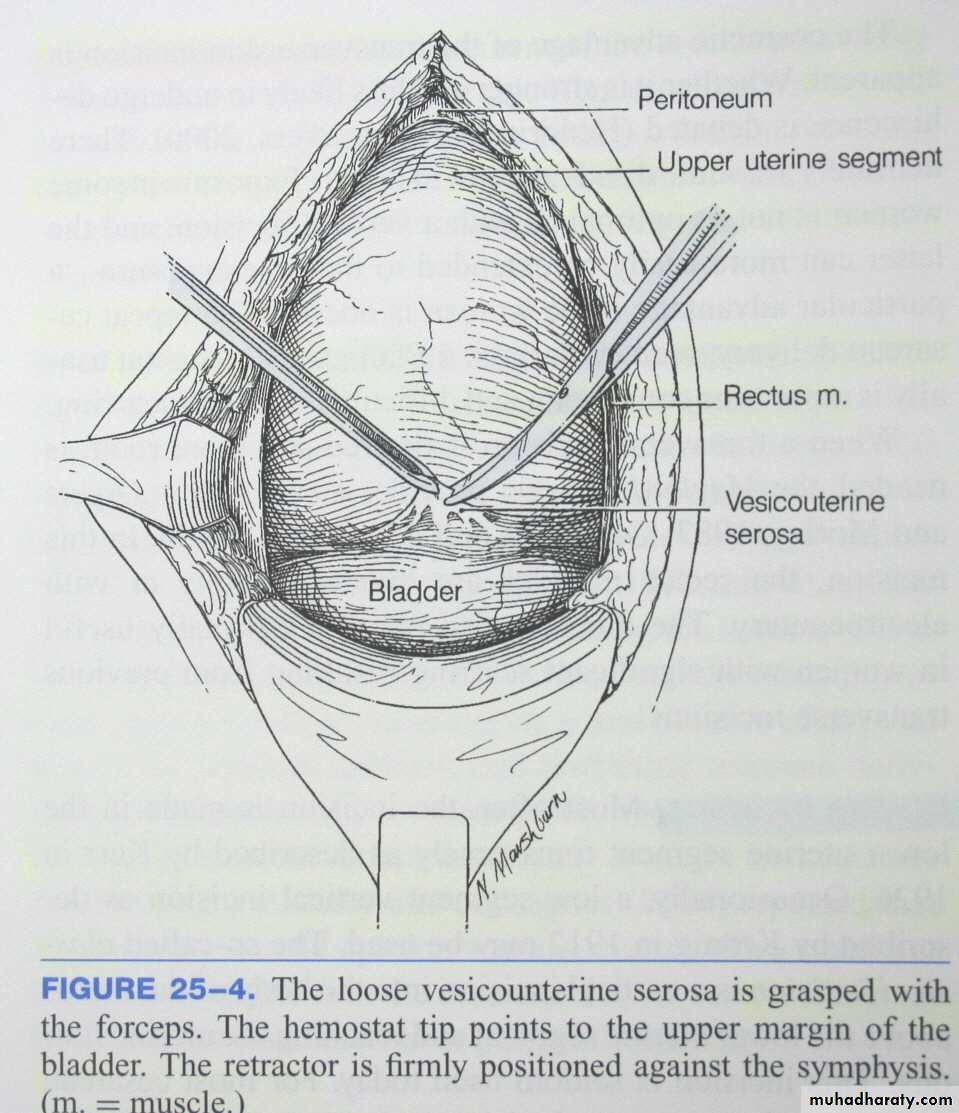
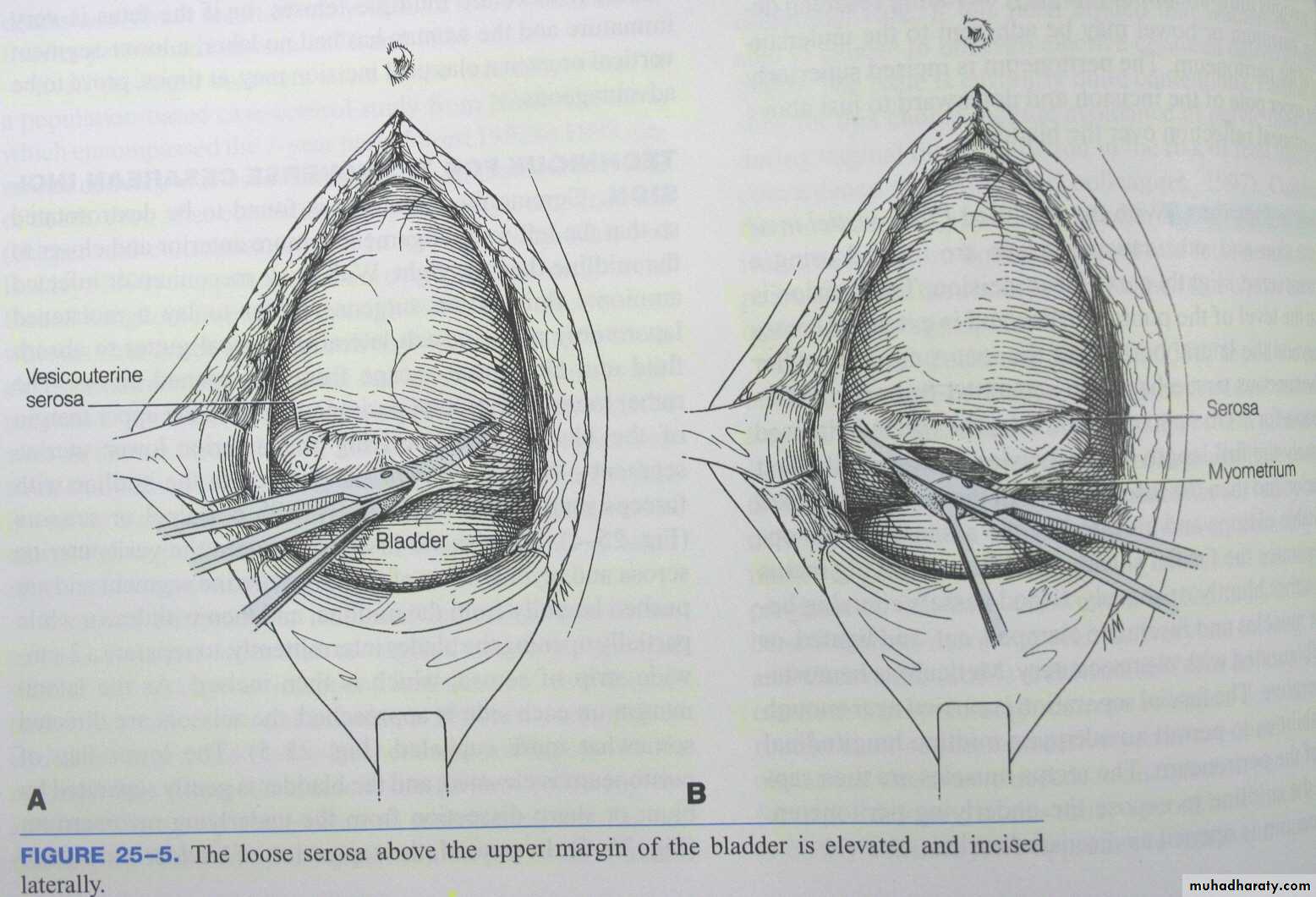
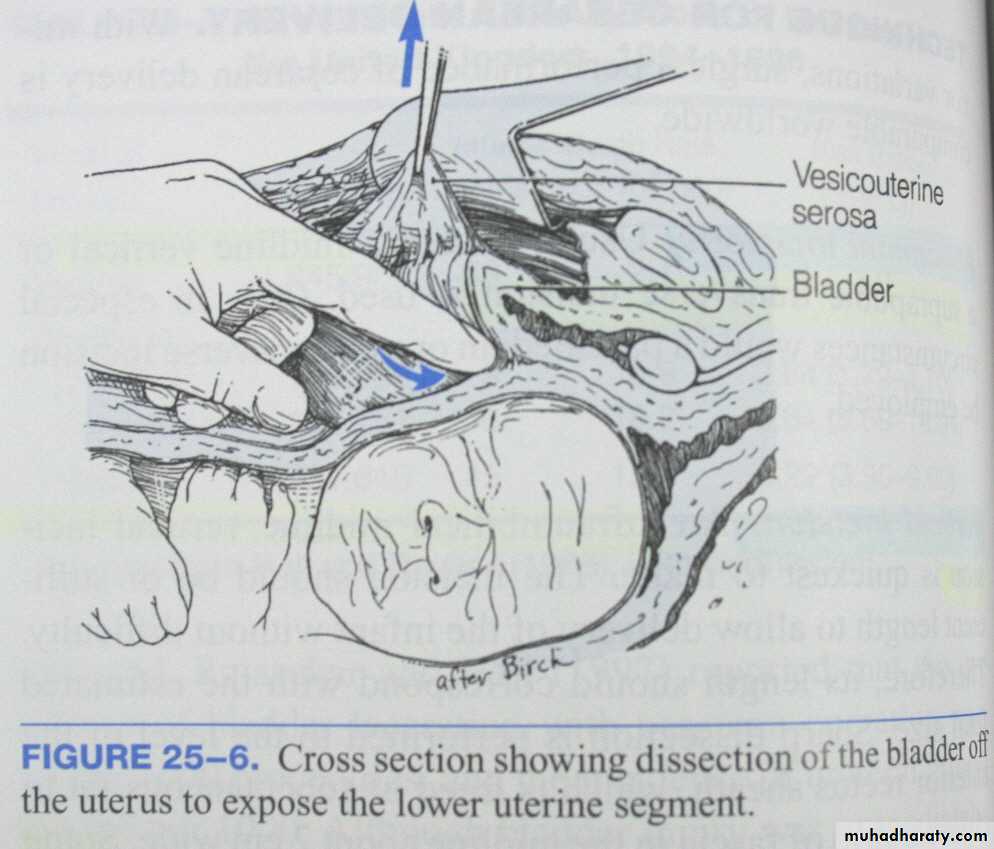
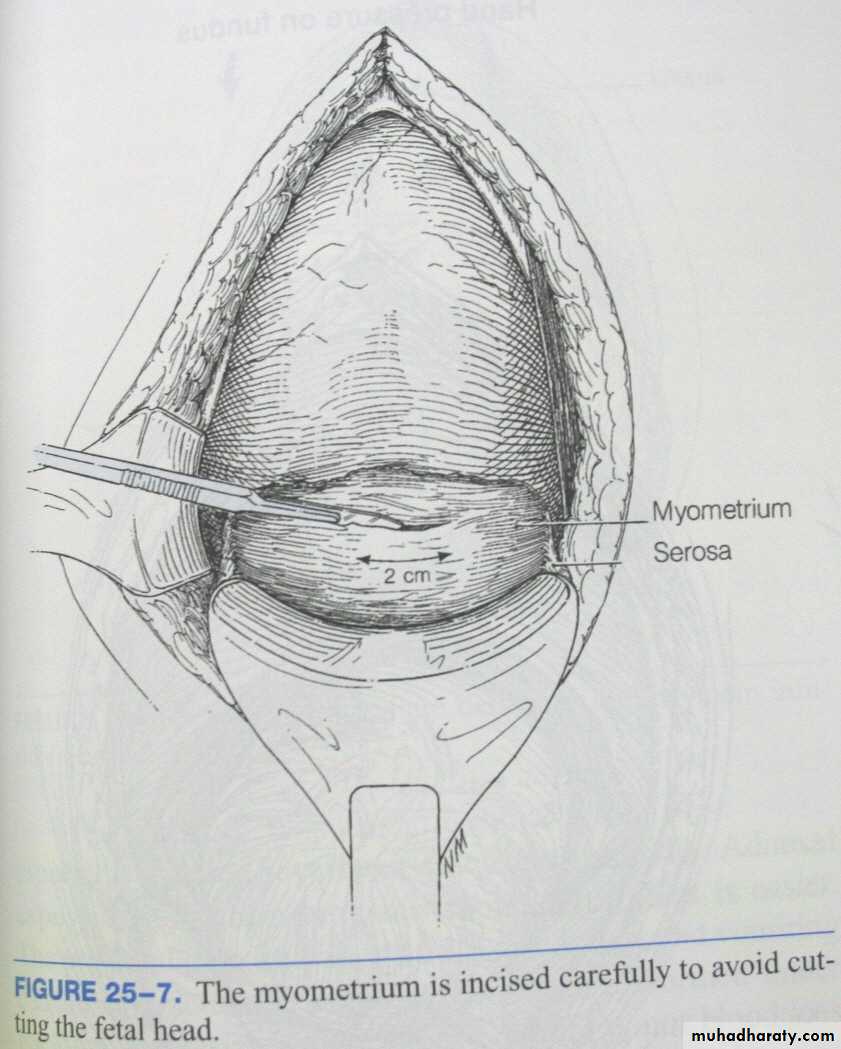
The uterus is opened through the lower uterine segment about 1 cm below the upper margin of the peritoneal reflection
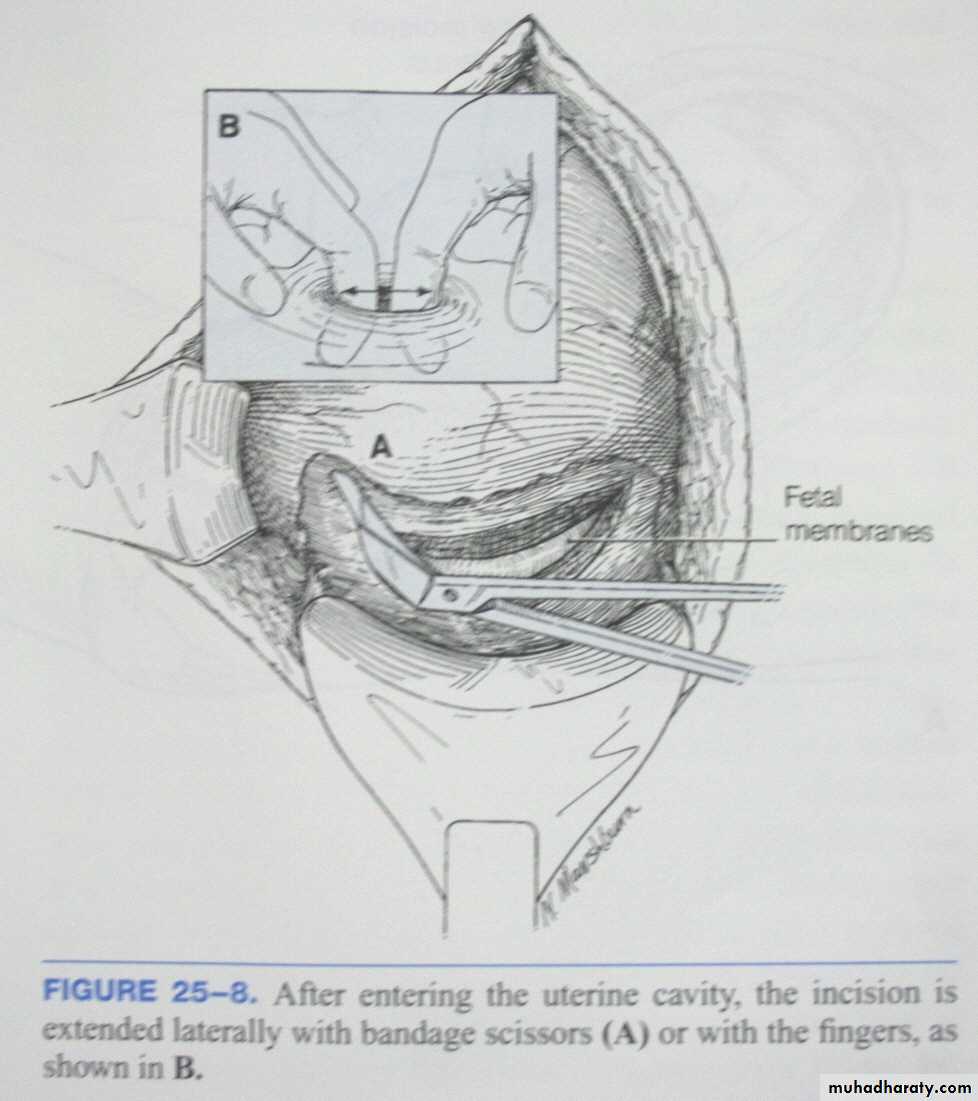
Uterine incision large enough to allow delivery of the head and trunk of the fetus without either tearing into or having to cut into the uterine arteries and veins that course through the lateral margins of the uterus
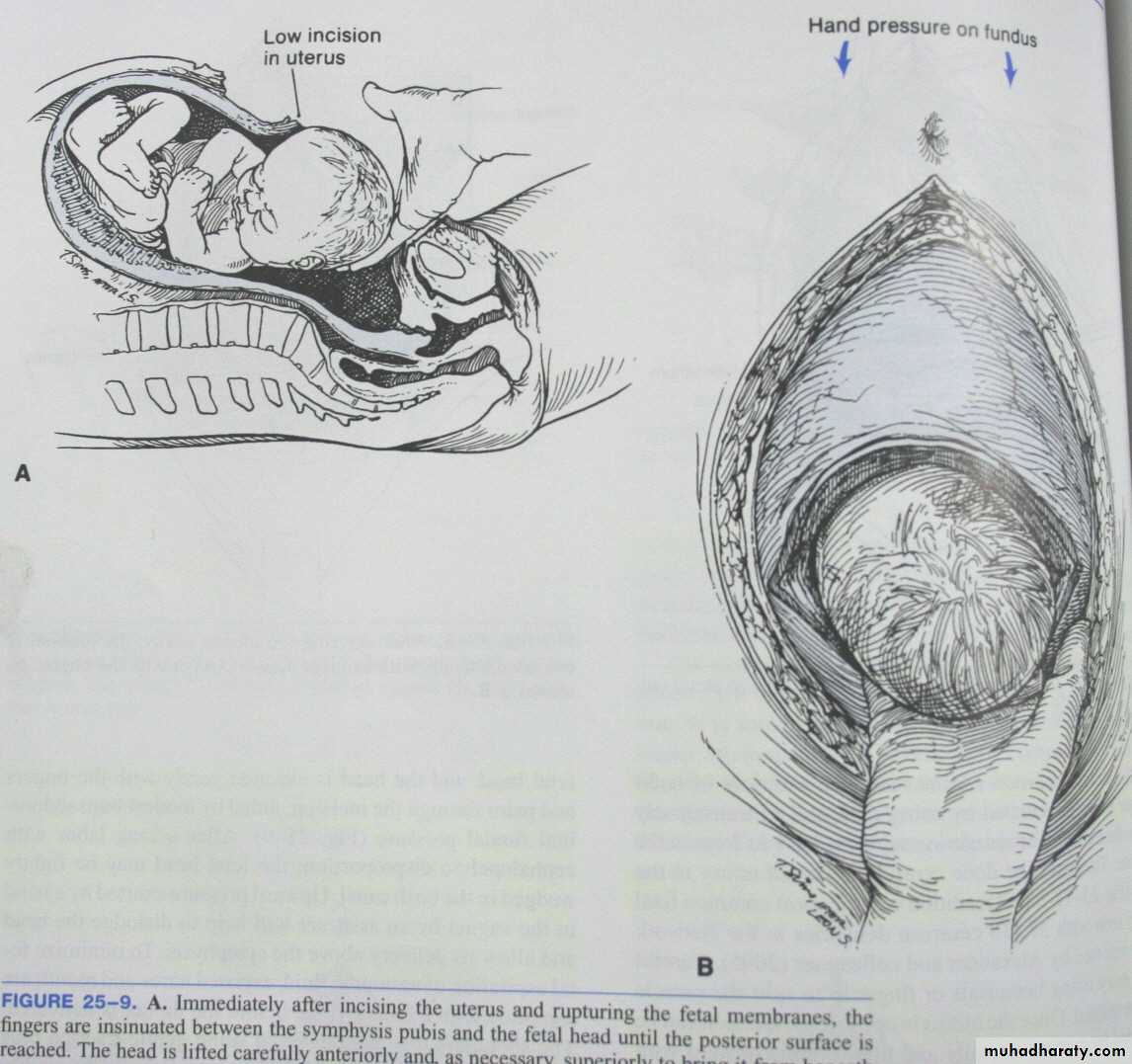
Hand is slipped into the uterine cavity between the symphysis and fetal head
Head is elevated gently with the fingers and palm through the incisionAided by modest transabdominal fundal pressure
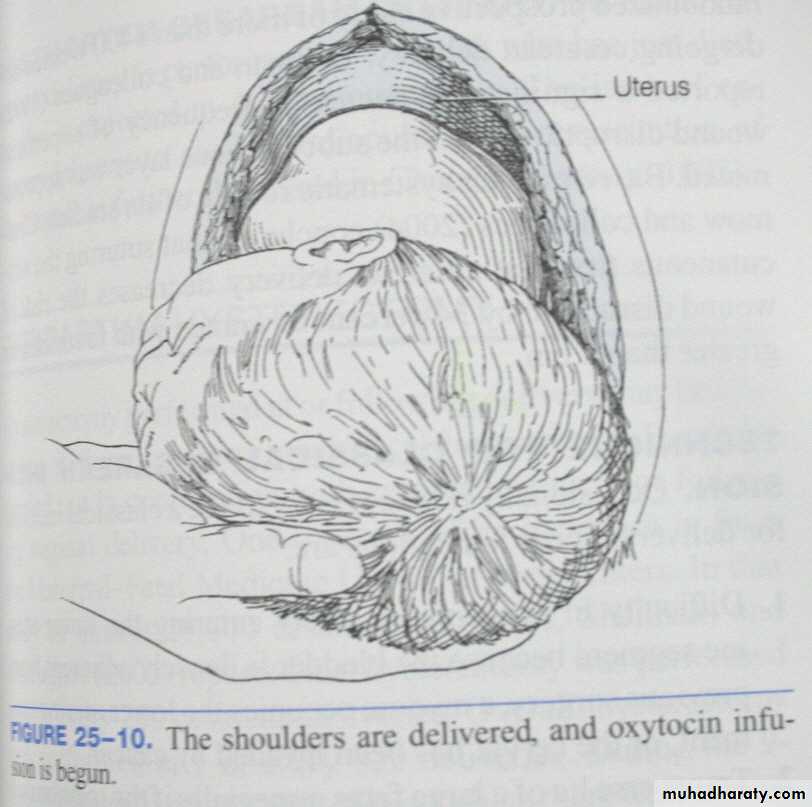
The shoulders then are delivered using gentle traction plus fundal pressure
And oxytocin infusion (10-20IU/L at 10ml/min) Until the uterus contracts satisfactorilyDelivery of the placenta:
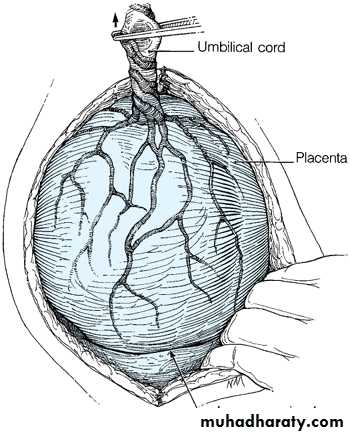
At CS, the placenta should be removed using controlled cord traction and not manual removal as this reduces the risk of endometritis.Spontaneous delivery of the placenta may reduce blood loss and decrease the chance of postoperative endometritis
By Keeping gentle traction on the cord and massage (rub) the uterus through the abdomen.
Deliver the placenta and membranes
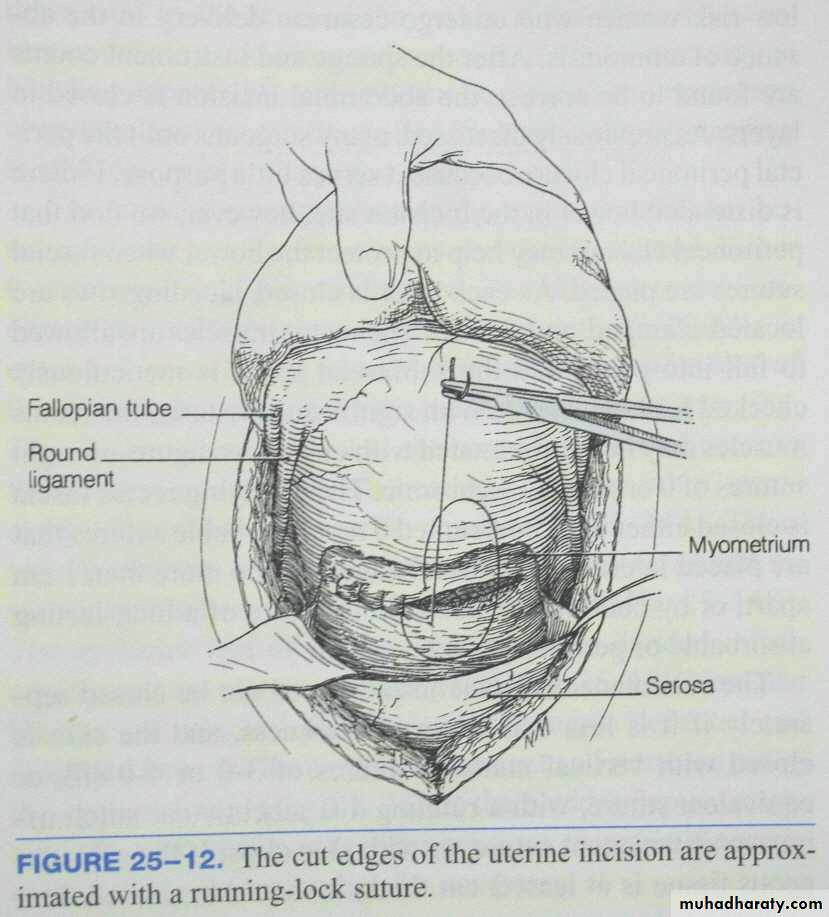
The upper and lower cut edges and each angle of the uterine incision are examined carefully for bleeding vessels
The uterine incision is closed with one or two layers of continuous absorbable suture.
Immediate post-operative care
After surgery is completed, the woman will be monitored in a recovery areato ensure that the uterus remains contracted, that there is no excessive vaginal bleeding or bleeding at the incision site, that there is adequate urine output, and to monitor routine vital signs (pulse, blood pressure, temperature, breathing). Pain medication is also given, initially through the IV line, and later with oral medications.
When the effects of anesthesia have worn off, about four to eight hours after surgery, the woman is transferred to a postpartum room
POSTNATAL CARE
Vital signs & blood loss must be moniteredUterine fundus palpated
Effective parentral analgesics
Deep breathing & coughing encouraged
Early mobilization
Fluid therapy &diet
Bladder & bowel function
Wound care
Breast care
Prophylaxis for thromboembolism
Review for consent of patient.
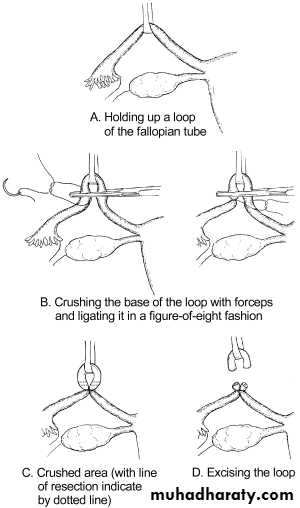
Grasp the least vascular, middle portion of the fallopian tube with a Babcock or Allis forceps.Hold up a loop of tube 2.5 cm in length
Crush the base of the loop with artery forceps and ligate it with 0 plain catgut suture .
Excise the loop (a segment 1 cm in length) through the crushed area.
Repeat the procedure on the other side
Cesarean Hysterectomy
Hysterectomy is carried out after caesarean section in the same sitting for one of the following reasons:Uncontrollable postpartum haemorrhage.
Unrepairable rupture uterus.
Operable cancer cervix.
Couvelaire uterus.
Placenta accreta cannot be separated.
Severe uterine infection particularly that caused by Cl. welchii.
Multiple uterine myomas in a woman not desiring future pregnancy although it is preferred to do it 3 months later.