1
Forth stage
Obstetric
Lec-12
.د
ولدان
1/1/2016
Diabetes mellitus in pregnancy
Definition
Gestational Diabetes (GDM) is defined, as glucose intolerance of variable degree with onset
or first recognition during the present pregnancy.
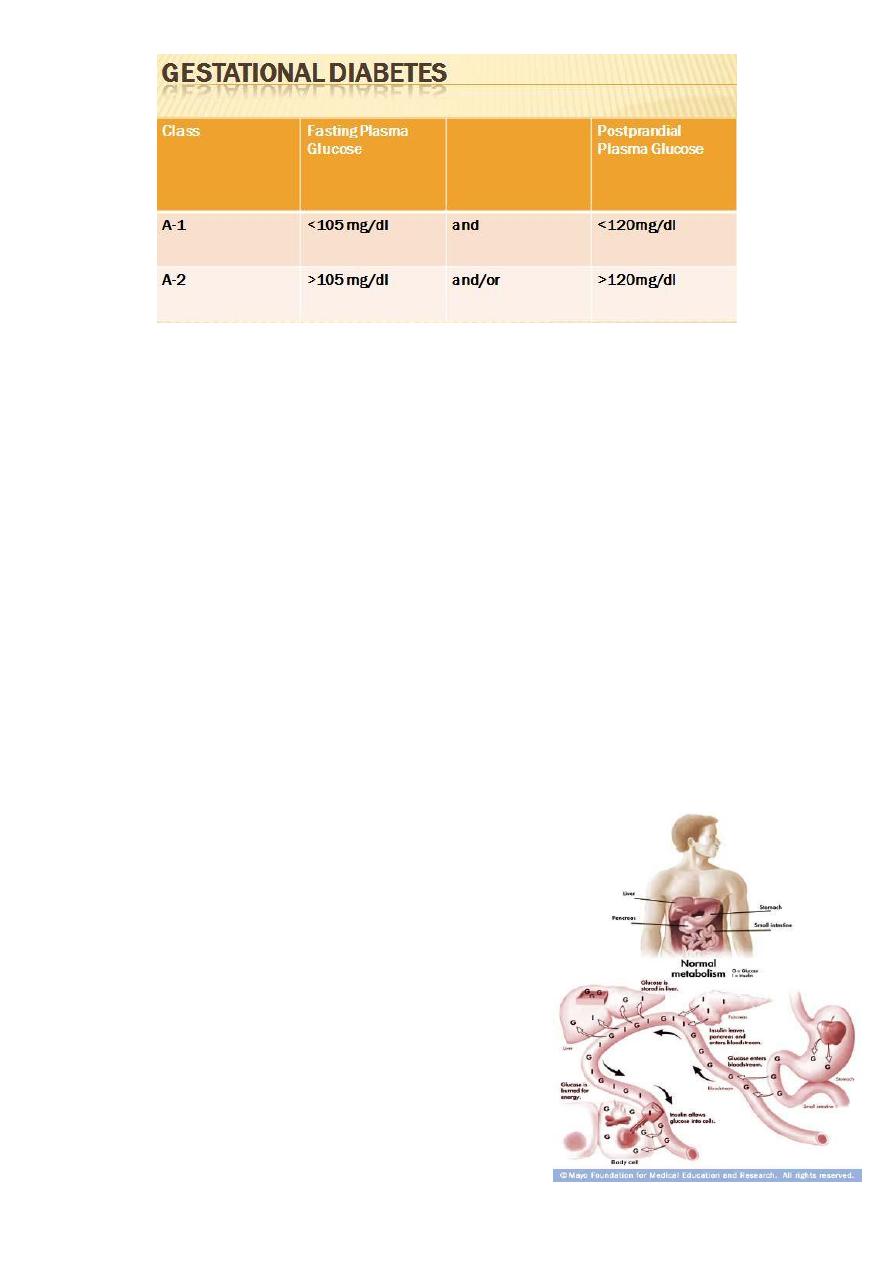
Gestational Diabetes (GDM)
-Definition: Insulin resistance/ glucose intolerance first diagnosed during pregnancy.
-Prevalence: 1-14% of all pregnancies.
-indicates predisposition to later development of Type 2 Diabetes.
-Chance of recurrence in future pregnancies: 30-84%.
-Within 10-20 years after delivery, approximately 50% of women who had gestational
diabetes will develop type 2 diabetes
-Varies by ethnicity – in the Hispanic population, up to 50% develop type 2 diabetes within
5 years of diagnosis of gestational diabetes
-Prevalence is wide-ranging and variable depending on ethnic makeup of the population.
-Also, patients’ first presentation may be during pregnancy
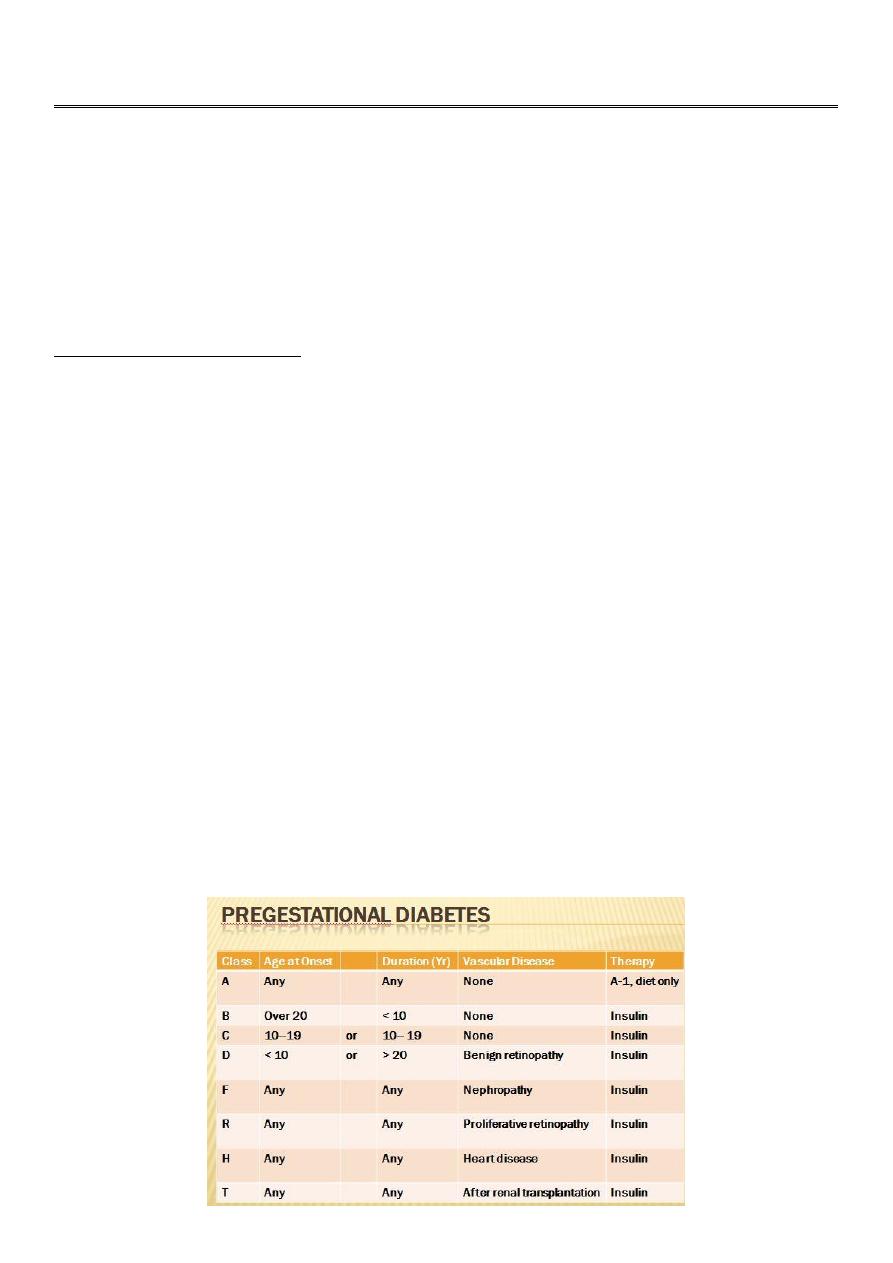
Classification
White classification (1965) is approved by The American College of Obstetricians and
Gynaecologists (1986) as follow:
2
-Gestational diabetes is appearance of diabetes for the first time during pregnancy and
disappear.
-In the original white classification, class A diabetes is asymptomatic diabetes with
abnormal glucose tolerance test i.e. chemical diabetes.
Phases of Diabetes Mellitus
1. Potential diabetes: There is high risk of developing diabetes e.g. if one or both
parents is diabetic.
2. Prediabetes: The period preceding the development of diabetes. It is a retrospective
diagnosis.
3. Latent diabetes: Diabetes appears only under stress conditions as pregnancy
(gestational diabetes) or with cortisone administration.
4. Chemical diabetes: An abnormal glucose tolerance test without symptoms.
5. Clinical diabetes: An abnormal glucose tolerance test with symptoms of diabetes.
Carbohydrate metabolism during pregnancy:
Pregnancy is a diabetogenic state manifested by insulin
resistance and hyperinsulinemia. This is because of the
placental secretion of diabetogenic hormones including
growth hormone, corticotropin-releasing hormone,
placental lactogen, and progesterone.
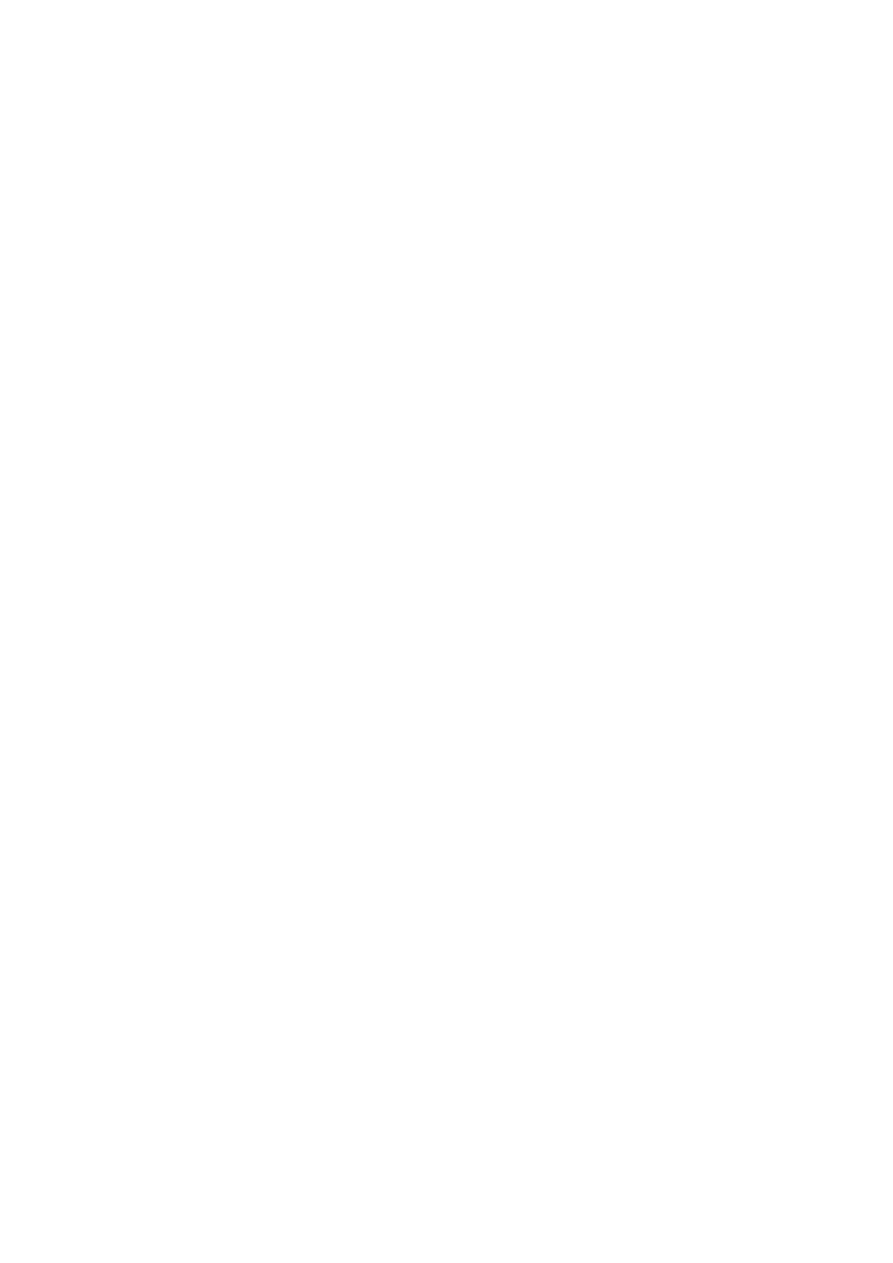
Normal glucose metabolism
Glucose enters bloodstream from food source.
Insulin aids in storage of glucose as fuel for cells.
3
Insulin resistance is defined as insensitivity of cells to insulin, therefore resulting in
increased levels of insulin and glucose in the bloodstream.
Let’s talk about the changes in metabolism that occur during pregnancy, specifically
carbohydrate metabolism. First of all, normal glucose metabolism is depicted here.
Glucose is absorbed from the stomach and small intestine and enters the bloodstream,
then is transported to various organs. Insulin, secreted by the pancreas is required to
permit entry of the glucose into the cell to be used.
Effect of Pregnancy on Diabetes
Pregnancy is diabetogenic due to increased production of insulin antagonists as
human placental lactogen, placental insulinase, cortisol, oestrogens and
progesterone.
Insulin requirements: increases during pregnancy due to increased production of
insulin antagonists while it decreases postpartum.
Reliance on urine for control of diabetes may lead to insulin overdosage due to
lowered renal threshold for glucose.
Effect of Diabetes on Pregnancy
A-Maternal:
1. Pregnancy induced hypertension (30%).
2. Infections: as monilial vulvo-vaginitis, urinary tract infections, puerperal sepsis and
breast infection.
3. Obstructed labour due to large sized baby.
4. Deficient lactation: is more common.
B-Foetal:
1. Abortions.
2. Polyhydramnios (30%): due to large placenta and foetal size.
3. Congenital anomalies (6%): This is about 4 times the normal incidence (1.5%). Sacral
dysgenesis is a specific anomaly related to diabetes.
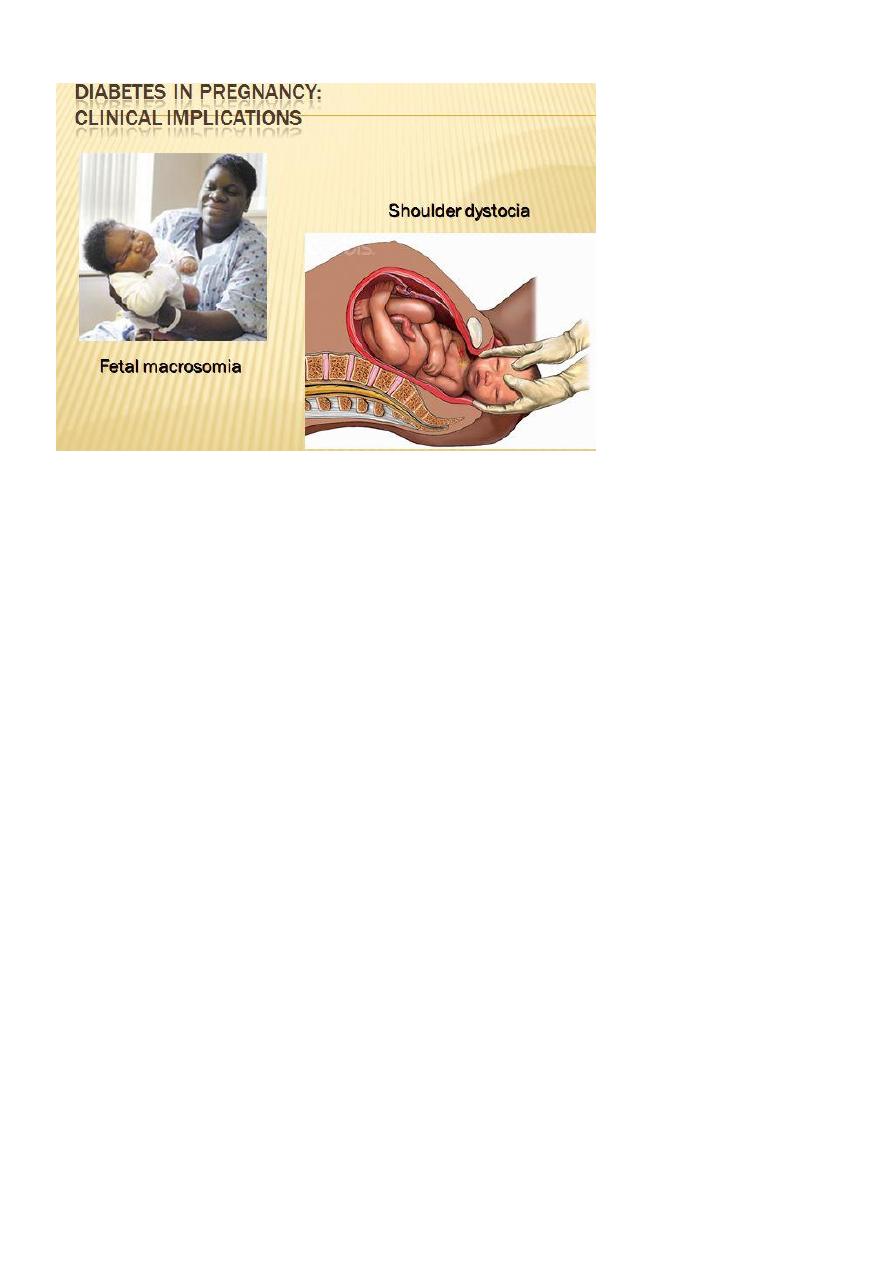
4. Macrosomia: i.e. foetal weight > 4 kg at term may cause obstructed or traumatic
delivery.
5. Preterm labour: with its complications mainly due to polyhydramnios.
4
Diabetes in pregnancy : Clinical implications
Intrauterine foetal death (5%): especially in the last 4 weeks due to;
ketosis,
hypoglycaemia,
pre-eclampsia,
congenital anomalies,
placental insufficiency.
Neonatal mortality and morbidity (5%): due to ;
hypoglycaemia,
respiratory distress syndrome,
congenital anomalies,
birth trauma,
hyperbilirubinaemia due to immaturity of the foetal liver,
hyperviscosity,
hypocalcaemia and hypomagnesaemia which may result from decreased parathyroid
hormone.
Methods of Screening
- Selective screening – it is not cost-effective to screen women who are less than 25 years of
age, have a normal body weight, no family history of diabetes, and are not at risk on the
basis of race or ethnicity.
- Screening based solely on risk factors will only identify approximately 50% of women with
GDM.
5
-Initially a 50-g oral glucose challenge is given and venous serum or plasma glucose is
measured one hour later; a value > or =140 mg/d L (7.8 m mol/L) is considered abnormal,
and is associated with a 25 to 30 percent risk of a macrosomic infant if no treatment is
offered.
-Such test can be performed at any time of the day and with disregard to previous meal
ingestion. Women with an abnormal value are then given a 75-g, two-hour oral glucose
tolerance test (GTT). The test is performed in the fasting state.
-SCREENING TECHNIQUE AND DIAGNOSTIC CRITERIA – Screening is optimally performed at
24 to 28 weeks of gestation. However, it can be done as early as the first prenatal visit if
there is a high degree of suspicion that the pregnant woman has undiagnosed type 2
diabetes.
Diagnosis
History
History of diabetes or symptoms suggesting it as loss of weight, polydepsia (thirst),
polyuria and polyphagia.
History of frequent severe pruritis (recurrent monilial infection).
History of repeated abortions, intrauterine foetal deaths or delivery of oversized
babies.
Investigations
Positive urine test: during routine antenatal care.
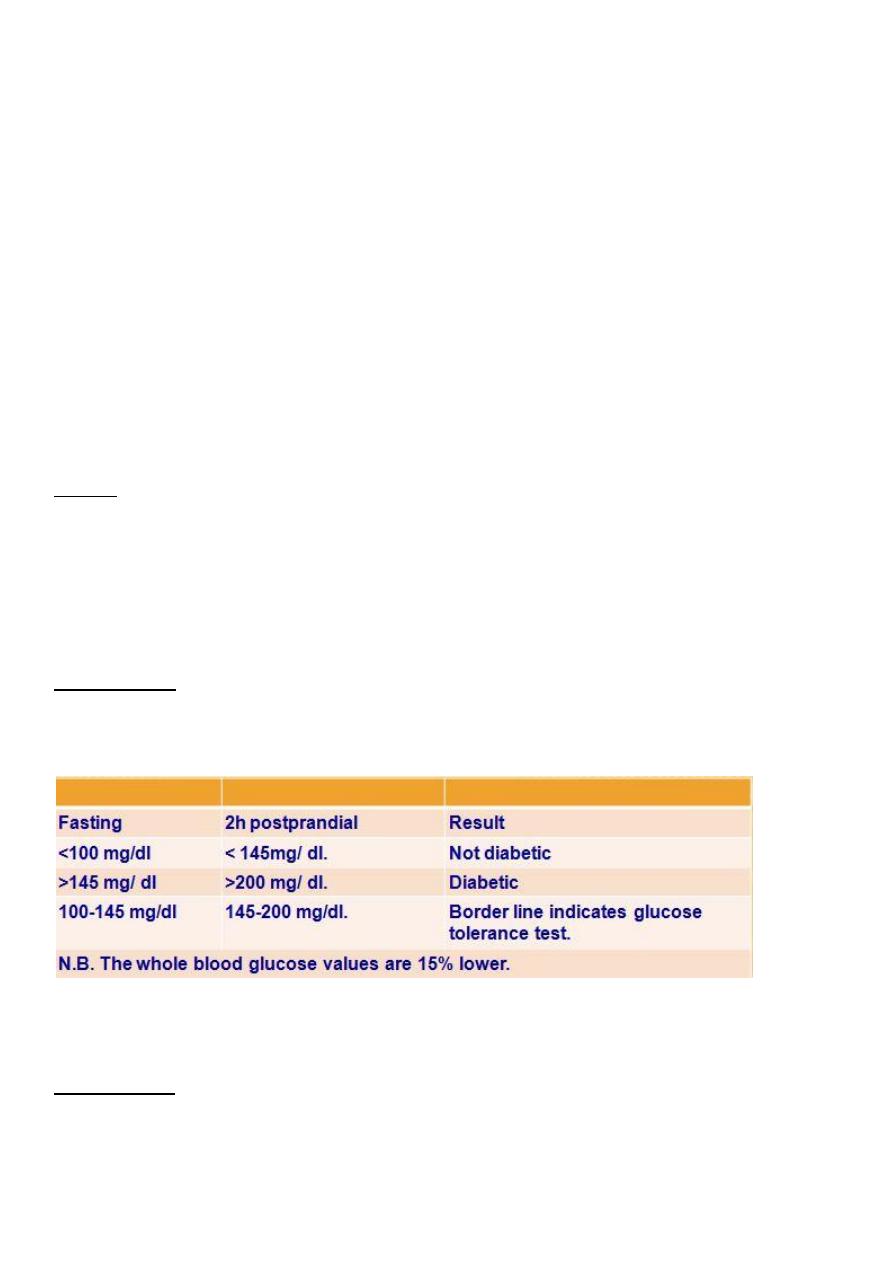
Fasting and 2 hours postprandial venous plasma sugar.
Glucose tolerance test (GTT):
Prerequisites:
Normal diet for 3 days before the test.
No diuretics 10 days before.
At least 10 hours fast.
6
Test is done in the morning at rest.
Oral glucose tolerance test:
Giving 75 gm (100 gm by other authors) glucose in 250 ml water orally.
Intravenous glucose tolerance test:
Giving 25 gm rapid IV, has little practical value due to bypassing the gut so there is no
stimulus to gut hormone production particularly glucagon.
Criteria for glucose tolerance test:
The maximum blood glucose values during pregnancy:
1. fasting 90 mg/ dl,
2. one hour 165 mg/dl,
3. 2 hours 145 mg/dl,
4. 3 hours 125 mg/dl.
If any 2 or more of these values are elevated, the patient is considered to have an
impaired glucose tolerance test.
Indications of performing glucose tolerance test:
1. Positive urine test.
2. First degree family history of diabetes.
3. Gross obesity.
4. Previous macrosomic babies.
5. Previous unexplained intrauterine or neonatal deaths.
6. Previous 2 or more unexplained abortions.
7. Current or previous congenital anomalies.
8. Current or previous polyhydramnios.
Glycosylated haemoglobin (Hb A1):
It is normally accounts for 5-6% of the total haemoglobin mass. A value over 10% indicates
poor diabetes control in the previous 4-8 weeks. If this is detected early in pregnancy, there
is a high risk of congenital anomalies and in late pregnancy it indicates increased incidence
of macrosomia and neonatal morbidity and mortality.
Differential Diagnosis of Glycosuria
1-Lactosuria: may be present during pregnancy, labour or puerperium. Lactose is
differentiated by:
Osazone test,
it does not ferment yeast, and

7
glucose oxidase test is negative.
2-Alimentary glycosuria:
Usually occurs early in pregnancy due to rapid absorption of glucose from the gut.
No symptoms of diabetes.
GTT is normal.
3-Renal glycosuria:
usually occurs in midpregnancy due to lowered renal threshold.
No symptoms of diabetes.
GTT is normal.
4-Reducing agents: as vitamin C, salicylates and morphine.
5-Diabetes mellitus.
Management
-Antenatal care
-Frequent antenatal visits: for maternal and foetal follow up.
-control of diabetes:
I.
Diet: is arranged to supply 1800 calories/ day with restriction of carbohydrates to 200
gm/ day, less fat and more proteins and vitamines.
II.
Insulin therapy:
1. Oral hypoglycaemics are contraindicated during pregnancy, labour and early
puerperium as they are not adequate for controlling diabetes, have teratogenic
effects and may result in neonatal hypoglycaemia.
2. Doses of insulin tend to increase in the first half of pregnancy, then stabilise and
finally rise in the last quarter, to be decreased again postpartum.
3. Twice daily (before breakfast and before dinner) injections of a combination of short
and intermediate acting insulins are usually sufficient to control most patients
otherwise a subcutaneous insulin pump is used.
4. Monocomponent insulins which do not provoke production of antibodies are
preferable e.g. " Actrapid" (short acting) and " Monotard" (intermediate acting).
5. The total first dose of insulin is calculated by : Starting with a low dose of 20 units
combined insulin then increase it according to the blood sugar level or according to
the patient’s weight as follow:
In the first trimester ............patient’s weight x 0.7
In the second trimester.........patient’s weight x 0.8
8
In the third trimester............patient’s weight x 0.9
6. If the total dose of insulin is less than 50 units/ day, it is given in a single morning
dose with the ratio:
Short acting (regular or Actrapid)/Intermediate (NPH or Monotard) = 0.5
In higher doses, 2/3 the dose is given in the morning with the same ratio and 1/3 the
dose is given in the evening in a ratio 1:1.
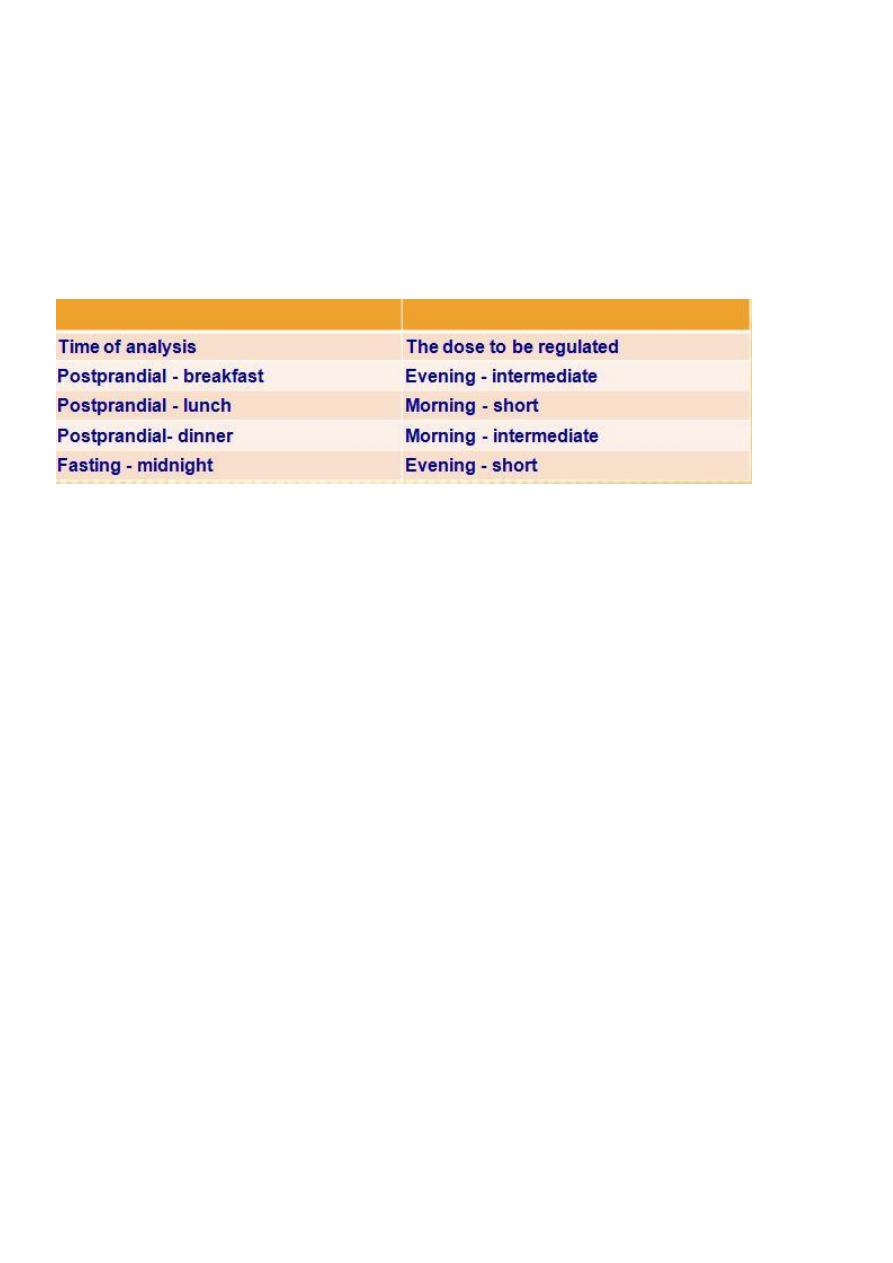
-Blood sugar analysis is carried out 4 times daily to regulate the doses as follow:
-The aim is to achieve normoglycaemic values as in GTT.
-Hospitalisation: if diabetics are not controlled as outpatients or complications develop.
-Evaluation of foetal well - being by:-
ultrasound weekly,
cardiotocography weekly,
serial oestriol estimation 3 times/ weekly,
amniocentesis before delivery for detection of phosphatidyl glycerol that indicates
lung maturity. L/S ratio is less reliable in diabetics.
- Delivery
Timing: pregnancy is terminated at 37 completed weeks to avoid intrauterine foetal
death.
Mode of delivery: vaginal delivery is induced in normal presentation, favourable
cervix, average sized baby and no foetal distress. Otherwise, caesarean section is
indicated.
-Insulin therapy:
Day prior to delivery:
1) Normal diet, normal morning insulin.
2) Reduce evening insulin by 25% or omit intermediate acting insulin.
Day of delivery:
5% glucose infusion in a rate of 125 ml/hour + short acting insulin 1-2 units/hour.
Postpartum:

9
Continue 5% glucose + insulin till oral feeding is established. When oral feeding is
allowed the pre-pregnancy dose of insulin is given.
-Neonatal care:
The neonate is managed as a premature baby as it is more liable for RDS.
5% glucose may given IV at a rate of 0.24 gm / kg/ hour to guard against possible
neonatal hypoglycaemia. Pulsed IM glucose is not preferred as they may sustain the
output of insulin from the foetal pancreas.
- Contraception:
Mechanical and chemical methods or sterilization are allowed but hormonal methods
are diabetogenic and IUDS may cause PID. Progestogen only contraception may be
used if the patient will accept the high possibility of menstrual irregularity.
