
Arrhythmias
•
Disturbance of heart rhythm and/or
conduction.
ot.com

pot.com
Arrhythmias
•
Sinus Rhythms
•
Premature Beats
•
Supraventricular Arrhythmias
•
Ventricular Arrhythmias
•
AV Junctional Blocks

spot.com
Sinus Rhythms
•
Sinus Bradycardia
•
Sinus Tachycardia
Sinus Bradycardia
•
Deviation from NSR
A sinus rate of less than 60/min

Causes of Sinus Bradycardia
•
•
MI
•
• Sinus node disease (sick sinus syndrome)
•
• Hypothermia
•
• Hypothyroidism
•
• Cholestatic jaundice
•
• Raised intracranial pressure
•
• Drugs, e.g. β-blockers, digoxin, verap
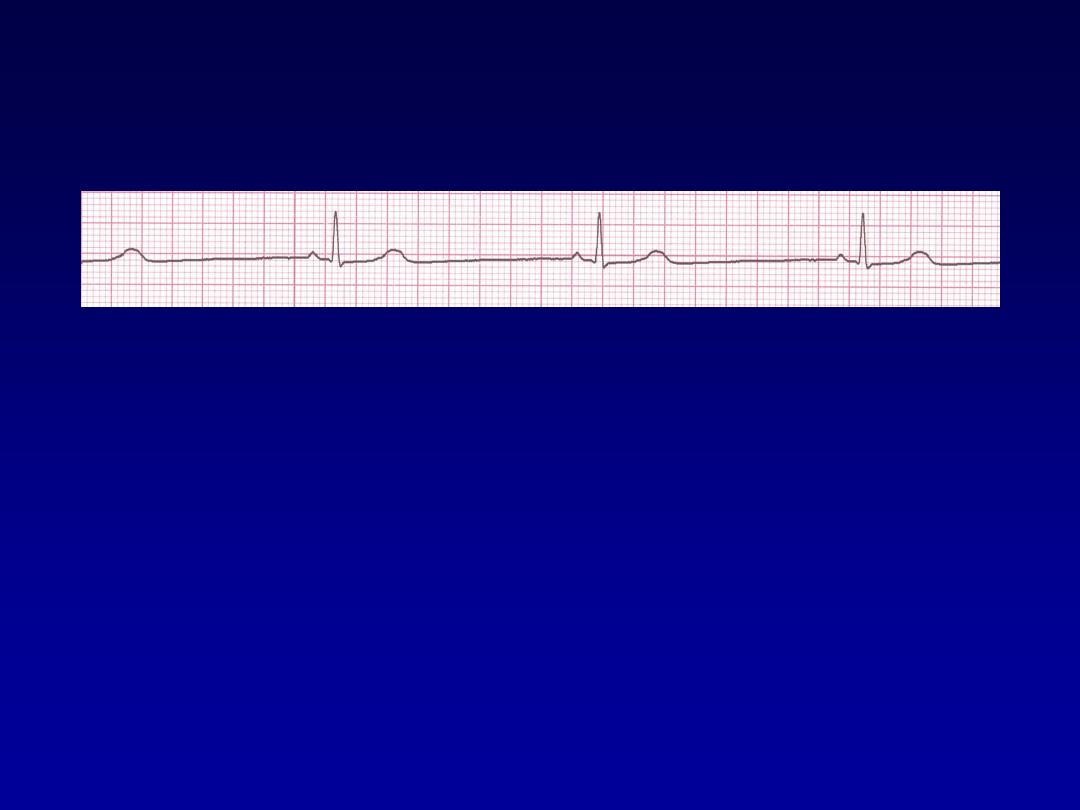
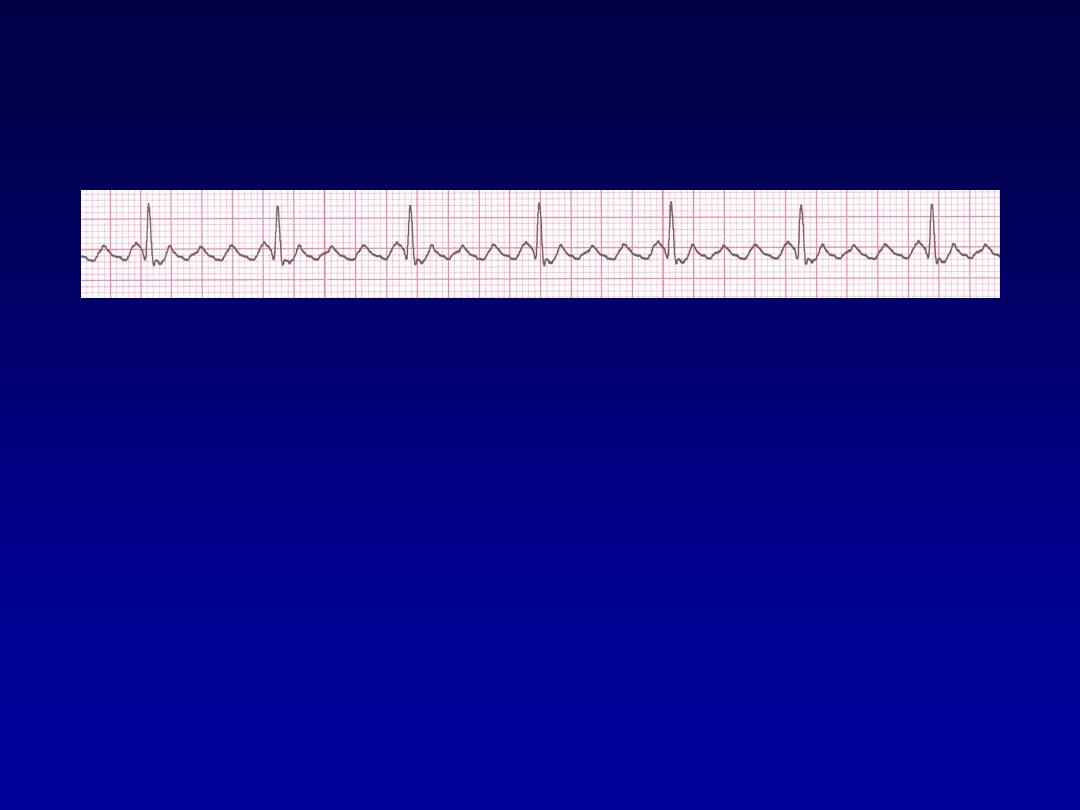
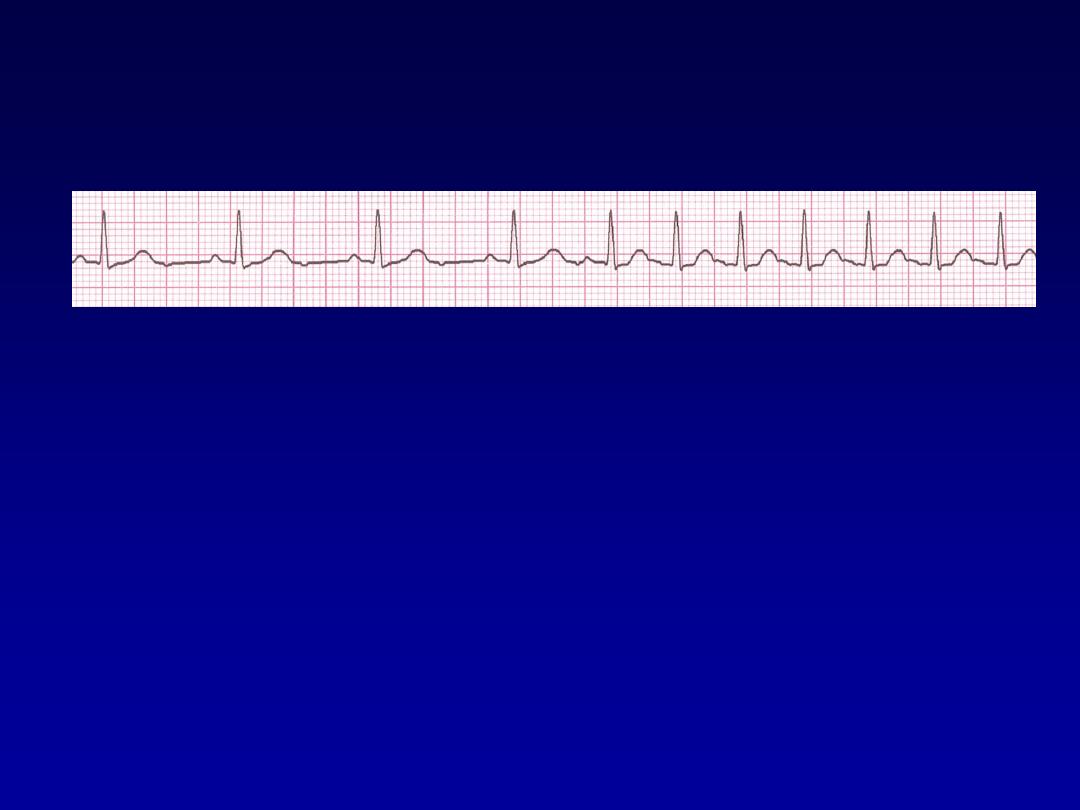
Rhythm
30 bpm
• Rate?
• Regularity?
regular
normal
0.10 s
• P waves?
• PR interval?
0.12 s
• QRS duration?
Interpretation?
Sinus Bradycardia
Sinus Tachycardia
•
Deviation from NSR
-
a sinus rate of more than 100/min

Causes of Sinus Tachycardia
•
Anxiety
•
• Fever
•
• Anaemia
•
• Heart failure
•
• Thyrotoxicosis
•
• Phaeochromocytoma
•
• Drugs, e.g. β-agonists (bronchodilators)
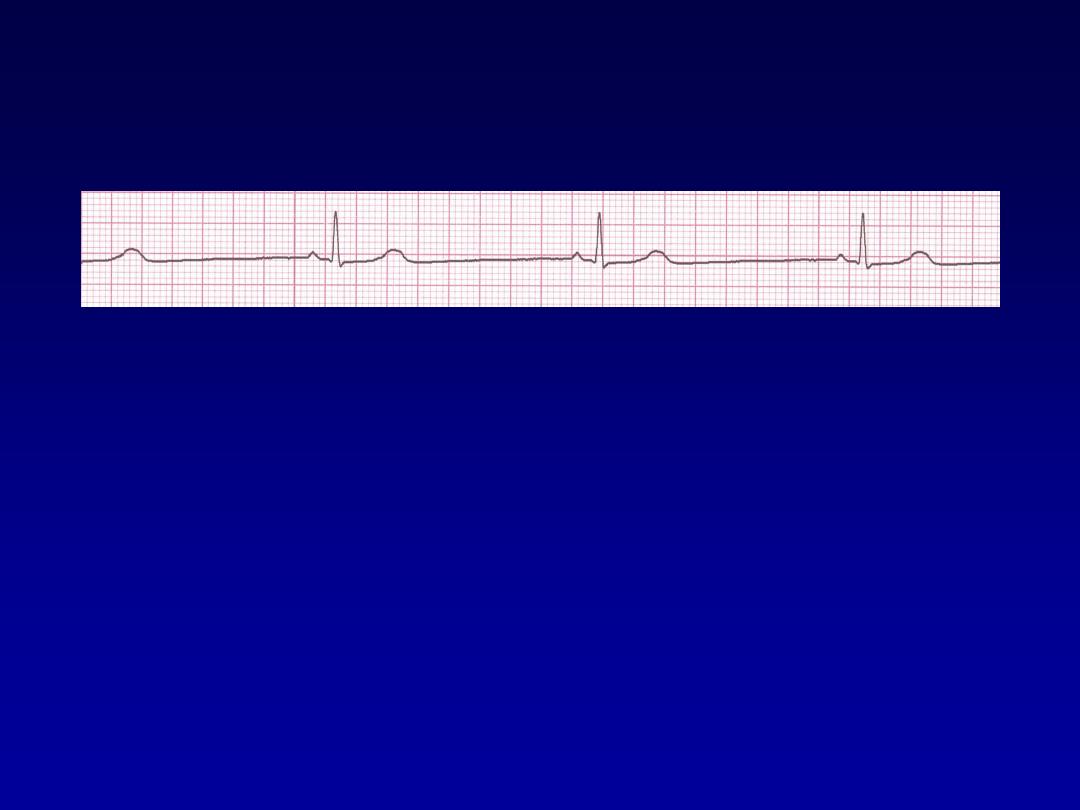
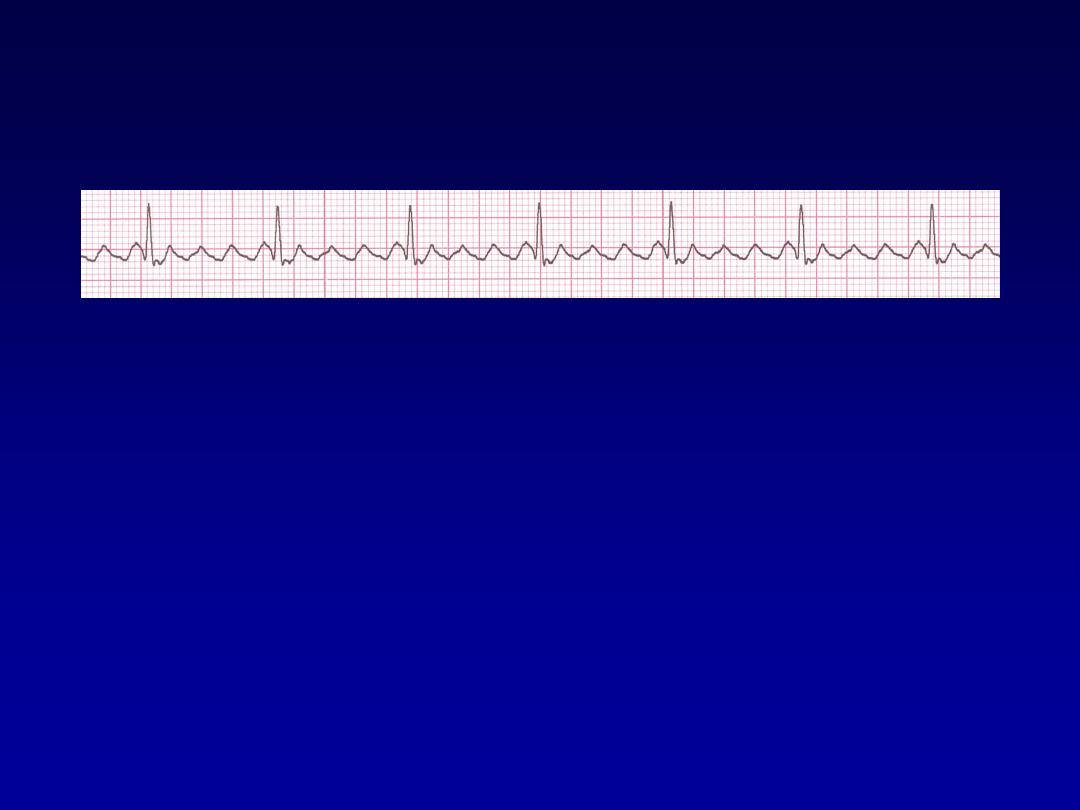
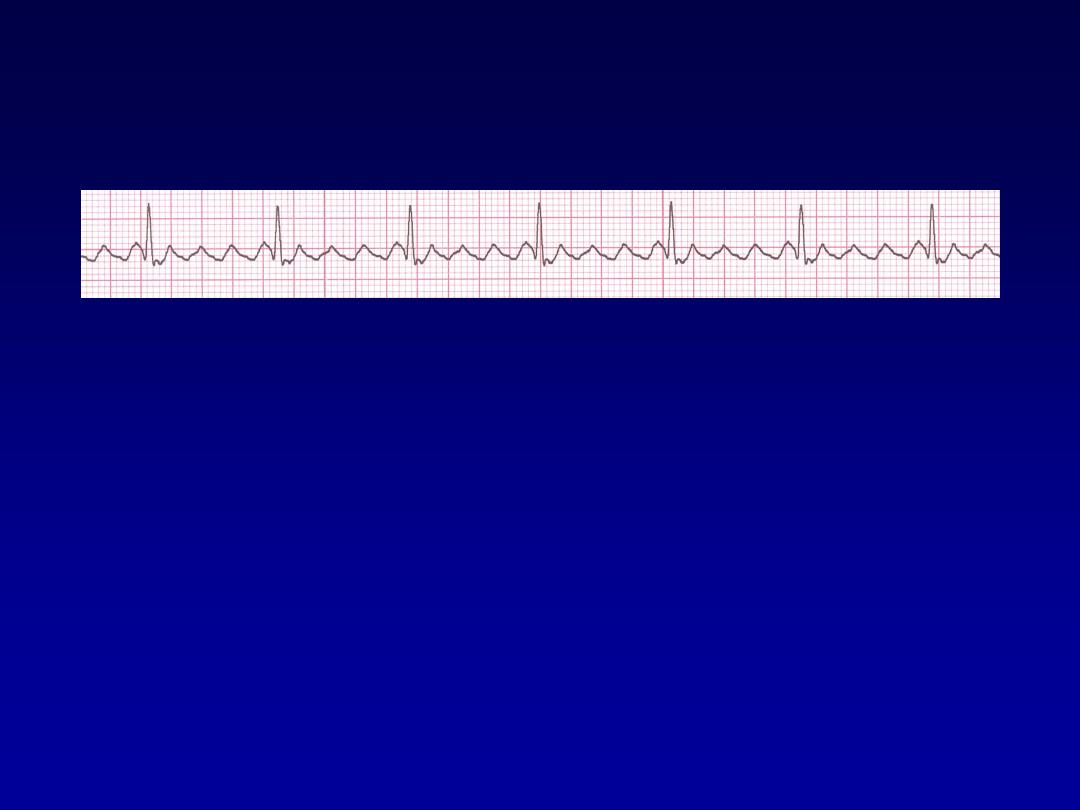
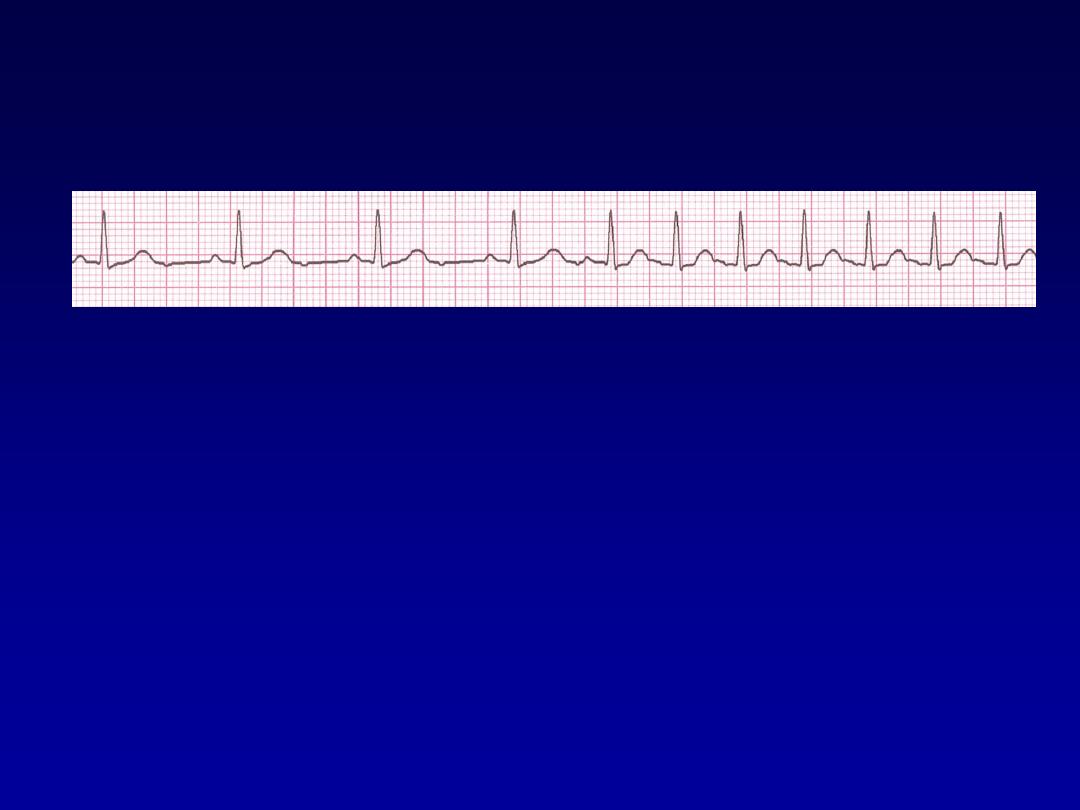
Rhythm
130 bpm
• Rate?
• Regularity?
regular
normal
0.08 s
• P waves?
• PR interval?
0.16 s
• QRS duration?
Interpretation?
Sinus Tachycardia

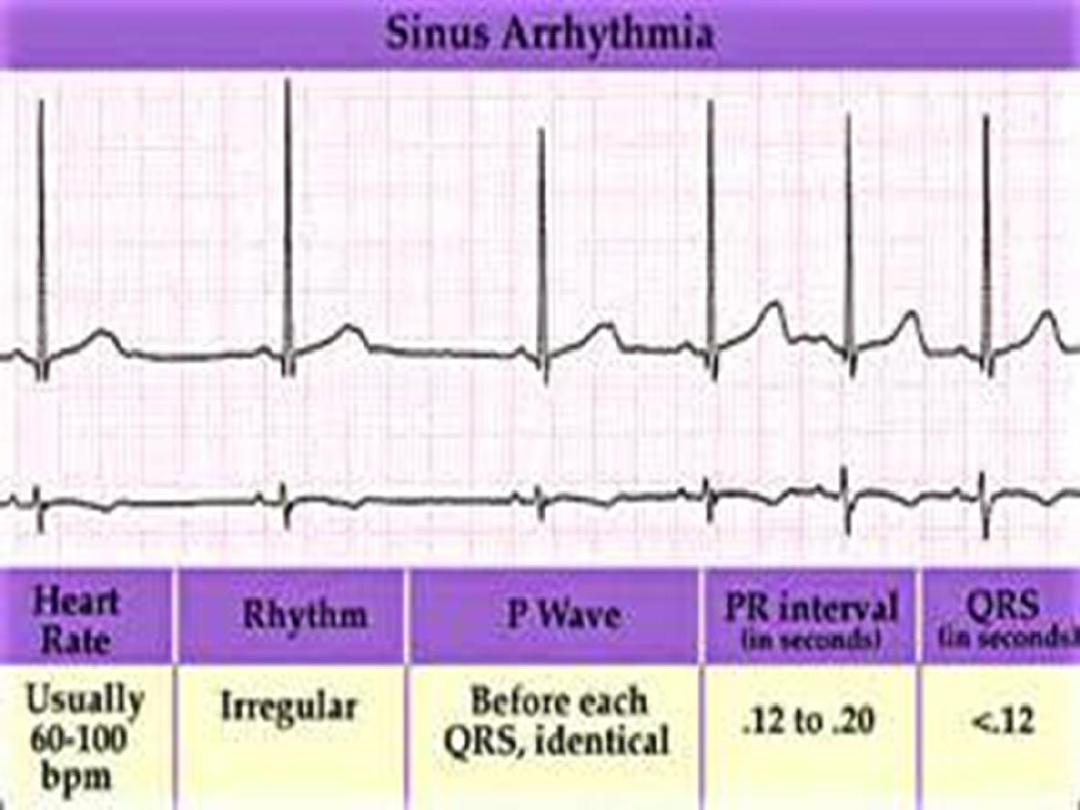
Sinus arrhythmia
•
Phasic alteration of the heart rate during
respiration (the sinus rate increases
during inspiration and slows during
expiration
For more presentations www.medicalppt.blogspot.com

Premature Beats
•
Premature Atrial Contractions
(PACs)
•
Premature Ventricular Contractions
(PVCs)
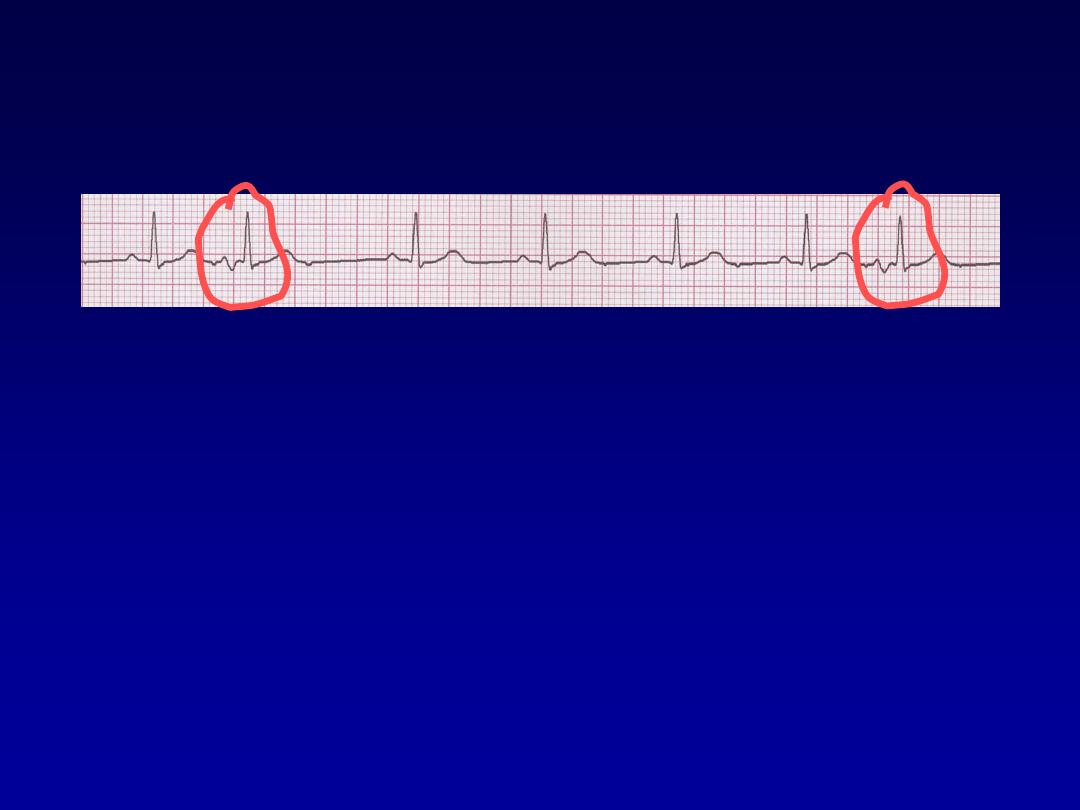
Premature Atrial Contractions
•
Deviation from NSR
–
These ectopic beats originate in the
atria (but not in the SA node),
therefore the contour of the P wave,
the PR interval, and the timing are
different than a normally generated
pulse from the SA node.
Rhythm
70 bpm
• Rate?
• Regularity?
occasionally irreg.
2/7 different contour
0.08 s
• P waves?
• PR interval?
0.14 s (except 2/7)
• QRS duration?
Interpretation?
NSR with Premature Atrial
Contractions
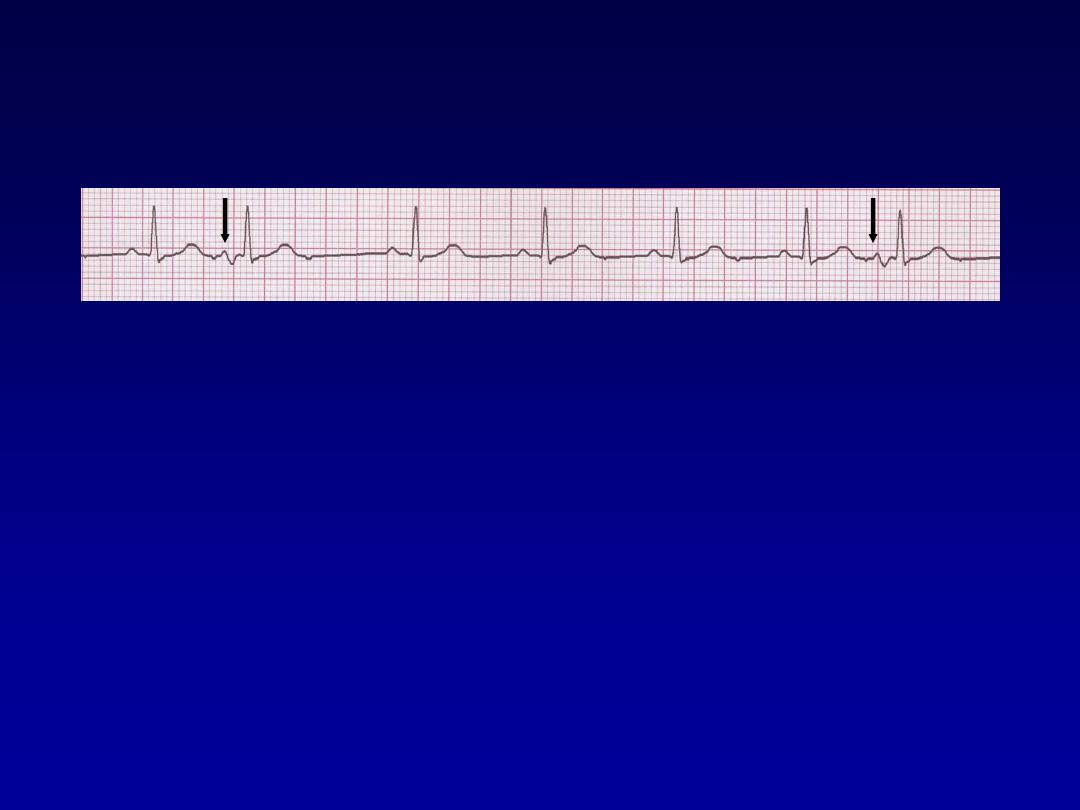
Premature Ventricular Contractions
PVCs
•
Deviation from NSR
–
Ectopic beats originate in the ventricles
resulting in wide and bizarre QRS
complexes.
–
When there are more than 1 premature
beats and look alike, they are called
“uniform”. When they look different, they are
called “multiform”
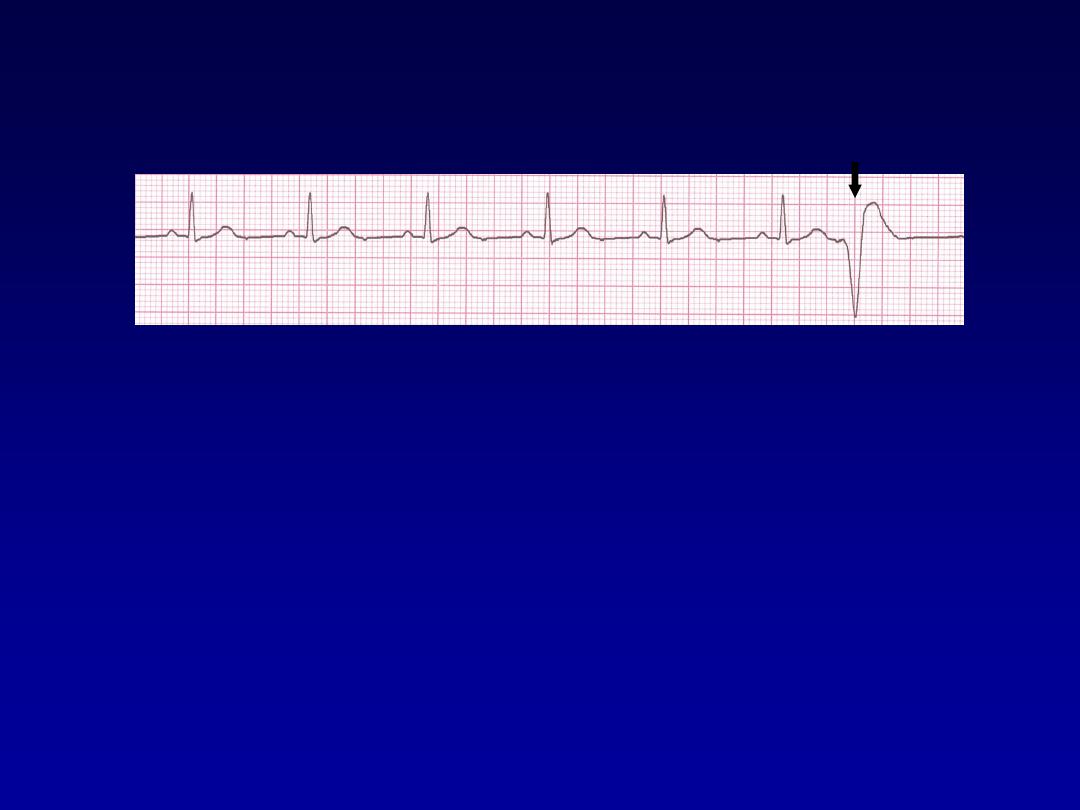
Rhythm
60 bpm
• Rate?
• Regularity?
occasionally irreg.
none for 7
th
QRS
0.08 s (7th wide)
• P waves?
• PR interval?
0.14 s
• QRS duration?
Interpretation?
Sinus Rhythm with 1 PVC

Supraventricular Arrhythmias
•
Atrial Fibrillation
•
Atrial Flutter
•
Paroxysmal Supraventricular
Tachycardia

Atrial Fibrillation
•
The most common sustained cardiac arrhythmia.
•
AF can cause palpitation, breathlessness and fatigue.
In patients with poor ventricular function or valve
disease, it may precipitate or aggravate cardiac
failure.
•
AF is associated with significant morbidity (
Thromboembolic )and a twofold increase in mortality .
•
AF can be classified as paroxysmal (intermittent
episodes which self-terminate within 7 days),
persistent
(prolonged episodes that can be
terminated by electrical or chemical cardioversion) or
permanent.

Common causes of atrial fibrillation
•
Coronary artery disease (including acute MI)
•
Valvular heart disease, especially rheumatic mitral
valve disease
•
Hypertension
•
Sinoatrial disease
•
Hyperthyroidism
•
Alcohol • Cardiomyopathy
•
Congenital heart disease
Chest infection
•
Pulmonary embolism
•
Pericardial disease
•
Idiopathic (lone atrial fibrillation)
Atrial Fibrillation
•
Deviation from NSR
–
No organized atrial depolarization, so
no normal P waves (impulses are not
originating from the sinus node).
–
Atrial activity is chaotic (resulting in an
irregularly irregular rate).
–
Common, affects 2-4%, up to 5-10% if
> 80 years old
Atrial Fibrillation
•
Etiology:
Recent theories suggest that it
is due to multiple re-entrant wavelets
conducted between the R & L atria.
Either way, impulses are formed in a
totally unpredictable fashion. The AV
node allows some of the impulses to
pass through at variable intervals (so
rhythm is irregularly irregular).
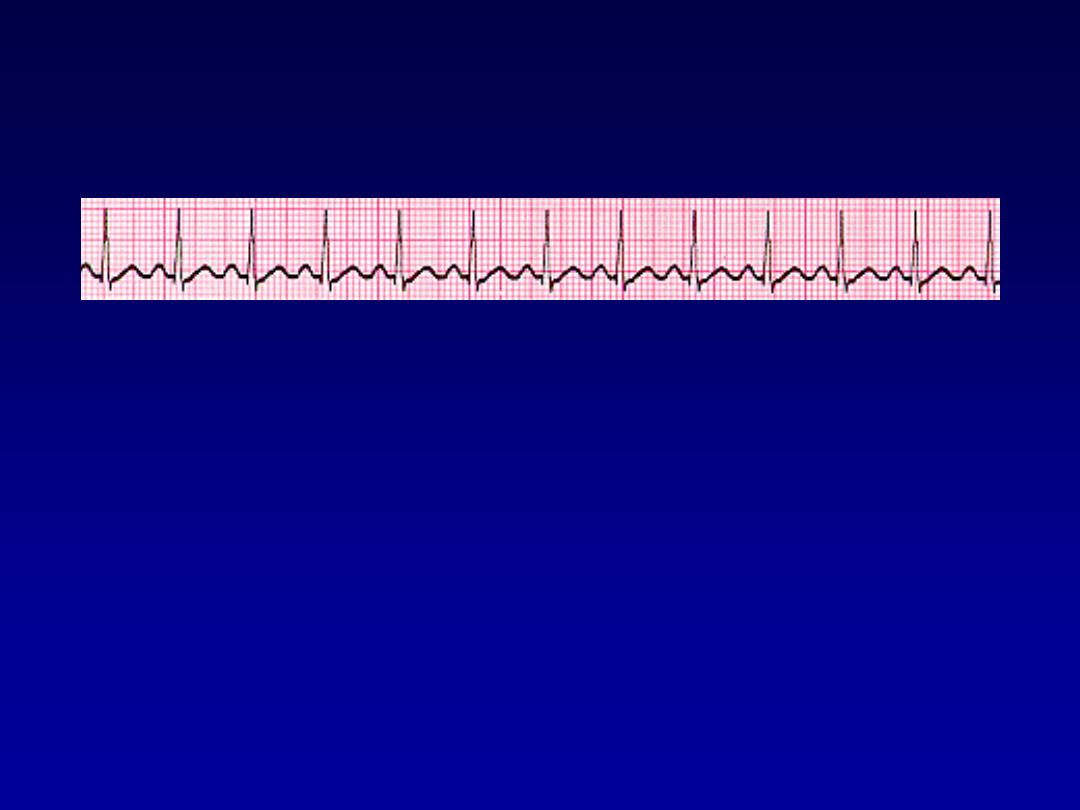
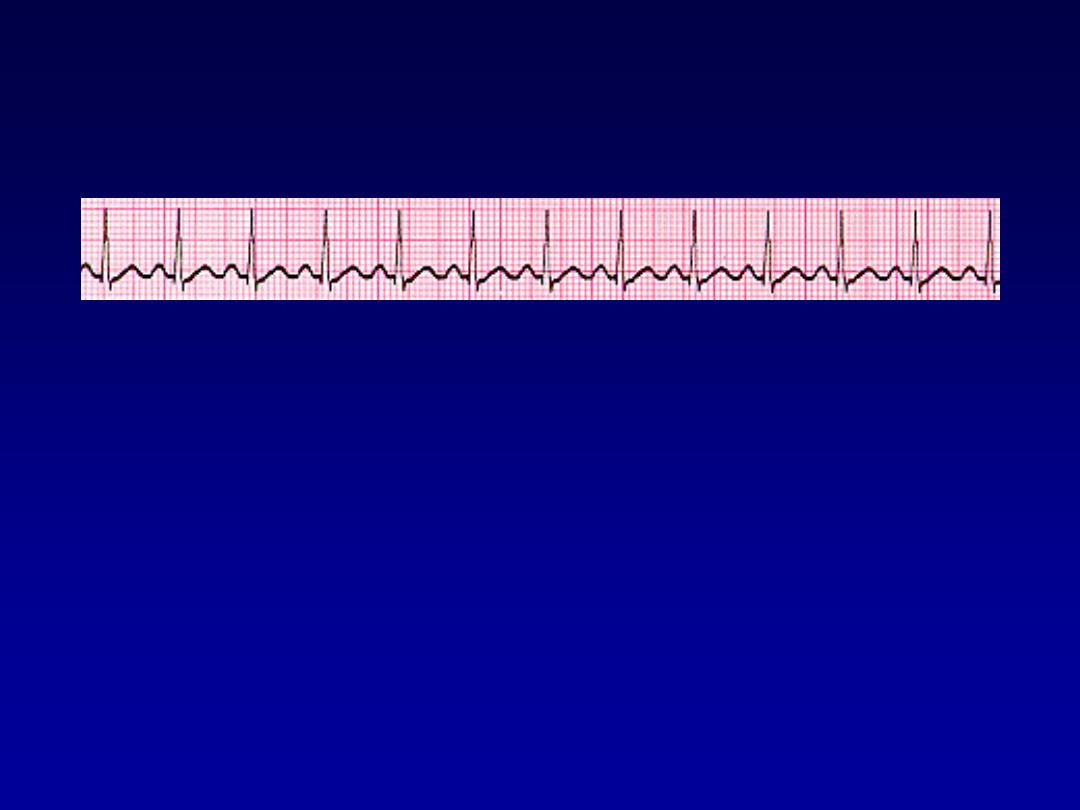
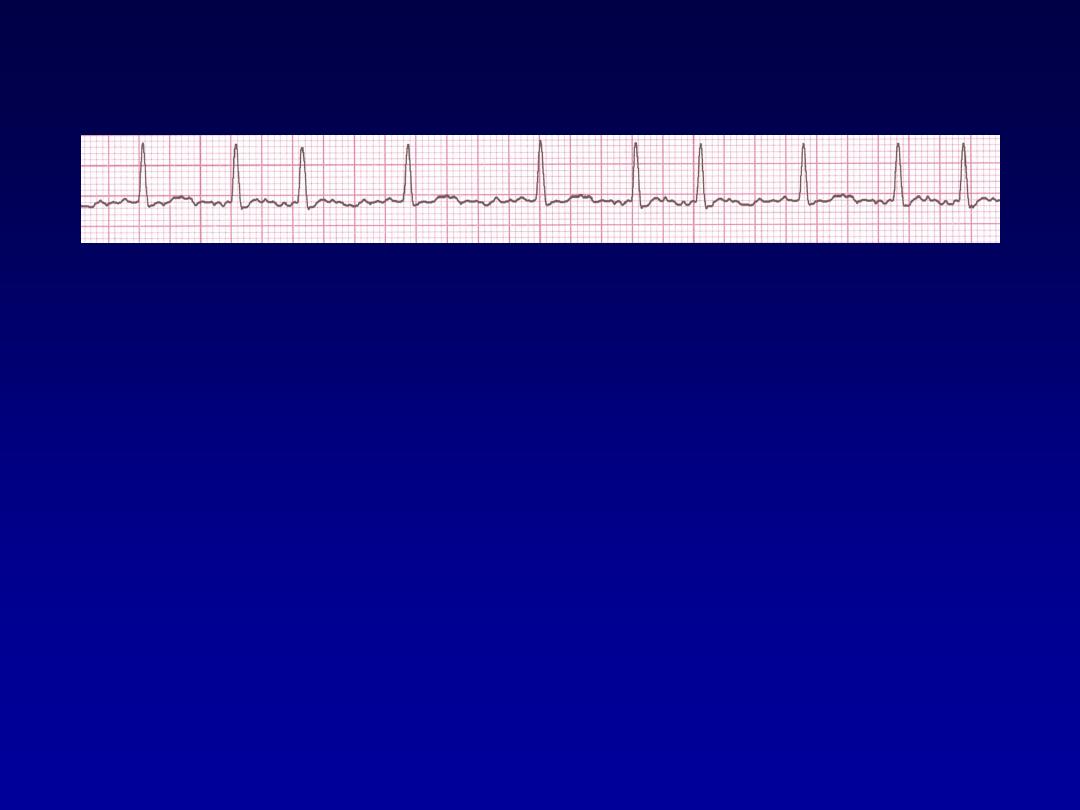
Rhythm
100 bpm
• Rate?
• Regularity?
irregularly irregular
none
0.06 s
• P waves?
• PR interval?
none
• QRS duration?
Interpretation?
Atrial Fibrillation

Management
•
Full history, physical examination, 12-lead ECG,
echocardiogram and thyroid function tests.
•
Restoration of sinus rhythm (
Rhythm control
),
•
Optimisation of the heart rate (
Rate control
)
•
Prevention of recurrent AF,
•
Reduction of the risk of thromboembolism,
•
Treatment of underlying cardiac disease
.
• Rhythm control
• Pharmacologic cardioversion
Flecainide
,Propafenon,Amiodaron
• Electrical cardioversion
- Less than 48 hours direct cardioversion.
- More than 48 hours +Anticoagulates for 4 weeks
prior and 3 months after.
Rate control
•
Using Digoxin, β-blockers and calcium antagonists,
such as verapamil or diltiazem
•
Catheter ablation in refractory cases

Prevention of
thromboembolism
•
Risk stratification is based on clinical
factors using the CHA2DS2-VASc
scoring system.
•
Warfarin INR 2-3
•
Aspirin
Atrial Flutter
•
Etiology:
a large (macro) re-entry circuit,
usually within the right atrium encircling
the tricuspid annulus with every 2nd,
3rd or 4th impulse generating a QRS
(others are blocked in the AV node as
the node repolarizes).
Atrial Flutter
•
Deviation from NSR
–
No P waves. Instead flutter waves (note
“sawtooth” pattern) are formed at a rate
of 250 - 350 bpm.
–
Only some impulses conduct through
the AV node (usually every other
impulse)

Causes and Symptoms
•
Similar to atrial fibrillation
•
Managemen
t
•
Treat the cause
•
Rate control -Digoxine B blocker,verapamil.
•
Rhythm control
–Amiodaron ,DC
•
Maintanance B- Blocker or amiodarone
•
Anticoagulant
•
Catheter ablation offers a 90% chance of complete cure
and is the treatment of choice for patients with persistent
symptoms
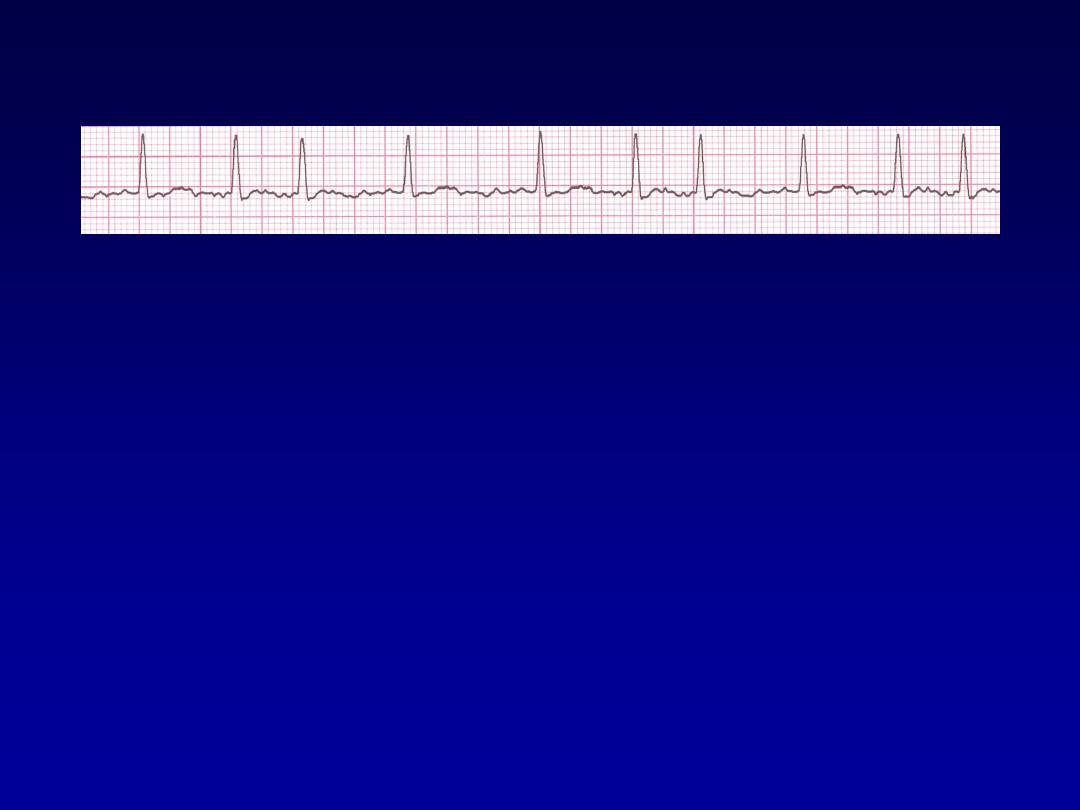
Atrial F
70 bpm
• Rate?
• Regularity?
regular
flutter waves
0.06 s
• P waves?
• PR interval?
none
• QRS duration?
Interpretation?
Atrial Flutter
Paroxysmal Supraventricular
Tachycardia (PSVT
PSVT
•
Deviation from NSR
–
The heart rate suddenly speeds up,
often triggered by a PAC (not seen
here) and the P waves are lost.
–
Tends to occur in normal heart.
PSVT
•
Etiology:
There are several types of
PSVT but all originate above the
ventricles (therefore the QRS is narrow).
•
Most common: abnormal conduction in
the AV node (reentrant circuit looping in
the AV node).
•
Rate 150-250
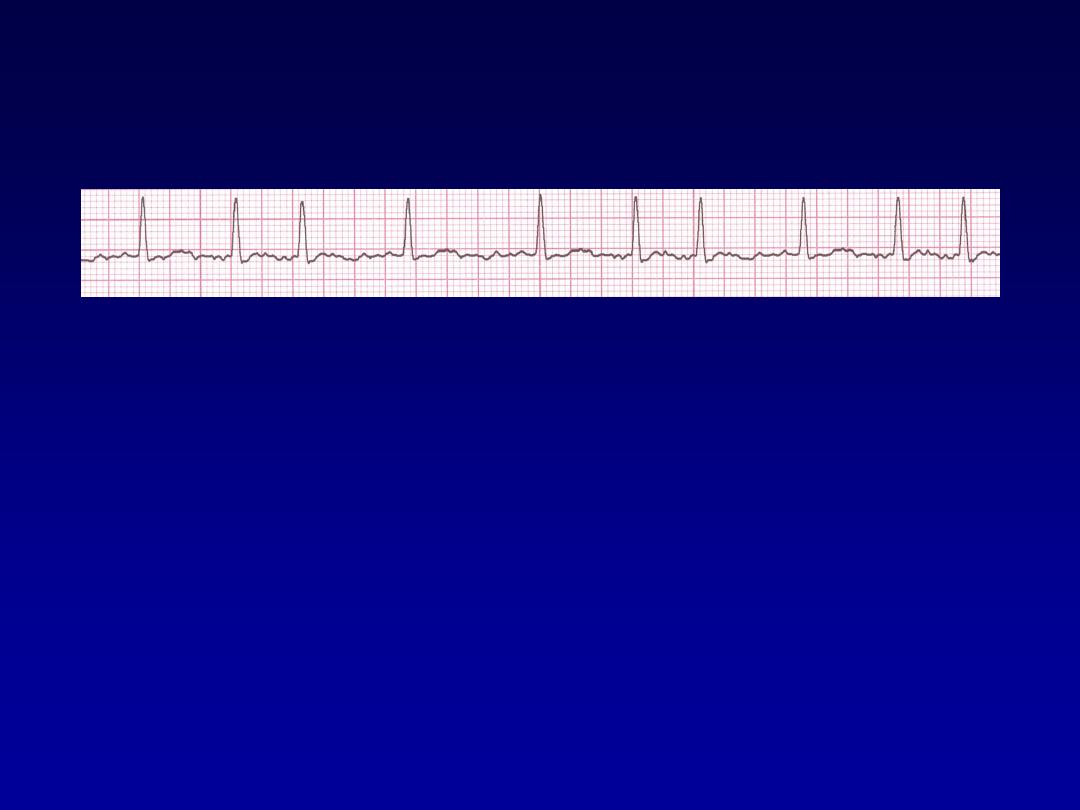
Paroxysmal Supraventricular
Tachycardia (PSVT
74 148 bpm
• Rate?
• Regularity?
Regular regular
Normal none
0.08 s
• P waves?
• PR interval?
0.16 s none
• QRS duration?
Interpretation?
Paroxysmal Supraventricular

Managment
•
Episode may be terminated by carotid sinus
pressure or by the Valsalva manœuvre.
Adenosine (3
–12 mg rapidly IV in incremental
doses until tachycardia stops) or verapamil (5
mg IV)
•
Recurrent SVT, catheter ablation is the most
effective therapy and will permanently
prevent SVT in more than 90% of cases

Ventricular Arrhythmias
•
Ventricular Tachycardia
•
Ventricular Fibrillation

Ventricular Tachycardia
•
Dangerous.
•
Nearly in abnormal heart.
•
3 or more sucsussive PVC at rate of
more than 120.
•
Can occur in normal heart.
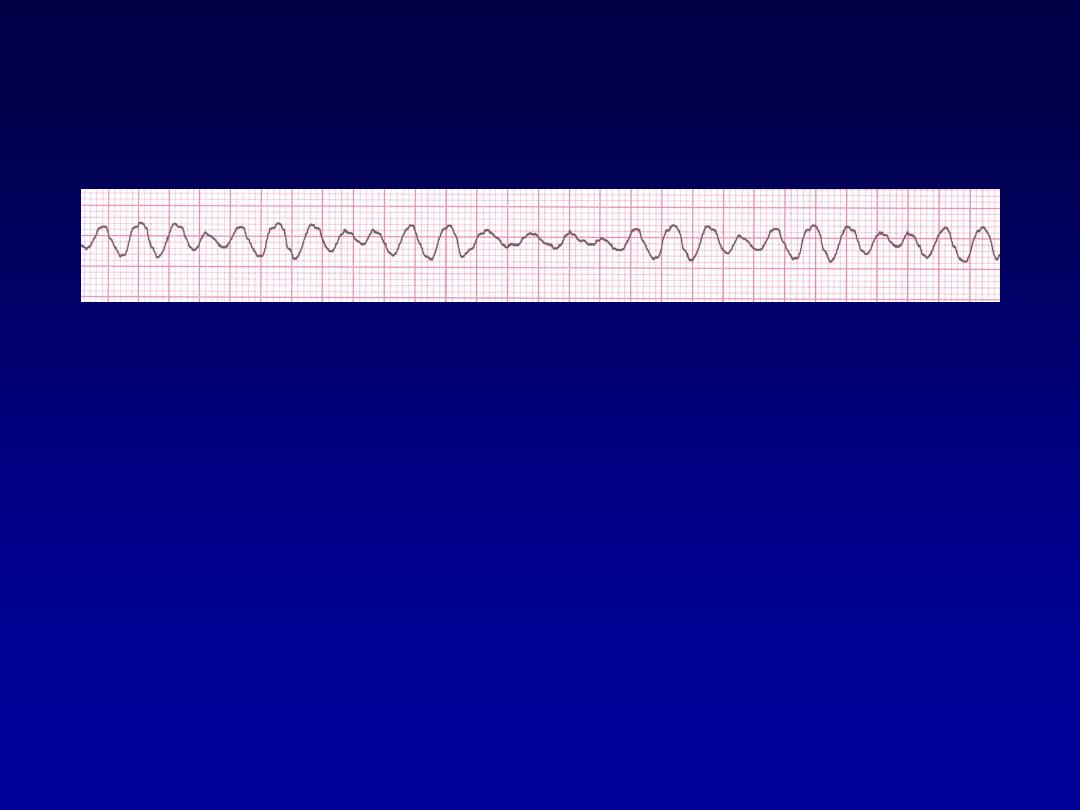
Ventricular Tachycardia
•
Deviation from NSR
–
Impulse is originating in the ventricles
(no P waves, wide QRS).
Ventricular Tachycardia
•
Etiology:
There is a re-entrant pathway
looping in a ventricle (most common cause).
•
Ventricular tachycardia (VT) occurs most
commonly in the settings of acute MI,
chronic coronary artery disease, and
cardiomyopathy.
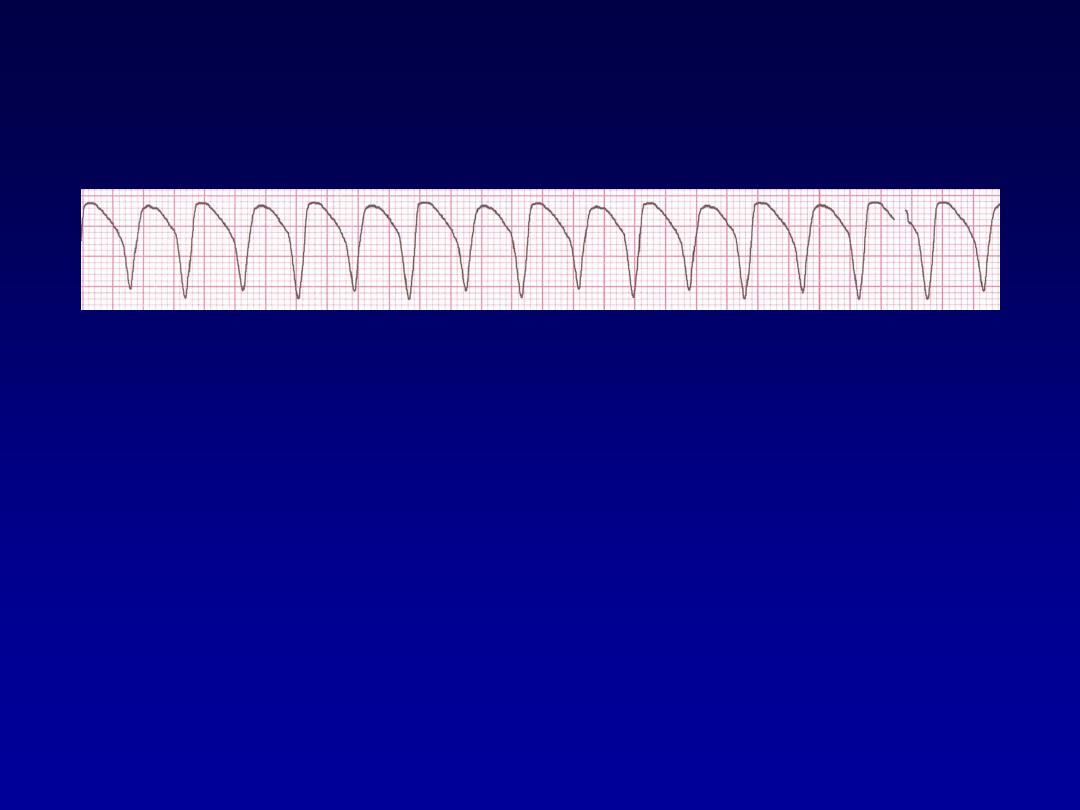
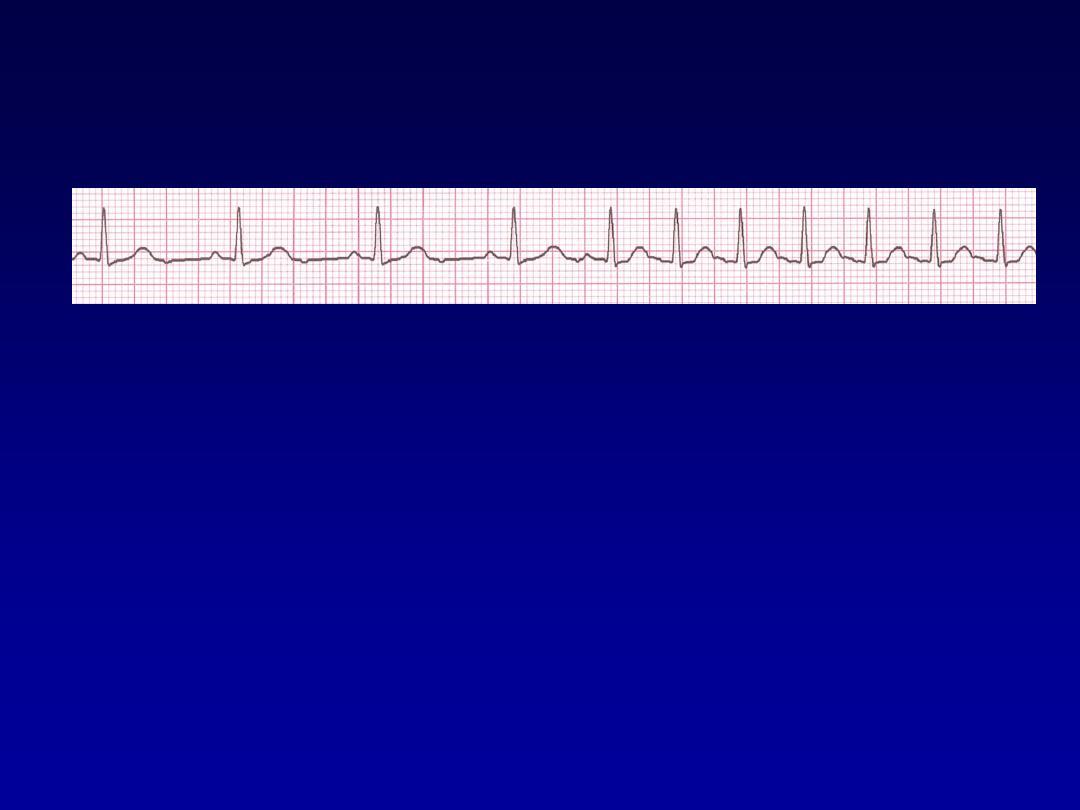
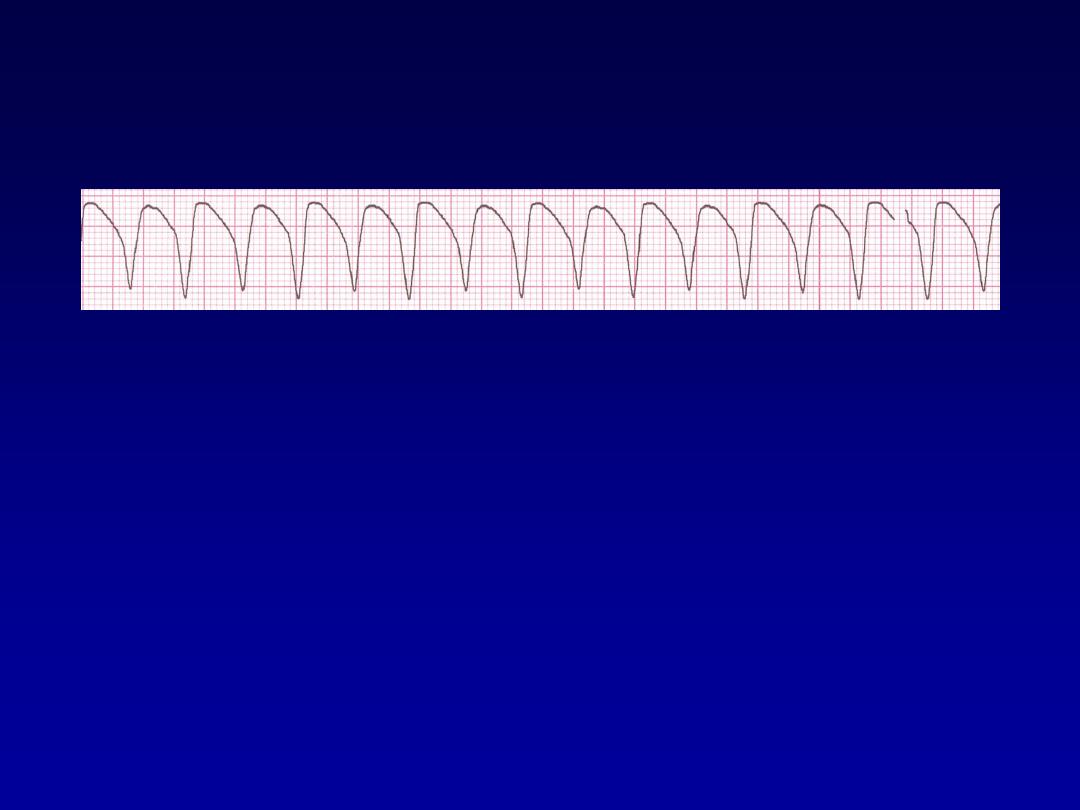
Rhythm
160 bpm
• Rate?
• Regularity?
regular
none
wide (> 0.12 sec)
• P waves?
• PR interval?
none
• QRS duration?
Interpretation?
Ventricular Tachycardia

Management
•
Treat cause.
•
Hemodynamically unstable DC
•
Stable IV amiodarone or lidocaine.
•
With poor LV function indication for ICD

Ventricular Fibrillation
•
CARDIAC ARREST
F
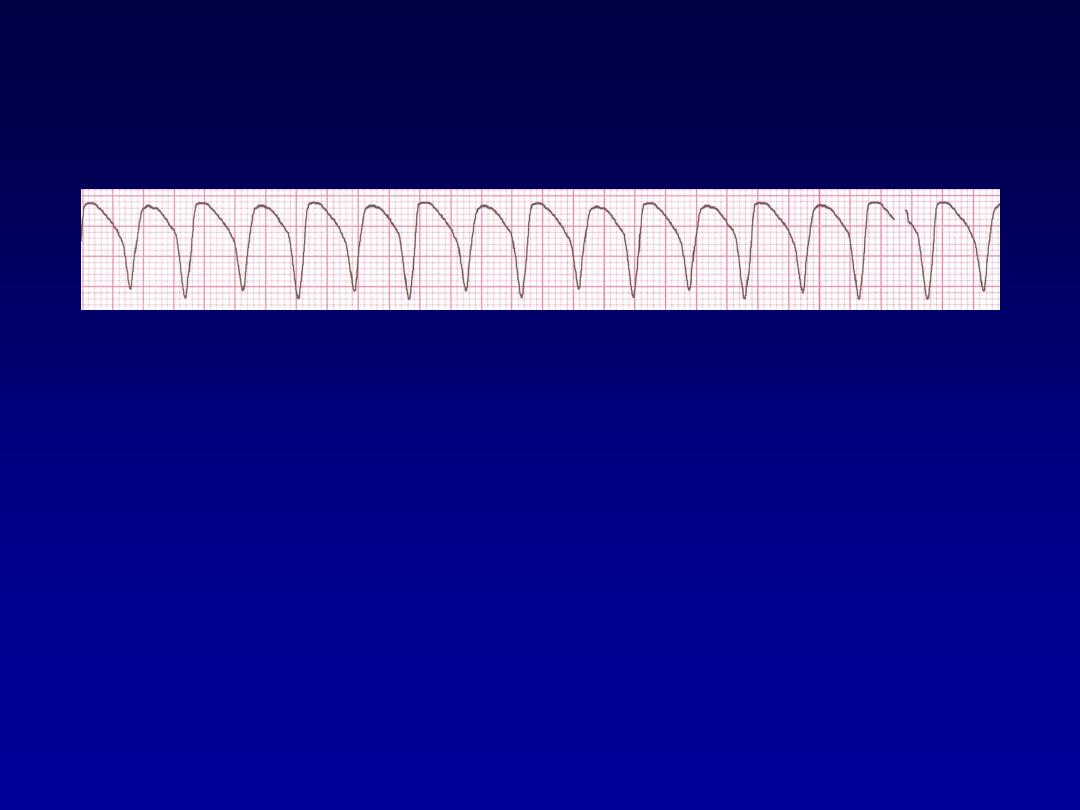
Ventricular Fibrillation
•
Deviation from NSR
–
Completely abnormal.
Ventricular Fibrillation
•
Etiology:
The ventricular cells are
excitable and depolarizing randomly.
•
Rapid drop in cardiac output and death
occurs if not quickly reversed
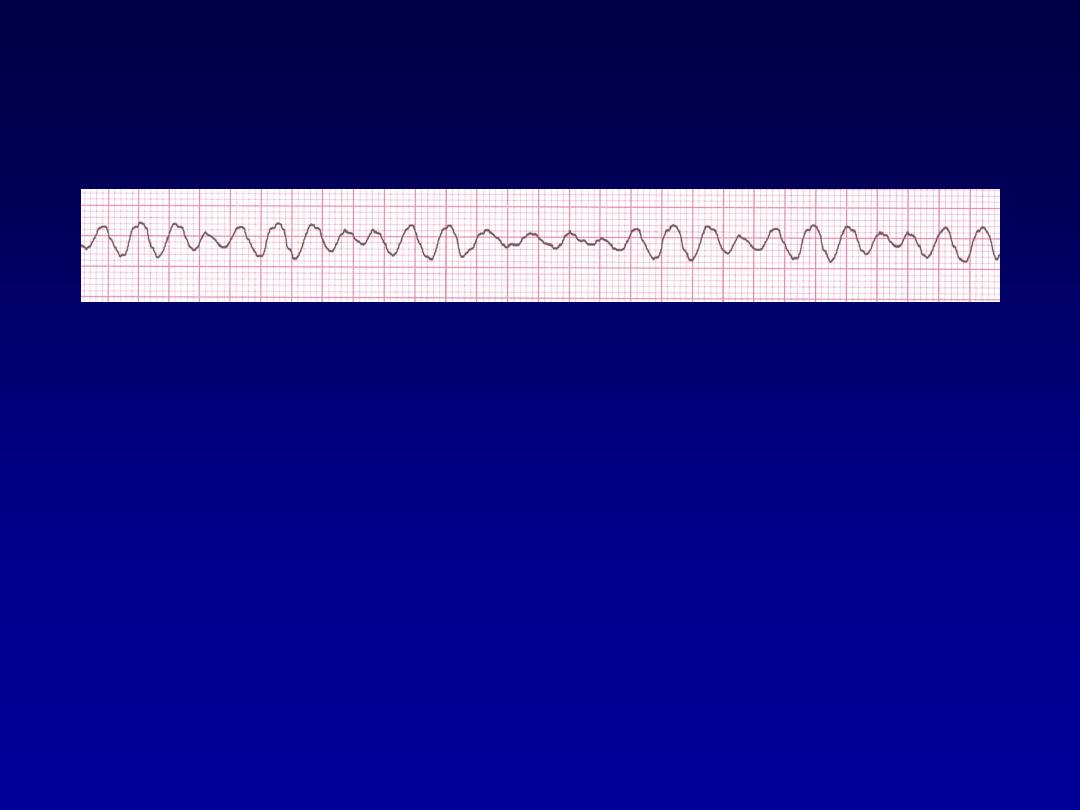
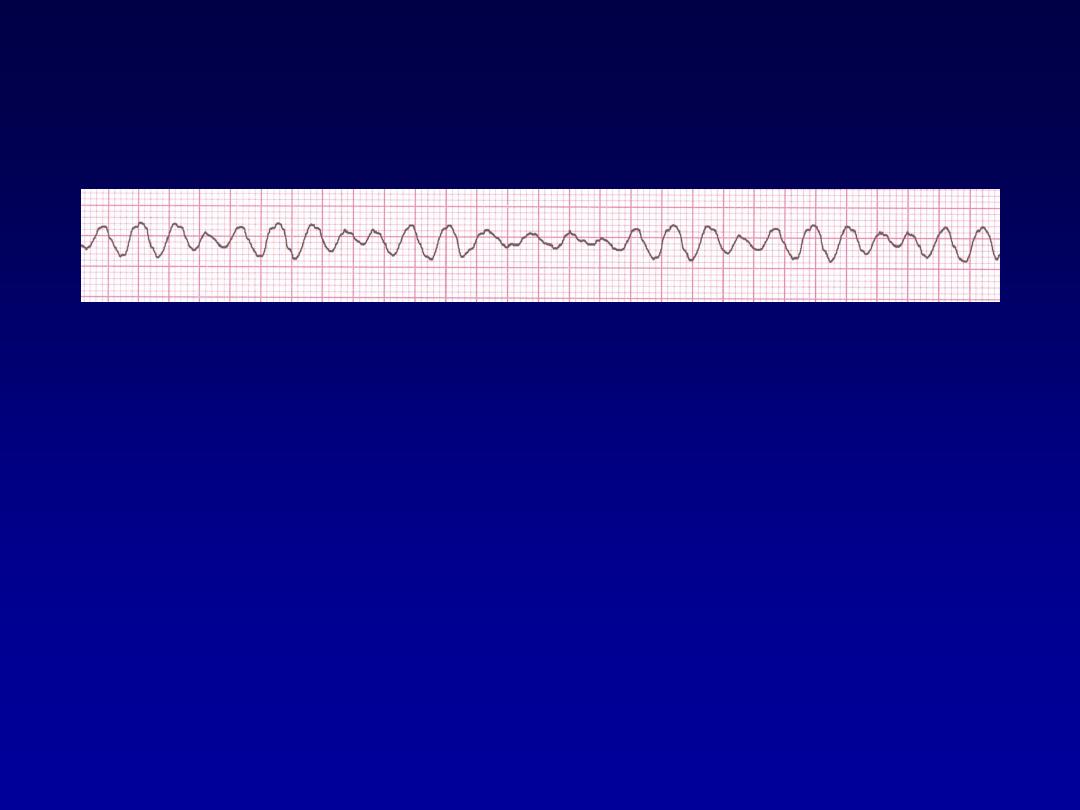
Rhythm
none
• Rate?
• Regularity?
irregularly irreg.
none
wide, if recognizable
• P waves?
• PR interval?
none
• QRS duration?
Interpretation?
Ventricular Fibrillation
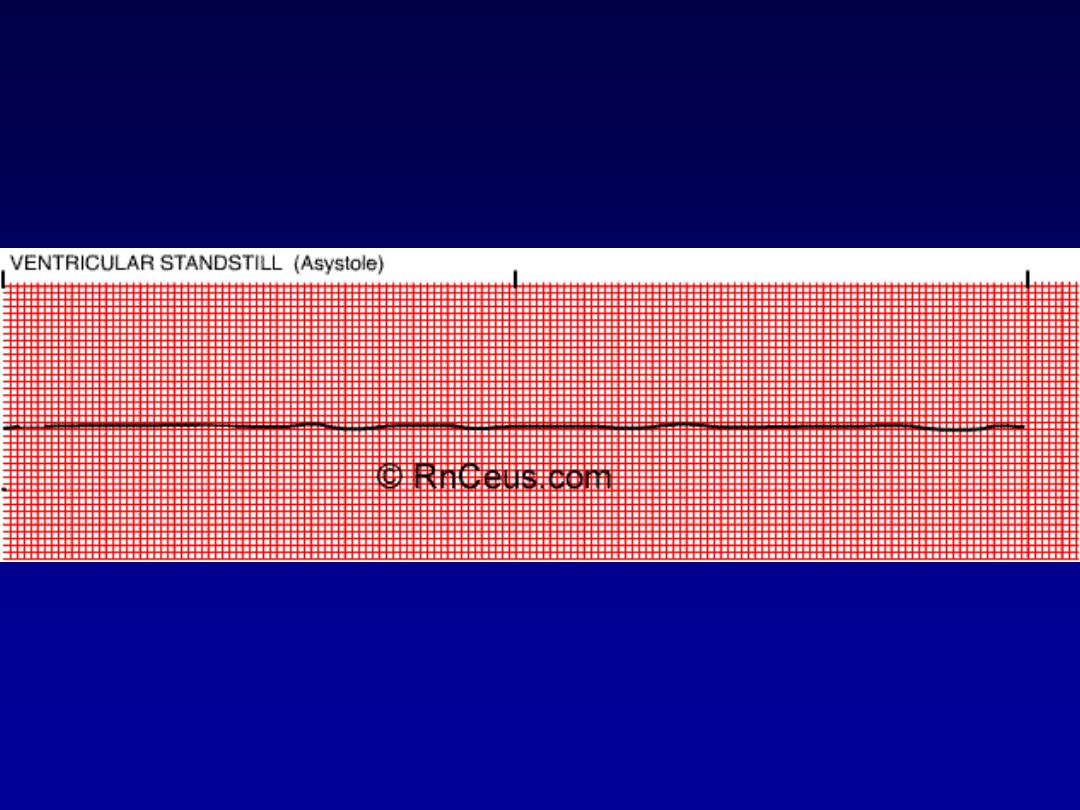
Asystole

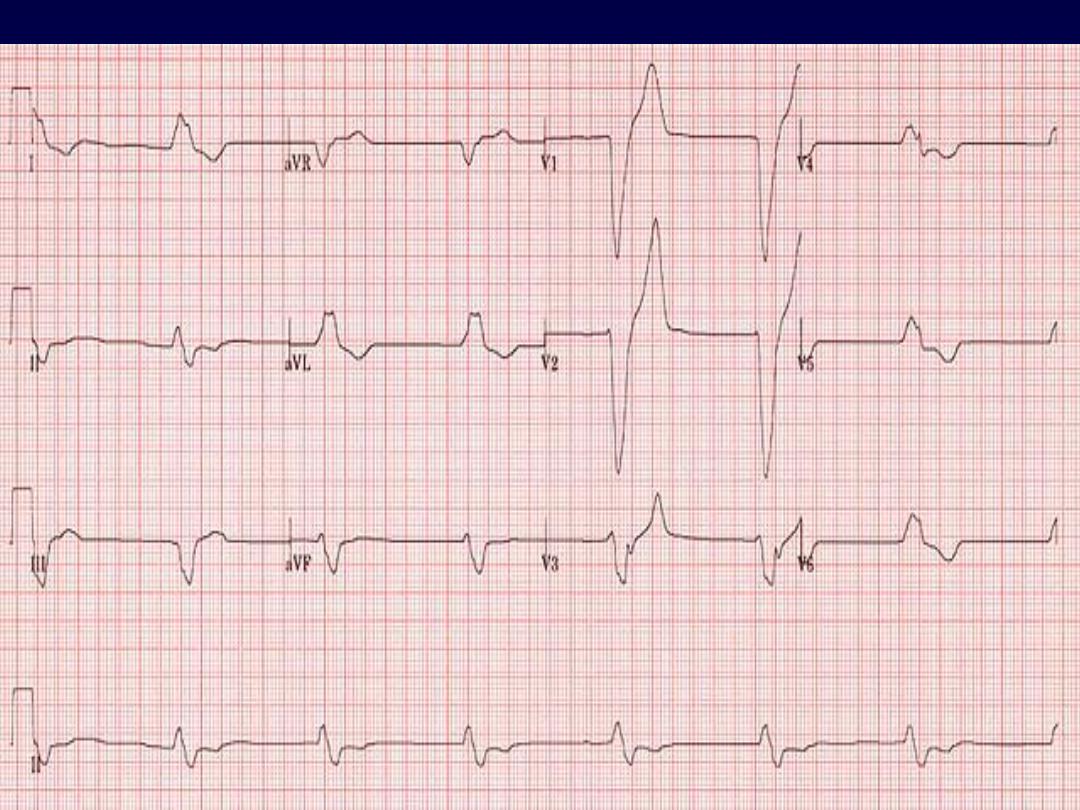
FIRST DEGREE A-V HEART
BLOCK
• Rate:
variable
• P wave:
normal
• QRS:
normal
• Conduction:
impulse originates in the SA node but has
prolonged conduction in the AV junction; P-R interval is > 0.20
seconds.
• Rhythm:
regular
•
This is the most common conduction disturbance. It occurs in
both healthy and diseased hearts.
•
First degree AV block can be due to:
inferior MI,
digitalis toxicity
hyperkalemia
increased vagal tone
acute rheumatic fever
myocarditis
.
•
Interventions include treating the underlying cause and
observing for progression to a mor
e advanced AV block.
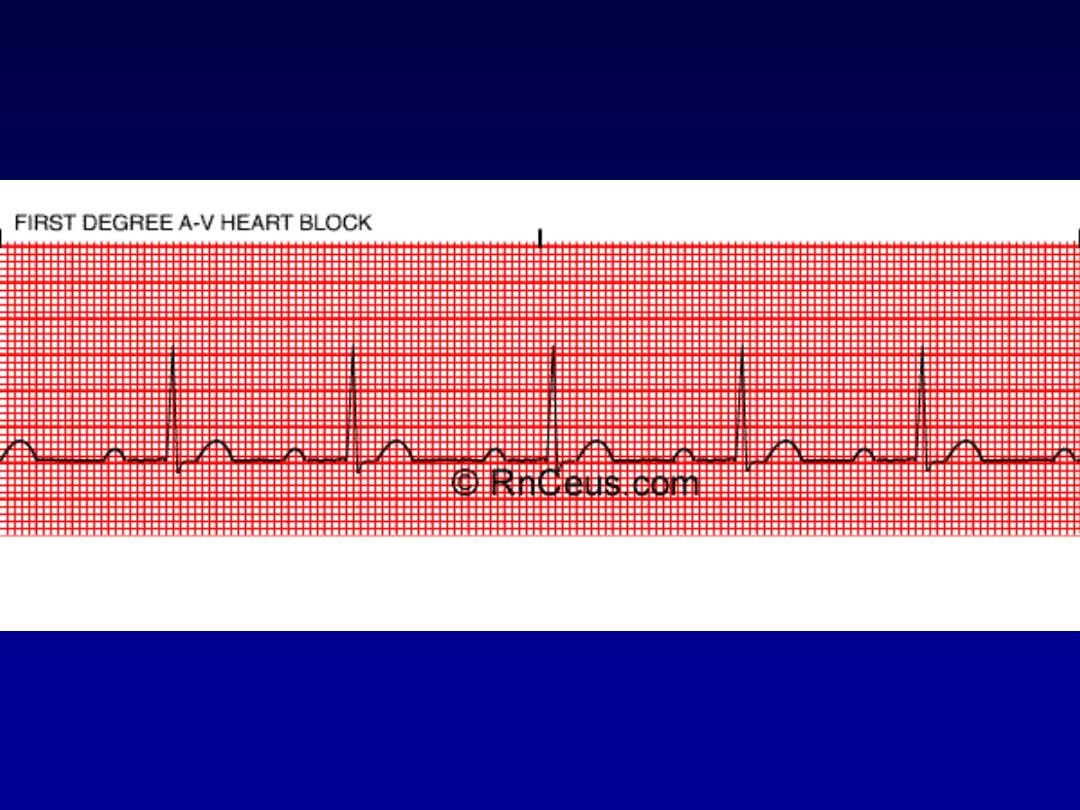
FIRST DEGREE A-V HEART BLOCK

SECOND DEGREE A-V BLOCK
MOBITZ TYPE I (WENCKEBACK)
• Rate:
variable
• P wave:
normal morphology with constant P-P interval
• QRS:
normal
• Conduction:
the P-R interval is progressively longer until one P
wave is blocked; the cycle begins again following the blocked P
wave.
• Rhythm:
irregular
•
Second degree AV block type I occurs in the AV node above the
Bundle of His.
•
It is often transient and may be due to acute inferior MI or
digitalis toxicity.
•
Treatment is usually not indicated as this rhythm usually
produces no symptoms.

SECOND DEGREE A-V BLOCK MOBITZ TYPE I (WENCKEBACK

SECOND DEGREE A-V BLOCK
MOBITZ TYPE II
• Rate:
variable
• P wave:
normal with constant P-P intervals
• QRS:
usually widened because this is usually associated with a
bundle branch block.
• Conduction:
P-R interval may be normal or prolonged, but it is
constant until one P wave is not conducted to the ventricles.
• Rhythm:
usually regular when AV conduction ratios are
constant
•
This block usually occurs below the Bundle of His and may
progress into a higher degree block.
•
It can occur after an acute anterior MI due to damage in the
bifurcation or the bundle branches.
•
It is more serious than the type I block.
•
Treatment is usually artificial pacing.
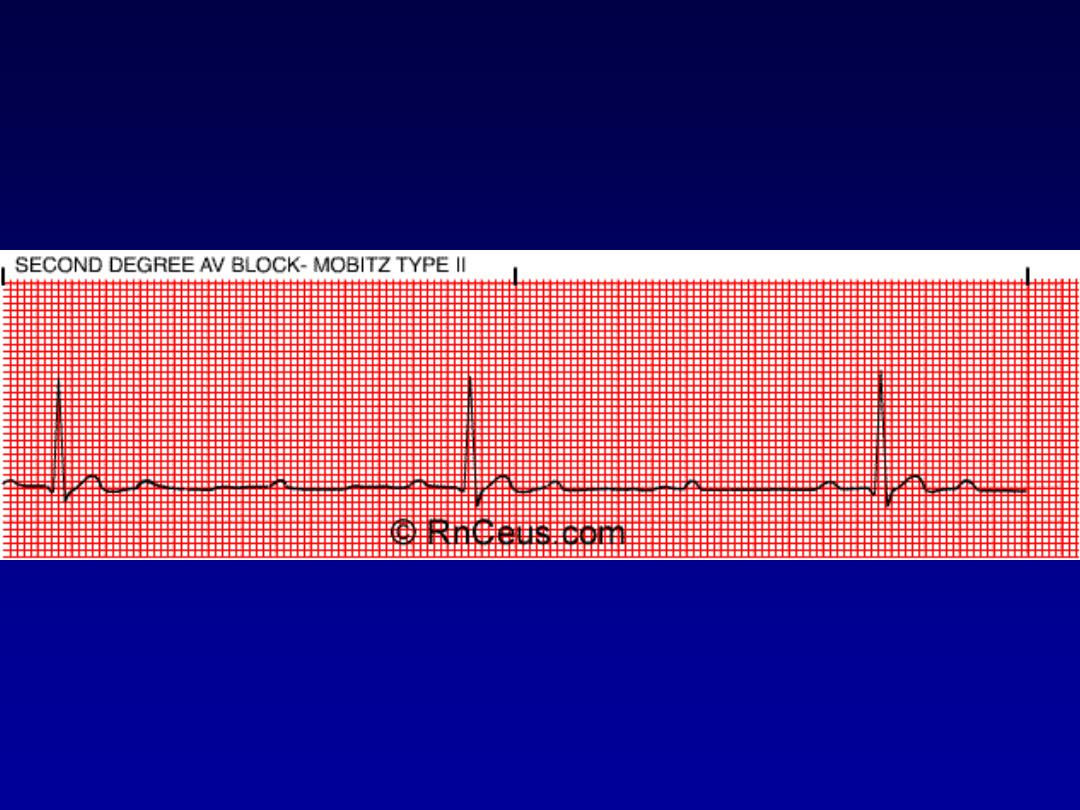
SECOND DEGREE A-V BLOCK MOBITZ TYPE II

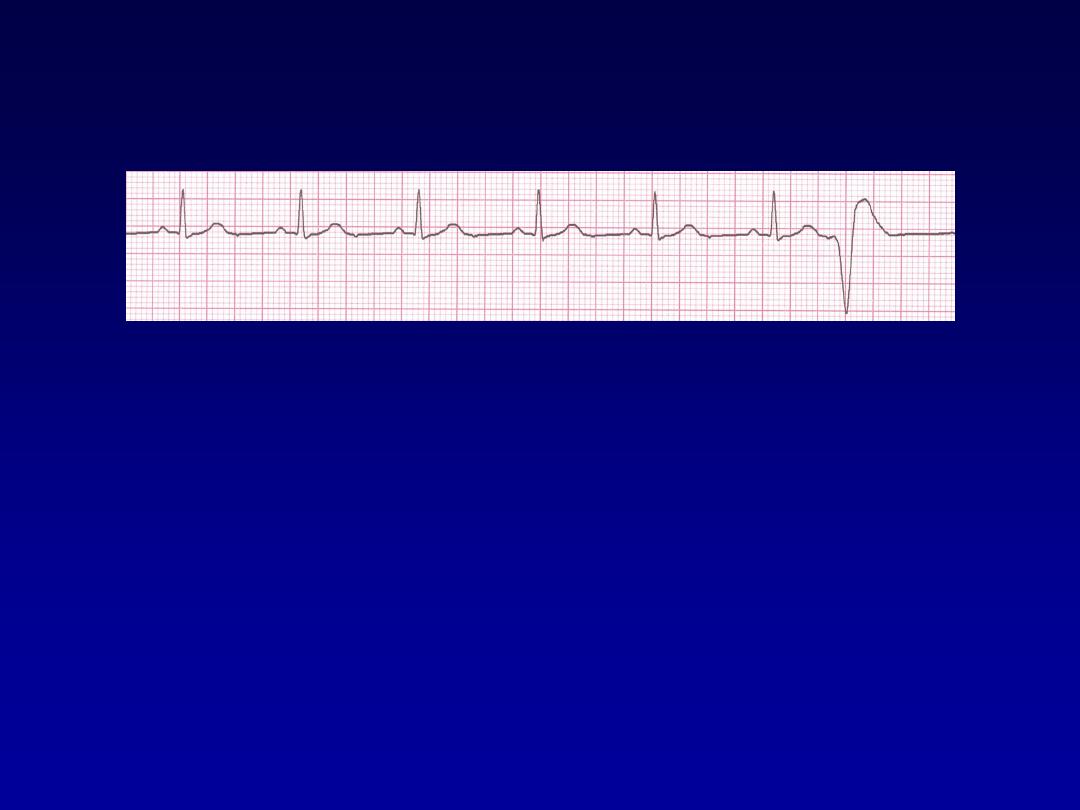
THIRD DEGREE (COMPLETE)
A-V BLOCK
•
Rate:
atrial rate is usually normal; ventricular rate is usually less than
70/bpm. The atrial rate is always faster than the ventricular rate.
•
P wave:
normal with constant P-P intervals, but not "married" to the
QRS complexes.
•
QRS:
may be normal or widened depending on where the escape
pacemaker is located in the conduction system
•
Conduction:
atrial and ventricular activities are unrelated due to the
complete blocking of the atrial impulses to the ventricles.
•
Rhythm:
irregular
•
Complete block of the atrial impulses occurs at the A-V junction,
common bundle or bilateral bundle branches.
•
Another pacemaker distal to the block takes over in order to activate
the ventricles or ventricular standstill will occur.
•
May be caused by:
digitalis toxicity
acute infection
MI and
degeneration of the conductive tissue.
•
Treatment modalities include:
external pacing and atropine for acute, symptomatic episodes and
permanent pacing for chronic complete heart block.

THIRD DEGREE (COMPLETE) A-V BLOCK

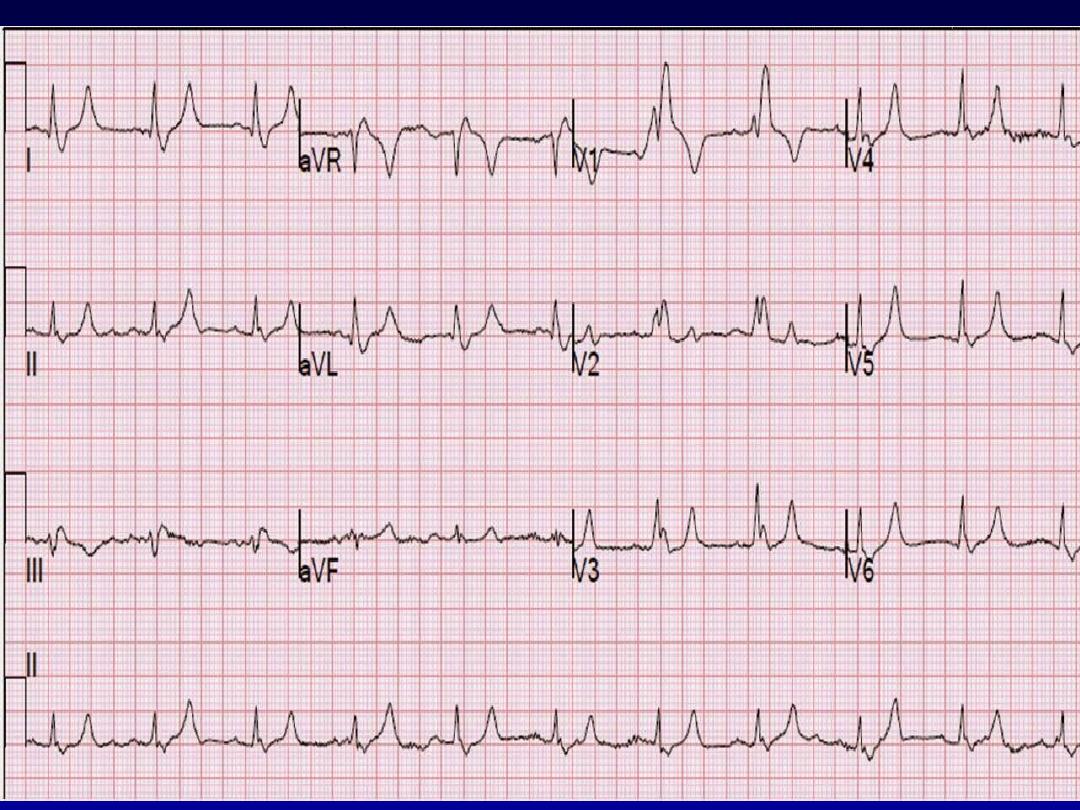
Bundle branch block and hemiblock
•
Left bundle branch block LBBB
•
Right bundle branch block RBBB
For more presentations www.medicalppt.blogspot.com
For more presentations www.medicalppt.blogspot.com
For more presentations www.medicalppt.blogspot.com

Questions
