Fifth stage
pediatricLec-6
د.اثل
17/11/2015
SEVERE CHILDHOOD UNDERNUTRITION (SCU)Protein energy malnutrition (PEM)Objective• To know the cause of SCU.• To know its types.• To define marasmus.• To distinguish its manifestation.• To define kwashiorkor.• To distinguish its manifestation.• To know the complication of PEM• To know the treatment of PEMProtein energy malnutrition(PEM)Marasmus was thought to result primarilyfrom inadequate energy intake, whereaskwashiorkor was thought to result primarilyfrom inadequate protein intake.Marasmic kwashiorkor, has features ofboth disorders (wasting and edema).
ETIOLOGY:✎ primary malnutrition : malnutritionresulting from inadequate food intake✎ secondary malnutrition :• increased nutrient needs.• decreased nutrient absorption.• increased nutrient losses.
MARASMUS(Non-edematous SCU)Can be defined as: Emaciation with body weightBelow 60 % of median (50th percentile) for ageOrBelow 70% of the ideal weight for heightAndDepleted body fat storeLoss of muscle mass and subcutaneous fat stores isconfirmed by inspection or palpation and quantified byanthropometric measurements.
CLINICAL MANIFESTATIONS:• Growth chart criteria.• Mental changes: irritability, listlessness, may be apathetic & weak• failure to gain weight, weight loss, until emaciation results.• Skin: dry ,thin, loses turgor and becomes wrinkled and loose assubcutaneous fat disappears. Loss of fat from the sucking pads of thecheeks often occurs late in the course of the disease; thus, the infant'sface may retain a relatively normal appearance compared with the restof the body, but this, too, eventually becomes shrunken and wizened. Head: may appear large but proportional to length• Hair: thin sparse easily pulled Tongue: atrophy of filliform papilli, monilial stomatitis• Muscles: atrophy and resultant hypotonia Abdomen may be distended or flat, and the intestinal pattern may bereadily visible.• temperature usually becomes subnormal and the pulse slows.• Constipation but may develop starvation diarrhea with frequent smallstool containing mucous• Infections and parasitic infestations are common.
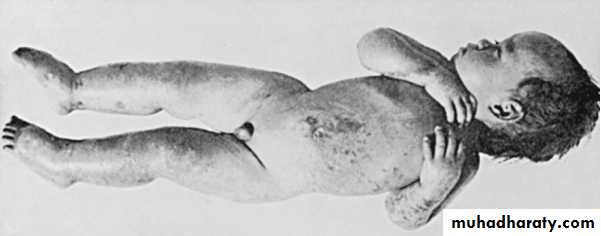
KwashiorkorEdematous SCUHypoalbuminemic, edematous malnutritionmay become evident from early infancy toabout 5 yr of age, usually after weaning fromthe breast.Can be defined as:☯ Body weight of the child ranges from 60-80% of expected weight for age☯ With edema.
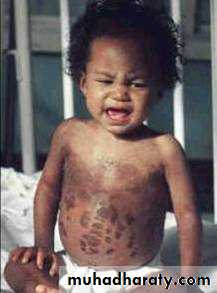
CLINICAL MANIFESTATIONS:• Growth chart criteria.• Mental changes: especially irritability and apathy, are common.Stupor, coma, and death may follow• Hair:– often sparse and thin, easily plucked, appears dull brown, red, oryellow-white.– nutritional repletion restores hair color, leaving a band of hairwith altered pigmentation followed by a band with normalpigmentation (flag sign).• Face: facial edema result in moon facies• Skin: a relative maintenance of subcutaneous adipose tissue, skinchanges are common and may include:– Hyperpigmented hyperkeratosis– Erythematous macular rash (pellagroid) on the trunk and extremities.Darkening of the skin appears in irritated areas but not in those exposedto sunlight, a contrast to the situation in pellagra– In the most severe form of kwashiorkor, a superficial desquamation occursover pressure surfaces ("flaky paint" rash).
Flaky paint” dermatosis on the thighs
Flaky paint” dermatosis
Diffuse fine scale in a reticulated pattern over the abdomen
Kwashiorkor, apathy and misery
• Edema:– Varies from a minor pitting of the dorsum of the foot to generalizededema with involvement of the eyelids and scrotum– Edema usually develops early; failure to gain weight may be masked byedema, which is often present in internal organs before it can berecognized in the face and limbs.• Muscle :marked atrophy of muscle mass.• Tongue and mouth: Angular cheilosis, atrophy of the filiformpapillae of the tongue, and monilial stomatitis are common• Abdomen: may reveal an enlarged, soft liver with an indefinite edge.The abdomen is distended, and bowel sounds tend to be hypoactive• GIT: anorexia ,vomiting, diarrhea.Others: Lymphatic tissue commonly is atrophic. Infections andparasitic infestations are common
COMPLICATIONS of PEM➷ Infection :Malnourished children are more susceptible to infection,especially sepsis, pneumonia, and gastroenteritis. because:☯ Malnutrition causes defects in host defenses.☯ Conversely, infection increases the metabolic needs of thepatient and often is associated with anorexia.☯ Children with FTT may suffer from a malnutrition-infectioncycle, in which recurrent infections exacerbate malnutrition,which leads to greater susceptibility to infection. Children withFTT must be evaluated and treated promptly for infection andfollowed closely. Treatment regimens should be appropriate forthe infection.
Noma
➷ Refeeding syndrome:• With the rapid reinstitution of feeding after starvation, fluidand electrolyte homeostasis may be lost, and the body may beunable to maintain normal serum concentrations of vitalelectrolytes.• Changes in serum electrolyte concentrations and the associatedcomplications resulting from these changes are collectively termedrefeeding syndrome.• These changes typically cause decrease in phosphorus, potassium,calcium, and magnesium and can result in life-threateningcardiac or neurological problems.• Serum phosphate levels of ≤0.5 mmol/L can produce weakness,rhabdomyolysis, neutrophil dysfunction, cardiorespiratoryfailure, arrhythmias, seizures, altered level of consciousness,or sudden death.• Refeeding syndrome can be avoided by slow institution ofnutrition for children with severe malnutrition, close monitoringof serum electrolytes during the initial days of feeding, andprompt replacement of depleted electrolytes.➷ Hypoglycemia is common after periods of severefasting, but also may be a sign of sepsis.➷ Hypothermia may signify infection or, withbradycardia, may signify a decreased metabolic rateto conserve energy. Bradycardia and poor cardiacoutput predispose the malnourished child to heartfailure, which is exacerbated by acute fluid orsolute loads.➷ Micronutrient deficiencies also can complicatemalnutrition. Vitamin A and zinc deficiencies arecommon in the developing world and are animportant cause of altered immune response andincreased morbidity and mortality.➷ Depending on the age at onset and the duration ofthe malnutrition, malnourished children may have– Permanent growth stunting– Delayed development
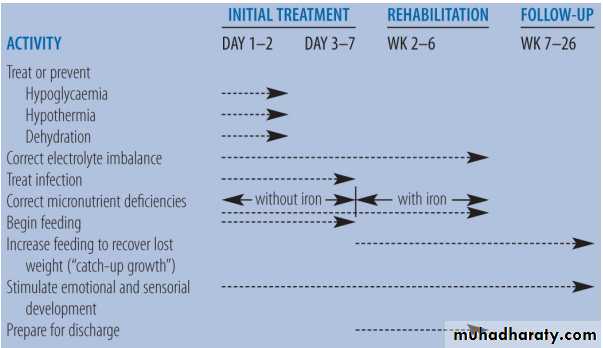
Treatment:In general the simples and leastcoasty approach is recommendedThe usual approach to treatment ofPEM includes three phases.1. stabilization phase:The first relatively brief phase (1-7 days) . During thisphase,☯ Dehydration, if present, is corrected and☯ Antibiotic therapy is initiated to control infection.Because of the difficulty of estimating hydration, oralrehydration therapy is preferred. If intravenous therapy isnecessary, estimates of dehydration should be assessedfrequently, particularly during the first 24hr of therapy.☯ Treat or prevent hypothermia, hypoglycemia, electrolyteimbalances.☯ Oral feedings are also started with specialized high-calorieformula, that can be made with simple ingredients. The initialphase of oral treatment is with the F75 diet (75 kcal or 315kg/100 mL).2. Rehabilitation phase2nd phase last (2-6weeks): includes• Continued antibiotic therapy with appropriate changes if theinitial combination was not effective and• Diet :providing maintenance requirements of energy and proteinalong with adequate electrolytes, trace minerals, and vitamins.Nutritional management similar to FTT• The rehabilitation diet is with the F100 diet (100 kcal or 420kg/100 mL). Feedings are initiated with higher frequency andsmaller volumes; over time, the frequency is reduced from 12 to 8to 6 feedings/24 hr.• If the infant is unable to take the feedings from a cup or bottle,administration of feedings by nasogastric tube rather than by theparenteral route is preferred.• Iron supplements are not recommended during the acuterehabilitation phase, especially for children with kwashiorkor, forwhom ferritin is often high. Additional iron may pose an oxidativestress, and iron supplementation has been associated with highermorbidity and mortality.By the end of the second phase:☢ Any edema that was present has usuallybeen mobilized.☢ Infections are under control.☢ The child is becoming more interested in hisor her surroundings, and his or her appetiteis returning.3. the final follow-up phaseWhich consists of feeding to covercatch-up growth as well as the provisionof emotional and sensory stimulation.The child should be fed ad libitum.The child should be switched graduallyto a recovery diet providing up to150kcal/kg/24hrூ In all phases, parental education iscrucial for continued effectivetreatment as well as prevention ofadditional episodes.Time Frame for the Management of a Child with Severe Malnutrition