Portal Hypertension
Portal hypertension is due to increased resistance to portal blood flow and to lesser extend to increased flow.Portal hypertension can be classified as:
Pre-hepatic.
Intra-hepatic and
Post-hepatic.
Causes are:
Prehepatic pre-sinusoidal:
Portal vein thrombosis due to sepsis (umbilical, portal pyaemia) or procoagulopathy or secondary to cirrhosis
Abdominal trauma including surgery
Intrahepatic pre-sinusoidal: Schistosomiasis, Congenital hepatic fibrosis, Drugs, Vinyl chloride, Sarcoidosis
Sinusoidal: Cirrhosis, Polycystic liver disease, Nodular regenerative hyperplasia, Metastatic malignant disease
Intrahepatic post-sinusoidal: Veno-occlusive disease
Post-hepatic post-sinusoidal : Budd–Chiari syndrome
Complications of portal hypertension:
Variceal bleeding: oesophageal, gastric, rectal (rare)Congestive gastropathy
Hypersplenism
Ascites
Iron deficiency anaemia
Renal failure
Hepatic encephalopathy
+ Caput medusa is a clinical feature
Esophageal Varices
Occurs in patients with signs of portal hypertension such as splenomegaly, abdominal wall collaterals or ascites.
Endoscopy is the diagnostic test for varices . and for endoscopic therapy (sclerotherapy and banding).
Esophageal varices are less likely to bleed if the portal pressure is < 12 mmHg..
Treatment
Vasopressin and analogues (octreotide, terlipressin).
Non-selective beta-blockers: used for primary prophylaxis.
Endoscopic scletrotherapy and/or banding (ligation).
Decompressive shunt procedures:
Surgical shunts: portocaval, mesocaval.
Transvenous intrahepatic portosystemic shunt (TIPS).
Ascites
Causes:Common causes:
•Malignant disease ( Hepatic, Peritoneal)
• Cardiac failure
• Hepatic cirrhosis
Other causes
• Hypoproteinaemia (Nephrotic syndrome,Protein-losing enteropathy, Malnutrition)
• Pancreatitis
• Lymphatic obstruction
• Hepatic venous occlusion
•Tuberculosis
Rare causes
• Meigs’ syndrome • Hypothyroidism
Pathogenesis of ascites appears to be due to cytokine-induced peripheral arterial vasodilatation with compensatory (and inappropriate) renovascular constriction.
Paracentesis is the best test to assess the etiology of ascites (color, albumin, amylase, WBC, cytology, microscopy & culture) *transudate has total protein less than 25g/l.
The serum ascites albumin gradient (SAAG) can differentiate ascites resulting from portal hypertension (transudate) from non-portal hypertensive causes (more than 11 is due to portal hypertension)
TREATMENT OF ASCITES
Restriction of dietary Na to 80 mmol/day (no adding table salt).If there is severe ascites we should restrict Na to (40 mmol/day) and should avoid drugs cause salt retention like NSAIDs.
Restriction of water to about 0.5-1 L/day which is important especially when Na fall below 125 mmol/L (because dilutional hyponatremia may occur).
Diuretic treatment: the best one is spironolacton in (100-400mg/day). Side effects are painful gynecomastia & hyperkalemia, some times loop diuretics for rapid treatment but given with K sparing diuretic (amiloride & trimetrine) or given K supplements.
Paracenthesis (aspiration of fluid LVP): 3-4 L can be taken over 1-2 hours specially in emergency to relieve the patient distress & we can repeat the aspiration of this amount if needed. To avoid PCD Support of circulation by colloid like human albumin solution in a dose of 8-10 gm for every liter of ascitic fluid aspirated or other plasma expander (Dextran, Polygeline) is indicated.
Le Veen shunt, by tube from peritoneum to internal jugular vein, it is effective treatment in resistant case but it can be complication by infection, S.V.C thrombosis & pulmonary edema.
Extracorporeal ultra filtration of ascitic fluid and IV or intra-peritoneal re-infusion can be used.
TIPS (trans jugular intra-hepatic porto-systemic stent shunt):-
By introducing stent through jugular vein to the liver for anastamosis the portal vein with systemic circulation.
Liver transplantation: In diuretic resistant ascites.
Spontaneous Bacterial Peritonitis
Abnormal gut permeability to bacteria.inability to clear infection.
Diagnosis made by paracentesis If ascites contains > 250 neutrophils/mm3.
First line therapy is third generation cephalosporin.
TREATMENT:
Treatment started immediately with broad spectrum antibiotics like cefotaxime.
Recurrence of this Condition is common and can be reduced by norfloxacin (400 mg/day).
Hepatic Encephalopathy
Hepatic encephalopathy is a neuropsychiatric syndrome caused by liver disease.Impaired hepatic metabolism of gut-derived neuroactive substances.
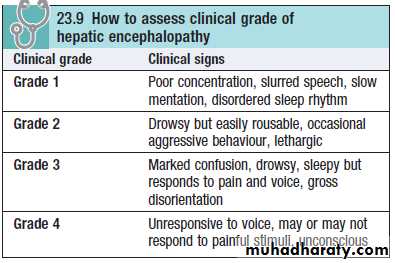
Clinical features:
Features include changes of intellect, personality, emotions and consciousness, with or without neurological signs (rare).As it progresses, confusion is followed by coma.
Convulsions sometimes occur.
Examination:
Fetor hepaticus, a sweet musty odour to the breathAsterixis
constructional apraxia
hyper-reflexia and bilateral extensor plantar responses
Rarely, chronic hepatic encephalopathy (hepatocerebral degeneration) gives rise to variable combinations of cerebellar dysfunction, Parkinsonian syndromes, spastic paraplegia and dementia.
Treatment: it is a reversible condition, unless it is a terminal stage
1. Remove the precipitating causes like:Uremia
Drugs (especially sedatives, antidepressants)
Dehydration (including diuretics, paracentesis)
Infection
Constipation
Trauma
Hypokalaemia
Excess dietary protein
↑Protein load (including GI bleeding)
Paracenthesis (vol.>3-5L.),
Portosystemic shunting
2. Also decrease protein intake < 20 g/day, glucose (300 g/day) is given orally or parentally in severe cases when the encephalopathy improve increase protein gradually
3. Antibiotics: For eradication of bacterial content of the bowel like Neomycine.
4. Lactulose: Multi-action (induce diarrhea, act as anti-bacterial agent.
5. In chronic encephalopathy liver transplantation is indicated.
HEPATORENAL SYNDROME
It is due to homodynamic dysfunction. The kidney structure is normal.Measure central venous pressure and give colloidal solutions like human albumin to maintain pressure between 0-5 cm of water.
Dopamine is given in a dose of (1-2/mg/kg/min.)
then diuretics
restrict protein intake to 20 g/day
Prognosis poor until liver transplantation is performed.
COAGLUPATHY
Deficient production of clotting and thrombocytopenia. Treatment: Oral vitamin K and platelet transfusion.