Date: 02/19/2014
Date: 02/19/2014Cardiology
Cardiology
Medicine
Medicine
Pgs. Num: 8
Pgs. Num: 8
Lec: 1
Lec: 1
Dr. Muzahim
Dr. Muzahim
Coronary Heart Disease (CHD)
Objectivesetiology
Risk factors of atherosclerosis
Clinical manifestations
Stable angina
Acute coronary syndrom (unstable angina & myocardial infarction)
Etiology
Disease of coronary arteries is almost always due to atheroma and its complications, particularly thrombosis.
Occasionally, the coronary arteries are involved in other disorders such as aortitis, polyarteritis, and other connective tissue disorders (vasculitis).
Risk Factors of Atheroma
Age and sex
Family history
Smoking
Hypertension
Hyperlipidemia
Diabets mellitus
Hemostatic factors
Physical inactivity
Obesity
Alcohol
Dietary factors
Personality
Social deprivation
Clinical manifestations
Stable angina
Unstable angina
Myocardial infarction
Heart failure
Arrhythmia
Sudden death
Angina pectoris
Is the symptom complex caused by transient myocardial ischaemia, it may occur when there is an imbalance between myocardial oxygen supply and demand.
Causes
1. Coronary atheroma is the most common cause of angina.
2. Other forms of heart disease:
a. aortic valve disease
b. hypertrophic cardiomyopathy.
Factors Precipitating Angina
Common
Physical exertion
Cold exposure
Heavy meals
Intense emotion
Uncommon
Lying flat (decubitus angina)
Vivid dreams (nocturnal angina)
Clinical features
The history Stable angina is characterized by central chest pain, discomfort or breathlessness that is precipitated by exertion or other forms of stress, and is promptly relieved by rest or by sublingual GTN. Usually few minutes in duration.
Physical examination is frequently negative, but should include a careful search for evidence of valve disease (particularly aortic), important risk factors (e.g. hypertension, diabetes), left ventricular dysfunction (e.g. cardiomegaly, gallop rhythm), other manifestations of arterial disease (e.g. carotid bruits, peripheral vascular disease) and unrelated conditions that may exacerbate angina (e.g. anemia, thyrotoxicosis).
Investigations
Resting ECG
The ECG is often normal but may show evidence of previous myocardial infarction occasionally, there is T-wave flattening or inversion in some leads, providing non-specific evidence of myocardial ischaemia or damage.
The most convincing ECG evidence of myocardial ischaemia is obtained by demonstrating reversible ST segment depression, with or without T-wave inversion, at the time the patient is experiencing symptoms (whether spontaneous or induced by exercise testing).
Exercise ECG
An exercise tolerance test (ETT) is usually performed using a standard treadmill or bicycle ergometer protocol. While monitoring the patient's ECG, blood pressure and general condition. Planar or down-sloping ST segment depression of 1 mm or more is indicative of ischemia; up-sloping ST depression is less specific and often occurs in normal individuals.
Exercise testing can be used to confirm or refute a diagnosis of angina and is also a useful means of assessing the severity of coronary disease and identifying high-risk individuals.
The amount of exercise which can be tolerated and the extent and degree of any ST segment change provide a useful guide to the likely extent of coronary disease.
False positive results in
a. the presence of digoxin therapy,
b. left ventricular hypertrophy,
c. left bundle branch block or
d. Wolff-Parkinson-White syndrome.
The predictive accuracy of exercise testing is lower in women than men. The test should be classed as inconclusive (and not negative) if the patient cannot achieve an adequate level
Other forms of stress testing
Myocardial perfusion scanningThis may be helpful in the evaluation of patients with an equivocal or uninterpretable exercise test and those who are unable to exercise; its predictive accuracy is higher than that of the exercise ECG.
Stress echocardiography
This is an alternative to myocardial perfusion scanning and can achieve similar predictive accuracy (superior to exercise ECG). The technique uses transthoracic echocardiography to identify ischaemic segments of myocardium and areas of infarction.
Coronary arteriography
Coronary arteriography provides detailed anatomical information about the extent and nature of coronary artery disease, and is usually performed with a view to coronary bypass grafting or percutaneous coronary intervention (PCI).
Management
The management of angina pectoris involves:
1. A careful assessment of the extent and severity of the disease.
2. The identification and control of significant risk factors (e.g. smoking, hypertension, hyperlipidaemia).
3. Control symptoms
4. Treatment to improve life expectancy
Treatment should start with a careful explanation of the problem, reassurance and a discussion of the potential lifestyle and medical interventions that may relieve symptoms and improve prognosis
ADVICE TO PATIENTS WITH STABLE ANGINA
Do not smoke
Aim at ideal body weight
Take regular exercise (exercise up to, but not beyond, the point of chest discomfort is beneficial and may promote collateral vessels)
Avoid severe unaccustomed exertion, and vigorous exercise after a heavy meal or in very cold weather
Take sublingual nitrate before undertaking exertion that may induce angina
Antiplatelet therapy
Low-dose (75-150 mg) aspirin reduces the risk of adverse events such as myocardial infarction and should be prescribed for all patients with coronary artery disease indefinitely. Clopidogrel (75 mg daily) is an equally effective antiplatelet agent that can be prescribed if aspirin causes troublesome dyspepsia or other side-effects.
Anti-anginal drug treatment
Five groups of drugs are used to help relieve or prevent the symptoms of angina:
1. Nitrates.
2. β-blockers.
3. Calcium antagonists.
4. Potassium channel activators.
5. I channel antagonist
Nitrates
These drugs act directly on vascular smooth muscle to produce venous and arteriolar dilatation; their beneficial effects in angina are due to a reduction in myocardial oxygen demand (lower preload and afterload) and an increase in myocardial oxygen supply (coronary vasodilatation).
Sublingual glyceryl trinitrate (GTN) administered from a metered-dose aerosol (400 μg per spray) or as a tablet (300 or 500 μg) allowed to dissolve under the tongue or crunched and retained in the mouth will usually relieve an attack of angina in 2-3 minutes.
Side effects include:
1. Headache
2. Hypotension
3. Rarely, syncope.
To avoid these symptoms the tablet may be spat out as soon as the angina is relieved. Patients often need to be reassured that GTN is not habit-forming and will not lose its effect if used repeatedly.
They should also be encouraged to use the drug prophylactically before engaging in exercise that is liable to provoke symptoms.
Sublingual GTN has a short duration of action
GTN can be given
Transcutaneously as a patch (5-10 mg daily),
As a slow-release buccal tablet (1-5 mg 6-hourly).
Other nitrates such as isosorbide dinitrate (10-20 mg 8-hourly) and isosorbide mononitrate (20-60 mg once or twice a day) can be given by mouth.
Headache is common but tends to diminish if the patient perseveres with the treatment.
Continuous nitrate therapy causes pharmacological tolerance and this should be avoided by using a regimen that includes a nitrate-free period of 6-8 hours every day.
Beta-blockers
These drugs lower myocardial oxygen demand by reducing heart rate, blood pressure and myocardial contractility. Unfortunately, they can exacerbate the symptoms of peripheral vascular disease and may provoke bronchospasm in patients with obstructive airways disease.
Calcium antagonists
These drugs inhibit the slow inward current caused by the entry of extracellular calcium through the cell membrane of excitable cells, particularly cardiac and arteriolar smooth muscle, and lower myocardial oxygen demand by reducing blood pressure and myocardial contractility.
Dihydropyridine calcium antagonists, such as:
Nifedipine and nicardipine, often cause a reflex tachycardia; it is often best to use these drugs in combination with a β-blocker.
Verapamil and diltiazem are particularly suitable for patients who are not receiving a β-blocker because they inhibit conduction through the AV node and tend to cause a bradycardia or even atrioventricular block in susceptible individuals.
The calcium antagonists may reduce myocardial contractility and can aggravate or precipitate heart failure. Other unwanted effects include peripheral oedema, flushing, headache and dizziness.
Potassium channel activators
This class of drug has arterial and venous dilating properties but does not exhibit the tolerance seen with nitrates. Nicorandil (10-30 mg 12-hourly orally) is the only drug in this class currently available for clinical use.
I channel antagonist
Ivabradine is the first class of drug.
It induces bradycardia by modulating ion channels in the sinus node.
It appears to be safe to use in patients with heart failure
Invasive treatment
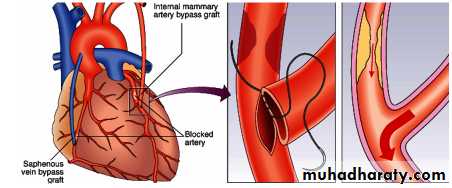
A. percutaneous transluminal coronary angioplasty, PTCA): Balloon and stent.
B. coronary artery bypass graft (CABG) surgery.
Coronary surgery is usually the preferred option in patients with three-vessel or left main disease, although recent trials have demonstrated that PCI is also feasible in such patients.
ANGINA WITH NORMAL CORONARY ARTERIES Approximately 10% of patients who report stable angina on effort will be found to have angiographically normal coronary arteries. Many of these patients are women and the mechanism of their symptoms is often difficult to establish.
Coronary artery spasm Vasospasm in coronary arteries may coexist with atheroma, especially in unstable angina , occasionally (< 1% of all cases of angina), however, vasospasm may occur without angiographically detectable atheroma. This form of angina is sometimes known as variant angina and may be accompanied by spontaneous and transient ST elevation on the ECG (Prinzmetal's angina).
Calcium antagonists, nitrates and other coronary vasodilators (e.g. nicorandil) are the most useful therapeutic agents but may be ineffective.
Syndrome X The constellation of typical angina on effort, objective evidence of myocardial ischaemia on stress testing, and angiographically normal coronary arteries is sometimes known as syndrome X. This disorder is poorly understood but carries a good prognosis and may respond to treatment with anti-anginal therapy.