
نماذج أسئلة في
)الطب الباطني (المرحلة السادسة
Q1:
A 35-year-old male patient presented with history of fever, fatigue, and
joint pain for three weeks duration. He gave history of dental extraction two
months ago. On examination: He looked ill, cardiac auscultation revealed an
apical pan systolic murmur radiated to left axilla. The spleen was just
palpable.
A. What is the likely diagnosis and the underlying cardiac valve lesion?
B. Mention 2 important investigations to confirm the diagnosis of his current
illness. Comment on the expected results.
C. What is your initial treatment of this patient?
Answer: A. infective endocarditis, mitral regurgitation
B. two important investigation:
1. Blood culture (3-6 sets of blood culture) should be taken prior to commencing.
Aseptic technique is essential. Aerobic and anaerobic cultures are required.
2. Echocardiography: particularly trans-oesophageal for detecting and following
the progression of vegetations, for assessing valve damage and for detecting abscess
formation.
C. Benzyl penicillin (1.2 g IV 4 hourly) and gentamicine (1 mg/KG IV 8-12 hourly). In
case of penicillin allergy, vancomycin (1 g 12 hourly IV) and gentamicin
Q2: A 60-year-old hypertensive lady, on hydrochlorothiazide 50 mg,
presented with a recent onset of polyuria, and polydypsia. Her BMI was 30,
BP: 160/100 mmHg. Fasting blood sugar was 12mmol/L.
A. What do you think the cause of her recent symptoms?
B. Mention 5 most important investigations you should do for her? Comment on
the significance of each test.
C. Outline the treatment of this patient.
Answer: A. Type 2 diabetes mellitus
B. 1. ECG: for changes of CAD and LVH
2. Echocardiography: to detect LVH and assessment of LV function
3. lipid profile: to detect dyslipidaemia
4. renal function test (including serum urea, creatinine and electrolytes)
5. serum uric acid (for associated hyperuricaemia)
6. GUE (for proteinuria)
C. Treatment:
Life style modification: patient education, weight reduction, regular exercise and reduction
of foods with high glycaemic index (like refined sugars), restriction of fatty food and salt,
with increased consumption of fruits and vegetables and oily fish
If hyperglycaemia is not controlled by the above measures, add metformin.

For hypertyension, hydrochlorothizide should be replaced by an ACE inhibitor (like
enalapril)or ARB (like valsartan).
Q3: A 30–year-old male patient with history of bloody diarrhea during the
last six weeks. He is admitted by his physician to the medical ward for
investigations.
A. If he develops tender hepatomegaly and general stool examination
is positives for trophozoites of certain parasites.
B. If the colonoscopy shows presence of mucosal inflammation, diffuse
ulcers and loss of mucosal vascular pattern involving the left side of
colon.
C. If this condition follows a several courses of different antibiotics for
treatment of a recurrent chest infection.
According to the above information mentioned in a, b, and c about the
patient's condition; answer the following questions:
1.
The most likely diagnosis in each of A, B, and C.
2. Mention another confirmatory test (investigation) for each of the
above diagnoses.
3. Describe briefly the drug therapy for each condition.
Answer: 1. A. amoebiasis , B. ulcerative colitis, C. pseudomembranous colitis
2. A. Ultrasound scan (for confirmation of liver abscess), serology (immunoflorescent
antibody detection) , or DNA detection (by PCR)
B. colonoscopic biopsy (showing the inflammation to be limited to the mucosa and spares
the deeper layers of the bowel wall, with acute and chronic inflammatory cell infiltration,
crypt abscess and loss of goblet cells)
C. colonoscopic appearance of adherent pseudomembrane, or essay for Cl. difficile toxin in
stool (using ELISA).
3. A. metronidazol 800 mg 8 hourly for 5-10 days, or tinidazol 2 g once daily for 3 days,
followed by diloxanide furoate, or paromomycin 500 mg 8 hourly for 10 days.
B. oral aminosalicylate (like mesalazine), combined with topical aminosalicylate
and corticosteroids. Oral prednisolone (40 mg daily) is indicated if initial therapy is
ineffective.
C. metronidazole 400 mg 8 hourly or vancomycin 125 mg 6 hourly orally

Q4: A 25-year-old male patient admitted to hospital with history of sudden
onset of severe generalized headache for six hours duration, followed later
by loss of consciousness. On examination: the patient was comatose, with
neck stiffness, normal temperature and no focal neurological signs.
A. What is the most likely diagnosis?
B. Mention 2 important investigations to confirm the diagnosis? Comment on the
expected results.
C. Mention the main lines of management.
Answer: A. subarachnoid haemorrhage
B. emergency CT (negative ion 15% of cases), if negative, lumbar puncture 12
hours after onset of symptoms. The CSF will be shown bloody or xanthochromic.
C. nimodipine 30 – 60 IV for 5 – 14 days followed by oral nimodipine 360 mg for
further 7 days. Referral to a neurosurgeon. Treatment of complications including obstructive
hydrocephalus, hyponatraemia, chest infection and venous thrombosis.
Q5:
A 63-year-old man who is a chronic heavy smoker presented with
worsening cough and hoarseness of voice of 3 months duration. On
examination: there was clubbing of fingers with dullness on percussion and
diminished breathing on auscultation at the left middle part of the chest.
A. What is the most likely diagnosis?
B. What investigations do you recommend to confirm the diagnosis. Comment on
the expected results.
C.
Enumerate three complications of this disease
.
Answer: A. bronchial carcinoma
B. 1. Chest X-ray: left hilar and lobar collapse
2. CT scan for assessment of tumour spread and guiding biopsy
3. bronchoscope and biopsy
C. (Any three of the following)
1. complications caused by local spread (like recurrent pneumonia, lung
abscess and pleural effusion)
2. complications caused by mediastinal spread (like superior vena cava
obstruction, oesophageal involvement, pericardial effusion and left recurrent laryngeal
nerve involvement (as in this patient))
3. metastatic spread (manifesting as epileptic seizure, jaundice and weight
loss)
4.non-metastatic extrapulmonary complication (like SIADH, hypercalcaemia
and ectopic ACTH secretion)
Single choice Questions:
The following are true regarding typhoid fever, except:
A. Incubation period is about 7-21 days.
B. A characteristic pink rash may appear on the trunk at the end of the first
week.
C. The intestine may perforate at the site of ulcerated Peyer's patches.
D. Stool culture is more likely to be positive than blood culture in the first
week.
E. Ceftriaxone is an effective once daily treatment.
Antibiotics are usually indicated in all the following cases of acute
diarrhea, except:
A. Staphylococcal food poisoning.
B. Bloody diarrhea caused by Shigella flexneri.
C. Cholera during an outbreak.
D. Bloody diarrhea in association with salmonellosis.
E. Non specific diarrhea with severe systemic toxicity
The following are true regarding ancyclosmiasis (hookworm
infestation), except:
A. Pulmonary eosinophilia may develop during larval migration.
B. The disease is acquired through larval penetration of the skin.
C. Iron deficiency anaemia is the most important clinical presentation.
D. `
E. Metronidazole is the drug of choice.
One of the following features is unlikely to occur in "tetanus":
A. Opisthotonus.
B. Dysphagia.
C. Apnoea.
D. Painful spasm of masseter muscles.
E. Tachycardia.
All of the following drugs can be used in the treatment of malaria,
except:
A. Chloroquine.
B. Praziquantel.
C. Primaquine.
D. Sulfadoxine.
E. Doxycycline.
Metabolic alkalosis occurs in the following conditions, except:
A. Acute pulmonary embolism.
B. Conn's syndrome.
C. Pyloric obstruction.
D. Thiazide diuretics.
E. Corticosteroid therapy.
Which of the following is the least likely to be associated with renal
failure?
A. Multiple myeloma.
B. Idiopathic thrombocytopenia.
C. Infective endocarditis.
D. SLE.
E. Systemic sclerosis.
The safest drug to be given to a patient with renal failure is:
A. Amphotericin B.
B. Indomethacin.
C. Ciprofloxacin.
D. Amikacin.
E. Co-trimoxazole.
Causes of hypokalaemia include all the following, except:
A. Villous adenoma of the rectum.
B. Renal tubular acidosis.
C. Licorice drinks.
D. Conn's syndrome (hyperaldosteronism).
E. B-blockers.
One of the following diseases is associated with respiratory acidosis?
A. Chronic obstructive pulmonary disease.
B. Pneumonia.
C. Acute renal failure.
D. Hyperventilation.
E. Acute gastroenteritis
Thrombocytopenia may be associated with all the following conditions,
except:
A. Hypersplenism.
B. HIV virus.
C. Vitamin B
12
deficiency.
D. Heparin therapy .
E. Chronic myeloid leukaemia.
All the following are true about megaloblastic anaemia, except:
A. Mild jaundice.
B. Anticonvulsant drugs are recognized causes.
C. MCV is 85 fl.
D. High reticulocyte count after giving treatment means a good response.
E. Addisonian pernicious anaemia is due to B
12
deficiency.
Which of the following is true in haemophilia A?
A. It is an x-linked recessive disorder.
B. It is due to factor IX deficiency.
C. Activated partial thromboplastin time (APTT) is normal.
D. Treatment with cryoprecipitate is useless.
E. Haemarthrosis doesn't occur in proximal joints.
Regarding Hodgkin's lymphoma; the following are true, except:
A. It usually presents as painless, rubbery lymphadenopathy of the neck.
B. Presence of lymphopenia is a good prognostic factor.
C. Raised LDH level is an adverse prognostic factor.
D. Lymph node biopsy characteristically shows the presence of Reed
Sternberg of B cell origin.
E. Radiotherapy is the treatment of choice for stage I disease.
Regarding chronic myeloid leukaemia (CML); the following are true,
except:
A. It is associated with Philadelphia chromosome in about 95% of cases.
B. It causes abdominal pain and fullness.
C. It is a recognized cause of huge splenomegaly.
D. Peripheral blood film often shows decreased number in the basophils and
eosinophils.
E. Imatinib is a first line therapy.
The least likely cause of polyarthritis is:
A. Rheumatoid arthritis.
B. Acromegaly.
C. Viral arthritis.
D. Tuberculosis.
E. Psoriasis.
All the following are characteristics of nodal generalized osteoarthritis,
except:
A. Symmetrical involvement of interphalangeal joints.
B. Presence of Heberden's nodes.
C. More common in male.
D. Peak onset at middle age.
E. Strong genetic predisposition.
Clinical features of seronegative of spondarthritis include the following,
except:
A. Sacroiliitis and inflammatory spondylitis.
B. Conjunctivitis.
C. Nail dystrophy.
D. Inflammatory enthesitis.
E. Association with aortic valve stenosis.
The following are features of systemic lupus erythematosus (SLE),
except:
A. Butterfly rash of the face.
B. Oral ulceration.
C. Non-erosive arthritis of the wrist joints.
D. Seizure or psychosis.
E. Lymphocytosis.
The following are recognized causes of osteoporosis, except:
A. Hyperparathyroidism.
B. Inflammatory bowel disease.
C. Heparin.
D. Obesity.
E. Immobilization.
Regarding gout; the following are true, except:
A. Primary gout is almost exclusively a male disease.
B. Shoulder joint is usually involved in the first attack.
C. Acute attack may simulate septic arthritis and cellulitis.
D. Indomethacin is effective treatment of the acute attack.
E. Allopurinol is of no benefit during the acute attack.
The following are recognized causes of hyperuricaemia, except:
A. Chronic renal failure.
B. Polycythaemia rubra vera.
C. Low-dose aspirin.
D. Alcohol
E. Sulfinpyrazone.
The following are recognized causes of osteoporosis, except:
A. Hyperparathyroidism.
B. Inflammatory bowel disease.
C. Heparin.
D. Obesity.
E. Immobilization.
In sepsis; all the following are true, except:
A. Blood culture is commonly negative.
B. Fungi are particularly important causes in neutropenic patients.
C. The infection may remain confined to the infected organ without
bloodstream invasion.
D. APC (activated protein C) activates the coagulation cascade.
E. Renal failure may result from acute tubular necrosis.
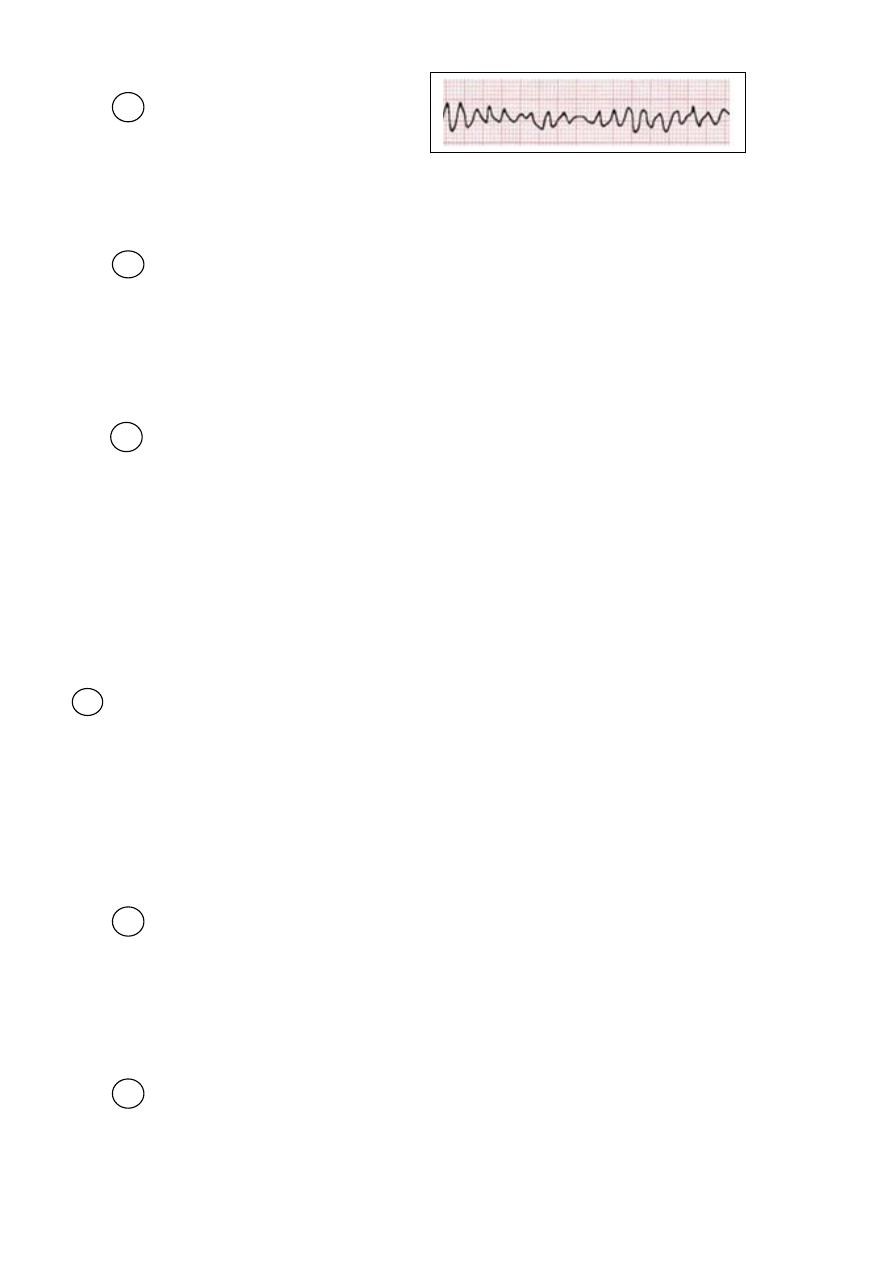
What does this ECG strip show?
A. Ventricular tachycardia.
B. Ventricular fibrillation.
C. Atrial fibrillation.
D. Supraventricular tachycardia.
E. Atrial flutter.
Which of the following is the most highly characteristic of osteomalacia?
A. Raised serum alkaline phosphatase.
B. Pseudo-fractures (Looser zones) on x-ray.
C. Bone tenderness.
D. Waddling gait.
E. Difficulty on rising up from a chair
The following are criteria for diagnosis of rheumatoid arthritis, except:
A. Duration of at least 3 weeks.
B. Presence of rheumatoid nodules.
C. Arthritis of hand joints.
D. Arthritis of three or more joint areas.
E. Symmetrical arthritis
All the following findings support the diagnosis of AIDS in a young male,
except:
A. Presence of multiple, purple skin nodules.
B. Esophagoscope shows extensive white plaques covering the wall.
C. CT of the brain shows multiple ring enhancing lesions.
D. Blood count shows lymphocyte count of > 2x10
9
/L.
E. Chest x-ray shows bilateral non homogenous opacities.
The following drugs (poisons) are effectively removed by dialysis in
overdose, except:
A. Salicylate.
B. Theophylline.
C. Carbamazepine.
D. Methanol.
E. Digoxin.
Regarding the management of acute pulmonary oedema; all the
following are of benefit, except:
A. High flow oxygen.
B. Furosemide I. V .
C. Nitroglycerine by intravenous infusion.
D. Morphine I. V.
E. Propranolol.
